Our objective was to compare the rate of complications in thoracolumbar fractures that occurred during the early postoperative period in patients with multiple high-energy trauma according to the time of surgery. As a secondary objective, to estimate which variables were associated with surgery before 72h.
Material and methodsRetrospective analysis of a series of patients with thoracolumbar fractures and multiple associated injuries in other anatomical regions due to high energy trauma. Surgically treated in an occupational trauma referral center, by the same surgical team and during the period between January 2013 and December 2019.
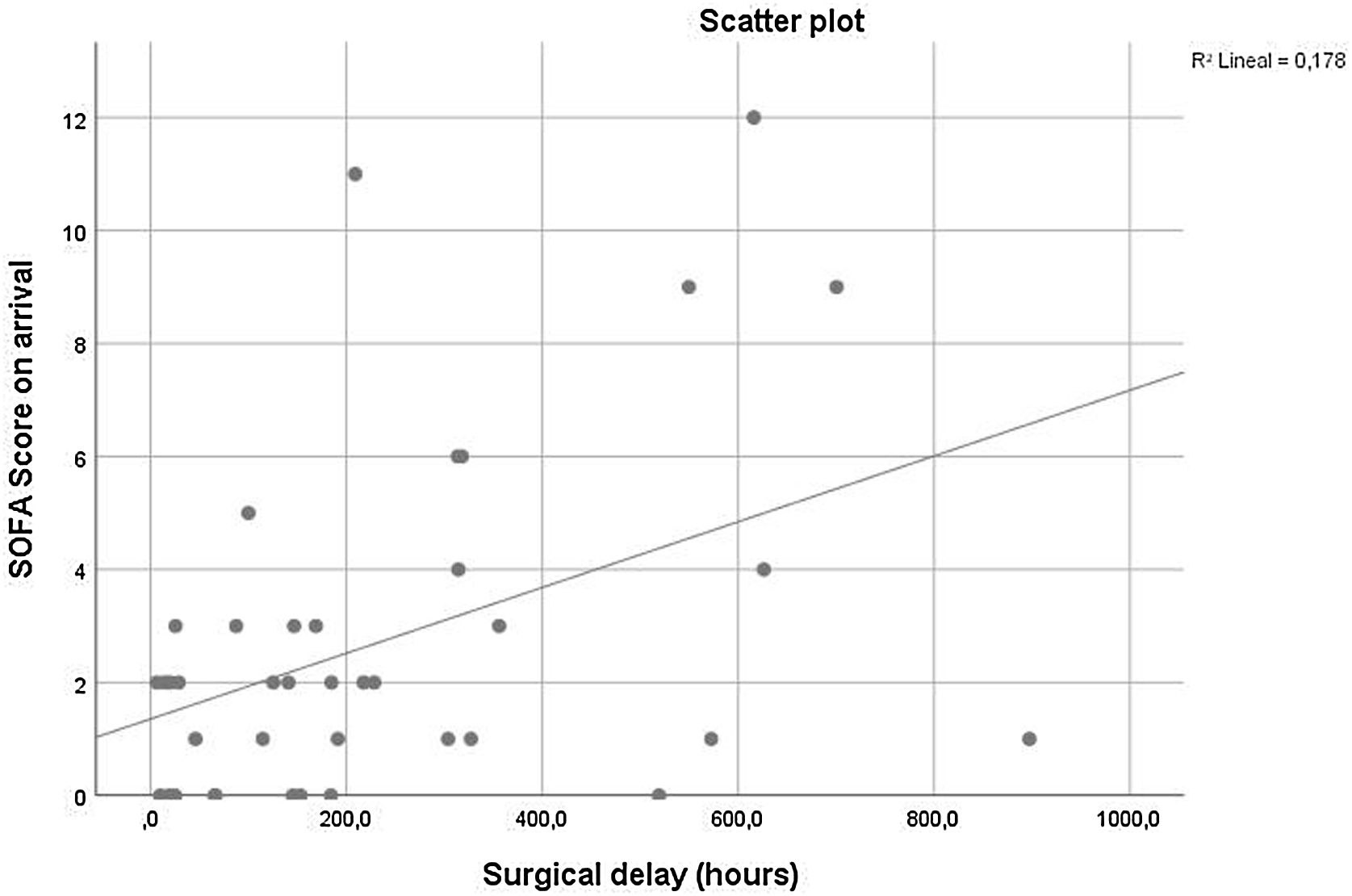
ResultsWe analyzed a sample of 40 patients (39 men and 1 woman). The rate of complications was independent of surgical delay (before and after 72h) (p=0.827). There were statistically significant differences between early and later surgery groups in the variables age, systolic blood pressure, initial SOFA score and presence of neurological damage (p=0.014; p=0.029; p=0.032; p=0.012). The overall surgical delay was correlated with the SOFA score (p=0.007).
ConclusionThe rate of early postoperative complications did not show significant differences between the early and late surgery groups. We observed that the patients who had been operated before 72h from trauma were younger, had more association with neurological syntoms, presented higher blood pressure values and less physiological damage. Surgical delay was positively correlated with SOFA score on arrival.
Nuestro objetivo es comparar la tasa de complicaciones acontecidas durante el postoperatorio temprano de fracturas toracolumbares en pacientes con traumatismos múltiples de alta energía según el momento de la cirugía. Como objetivo secundario, estimar qué variables se asociaron el desarrollo de la cirugía antes de las 72h.
Materiales y métodosAnálisis retrospectivo de una serie de pacientes con fracturas toracolumbares y múltiples lesiones asociadas en otras regiones anatómicas por traumatismo de alta energía. Tratados quirúrgicamente en un centro de derivación de trauma laboral, por el mismo equipo quirúrgico y durante el período comprendido entre enero de 2013 y diciembre de 2019.
ResultadosSe incluyeron 40 pacientes (39 hombres y una mujer). La tasa de complicaciones tempranas fue independiente del momento de la cirugía (antes o después de las 72h) (p=0,827). Se presentaron diferencias estadísticamente significativas entre ambos grupos en las variables edad, presión arterial sistólica, puntuación SOFA inicial y presencia de daño neurológico (p=0,014; p=0,029; p=0,032; p=0,012). La demora quirúrgica global se correlacionó con el puntuación SOFA al ingreso (p=0,007).
ConclusiónLa tasa de complicaciones en el postoperatorio temprano de fracturas toracolumbares no mostró diferencias significativas entre los grupos de cirugía temprana y tardía. Los pacientes operados antes de las 72h del trauma fueron más jóvenes, presentaron valores más elevados de presión arterial, menor daño fisiológico y asociaron síntomas neurológicos con mayor frecuencia. La demora quirúrgica se correlacionó positivamente con la puntuación SOFA al ingreso.
Traumatic thoracolumbar fractures are associated with high morbidity, mortality and socioeconomic impact.1 Its surgical timing in high-energy multiple trauma patients remains controversial. Associated life-threatening injuries and clinico-physiological heterogeneity of these patients make it difficult to develop quality clinical trials to determine guidelines.2 In addition, there is great variability in “polytrauma patient” definition in the literature. This group of patients is especially vulnerable to vertebral injuries, with an incidence of 36% according to published records.3,4
There is a certain consensus on the benefit on neurological recovery of early surgery for thoracolumbar fractures with associated neurological deficit. However, the amount of evidence on the clinical impact of early surgery and the rate of complications in multiple trauma patients is still controversial. Additionally the available literature has a highly variable definition of what is considered “early” surgery, ranging from <8 to <72h after injury.5–7
Bellabarba et al. after a systematic review recommended that ideally, patients with unstable thoracic fractures should undergo early stabilization (<72h) of their injury to reduce morbidity and possibly mortality. The literature suggests that early surgical intervention would be associated with shorter hospitalization time, shorter stay in the intensive care unit (ICU) and morbidity. In fact, authors propose early stabilization in the framework of “Damage Control Surgery” in severely injured trauma patients.8–11
In contrast, other authors have observed a higher rate of complications associated with the “second impact” of spinal surgery, especially in thoracic fractures.12–14
Our objective is to compare the rate of complications in the early postoperative period of thoracolumbar fractures in patients with high-energy multiple trauma according to the surgical time. Additionally to estimate the variables that were associated with the surgical timing decision in our case series.
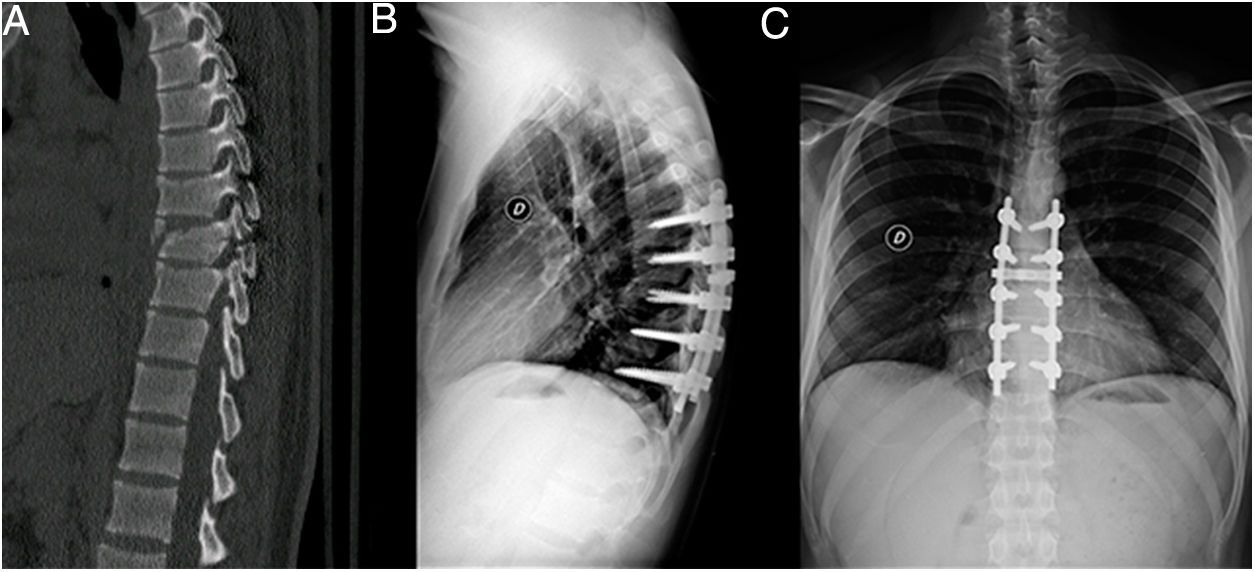
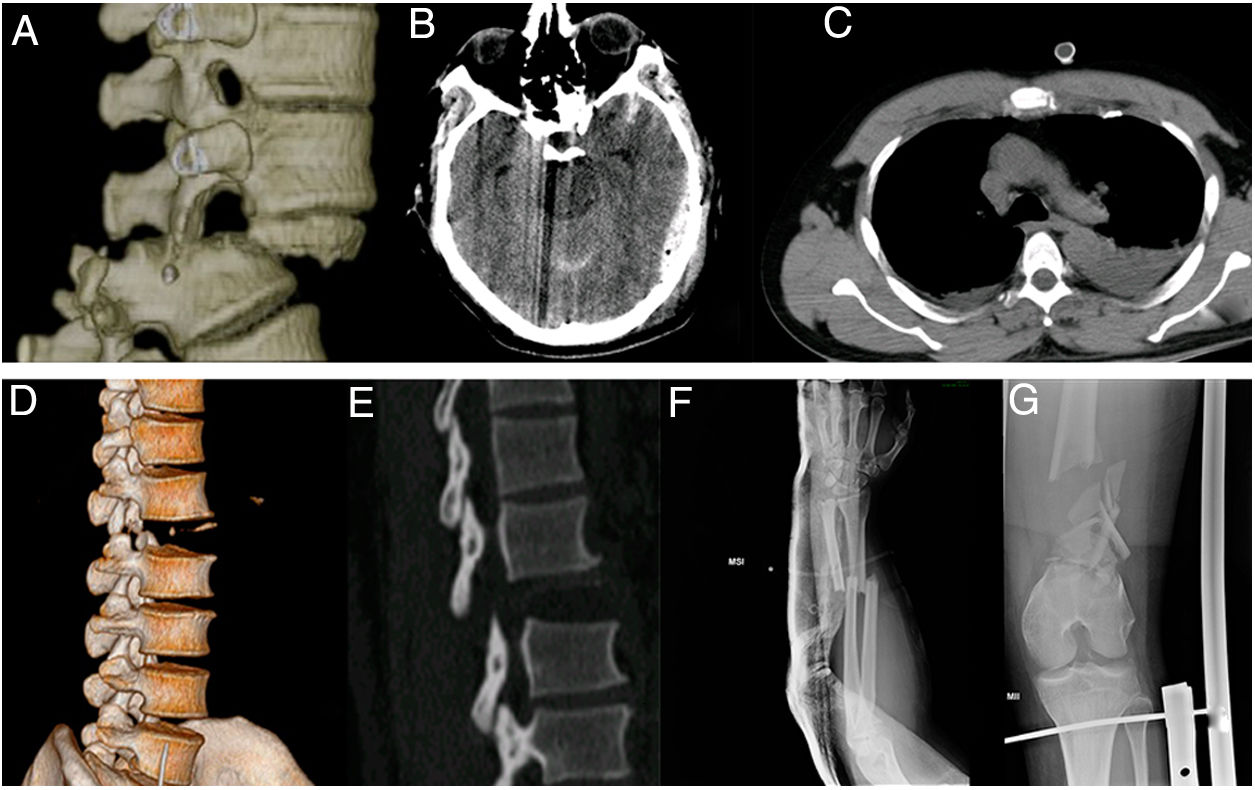
Material and methodsWe conducted a retrospective observational study of patients with thoracolumbar fractures caused by high-energy trauma with significant associated injuries in other anatomical regions (Fig. 1). Surgically treated in our institution, a reference center for occupational trauma, by the same surgical team and during the period between January 2013 and December 2019. Inclusion criteria: patients treated surgically for high-energy thoracolumbar vertebral fractures with multiple trauma. We define multiple trauma patients as those with significant non-vertebral injuries. “Significant” was defined using the AIS (Abbreviated Injury Scale) greater than or equal to 3.15 Exclusion criteria: incomplete medical records, arrival time greater than 72h from the trauma, penetrating trauma and patients undergoing percutaneous surgical procedures.
Data were obtained from medical records and images of our institution. Thoracolumbar spine images were analyzed and classified by two senior authors, and clinical scores were assessed by independent intensive care physicians of our institution. As a dependent variable we record the number of complications during the early postoperative period defined as the first 10 days after surgery. The complications were classified into “clinical complications” (death, bacteremia, pneumonia, acute respiratory distress syndrome (ARDS), multiple organ failure, nosocomial infections and septic shock), “surgical complications” (intraoperative, associated with the evolution of the wound, the fracture and the implant) and “other complications” (grouping those associated with prolonged hospitalization and traumatic comorbidities).
Additionally, we measured as secondary outcome variables: postoperative neurological status according to “American Spinal Cord Association impairment scale” (ASIA) at last available follow-up,16 length of stay in intensive care unit (ICU) and physiological status after surgery estimated by “Sequential Organ Failure Assessment” score (SOFA).17 SOFA is a scoring system used for patients admitted to the ICU to determine the level of organ dysfunction and the risk of mortality. It includes the variables PaO2/FiO2, number of platelets, Glasgow scale, bilirubin, mean arterial pressure and creatinine.
The main independent variable was surgical delay defined as the period of time from injury to spine surgery (h). Other independent variables recorded were age, sex, type of trauma, previous comorbidities, thoracolumbar fractured vertebra, vertebral region (thoracic or lumbar), type of injury according AO Spine thoracolumbar injury classification system (AOSTLICS),18 ASIA on arrival, Injury Severety Score (ISS),19 significant injuries in other anatomical regions (“Head”, “Neck and Cervical Spine”, “Face”, “Thorax and Thoracic spine”, “Abdomen and Lumbar Spine”, “Pelvis and Limbs” and “External or Skin”) defined according to an Abbreviated Injury Scale greater than or equal to 3,15 previous damage control surgery, other major surgeries, physiological status on arrival according to SOFA, polytraumatized criteria according to Berlín Definition (“2 or more significant lesions and presence of 1 or more of the following pathological conditions: arterial hypotension less than 90mmHg, Glasgow scale less than 8, base excess than −6.0, partial thromboplastin time or PTT greater than or equal to 40s, international normalized ratio or INR greater or equal to 1.4, age greater than or equal to 70 years”),3 arterial lactic acid on arrival and intercurrences previous to spine surgery, type of surgery and levels of fusion.
The authors made a comparison between two groups based on surgical delay less than or greater than 72h (early or late surgery, respectively). We decided to use this time cut point on the basis that it is the most used time interval in previous studies according to our bibliographic review.8,10,12
In our center, the decision-making on timing of surgery for unstable thoracolumbar fractures had been done through an interdisciplinary work guided by the intensive care unit/emergency physicians, who were responsable of the initial management and resuscitation. This process included the participation of our spine team and others specialists according to the associated injuries (Pelvis and hip, Lower limb, Upper limb, Plastic Surgery, General Surgery, Vascular surgery, Neurosurgery). The clinical and neurological status on arrival, and the treatment of life-threatening injuries (damage control surgery) were prioritized.
Ethical approval was granted by the research ethics committee of our institution and informed written consent for the publication of patient information and images was provided by the patients or by a legally authorized representative.
Statistical analysis: the categorical variables were expressed in number and percentage and were analyzed by the Chi Square method or Fisher's test. The interval variables were described with the mean and median, according to the type of distribution and dispersion measure: standard deviation (SD) or 25–75 interquartile range (IQR). The Shapiro Wilk normality test was performed to estimate the type of distribution of the quantitative variables. For the comparison of continuous variables, the Student's T test or the Mann–Whitney U test were used, according to the distribution expressed. The Pearson correlation test was performed for the analysis of continuous variables. Values of p<0.05 were considered statistically significant. SPSS Statics 25 software was used for the analysis.
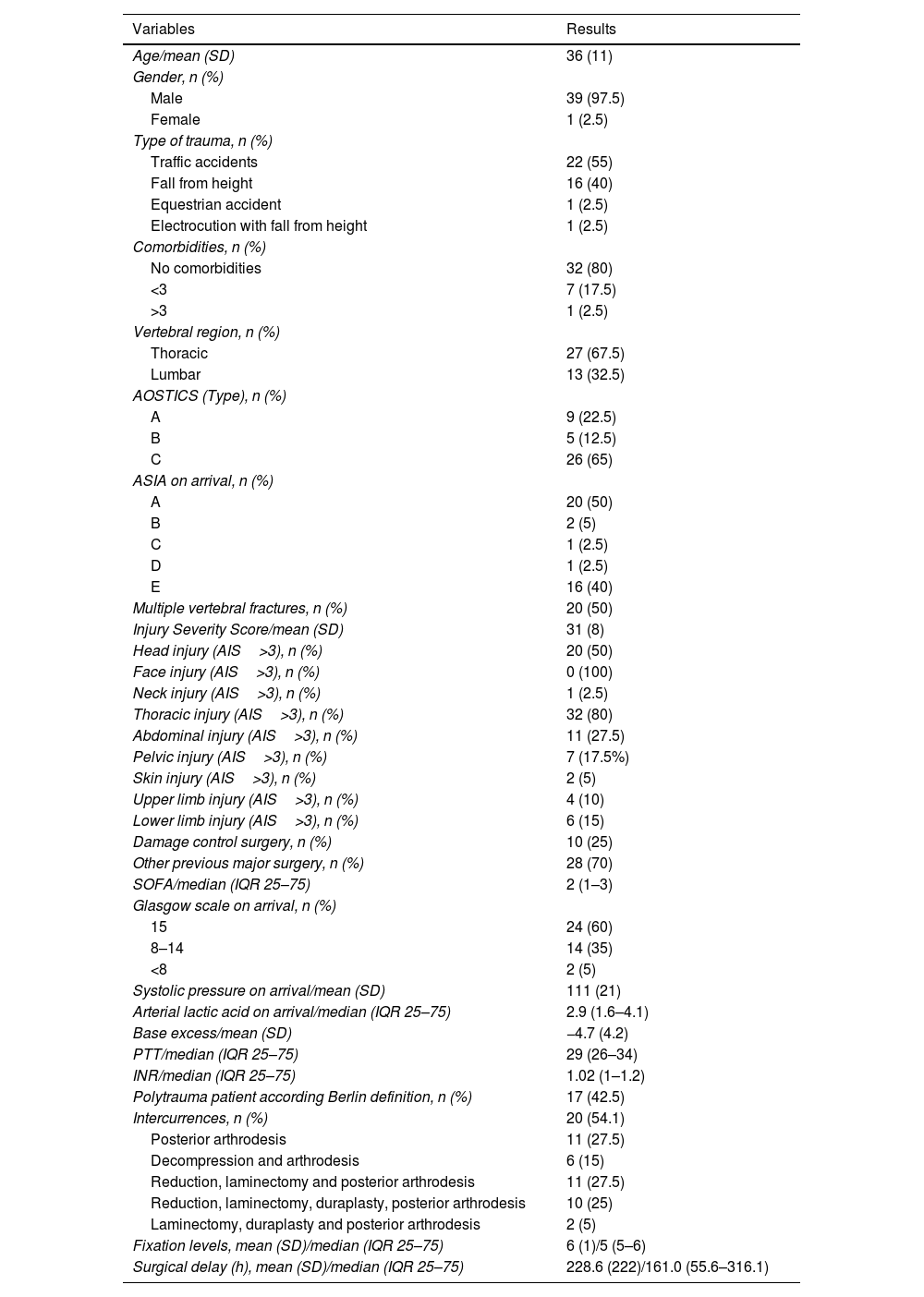
ResultsWe revised 104 patients surgically treated for thoracolumbar high energy trauma fractures during the study period of time. We included 54 patients with associated significant injuries in other anatomical regions and 14 patients were excluded according to our exclusion criteria (penetrating injuries: 3 cases; arrival time greater than 72h from the trauma: 11 cases). So our sample comprised 40 patients (39 males and 1 female). The types of trauma were 22 traffic accidents (55%), 16 fall from height (40%), 1 equestrian accident (2.5%) and 1 electrocution with fall from height (2.5%). All patients were treated by conventional posterior approach and surgical procedures were 11 arthrodesis (27.5%), 6 decompression and arthrodesis (15%), 11 reduction, decompression and arthrodesis (27.5%), 10 reduction, decompression, duraplasty and arthrodesis 25%, 2 decompression, duraplasty and arthrodesis (5%). Median fixation levels were 5 (IRQ=5–6). The description of the sample was summarized in Tables 1 and 2.
Sample description (independent variables).
| Variables | Results |
|---|---|
| Age/mean (SD) | 36 (11) |
| Gender, n (%) | |
| Male | 39 (97.5) |
| Female | 1 (2.5) |
| Type of trauma, n (%) | |
| Traffic accidents | 22 (55) |
| Fall from height | 16 (40) |
| Equestrian accident | 1 (2.5) |
| Electrocution with fall from height | 1 (2.5) |
| Comorbidities, n (%) | |
| No comorbidities | 32 (80) |
| <3 | 7 (17.5) |
| >3 | 1 (2.5) |
| Vertebral region, n (%) | |
| Thoracic | 27 (67.5) |
| Lumbar | 13 (32.5) |
| AOSTICS (Type), n (%) | |
| A | 9 (22.5) |
| B | 5 (12.5) |
| C | 26 (65) |
| ASIA on arrival, n (%) | |
| A | 20 (50) |
| B | 2 (5) |
| C | 1 (2.5) |
| D | 1 (2.5) |
| E | 16 (40) |
| Multiple vertebral fractures, n (%) | 20 (50) |
| Injury Severity Score/mean (SD) | 31 (8) |
| Head injury (AIS>3), n (%) | 20 (50) |
| Face injury (AIS>3), n (%) | 0 (100) |
| Neck injury (AIS>3), n (%) | 1 (2.5) |
| Thoracic injury (AIS>3), n (%) | 32 (80) |
| Abdominal injury (AIS>3), n (%) | 11 (27.5) |
| Pelvic injury (AIS>3), n (%) | 7 (17.5%) |
| Skin injury (AIS>3), n (%) | 2 (5) |
| Upper limb injury (AIS>3), n (%) | 4 (10) |
| Lower limb injury (AIS>3), n (%) | 6 (15) |
| Damage control surgery, n (%) | 10 (25) |
| Other previous major surgery, n (%) | 28 (70) |
| SOFA/median (IQR 25–75) | 2 (1–3) |
| Glasgow scale on arrival, n (%) | |
| 15 | 24 (60) |
| 8–14 | 14 (35) |
| <8 | 2 (5) |
| Systolic pressure on arrival/mean (SD) | 111 (21) |
| Arterial lactic acid on arrival/median (IQR 25–75) | 2.9 (1.6–4.1) |
| Base excess/mean (SD) | −4.7 (4.2) |
| PTT/median (IQR 25–75) | 29 (26–34) |
| INR/median (IQR 25–75) | 1.02 (1–1.2) |
| Polytrauma patient according Berlin definition, n (%) | 17 (42.5) |
| Intercurrences, n (%) | 20 (54.1) |
| Posterior arthrodesis | 11 (27.5) |
| Decompression and arthrodesis | 6 (15) |
| Reduction, laminectomy and posterior arthrodesis | 11 (27.5) |
| Reduction, laminectomy, duraplasty, posterior arthrodesis | 10 (25) |
| Laminectomy, duraplasty and posterior arthrodesis | 2 (5) |
| Fixation levels, mean (SD)/median (IQR 25–75) | 6 (1)/5 (5–6) |
| Surgical delay (h), mean (SD)/median (IQR 25–75) | 228.6 (222)/161.0 (55.6–316.1) |
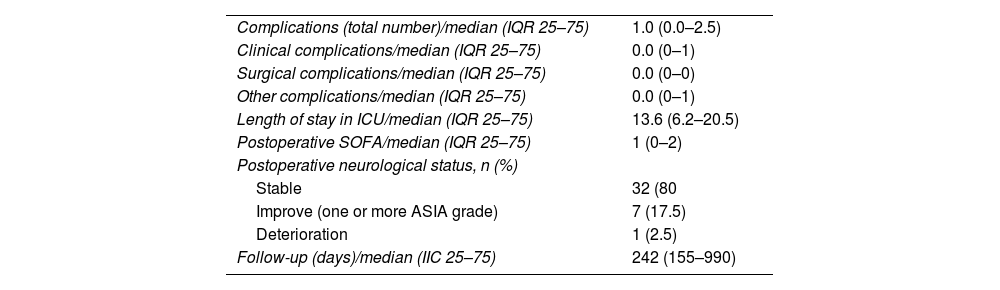
Sample description (dependent variables).
| Complications (total number)/median (IQR 25–75) | 1.0 (0.0–2.5) |
| Clinical complications/median (IQR 25–75) | 0.0 (0–1) |
| Surgical complications/median (IQR 25–75) | 0.0 (0–0) |
| Other complications/median (IQR 25–75) | 0.0 (0–1) |
| Length of stay in ICU/median (IQR 25–75) | 13.6 (6.2–20.5) |
| Postoperative SOFA/median (IQR 25–75) | 1 (0–2) |
| Postoperative neurological status, n (%) | |
| Stable | 32 (80 |
| Improve (one or more ASIA grade) | 7 (17.5) |
| Deterioration | 1 (2.5) |
| Follow-up (days)/median (IIC 25–75) | 242 (155–990) |
The results of comparing two groups of patients according to the hours from injury to surgery (before or after 72h) are summarized in Tables 3 and 4.
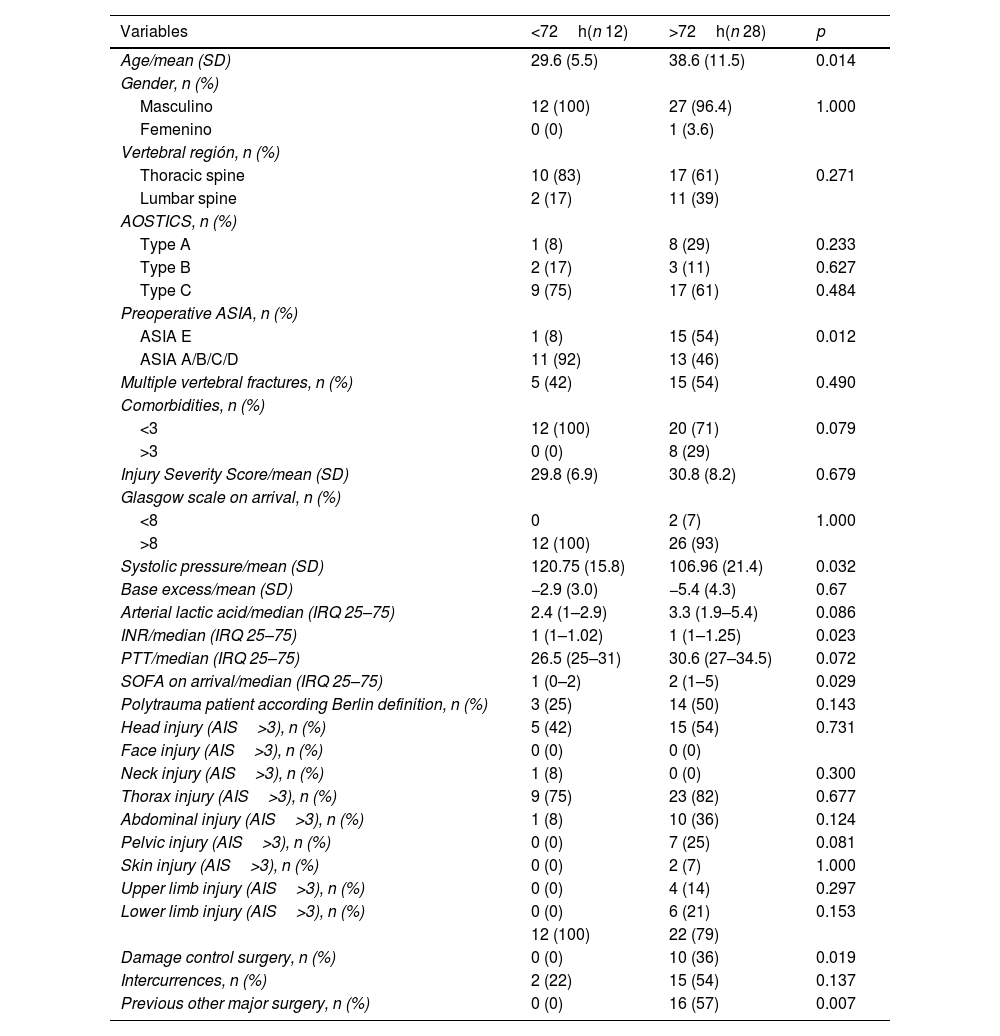
Comparison of independent variables between groups according to surgical timing.
| Variables | <72h(n 12) | >72h(n 28) | p |
|---|---|---|---|
| Age/mean (SD) | 29.6 (5.5) | 38.6 (11.5) | 0.014 |
| Gender, n (%) | |||
| Masculino | 12 (100) | 27 (96.4) | 1.000 |
| Femenino | 0 (0) | 1 (3.6) | |
| Vertebral región, n (%) | |||
| Thoracic spine | 10 (83) | 17 (61) | 0.271 |
| Lumbar spine | 2 (17) | 11 (39) | |
| AOSTICS, n (%) | |||
| Type A | 1 (8) | 8 (29) | 0.233 |
| Type B | 2 (17) | 3 (11) | 0.627 |
| Type C | 9 (75) | 17 (61) | 0.484 |
| Preoperative ASIA, n (%) | |||
| ASIA E | 1 (8) | 15 (54) | 0.012 |
| ASIA A/B/C/D | 11 (92) | 13 (46) | |
| Multiple vertebral fractures, n (%) | 5 (42) | 15 (54) | 0.490 |
| Comorbidities, n (%) | |||
| <3 | 12 (100) | 20 (71) | 0.079 |
| >3 | 0 (0) | 8 (29) | |
| Injury Severity Score/mean (SD) | 29.8 (6.9) | 30.8 (8.2) | 0.679 |
| Glasgow scale on arrival, n (%) | |||
| <8 | 0 | 2 (7) | 1.000 |
| >8 | 12 (100) | 26 (93) | |
| Systolic pressure/mean (SD) | 120.75 (15.8) | 106.96 (21.4) | 0.032 |
| Base excess/mean (SD) | −2.9 (3.0) | −5.4 (4.3) | 0.67 |
| Arterial lactic acid/median (IRQ 25–75) | 2.4 (1–2.9) | 3.3 (1.9–5.4) | 0.086 |
| INR/median (IRQ 25–75) | 1 (1–1.02) | 1 (1–1.25) | 0.023 |
| PTT/median (IRQ 25–75) | 26.5 (25–31) | 30.6 (27–34.5) | 0.072 |
| SOFA on arrival/median (IRQ 25–75) | 1 (0–2) | 2 (1–5) | 0.029 |
| Polytrauma patient according Berlin definition, n (%) | 3 (25) | 14 (50) | 0.143 |
| Head injury (AIS>3), n (%) | 5 (42) | 15 (54) | 0.731 |
| Face injury (AIS>3), n (%) | 0 (0) | 0 (0) | |
| Neck injury (AIS>3), n (%) | 1 (8) | 0 (0) | 0.300 |
| Thorax injury (AIS>3), n (%) | 9 (75) | 23 (82) | 0.677 |
| Abdominal injury (AIS>3), n (%) | 1 (8) | 10 (36) | 0.124 |
| Pelvic injury (AIS>3), n (%) | 0 (0) | 7 (25) | 0.081 |
| Skin injury (AIS>3), n (%) | 0 (0) | 2 (7) | 1.000 |
| Upper limb injury (AIS>3), n (%) | 0 (0) | 4 (14) | 0.297 |
| Lower limb injury (AIS>3), n (%) | 0 (0) | 6 (21) | 0.153 |
| 12 (100) | 22 (79) | ||
| Damage control surgery, n (%) | 0 (0) | 10 (36) | 0.019 |
| Intercurrences, n (%) | 2 (22) | 15 (54) | 0.137 |
| Previous other major surgery, n (%) | 0 (0) | 16 (57) | 0.007 |
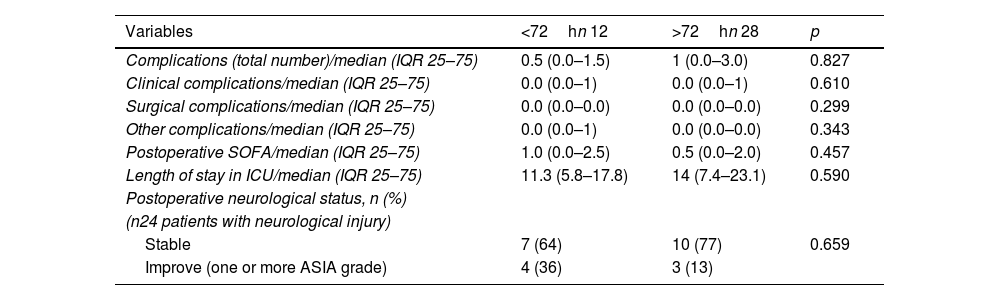
Comparison of dependent variables between groups according to surgical timing.
| Variables | <72hn 12 | >72hn 28 | p |
|---|---|---|---|
| Complications (total number)/median (IQR 25–75) | 0.5 (0.0–1.5) | 1 (0.0–3.0) | 0.827 |
| Clinical complications/median (IQR 25–75) | 0.0 (0.0–1) | 0.0 (0.0–1) | 0.610 |
| Surgical complications/median (IQR 25–75) | 0.0 (0.0–0.0) | 0.0 (0.0–0.0) | 0.299 |
| Other complications/median (IQR 25–75) | 0.0 (0.0–1) | 0.0 (0.0–0.0) | 0.343 |
| Postoperative SOFA/median (IQR 25–75) | 1.0 (0.0–2.5) | 0.5 (0.0–2.0) | 0.457 |
| Length of stay in ICU/median (IQR 25–75) | 11.3 (5.8–17.8) | 14 (7.4–23.1) | 0.590 |
| Postoperative neurological status, n (%) | |||
| (n24 patients with neurological injury) | |||
| Stable | 7 (64) | 10 (77) | 0.659 |
| Improve (one or more ASIA grade) | 4 (36) | 3 (13) | |
The median number of complications was lower in patients operated early (median=0.5/IRQ=0.0–1.5) compared to those surgically treated before 72h (median 1/IRQ=0.0–3.0). However, this association was not statistically significant [p=0.827 (total); p=0.610 (clinical); p=0.299 (surgical); p=0.343 (others)]. The complications recorded were:
- -
Clinical complications (n=26): 10 urinary tract infections (25%), 4 sepsis (10%), 3 pneumonias (7.5%), 3 febrile syndromes without focus (7.5%), 2 atelectasis (5%), 1 ARDS (2.5%), 1 septic shock (2.5%), 1 neurogenic shock (2.5%), 1 deep vein thrombosis (2.5%), 1 liver failure (2.5%).
- -
Surgical complications (n=7): 5 surgical site infections (12.5%), 1 hematoma (2.5%), 1 injury dehiscence (2.5%).
- -
Other complications (n=11): 5 decubitus ulcers 5 (12.5%), 4 empyema (10%), 1 symptomatic hyponatremia (2.5%), 1 infection at the surgical site of non-vertebral surgery (2.5%).
The median postoperative SOFA score was higher in the group of patients operated before 72h from trauma (1.0/IRQ=0.0–2.5) compared to those treated after 72h (0.5/IRQ=0.0–2.0) however the association was not significant (p=0.457).
Neurological recoveryOn arrival, 24 patients (60%) associated neurological symptoms, within this group 22 (92%) had a severe neurological injury (20 ASIA A and 2 ASIA B). Postoperative improvement in 1 or more grades of the ASIA was obtained in 7 patients (29%). Neurological recovery was more frequent in patients operated before 72h, however, this association was not statistically significant (p=0.659).
Variables associated with the surgical time (before or after 72h) in our case-seriesEarly surgery was significantly associated with a lower mean age (p=0.014), lower SOFA score on arrival (p=0.029), higher systolic pressure values (p=0.032) and the presence of preoperative neurological deficit (p=0.012).
Previous damage control surgery (laparotomy or external fixation of the pelvis) and other major surgeries were significantly associated with spine surgery after 72h (p=0.019 and p=0.007 respectively).
The main non-vertebral significant injuries in our sample were: 32 closed chest traumas (80%), 20 severe skull traumas (50%), 11 closed abdomen traumas (27.5%) and 7 pelvic traumas (17.5%). The association between these injuries and the surgical timing was not statistically significant. However, we can highlight that all patients who suffered pelvic fractures were operated after 72h and the p value was close to 0.05 (p=0.08) (Figs. 2 and 3).
Cases of high energy multiple trauma patients with thoracolumbar fractures. Case example 1 (A, B and C): T12-L1 type C fracture associated with cranioencephalic trauma and hemothorax. Case example 2 (D, E, F and G): L1-L2 type C fracture associated with severe upper and lower limbs fractures.
The surgical delay since trauma showed a statistically significant correlation with the magnitude of the preoperative SOFA score (p=0.007/Pearson's correlation coefficient=0.422) (Fig. 4).
DiscussionSeveral authors estimated that early surgery could be associated with shorter hospital stays, shorter ICU stays, shorter days of mechanical ventilation, and lower respiratory morbidity.8–10 However, the evidence that support this conclusion in Latin America are still scarce. Otherwise, higher mortality in patients with unstable thoracolumbar fractures operated before 72h was described in a prospective study.12 We report lower complication rates and ICU stays days in patients surgically treated before 72h although this findings were not statistically significant in our study. Deaths were not reported during our sample follow-up. Additionally, early surgery did not associate differences in the SOFA score on postoperative ICU admission compared to late surgery.
Among the clinical complications in our series, grouped respiratory complications (pneumonia, atelectasis, ARDS) were the most frequent after urinary tract infections. The respiratory complications were independent from the moment of the surgery.20–22
Spine surgical timing making-decision process in trauma patients implies a multidisciplinary assessment with the agreement of clinical and surgical criteria. It could be a difficult process to achieve. Retrospective analysis of our series showed that both groups did not present differences according to the severity of the trauma, however early surgery group patients were significantly younger, with more stable hemodynamic conditions, physiologically less compromised according to the SOFA score and with more frequently associated neurological compromise. Furthermore, surgical delay was positively correlated with the magnitude of the SOFA score on arrival, suggesting that the “decision-making” process in our sample was associated more with the physiological assessment than with the strictly anatomical one. The authors suggest the need for future research to estimate whether the SOFA score could be a prognostic factor in deciding spinal surgery in trauma patients.
Other variables significantly associated with surgical delay in our series were the need for damage control surgery (laparotomy, pelvic fixation) or other major surgical interventions to prioritize the treatment of life-threatening injuries such as unstable pelvic trauma.
Neurological recovery, measured as a secondary outcome, did not show differences between the groups, however we believe that this was related to the small sample size and the predominant severe neurological damage on arrival (22 “ASIA A” and 2 “ASIA B”). Regardless of surgical delay, 29% of cases (7 of 24 patients) improved neurological status by 1 or more degrees on the ASIA after surgery.
This paper included only patients operated through a posterior conventional approach, the benefits of minimally invasive surgery should be considered for future investigations.23
Our study has the weakness of being retrospective with a possible registry bias and the inclusion of a small sample. We believe that it is necessary to continue developing future research with a higher level of evidence. Otherwise, we consider that our paper adds information on the benefits of early surgery in a Latin American Center, in line with what has been reported in other regions of the world.
ConclusionEarly surgery for unstable thoracolumbar fractures was a safe treatment strategy in a trauma center in Latin America. The rate of early postoperative complications did not show significant differences between early and late surgery groups (before and after 72h).
Patients surgically treated before 72h after trauma were younger and presented higher blood pressure values, less physiological damage, and suffered neurological damage more frequently.
Surgical delay was positively correlated with SOFA score on arrival.
Level of evidenceLevel of evidence IV.
Funding sourcesThis research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Conflicts of interestThe authors declare that there is no conflict of interest.