Two out of three wrist fractures seen in an emergency department are displaced but most can be treated conservatively after closed reduction. Patient-reported pain during closed reduction of distal radius fractures varies widely and the best method to decrease the perceived pain has not been well established. The purpose of this study was to assess pain during closed reduction of distal radius fractures after using haematoma block as method of anaesthesia.
Patients and methodsCross-sectional clinical study including all patients who presented an acute fracture of the distal radius requiring closed reduction and immobilisation during a six-month period in two University Hospitals. Demographic data, fracture classification, perceived pain using a visual analogue scale at different times of reduction and complications were registered.
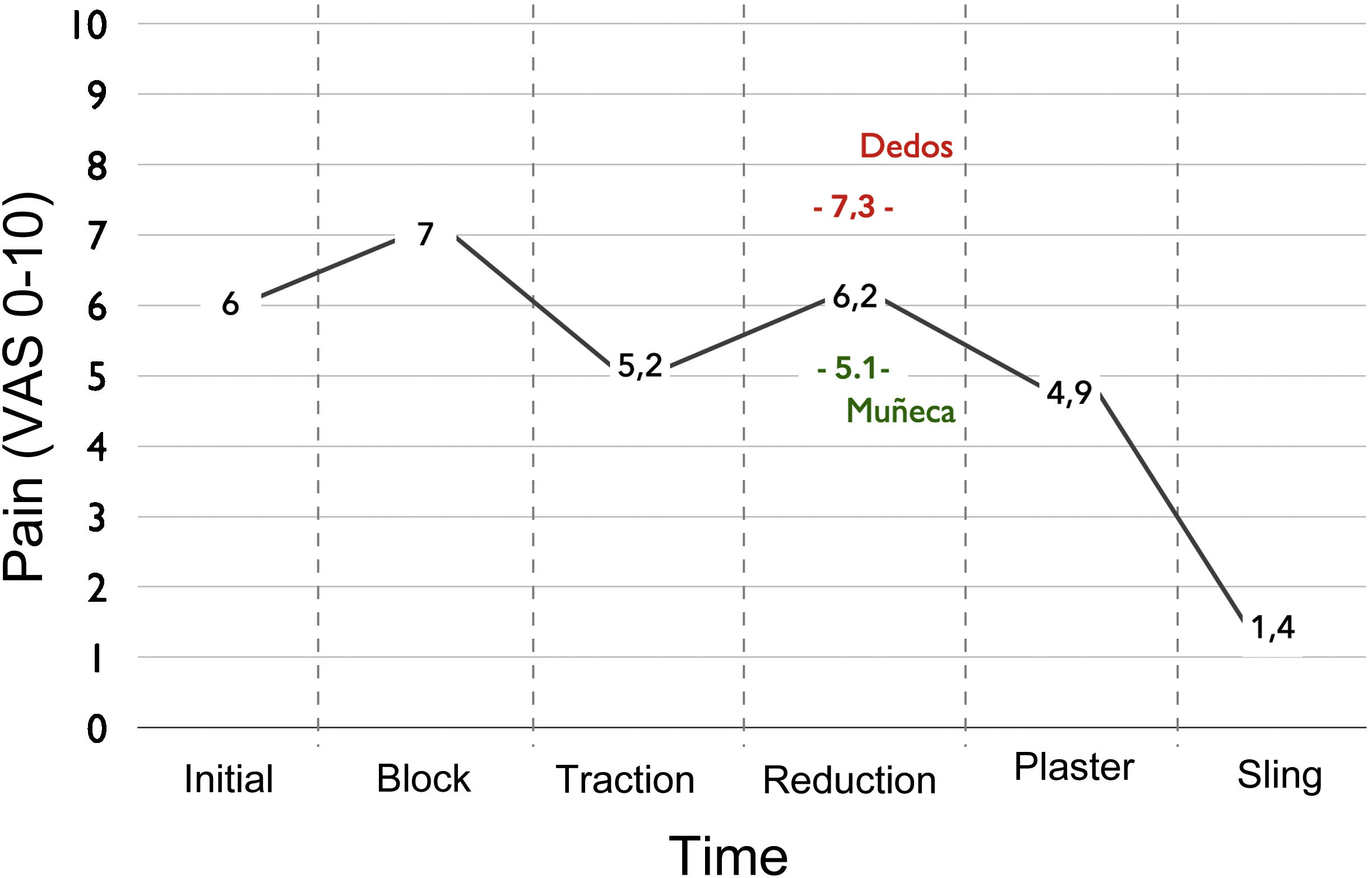
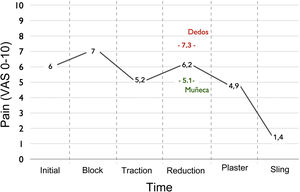
ResultsNinety-four consecutive patients were included. Mean age was 61 years. Mean pain score at initial assessment was 6 points. After the haematoma block, the perceived pain during the reduction manoeuvre improved to 5.1 points at the wrist, but increased to 7.3 points at the fingers. Pain decreased to 4.9 points during cast placement and reached 1.4 point after sling placement. The reported pain was higher in women at all times. There were no significant differences according to the according to the type of fracture. No neurological or skin complications were observed.
ConclusionsHaematoma block is only a mildly effective method to reduce wrist pain during closed reduction of distal radius fractures. This technique slightly decreases the perceived pain in the wrist and does not reduce the pain in the fingers. Other reduction methods or other analgesic techniques may be more effective options.
Level of evidence: Therapeutic study. Cross-sectional study – Level IV.
Dos de cada tres fracturas de muñeca están desplazadas pero la mayoría pueden tratarse de forma conservadora tras una reducción cerrada. El dolor que refieren los pacientes durante la reducción cerrada de estas fracturas es variable y el mejor método para controlarlo no está bien establecido. El objetivo de este estudio fue evaluar el dolor durante la reducción cerrada de fracturas de radio distal tras utilizar el bloqueo del haematoma como método anestésico.
Material y métodoEstudio clínico transversal que incluyó a todos los pacientes que presentaron una fractura aguda de radio distal que requirió reducción cerrada e inmovilización durante un periodo de seis meses en dos Hospitales Universitarios. Se registraron datos demográficos, clasificación de la fractura, dolor percibido mediante una escala visual analógica en diferentes momentos de la reducción y complicaciones.
ResultadosSe incluyeron 94 pacientes consecutivos. La edad media fue de 61 años. La puntuación media del dolor en la evaluación inicial fue de seis puntos. Tras realizar el bloqueo del haematoma, el dolor percibido durante la maniobra de reducción descendió a 5,1 puntos en la muñeca, pero aumentó a 7,3 puntos en los dedos. El dolor disminuyó a 4,9 puntos durante la colocación del yeso y alcanzó 1,4 puntos tras la colocación del cabestrillo. El dolor referido fue mayor en las mujeres en todos los momentos. No hubo diferencias significativas según el tipo de fractura. No se observaron complicaciones neurológicas ni cutáneas.
ConclusionesEl bloqueo del haematoma es un método solo ligeramente efectivo para reducir el dolor en la muñeca durante la reducción cerrada de las fracturas de muñeca. Esta técnica disminuye ligeramente el dolor percibido en la muñeca y no reduce el dolor en los dedos. Otros métodos de reducción u otras técnicas analgésicas pueden ser opciones más efectivas.
Nivel de evidencia: Estudio terapéutico. Estudio transversal – Nivel IV.
Fractures of the distal radius represent 17% of all the fractures treated in emergency departments, with an incidence in Europe in individuals over the age of 50 years that varies from 35 to 105 fractures per 10,000 inhabitants per year.1,2 They occur more frequently in women and in the Scandinavian countries, and these figures are increasing.3
Two of every three wrist fractures seen in an emergency department are displaced, and the majority of them can be treated conservatively after a closed reduction. Although the optimum treatment strategy is still unclear, the majority of recently published papers support conservative treatment in patients over the age of 65 years.4–10,2,11–13
There are many controversies about the conservative treatment of wrist fractures. These include the advisability of reducing the fracture several times, the reduction manoeuvre per se, the type of anaesthesia to be used, the position of the wrist during the time it is immobilised, the type of immobilisation, the material to be used and the duration of immobilisation.13
The pain perceived by the patient during the closed reduction of distal radius fractures does not only cause them discomfort and stress, as it also interferes with the success of the reduction. In spite of this, the pain associated with wrist fractures has not been studied very much,14–17 so that the intensity of the pain at different moments of the reduction and the best way of controlling this pain have yet to be clearly defined.
The intensity of the pain varies widely, from 3 to 10 points on a visual analogue scale (VAS) from 0 to 10 points.13,14 Different methods of anaesthesia and analgesia have been described, and haematoma block is the most widely used by orthopaedic surgeons and traumatologists. This anaesthetic technique has been shown to be safe,15 and according to the available literature it is similar in the efficacy of pain relief to blockage of the brachial plexus.18–23
The aim of this study was to evaluate perceived pain at different moments of the closed reduction of a distal radius fracture after using haematoma block as the anaesthetic technique.
MethodsPopulation and study designAfter approval by the relevant Clinical Research Ethics Committee (CEI/CEIm 2022-116-1), all of the patients diagnosed with displaced fracture of the distal radius seen in the Emergency by the orthopaedic surgery and traumatology team on duty during a six-month period were invited to take part in this cross-sectional clinical study. All of the subjects gave their informed consent before the study.
Inclusion criteria: acute fracture of the distal radius (<3 days evolution) requiring closed reduction and immobilisation. Exclusion criteria: age <16 years or the presence of an open physis in the simple X-ray image, open fractures, pathological fractures, local infection, neurological disease with cognitive deterioration or the presence of osteosynthesis material in the same segment of the affected limb.
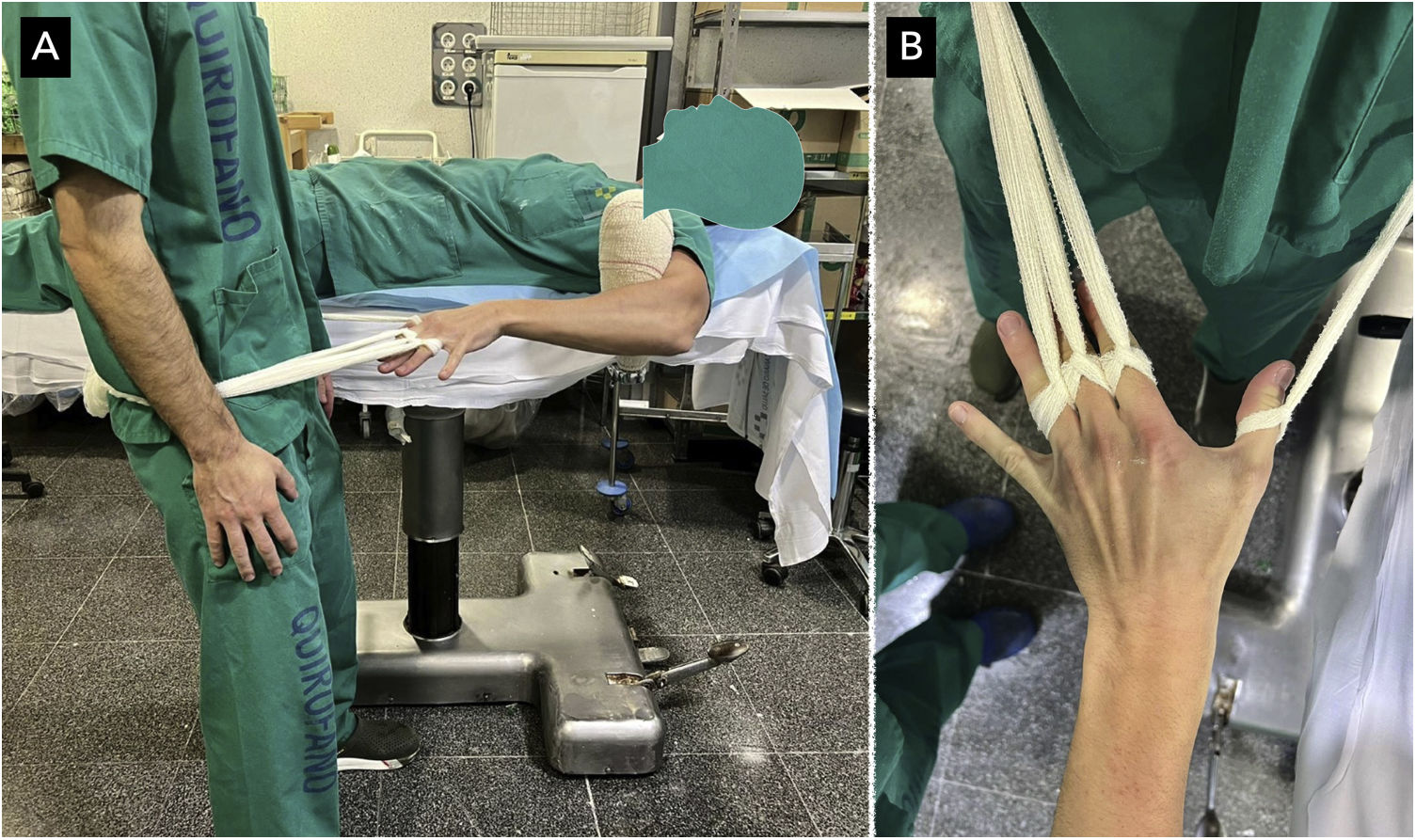
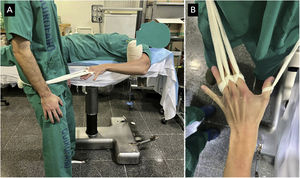
Reduction technique10mL of 2% mepivacaine was used to block the haematoma (mepivacaine 20mg/mL; B. Braun Medical S.A., Barcelona, Spain). The location of the fracture was identified by palpation of the back of the wrist. The back of the wrist was washed using a disinfectant solution and a 21G needle was inserted (SurGuard2, Terumo®, Terumo Medical Corporation, U.S.A.) into the centre of the fracture at a 30° angle from proximal to distal. Correct insertion of the needle was confirmed by aspiration of the fracture haematoma. After 5–10min the reduction was performed using 10cm wide bandage knotted at the base of the thumb, index, middle and ring fingers (Fig. 1). Manual reduction was carried out after maintaining traction during 10min to reduce the muscular tension. A circular closed plaster was put into place after the reduction, followed finally by a sling.
Instruments and measurementsDemographic data were recorded, together with comorbidities and the fracture pattern according to the Arbeitsgemeinshaft für Osteosynsthesefragen (AO) classification.24 The pain score was measured using a line 10cm long, from 0 (no pain) to 10 (the worst pain that I have experienced). Pain was evaluated before the physical examination, during the haematoma block, axial traction, the reduction manoeuvre, placement of the plaster cast, after the placement of the sling and before discharge from hospital (30–45min after the procedure).
According to the clinical practice guide for distal radius fractures by the American Academy of Orthopaedic Surgeons (AAOS) and the American Society for Surgery of the Hand (ASSH),25 fracture reduction is considered to be satisfactory when, after closed reduction, radial shortening is less than 3mm, the angle of the face of the joint of the radius or palmar tilt is less than 10° to the dorsal plane and the displacement or step within the joint is less than 2mm.
Statistical analysisNo minimum clinically important difference (MCID) has been established in the VAS for pain during the reduction of wrist fractures. Previously published studies of other pathologies cite a difference of 1.2 points (95% confidence interval [95% CI]: 0.9–1.5)26 and 1.3 points (95% CI: 1.0–1.6)27 and we used these data as a guide when analysing the results. The fact that the MCID may vary depending on the pathology studied should be taken into account.
All of the data were analysed using Microsoft Excel 2011 (version 14.6.0; 2010 Microsoft Corporation, U.S.A.), StatPlus: MAC (version V6 2016; © AnalystSoft Inc., U.S.A.) and MatLab (version R2019a; © The MathWorks Inc., U.S.A.). A value of P<.05 was considered to be statistically significant.
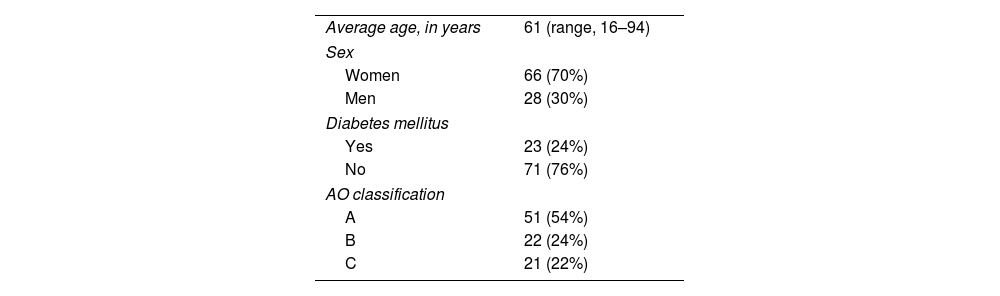
ResultsNinety-four consecutive patients were included. Their demographic data and fracture classifications are shown in Table 1.
The average VAS score for pain before physical examination was six points (range, 1–10; standard deviation [SD] 2.6; 95% CI: 5.8–6.5 points). During the blocking of the haematoma the average pain score amounted to 7.1 points (range, 1–10; SD: 2.4; 95% CI: 6.6–7.5). During axial traction the pain score was 5.2 points (range, 0–10; SD: 3.2; 95% CI: 4.6–5.9). During the reduction manoeuvre the average score on the pain VAS in the wrist was 5.1 points (range, 0–10; SD: 3.4; 95% CI: 4.3–5.9) and 7.3 points in the fingers (range, 2–10; SD: 2.6; 95% CI: 6.7–7.8). During placement of the plaster the pain score fell to 4.9 points (range, 0–10; SD: 3.1; 95% CI: 4.2–5.5). During the placement of the sling the average VAS score for pain was 1.4 points (range, 0–7; SD: 2; 95% CI: 1–1.8) and, lastly, before discharge from hospital the score was 1 point (range, 0–5; SD: 1.3; 95% CI: 0.7–1.3) (Fig. 2).
The men were significantly younger than the women (46 years old vs. 68 years old; P<.05).
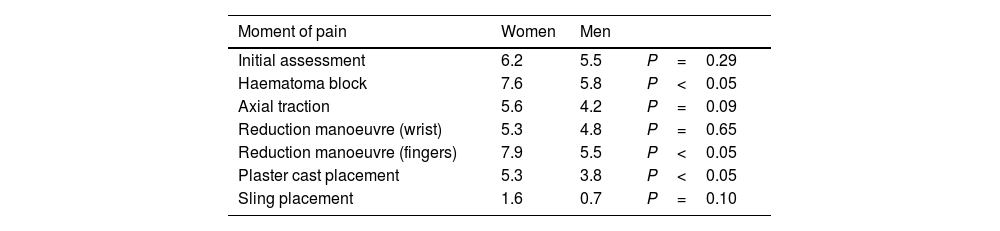
At all times the women described higher levels of pain than the men, and this difference was statistically significant during the blockage of the haematoma, the reduction manoeuvre and the placement of the plaster (Table 2).
Perceived pain according to sex.
| Moment of pain | Women | Men | |
|---|---|---|---|
| Initial assessment | 6.2 | 5.5 | P=0.29 |
| Haematoma block | 7.6 | 5.8 | P<0.05 |
| Axial traction | 5.6 | 4.2 | P=0.09 |
| Reduction manoeuvre (wrist) | 5.3 | 4.8 | P=0.65 |
| Reduction manoeuvre (fingers) | 7.9 | 5.5 | P<0.05 |
| Plaster cast placement | 5.3 | 3.8 | P<0.05 |
| Sling placement | 1.6 | 0.7 | P=0.10 |
No statistically significant differences were found in pain levels according to patient age (P>.05 at all times). The cut-off point was arbitrarily set at 65 years as this is the age most widely used in the literature.
The AO perceived pain in type A fractures averaged 5.6 points. It was 6.5 points in type B fractures and 6.7 points in type C ones. These differences were not statistically significant (P=.14).
Perceived pain at the centre of the fracture improved after the haematoma block, falling from six points in the first assessment to 5.1 points during the reduction manoeuvre (P=0.06).
Perceived pain in the fingers during the reduction manoeuvre exceeded the pain in the wrist (7.3 points vs. 5.1 points). This difference was clinically and statistically significant (P<.05).
The quality of the fracture reduction was analysed in 86 cases. The reduction could not be assessed in the eight remaining cases of the series of 94 consecutive cases due to computer problems which prevented evaluation of the check-up X-ray image, or because clinical data were lacking.
According to the radiological criteria used, fracture reduction was satisfactory in 73 of 86 cases (85%). Perceived pain in the wrist was similar in both groups during the reduction manoeuvre (5.1 in the satisfactory reduction group and 5.8 in the group with unsatisfactory reduction, P=.62). This was also the case for perceived pain in the fingers (7.3 points vs. 6.6 points, P=.36) and pain during placement of the plaster (5.2 points vs. 4.6 points, P=.56). Perceived pain measured after the procedure and placement of the sling was less in those cases in which reduction was satisfactory, although this difference was not statistically significant (1.2 points vs. 2.2 points, P=.09).
There were no neurological, cutaneous or any other type of complications
DiscussionThe data from this cross-sectional clinical study suggest that haematoma block is not a sufficiently effective form of anaesthesia for the closed reduction of distal radius fractures. In our group of patients, this technique reduced perceived pain in the wrist by only 0.9 points (15%) and it did not treat the perceived pain in the fingers.
The average VAS score for pain in our cohort was six points, and this agrees with previously published data, where the score ranges from 3 to 10 points.13,14
The average age of the men was lower than that of the women, and this is probably associated with the cause of the fracture. The main causes in men were sports injuries or work accidents, while in women the main cause was falling at the same height.
Closed reduction and immobilisation in a plaster cast is a useful option when treating the majority of wrist fractures, although the patient suffers a relevant degree of pain during closed reduction and placement of the plaster cast.
Several methods of analgesia have been described, and these may be classified as: (1) intravenous sedation-analgesia (using a combination of opiates and benzodiazepines) and (2) nerve blocks that may in turn be classified as: (a) regional blocks: supraclavicular, axillar, brachial, peripheral at the elbow, peripheral at the wrist and Bier's block and (b) local blocks: haematoma block and periosteal block.28
According to some studies sedation-analgesia is still the most popular method of analgesia for the closed reduction of distal radius fractures.29 Although it offers excellent pain relief, it also causes several side effects, such as nausea and vomiting, respiratory depression, dysphoria and hallucinations. Using this method also consumes resources and time in the Emergency Department, as patients have to be under observation for a long period of time before they can be safely discharged to home.22,29,30
Buier's intravenous block has advantages over sedation-analgesia because it requires less time to be spent in the Emergency Department31 and complications are rare, even though they are possible.32 A disadvantage is that it requires monitoring and medical vigilance during and after the procedure in rooms that have been prepared for it.
Haematoma block is a classic and widely used technique that has been proven to be safe, and it does not increase the risk of infection after any possible surgical treatment.15
In our work the wrist pain perceived by the patient improved by 0.9 points on the VAS (from 6 to 5.1 points) after blocking the haematoma, and the pain continued to improve until the end of the procedure. There was a notable difference between the perceived pain in the wrist and in the fingers during the reduction manoeuvre (5.1 points vs. 7.3 points).
10mL of a 2% mepivacaine solution was used to block the haematoma, which is normal practice in our context. There is controversy in the available literature as to the best local anaesthetic and the ideal volume of the same, as some works suggest that a higher volume is associated with a better analgesic effect, while other studies do not find any differences.33,19 This aspect could be studied in future works.
A 10cm wide bandage knotted at the base of the thumb, index, middle and ring fingers was used to achieve traction during the reduction manoeuvre, as this is the most widely used method in our hospital. The use of other traction techniques, such as manual traction applied by another researcher or the use of finger cots such as those used in wrist arthroscopy may be useful options to reduce perceived pain in the fingers.
The women in our study described feeling more pain than the men at all of the moments when this was evaluated. This finding agrees with the available literature, which suggests that women feel pain more intensely than men.34,35
This study has limitations. Interviewer and responder bias is an intrinsic risk when questioning about pain scores. With the aim of restricting this, the procedure and VAS assessment were performed in a standardised way. Pain perception is a multifactorial process that involves factors, including psychological ones, that were not evaluated in this study. This was a cross-sectional study rather than a comparative one, so that it has no control group. A larger sample would have been useful when analysing subgroups.
To conclude, according to the data obtained in this clinical study, haematoma block is an anaesthetic technique that is only slightly effective in reducing wrist pain during the closed reduction of distal radius fractures. It does not provide perceived pain relief in the fingers. Other reduction methods, other anaesthetic techniques or the modification of the haematoma block could be more effective options to achieve appropriate pain management during the closed reduction of distal radius fractures.
Level of evidenceLevel of evidence IV.
FundingThis study was partially financed by the Fundación del Colegio Oficial de Médicos de Las Palmas (Grant: XXVIII Edición Becas I+E – 2023).
Conflict of interestsThe authors have no conflict of interests to declare.
This work would not have been possible without the input from Dr. Luis Bahillo, Dr. Ariadna Santana, Dr. Esther Romero, Dr. Daniel de Santos, Dr. Bárbara González, Dr. Raquel Izquierdo, Dr. Antonio Ortega-Betancor, Dr. Guillermo Bernal and Dr. Patricia Fleitas. We would like to sincerely thank all of them.