Thanks to improvements in the medical treatment of Parkinson's disease (PD), the life expectancy of these patients has increased, but the overall outcome after total knee arthroplasty (TKA) is controversial. We aim to analyse a series of patients with PD, evaluating their clinical status, functional results, complications and survival rates after TKA.
MethodsWe retrospectively studied 31 patients with PD operated between 2014 and 2020. The mean age was 71 years (SD±5.8). There were 16 female patients. The mean follow-up was 68.2 months (SD±36). We used the knee scoring system (KSS) and the visual analogue scale (VAS) for the functional evaluation. The modified Hoehn and Yahr scale was used to assess the severity of PD. All complications were recorded, and survival curves were performed.
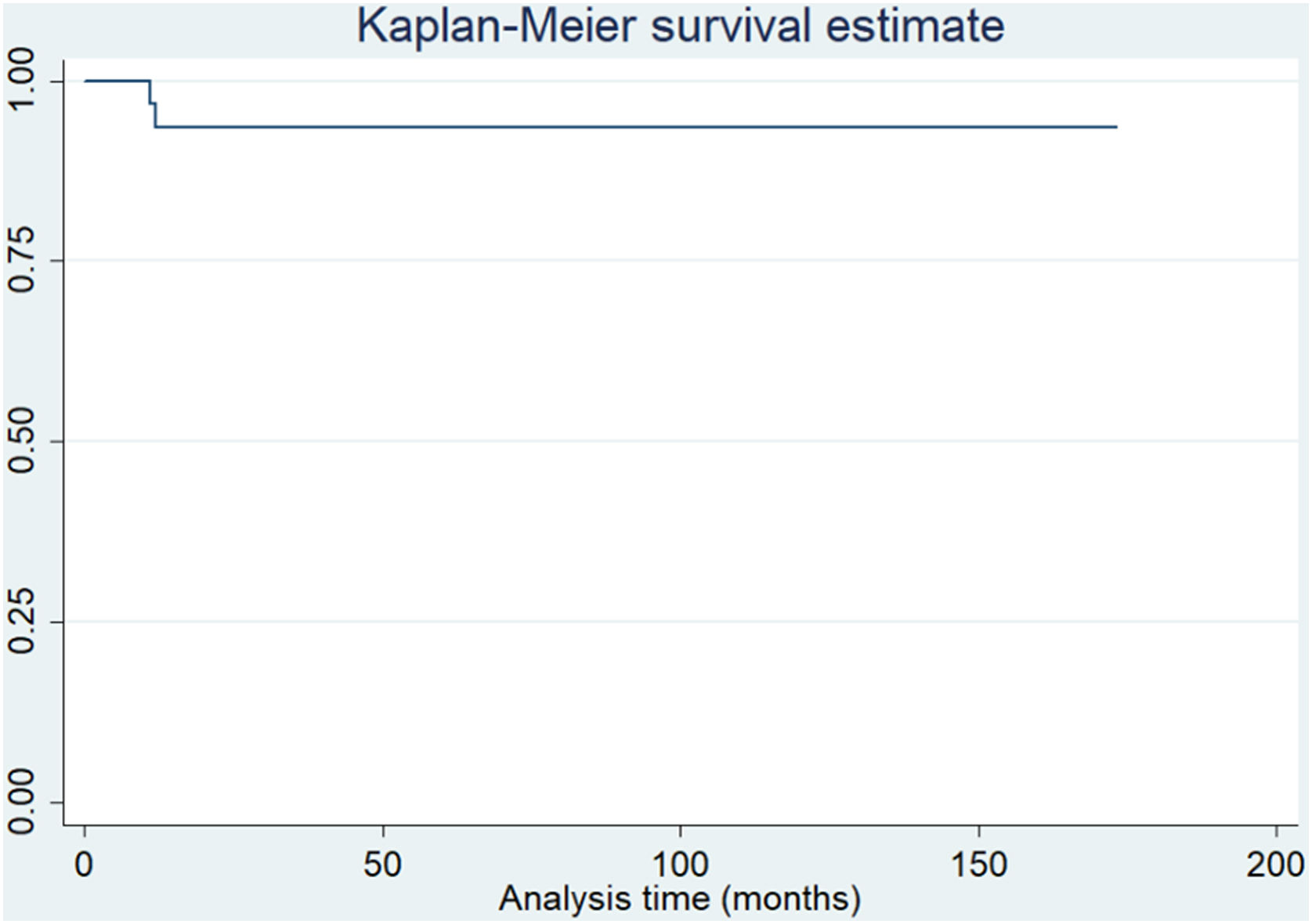
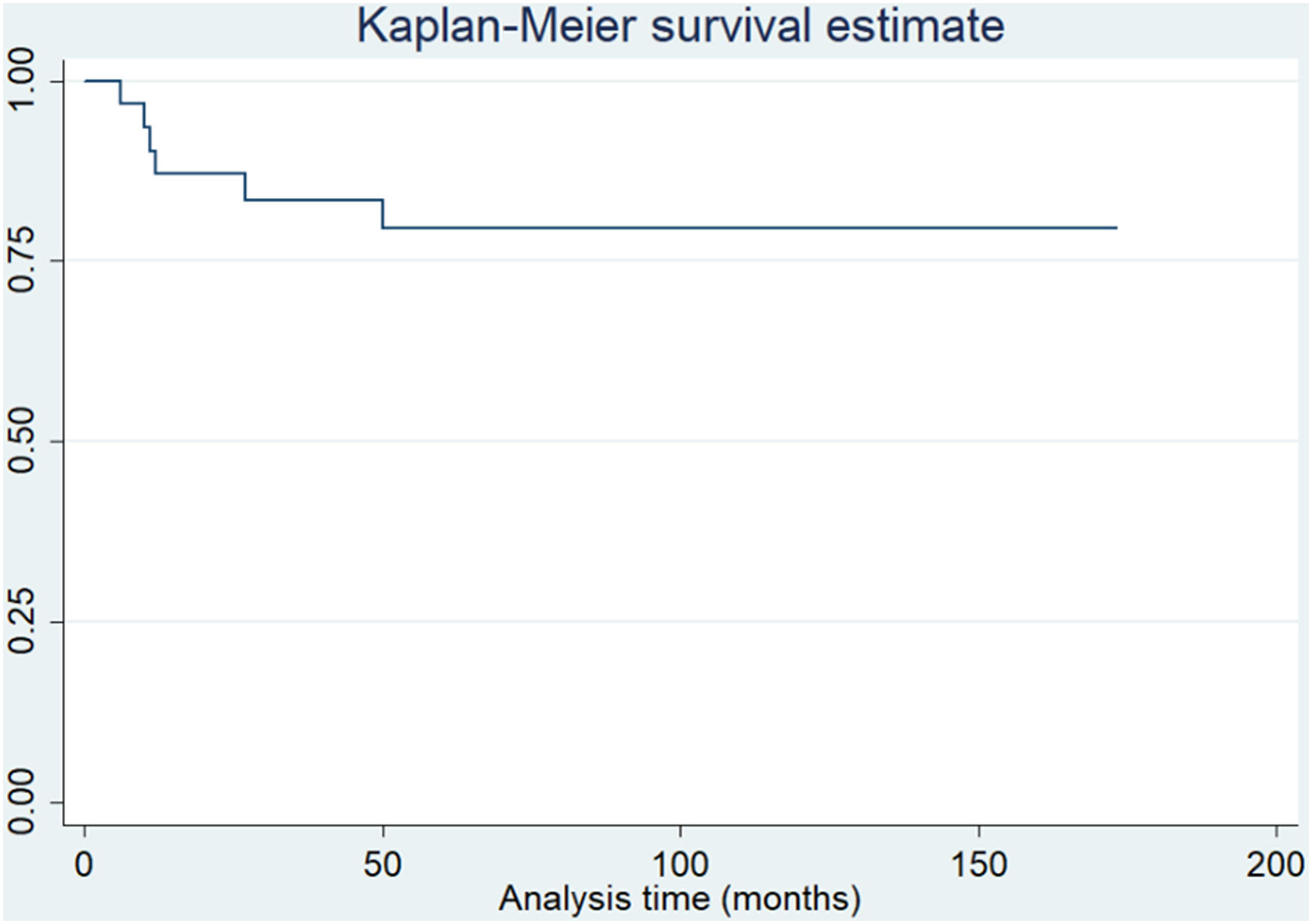
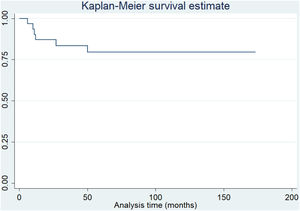
ResultsThe mean postoperative KSS evaluation had an increase of 40 points [35 (SD±15) vs 75 (SD±15) (p<.001)]. The mean postoperative VAS decreased 5 points [8 (SD±2) vs 3 (SD±2) (p<.001)]. Thirteen patients reported being very satisfied, 13 were satisfied, and only 5 were poorly satisfied. Seven patients suffered surgical complications, and 4 patients had recurrent patellar instability. At a mean 68.2 months follow-up, the overall survival rate was 93.5%. When considering the secondary patellar resurfacing as the endpoint, the survival rate was 80.6%.
ConclusionsIn this study, TKA was associated with excellent functional outcomes in patients with PD. At a mean 68.2 months follow-up, TKA had excellent survivorship in the short term, with recurrent patellar instability as the most common complication. Even though these findings confirm the effectiveness of TKA in this population, a thorough clinical evaluation and multidisciplinary approach are needed to decrease the likelihood of complications.
Gracias a las mejoras en el tratamiento médico de la enfermedad de Parkinson (EP), la esperanza de vida de estos pacientes ha aumentado. Los resultados generales después de la artroplastia total de rodilla (ATR) son controvertidos. Nuestro objetivo es analizar una serie de pacientes con EP, evaluando su estado clínico, resultados funcionales, complicaciones y tasas de supervivencia después de la ATR.
MétodosSe estudiaron retrospectivamente 31 pacientes con EP operados entre 2014-2020. La edad media fue de 71 años (DE ± 5,8). Había 16 pacientes mujeres. El seguimiento medio fue de 68,2 meses (DE ± 36). Se utilizó el Knee Scoring System (KSS) y la escala visual analógica (EVA) para la evaluación funcional. Se utilizó la escala modificada de Hoehn y Yahr para evaluar la gravedad de la EP. Se registraron todas las complicaciones y se realizaron curvas de supervivencia.
ResultadosLa evaluación media postoperatoria del KSS tuvo un aumento de 40 puntos (35 [DE ± 15] vs. 75 [DE ± 15] [p < 0,001]). La media de EVA postoperatoria disminuyó cinco puntos (8 [DE ± 2] vs. 3 [DE ± 2] [p < 0,001]). Trece pacientes informaron estar muy satisfechos, 13 estaban satisfechos y solo cinco estaban poco satisfechos. Siete pacientes sufrieron complicaciones quirúrgicas y cuatro tuvieron inestabilidad rotuliana recurrente. Con una media de 68,2 meses de seguimiento, la tasa de supervivencia global fue de 93,5%. Al considerar el rescate rotuliano secundario como punto final, la tasa de supervivencia fue de 80,6%.
ConclusionesEn este estudio, la ATR se asoció con muy buenos resultados funcionales en pacientes con EP. A una media de 68,2 meses de seguimiento, la ATR tuvo una buena supervivencia a corto plazo, siendo la inestabilidad rotuliana recurrente la complicación más frecuente. Aunque estos hallazgos confirman la efectividad de la ATR en esta población, se necesita una evaluación clínica exhaustiva y un enfoque multidisciplinario para disminuir la probabilidad de complicaciones.
Parkinson's disease (PD) is a chronic, progressive, neurodegenerative disorder with an incidence of approximately 31 per 100,000 inhabitants in Argentina and 4 million people worldwide.1 The prevalence increases with age, with values around 1% in people over 65 and 3.1% between 75 and 84 years of age.2 The most common clinical picture includes tremor, rigidity, bradykinesia and unsteadiness with loss of postural reflexes. Consequently, gait is markedly impaired at the onset of ambulation, slow execution of movements, excessively short step length and forward displacement of the centre of gravity. Due to these changes, these patients are at increased risk of falls during ambulation.3,4
Due to improvements in the medical management of PD, the life expectancy of this population has increased and an increased incidence of osteoarthrosis has been reported in these patients.5 Total knee arthroplasty (TKA) poses a real challenge in patients with PD as an underlying disease, and musculoskeletal imbalance may negatively affect postoperative outcomes.6 Although the current literature is sparse, most studies have reported good functional outcomes and a high complication rate after TKA in this population.6 This study aimed to analyse a consecutive series of patients with PD, evaluating their pre- and postoperative clinical status, functional outcomes, complications and survival rate after TKA.
MethodsThis study was conducted in accordance with the principles of the 1964 Declaration of Helsinki and was approved by the Institutional Research Ethics Board (CEPI no. 6049). Informed consent was obtained from all participants, and consent to publish was obtained from patients whose radiographs appear in this publication.
After obtaining Institutional Review Board approval, we retrospectively reviewed electronic medical records of patients treated by 3 arthroplasty surgeons at a single institution. A total pooled record was used to identify 31 patients with PD who underwent cemented TKA between 2014 and 2020 with a minimum follow-up of 3 years. All patients with PD under follow-up by the Neurology service, older than 60 years with symptomatic knee and need for TKA were included. All cases with inadequate radiographs, previous TKA, history of periprosthetic joint infections and follow-up<3 years were excluded. At the end of the review, no patients were lost to follow-up, and all cases were included in the analysis.
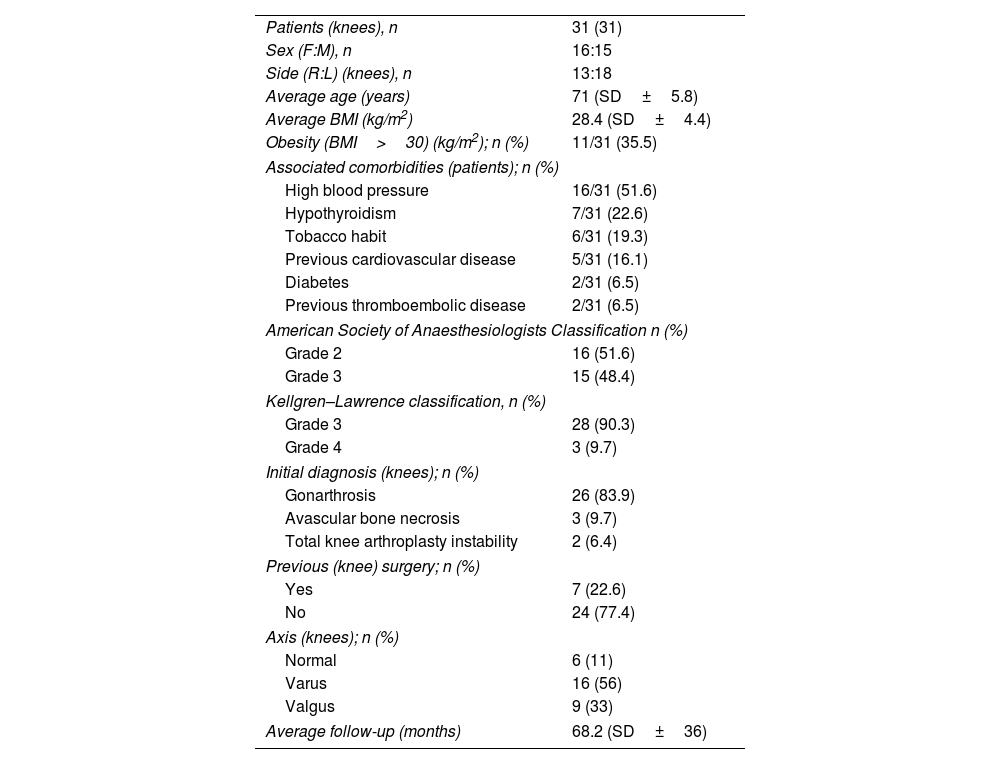
All data were retrieved from the institution's prospectively collected electronic database. Two investigators (FDD and AGM) who were not involved in the original patient care reviewed these data. Demographic variables included age, date of birth, sex, height, weight, body mass index, side, diagnosis, type of deformity, American Society of Anaesthesiologists classification,7 Kellgren–Lawrence classification,8 length of hospital stay and follow-up. The mean age of the series was 71 years (standard deviation [SD]±5.8). There were 16 (51.6%) female patients. Eleven patients (35.5%) were obese, defined by a body mass index≥30kg/m2. Seven (22.6%) patients had previously undergone surgery at our institution. All of them had undergone simple arthroscopies due to meniscal lesions. The mean follow-up was 68.2 months (SD±36). Demographic characteristics are shown in Table 1.
Demographic characteristics of the series.
| Patients (knees), n | 31 (31) |
| Sex (F:M), n | 16:15 |
| Side (R:L) (knees), n | 13:18 |
| Average age (years) | 71 (SD±5.8) |
| Average BMI (kg/m2) | 28.4 (SD±4.4) |
| Obesity (BMI>30) (kg/m2); n (%) | 11/31 (35.5) |
| Associated comorbidities (patients); n (%) | |
| High blood pressure | 16/31 (51.6) |
| Hypothyroidism | 7/31 (22.6) |
| Tobacco habit | 6/31 (19.3) |
| Previous cardiovascular disease | 5/31 (16.1) |
| Diabetes | 2/31 (6.5) |
| Previous thromboembolic disease | 2/31 (6.5) |
| American Society of Anaesthesiologists Classification n (%) | |
| Grade 2 | 16 (51.6) |
| Grade 3 | 15 (48.4) |
| Kellgren–Lawrence classification, n (%) | |
| Grade 3 | 28 (90.3) |
| Grade 4 | 3 (9.7) |
| Initial diagnosis (knees); n (%) | |
| Gonarthrosis | 26 (83.9) |
| Avascular bone necrosis | 3 (9.7) |
| Total knee arthroplasty instability | 2 (6.4) |
| Previous (knee) surgery; n (%) | |
| Yes | 7 (22.6) |
| No | 24 (77.4) |
| Axis (knees); n (%) | |
| Normal | 6 (11) |
| Varus | 16 (56) |
| Valgus | 9 (33) |
| Average follow-up (months) | 68.2 (SD±36) |
BMI: body mass index; F: female; L: left; M: male; R: right; SD: standard deviation.
All patients received combined replacement anaesthesia of motor block and spinal anaesthesia prior to the surgical procedure performed by the same group of anaesthesiologists. All patients received the same preoperative antibiotic therapy with 3 doses of intravenous cefazolin (1g/8h).
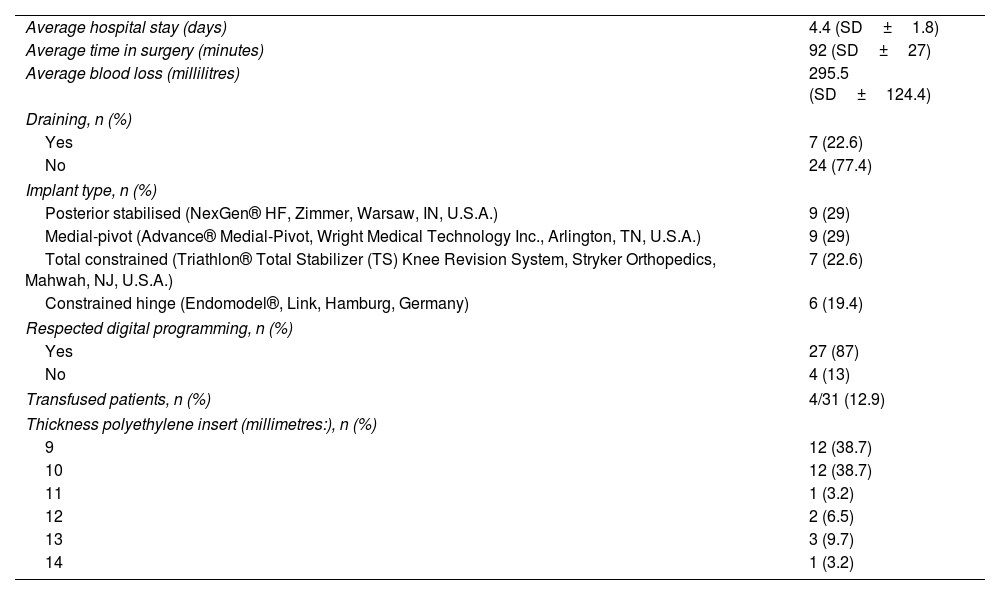
Three knee surgeons performed all surgeries through a medial parapatellar approach. The surgical technique followed the principles of gap balancing or major resection according to the surgeon's preference. The distal femoral cut was performed using an intramedullary femoral guide for a distal femoral valgus resection of 6° and a neutral tibial cut. Prostheses with different degrees of constriction (posterior stabilised, medial pivot, total stabilised and hinge) were used according to intraoperative stability (Table 2).
Postoperative characteristics and results.
| Average hospital stay (days) | 4.4 (SD±1.8) |
| Average time in surgery (minutes) | 92 (SD±27) |
| Average blood loss (millilitres) | 295.5 (SD±124.4) |
| Draining, n (%) | |
| Yes | 7 (22.6) |
| No | 24 (77.4) |
| Implant type, n (%) | |
| Posterior stabilised (NexGen® HF, Zimmer, Warsaw, IN, U.S.A.) | 9 (29) |
| Medial-pivot (Advance® Medial-Pivot, Wright Medical Technology Inc., Arlington, TN, U.S.A.) | 9 (29) |
| Total constrained (Triathlon® Total Stabilizer (TS) Knee Revision System, Stryker Orthopedics, Mahwah, NJ, U.S.A.) | 7 (22.6) |
| Constrained hinge (Endomodel®, Link, Hamburg, Germany) | 6 (19.4) |
| Respected digital programming, n (%) | |
| Yes | 27 (87) |
| No | 4 (13) |
| Transfused patients, n (%) | 4/31 (12.9) |
| Thickness polyethylene insert (millimetres:), n (%) | |
| 9 | 12 (38.7) |
| 10 | 12 (38.7) |
| 11 | 1 (3.2) |
| 12 | 2 (6.5) |
| 13 | 3 (9.7) |
| 14 | 1 (3.2) |
SD: standard deviation.
Routine thromboembolic prophylaxis was indicated for 15 days in all patients according to their history and comorbidities. It consisted of 40mg enoxaparin/day subcutaneously in patients at high clinical risk and 325mg aspirin/day orally in patients at low clinical risk. The postoperative rehabilitation protocol included early mobilisation after surgery, ambulation with a walker for 15 days and full weight bearing. Rehabilitation was similar in all patients, with a standard protocol focusing on early prevention of flexion contractures. For patients with early flexion contractures and unresponsive to terminal extension, splints were used in addition to manual treatment to avoid a definitive semi-flexed posture. Subsequently, patients were encouraged to progressively return to normal daily activities as tolerated with a cane for at least one month depending on their clinical evolution and follow-up radiographic findings.
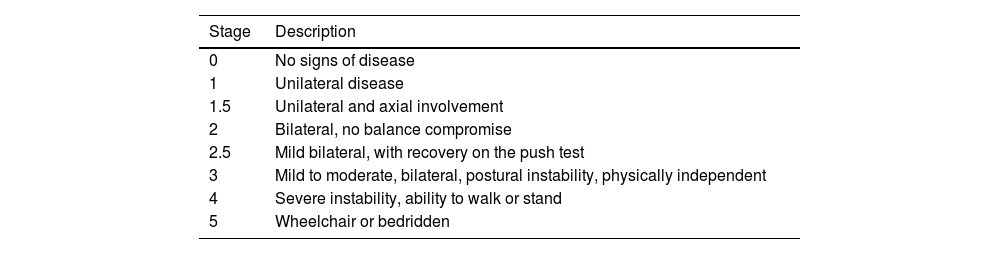
Functional outcomes were assessed using the knee society score (KSS),9 pain assessment using the visual analogue scale (VAS) and subjective patient satisfaction according to the 5-point Likert scale (poor, moderate, good, very good and excellent). Finally, the modified Hoehn and Yahr scale10 (Table 3) was used to determine the severity and progression of PD. All patients were graded before surgery and during each follow-up visit. All patients were under the follow-up of the neurologist department and were taking appropriate medication for their condition.
Modified Hoehn and Yahr scale.
| Stage | Description |
|---|---|
| 0 | No signs of disease |
| 1 | Unilateral disease |
| 1.5 | Unilateral and axial involvement |
| 2 | Bilateral, no balance compromise |
| 2.5 | Mild bilateral, with recovery on the push test |
| 3 | Mild to moderate, bilateral, postural instability, physically independent |
| 4 | Severe instability, ability to walk or stand |
| 5 | Wheelchair or bedridden |
Anteroposterior, lateral and axial radiographs of the knee were obtained immediately after surgery, at 15 days, 45 days, 12 months and then annually. Alignment was assessed by hip-to-ankle radiographs to confirm the preoperative anatomical and mechanical axis. For this study, all patients were contacted for clinical and radiological evaluation. Two authors reviewed the radiographs (FDD and AGM) to determine the presence of any signs of loosening, subsidence or progressive radiolucency, comparing the immediate postoperative radiographs with those at the last follow-up.
All complications were recorded and divided according to the time of occurrence. All failures and subsequent revision surgeries were recorded between the index procedure and the last follow-up in each patient. Progressive radiolucent lines greater than 2mm or subsidence, associated with clinical symptoms of loosening, such as baseline pain, thigh pain and tibial pain, were used to define aseptic loosening.11
We define an aseptic implant failure as any time revision surgery was performed for non-infectious causes, including evidence of loosening, instability or periprosthetic periprotésicas.12 According to the standardised definitions by the Musculoskeletal Infection Society as revised at the International Consensus Meeting, we considered septic failure as any case requiring revision surgery due to surgical site infection. We assessed with routine blood tests, including erythrocyte sedimentation rate and C-reactive protein, along with joint aspiration for cell count and culture.
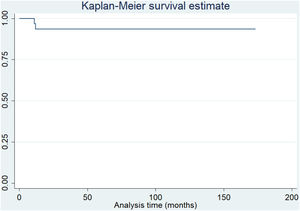
Statistical analysisContinuous variables were expressed as means and SD. Categorical variables were reported as frequencies and percentages. Continuous variables were compared using the independent samples t-test, where data are normally distributed, and the Mann–Whitney U-test when otherwise. Categorical variables were compared using Chi-square and Fisher's exact tests. Kaplan–Meier survival curves were estimated, defining failure as the need for any additional femoral or tibial revision surgery with implant removal, regardless of the reason. Variables were considered statistically significant at p<.05. Data analysis was performed using IBM SPSS Statistics (IBM Corp., Armonk, NY, USA).
ResultsThe mean operative time was 92min (SD±27) and the mean hospital stay was 4.4 days (SD±1.8). Mean blood loss was 295.5ml (SD±124.4), and only 4 patients required blood transfusion after surgery. Postoperative details are shown in Table 2.
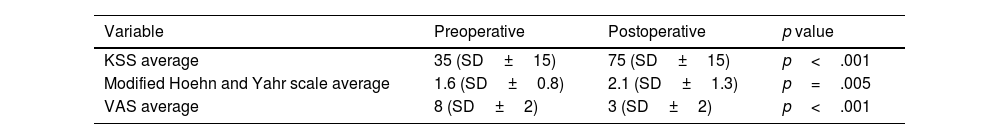
There was a significant improvement in KSS assessment when comparing preoperative and postoperative values (KSS 35 [SD±15] vs. KSS 75 [SD±15] points [p<0.001]). Mean VAS improved from 8 points (DE±2) preoperatively to 3 points (SD±2) postoperatively (p<.001). Regarding subjective patient satisfaction, 13 patients reported being very satisfied, 13 were satisfied and only 5 were dissatisfied. The mean value of the modified Hoehn and Yahr scale progressed from 1.6 (SD±0.8) points preoperatively to 2.1 (SD±1.3) points at the end of follow-up (p=.005). Although 8 patients (26%) had a progression in disease severity, none of them required the use of a wheelchair for mobility. The functional assessment is summarised in Table 4.
Radiographic evaluation with hip-to-ankle radiographs revealed overall postoperative neutral mechanical alignment in all patients. No progressive radiolucent lines were detected around any of the components at follow-up. At the last follow-up, there was no evidence of periprosthetic osteolysis, subsidence or aseptic loosening around the femoral or tibial components.
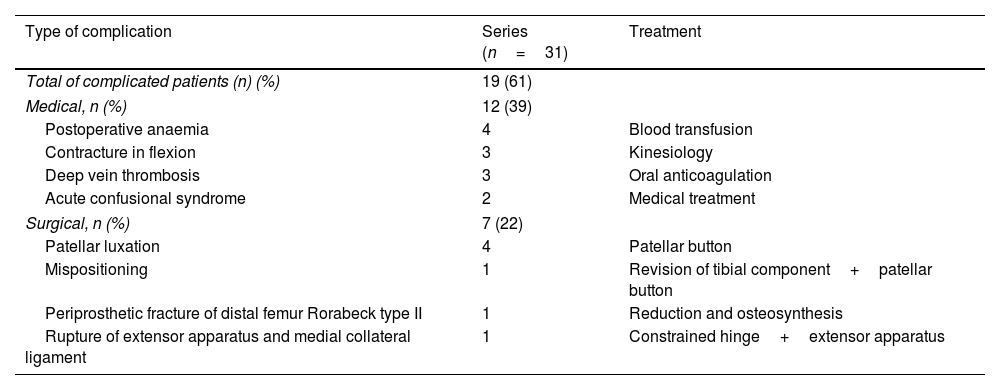
Nineteen (61%) patients experienced medical (n=12) or surgical (n=7) complications during follow-up. There were no intraoperative complications in any of the surgical procedures. Regarding infection outcomes, no surgical site infections were reported at the last follow-up.
During hospital stay, only 4 patients suffered from symptomatic postoperative anaemia. They had haemoglobin<8mg/dl, haematocrit<20% and required blood transfusion. In addition, 2 patients suffered acute confusional syndrome requiring medical treatment and extended hospital stay.
Three patients developed deep vein thrombosis during the first 6 weeks, successfully treated with oral anticoagulation. Finally, 3 TKA developed flexion contracture successfully treated with physiotherapy without considering revision surgery.
Seven patients suffered postoperative complications requiring surgical resolution. Four patients had persistent anterior knee pain due to hyperpressure and one patient had patellar instability following a fall with recurrent subluxation. They were initially treated conservatively, but eventually underwent reoperation in a median time of 23 months (SD±20). All underwent secondary patellar salvage with good results and no recurrence at last follow-up. One patient sustained a periprosthetic Rorabeck type II periprosthetic fracture of the distal femur due to low energy trauma 18 months after index surgery. The fracture was successfully treated with open reduction and internal fixation using a locking compression plate without further complications at the end of follow-up.
Regarding implant failures, the patient presented with pain and instability of the TKA during the first postoperative year. No signs of loosening were evident on serial radiographs, and computed tomography showed excessive tibial component intrarrowing. After 12 months of follow-up, tibial component revision using a constrained implant (Triathlon® Total Stabilizer [TS] Knee Revision System, Stryker Orthopedics, Mahwah, NJ, USA) and patellar rejuvenation was performed with good results and no recurrence at last follow-up. Finally, one patient suffered a disruption of the extensor mechanism and a complete medial collateral ligament injury with severe varus/valgus instability after low-energy trauma at 11 months follow-up. Treatment included one-stage revision surgery using a hinged prosthesis (Endo-Model®, Link, Hamburg, Germany) with additional repair of the extensor mechanism with a mesh. Detailed complications and treatment are shown in Table 5.
Complications recorded in the series.
| Type of complication | Series (n=31) | Treatment |
|---|---|---|
| Total of complicated patients (n) (%) | 19 (61) | |
| Medical, n (%) | 12 (39) | |
| Postoperative anaemia | 4 | Blood transfusion |
| Contracture in flexion | 3 | Kinesiology |
| Deep vein thrombosis | 3 | Oral anticoagulation |
| Acute confusional syndrome | 2 | Medical treatment |
| Surgical, n (%) | 7 (22) | |
| Patellar luxation | 4 | Patellar button |
| Mispositioning | 1 | Revision of tibial component+patellar button |
| Periprosthetic fracture of distal femur Rorabeck type II | 1 | Reduction and osteosynthesis |
| Rupture of extensor apparatus and medial collateral ligament | 1 | Constrained hinge+extensor apparatus |
At a median follow-up time of 68.2 months (SD±36), taking revision surgery for any reason as an endpoint, survival was 93.5% (Fig. 1). Furthermore, considering secondary patellar salvage as the end point, survival was 80.6% (Fig. 2).
This study demonstrated that TKA was associated with very good functional outcomes in patients with PD. At a median follow-up of 68.2 months, TKA had a good survival rate, with recurrent patellar instability being the most frequent complication in this cohort of patients. Several studies13–19 reported similar results in PD patients treated with TKA, with survival rates ranging from 87% to 100% at mid-term follow-up. In addition, a recent systematic review20 demonstrated excellent functional outcomes in patients with neurological disorders, but highlighted the significant risk of complications. In this regard, careful preoperative planning, perioperative patient care and appropriate implant selection would mitigate the likelihood of complications.
In 1985, Oni y Mackenney21 reported one of the first case series analysing the results of TKA in patients with PD. The authors reported very poor results and strongly recommended contraindication of TKA in this group of patients. Our study demonstrated significant functional improvement when comparing preoperative and postoperative KSS (35 [SD±15] vs. 75 [DE±15] [p<.001]). In addition, we report similar results with respect to pain assessment [preoperative VAS 8 (SD±2) vs. postoperative VAS 3 (SD±2) (p<.001)]. There is some controversy regarding the functional outcomes reported in the current literature when analysing TKA in PD. Several studies have shown promising results,13,18,19,22 but others reported poor results.23,24 It is essential to mention that most of the poor results have been reported in studies including a control group of patients without PD. Despite this, Goh et al.24 performed an additional assessment of patient satisfaction and reported no significant difference in satisfaction rate between the PD group (80.4%) and the control group (85.5%) (p=.476). Similarly, in our study, we identified 26 patients (84%) who were satisfied or very satisfied at the end of follow-up.
PD has a chronic and progressive course, and its progression over time directly affects the patient's motor skills. Although the modified Hoehn and Yahr scale reported a significant progression of PD severity in 26% of patients at the last follow-up (preoperative 1.6 [SD±.8] vs. postoperative 2.1 [SD±1.3], [p=.005]), all patients were able to ambulate and perform daily activities without using a wheelchair or being bedridden unless assisted. We believe that this additional functional assessment is relevant to the indication and prognosis of TKA, as patients and surgeons continue to believe that increased stiffness, bradykinesia and risk of falls could pose a threat to the success of TKA. The relationship of TKA survival and the Hoehn and Yahr scale was previously published by Rong et al. in 2019 and by Montiel et al. in 202119,22 with rates similar to those proposed in this paper.
Most studies analysing the reasons for failure or reinterventions after TKA in patients with PD have concluded that flexion contractures and extensor mechanism complications are the most frequent causes.17–24 In our series, we presented 3 patients (9.7%) with flexion contractures in the early postoperative period. All of them underwent intensive physiotherapy with satisfactory results and without the need for further surgery. On the other hand, patellofemoral pathology, including anterior pain and instability, was the most common reason for revision surgery in this cohort of patients, and no cases of aseptic or septic loosening were reported. For this reason, despite the low level of evidence in our study, we suggest that the surgeon consider routine patella replacement and have implants of greater constriction in PD patients undergoing TKA to reduce complications. Regarding failures, Schroer et al.25 analysed data from 6 joint arthroplasty centres to determine the mechanism of failure and time to failure. Aseptic loosening was the predominant cause of failure (31.2%), followed by instability (18.7%) at a mean time of 5.9 years. Interestingly, 35.3% of all revisions occurred less than 2 years after primary TKA, and 60.2% in the first 5 years.
In our study, recurrent anterior knee pain was the main failure mechanism in our series. Similarly, complications requiring surgical treatment occurred at a median time of 23 months (SD±20). Although our study has a short-term follow-up (68.2 months [SD±36]), assuming that early failures are mainly surgeon-dependent and in accordance with the above, we believe this is a reasonable period to predict the long-term behaviour of TKA in these patients.
Our study was not without limitations. First, its retrospective nature correlated with the unique biases of the study design and the lack of a control group. The sample size of the series resulted in a small number of included cases, which restricted the production of more precise statistical analyses.
However, as far as we are concerned, it is one of the few studies that includes the modified Hoehn and Yahr scale for preoperative and postoperative assessment of all patients.19–22 Secondly, our survival rates should be considered as best-case estimates. Because there was a short-term follow-up period, we expect that some of these patients may still undergo revision arthroplasty for any reason at longer follow-up. Third, our data did not include sufficient complete information on demographics and frailty-specific comorbidities or perioperative factors that would contribute to the development of complications. Therefore, complication outcomes should also be considered as best-case estimates. Finally, the gold standard in the analysis of initial implant stability is radiostereometric analysis.26 Another reliable option to assess implant migration is EBRA-FCA,27 which can also measure stem subsidence without the need for tantalum markers using standard radiographs. Unfortunately, we were unable to perform this type of assessment due to lack of resources at our centre at the time of this study.
ConclusionsIn this study, TKA was associated with good functional outcomes in patients with PD. At a median follow-up of 68.2 months, TKA had good short-term survival, with recurrent patellar instability being the most frequent complication. Although these findings confirm the effectiveness of TKA in this population, a thorough clinical evaluation and a multidisciplinary approach are needed to decrease the likelihood of complications.
Level of evidenceLevel of evidence iv.
Authors' contributionsAll authors contributed to the study conception and design, and read and approved the final manuscript.
Conceptualisation: Lisandro Carbo; Data curation: Fernando Díaz-Dilernia, Agustin García-Mansilla; Methodology: Fernando Díaz Dilernia; Analysis and formal research: Fernando Díaz Dilernia, Agustín García-Mansilla; Writing – preparation of the original draft: Fernando Díaz Dilernia, Agustín García-Mansilla; Script – review and editing: Fernando Díaz Dilernia, Agustín García-Mansilla; Resources: Tomás Nicolino, Julián Costantini, Lisandro Carbo; Project administration: Tomas Nicolino, Julián Costantini; Management: Lisandro Carbo.
Conflict of interestsThe authors have no conflict of interests to declare.
FundingThe authors declare that they have received no funding for the conduct of the present research, the preparation of the article, or its publication.