The prevalence of adult spinal deformity has been increasing exponentially over time. Surgery has been credited with good radiological and clinical results. The incidence of complications is high. MIS techniques provide good results with fewer complications. This is a retrospective study of 25 patients with an adult spinal deformity treated by MIS surgery, with a minimum follow-up of 6 months. Radiological improvement was SVA from 5 to 2cm, coronal Cobb angle from 31° to 6°, and lumbar lordosis from 18° to 38°. All of these parameters remained stable over time. We also present the complications that appeared in 4 patients (16%). Only one patient needed reoperation. We describe the technique used and review the references on the subject. We conclude that the MIS technique for treating adult spinal deformity has comparable results to those of the conventional techniques but with fewer complications.
La deformidad del adulto es una entidad cuya prevalencia aumenta de forma exponencial con el paso del tiempo. La cirugía ha demostrado ser un tratamiento eficaz con buenos resultados tanto clínicos como radiológicos. La elevada incidencia de complicaciones que se presentan con la cirugía convencional ha hecho posible la aparición de técnicas MIS con resultados muy prometedores desde el punto de vista clínico y radiológico. El presente estudio revisa de forma retrospectiva 25 pacientes con una deformidad del adulto tratados con técnicas MIS y con un seguimiento mínimo de 6 meses. La mejoría radiológica fue: SVA de 5 a 2cm, ángulo de Cobb coronal de 31° a 6° y la lordosis lumbar pasó de 18° a 38°. Todos estos parámetros se mantuvieron estables en el tiempo. Se presentan también las complicaciones que fueron en cuatro pacientes (16%), siendo necesaria la reintervención solo en un caso. Se realiza una descripción de la técnica utilizada y se lleva a cabo una revisión de la bibliografía sobre el tema, concluyendo que la técnica MIS en el tratamiento de la deformidad del adulto presenta unos resultados comparables a las técnicas convencionales pero con una menor tasa de complicaciones.
Adult spinal deformity (ASD) is defined as a deformity where the coronal plane reaches more than 20 Cobb degrees in a skeletally mature patient.1 The incidence of this type of deformity increases with the age of the population. The clear ageing tendency of the population and projections for the forthcoming years indicate that the prevalence of this problem is increasing exponentially. If we also bear in mind that the incidence of the deformity is twice as high in women as in men, and that women live longer than men, we face a real health problem and one that we are already witnessing.2
Several papers3–5 demonstrate that surgical correction of the deformity, especially in the sagittal plane, improves the quality of life of patients with ASD. However, the high rate of complications after surgical treatment (up to 100% risk of suffering a complication)6,7 make it the final option to be considered. The emergence of new surgical techniques that we term minimally invasive because there is a less aggressive approach to these types of disorder has considerably reduced the rate of complications maintaining the principal objective of surgery which is to restore the balance of the spine and decompress the neurological elements that have been compromised by the deformity.
We highlight 3 MIS procedures that can be used in treating adult spinal deformity:
- •
XLIF alone.
- •
cMIS: XLIF associated with posterior segmental instrumentation.
- •
hMIS: combination of the MIS technique and open technique. According to our criteria, we perform this technique when the patient has: thoracolumbar kyphosis (T11-L2) greater than 20 degrees, thoracic scoliosis greater than 40 degrees or thoracic kyphosis greater than 60 degrees. In these cases we associate MIS with conventional open surgery in the thoracic region. A typical construction would be: 4 lateral cages L1–L4, TLIF MIS L5-S1, MIS AIS2 screws, percutaneous screws T11-S1, and open surgery with facetectomy and open arthrodesis of T5–T10.
Whatever the MIS technique used, the rate of complications is considerably lower than that of open surgery.8
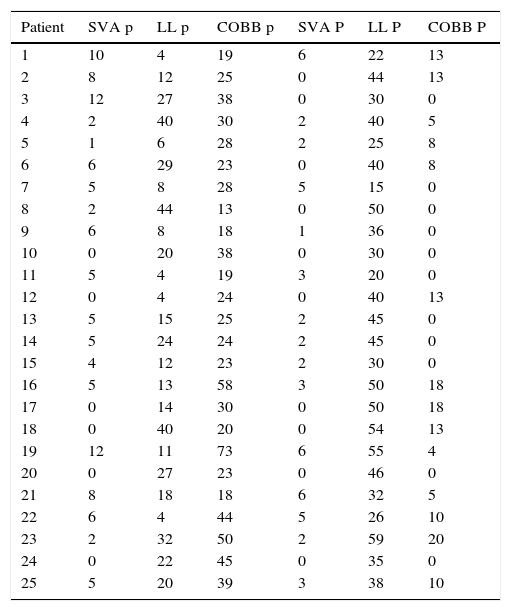
Material and methodPatients operated for adult spinal deformity were reviewed retrospectively from May 2012 to September 2016. Minimum follow-up was 6 months. Coronal deformity and the pre and postoperative pelvic parameters were recorded (Table 1).
Pre and postoperative radiological parameters.
| Patient | SVA p | LL p | COBB p | SVA P | LL P | COBB P |
|---|---|---|---|---|---|---|
| 1 | 10 | 4 | 19 | 6 | 22 | 13 |
| 2 | 8 | 12 | 25 | 0 | 44 | 13 |
| 3 | 12 | 27 | 38 | 0 | 30 | 0 |
| 4 | 2 | 40 | 30 | 2 | 40 | 5 |
| 5 | 1 | 6 | 28 | 2 | 25 | 8 |
| 6 | 6 | 29 | 23 | 0 | 40 | 8 |
| 7 | 5 | 8 | 28 | 5 | 15 | 0 |
| 8 | 2 | 44 | 13 | 0 | 50 | 0 |
| 9 | 6 | 8 | 18 | 1 | 36 | 0 |
| 10 | 0 | 20 | 38 | 0 | 30 | 0 |
| 11 | 5 | 4 | 19 | 3 | 20 | 0 |
| 12 | 0 | 4 | 24 | 0 | 40 | 13 |
| 13 | 5 | 15 | 25 | 2 | 45 | 0 |
| 14 | 5 | 24 | 24 | 2 | 45 | 0 |
| 15 | 4 | 12 | 23 | 2 | 30 | 0 |
| 16 | 5 | 13 | 58 | 3 | 50 | 18 |
| 17 | 0 | 14 | 30 | 0 | 50 | 18 |
| 18 | 0 | 40 | 20 | 0 | 54 | 13 |
| 19 | 12 | 11 | 73 | 6 | 55 | 4 |
| 20 | 0 | 27 | 23 | 0 | 46 | 0 |
| 21 | 8 | 18 | 18 | 6 | 32 | 5 |
| 22 | 6 | 4 | 44 | 5 | 26 | 10 |
| 23 | 2 | 32 | 50 | 2 | 59 | 20 |
| 24 | 0 | 22 | 45 | 0 | 35 | 0 |
| 25 | 5 | 20 | 39 | 3 | 38 | 10 |
Cobb: lumbar curve angulation in degrees; LL: lumbar lordosis in degrees; p: preoperative; P: postoperative; SVA: sagittal alignment in centimetres.
The type of deformity was classified according to Mummaneni et al.9
The complications of the surgery were recorded and both the motor and sensory neurological changes as a result of the procedure.
Selection of patients and fusion levelsAll the patients operated were class or type II.9 In cases where a posterior fixation was performed (23), the procedure took place in 2 stages, starting with a lateral interbody fusion (XLIF) and then the second stage a week later.
Selection of the fusion levels was:
- •
Lumbar curve: from L1 to L5 by the direct lateral approach. The L5-S1 space was included in the fusion as long as there was a residual curve at this level, degenerative disease or spondylolisthesis.
- •
Thoracic curve: this was performed using the open posterior approach with screws from T5 to T10, in cases with a thoraco-lumbar kyphosis greater than 20 degrees (T11 to L2), thoracic scoliosis of more than 40 degrees or thoracic kyphosis of more than 60.
- •
Extension to the ilium: as long as the fusion extended above L2 fixation to the ilium was performed with a screw AIS2.
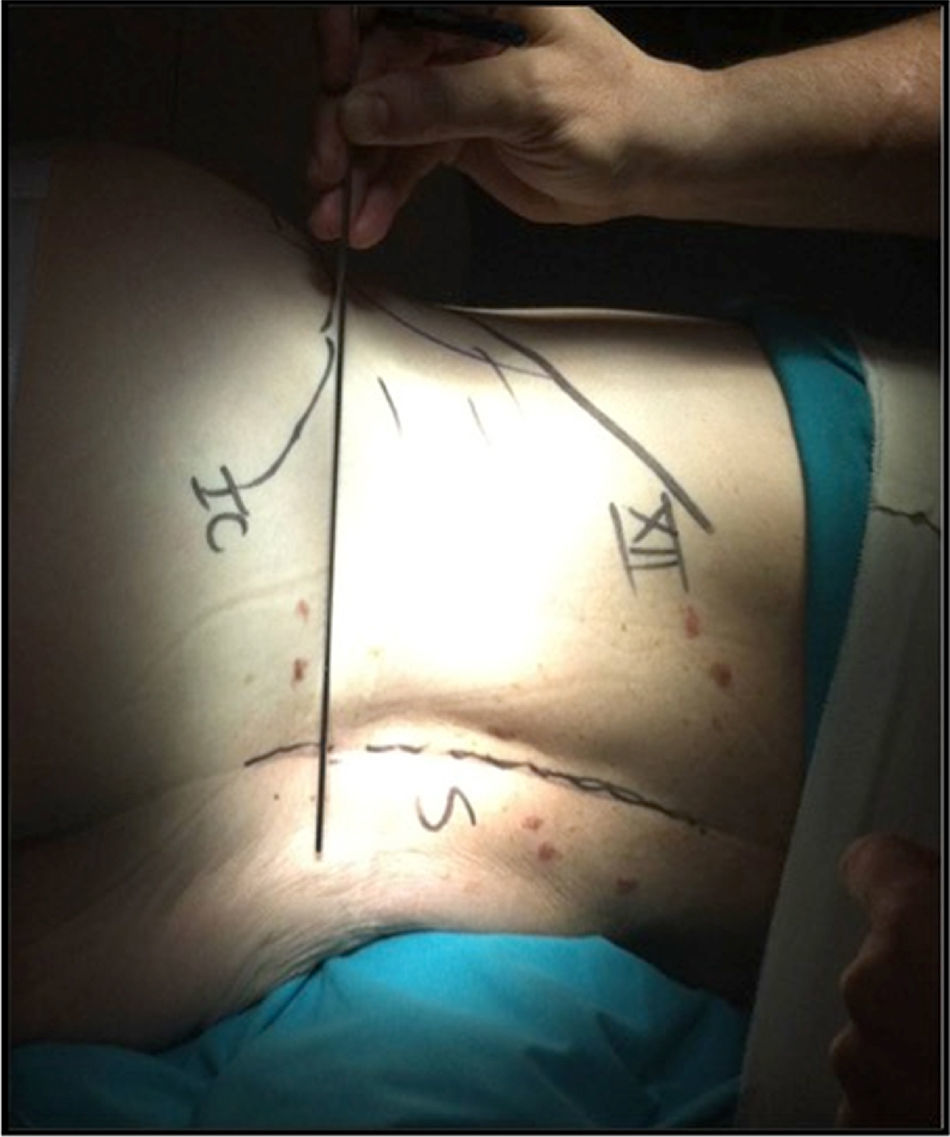
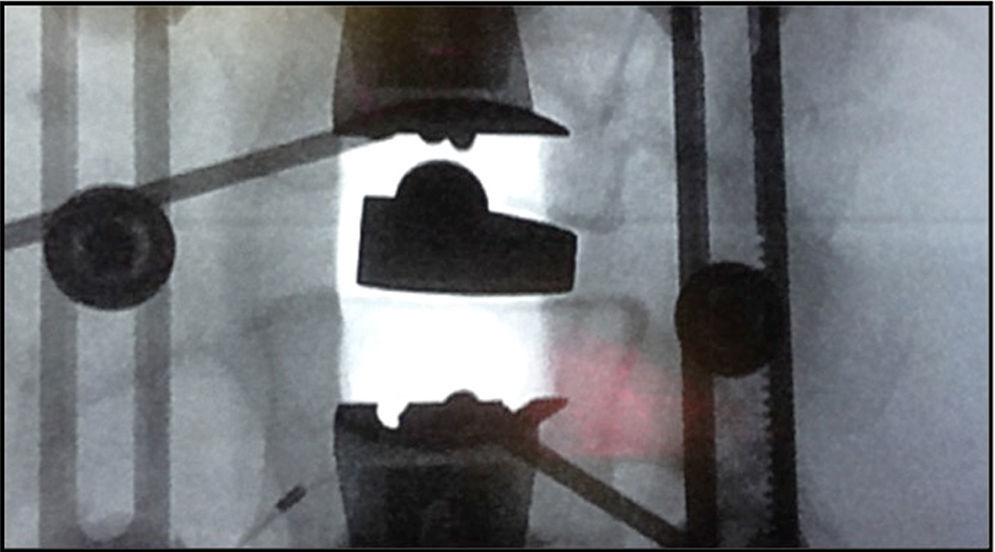
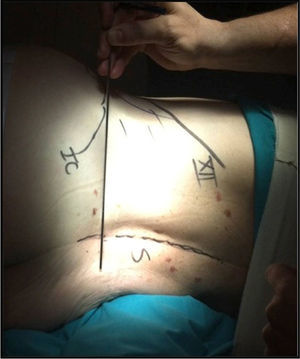
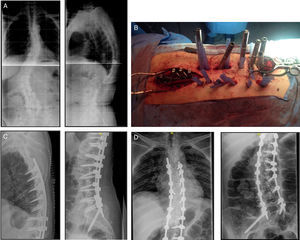
The patient is placed in the lateral decubitus position (Fig. 1) on a radiotransparent table with a break at the lumbosacral area. Whenever possible, due to the position of the iliac crest, we approach the lumbar spine from the concavity. In cases of major curves, the position of the segmental arteries needs to be taken into consideration. In these cases, we perform an angio-CAT scan and follow the principles of Takata et al.10 If we are going to put the vessels at risk, we approach the spine through its convexity. Using an image intensifier in lateral view, a vertical line is marked that crosses the centre of the intervertebral disc to be operated and another horizontal line at its mid point. An incision of around 3 or 4cm is made through which up to 3 levels can be approached. When 4 levels are to be approached we make 2 transversal incisions (Fig. 2) centred in the vertebral body instead of in the disc. After the skin and subcutaneous cell tissue, the fascia of the oblique abdominal musculature is opened and the corresponding muscles (oblique major, oblique minor and transverse), until the retroperitoneum. The transverse process of the superior vertebra, the psoas muscle and the intervertebral disc are palpated by blunt finger dissection. Under radioscopic control the guide needle is placed in the appropriate position and a first neurophysiological check is made. Using a series of dilators a working window is achieved through the psoas muscle. We use the Ravine© (K2M) dilator, which is entered through the needle placed in the intravertebral disc. Under radioscopic control the site is located where the first valve of the separator is to be fixed to the vertebral body with a nail of the same length (Fig. 3). The needle is then removed from the intervertebral disc and the other valve is opened and fixed to the other vertebral body. After placing light sources, additional blades can be placed with special care under neurophysiological monitoring at all times. Once the intervertebral disc has been located, the annulus fibrosis is opened with the scalpel and the discectomy is performed. At this point it is essential to section the contralateral annulus under radioscopic control. The vertebral discs are then prepared up to the subchondral bone and dilators are introduced which give us an idea of the size, length and thickness of the implant. If the deformity is major, we release the ipsilateral third of the LLCA.5 Once the measurements have been taken, a test cage is inserted and its placement is checked under radioscopic control, as well as its primary stability. The definitive implant is inserted filling it with demineralised bone matrix (DBM) to enable interbody fusion.
Posterior interbody fusion- •
Lumbar interbody fusion. Percutaneous screws. Using an image intensifier the pedicles are located under both AP and lateral view. The spinous process in the mid line and the vertebral discs should be seen as one line. Under lateral view the superimposed facet joints and the discs should be seen as one line. The skin incision is made; the Jamshidy needle is inserted under radioscopic control through 2 projections, until the desired position is achieved. Then a flexible needle is positioned which will serve as a guide. The dilators are introduced through this needle to continue with the tap and finally with positioning the screw.
After placing the screws, the MIS release of the joints with motor is performed and placement of DBM to facilitate fusion at this level.
- •
MIS TLIF L5-S1. The side where this technique is to be performed is decided depending on the radiological and clinical findings. Once decided, the MIS separator is placed, the joint processes are resected. Root L5 is located and separated cranially, as well as the dural sac protected by the yellow ligament medially. Disc L5-S1 is located and after careful bipolar diathermy haemostasis the discectomy is performed and an interbody cage of the correct length and height is placed.
- •
Screws AIS2. Using the MIS incision of the TLIF the intervertebral foramina of S1 and S2 are located. A puncture is made aligned with them in the sacrum. The pedicle probe is introduced with 20 degrees of anterior angulation and about 40 degrees caudal angulation. The probe is advanced under radioscopic control. Every so often the correct intraosseous trajectory is checked. When the sacro-iliac joint is reached some resistance is felt, which means it is necessary to use a hammer. When we have completed the procedure, the most proximal part of the orifice created is tapped and a polyaxial iliac screw of 8.5mm in diameter and between 70 and 90mm in length is introduced. The advantages of this screw compared to the traditional iliac screw have been well explained by Kebaish.11
- •
Thoracic interbody fusion. We make a conventional midline incision in the thoracic region. The paravertebral muscles are disinserted, the joints are identified and are resected with an osteotome (to then use them as a graft). Using the “free hand” technique described by Kim et al.,12 we then place the pedicle screws as planned previously.
- •
Placement of rods and graft. After measuring the length of the rods, the appropriate profiles are given and the necessary correction manoeuvres made to place the spine in the desired position. Then the autograft obtained from the thoracic joint processes is mixed with DBM and positioned in the posterolateral area of the thoracic spine.
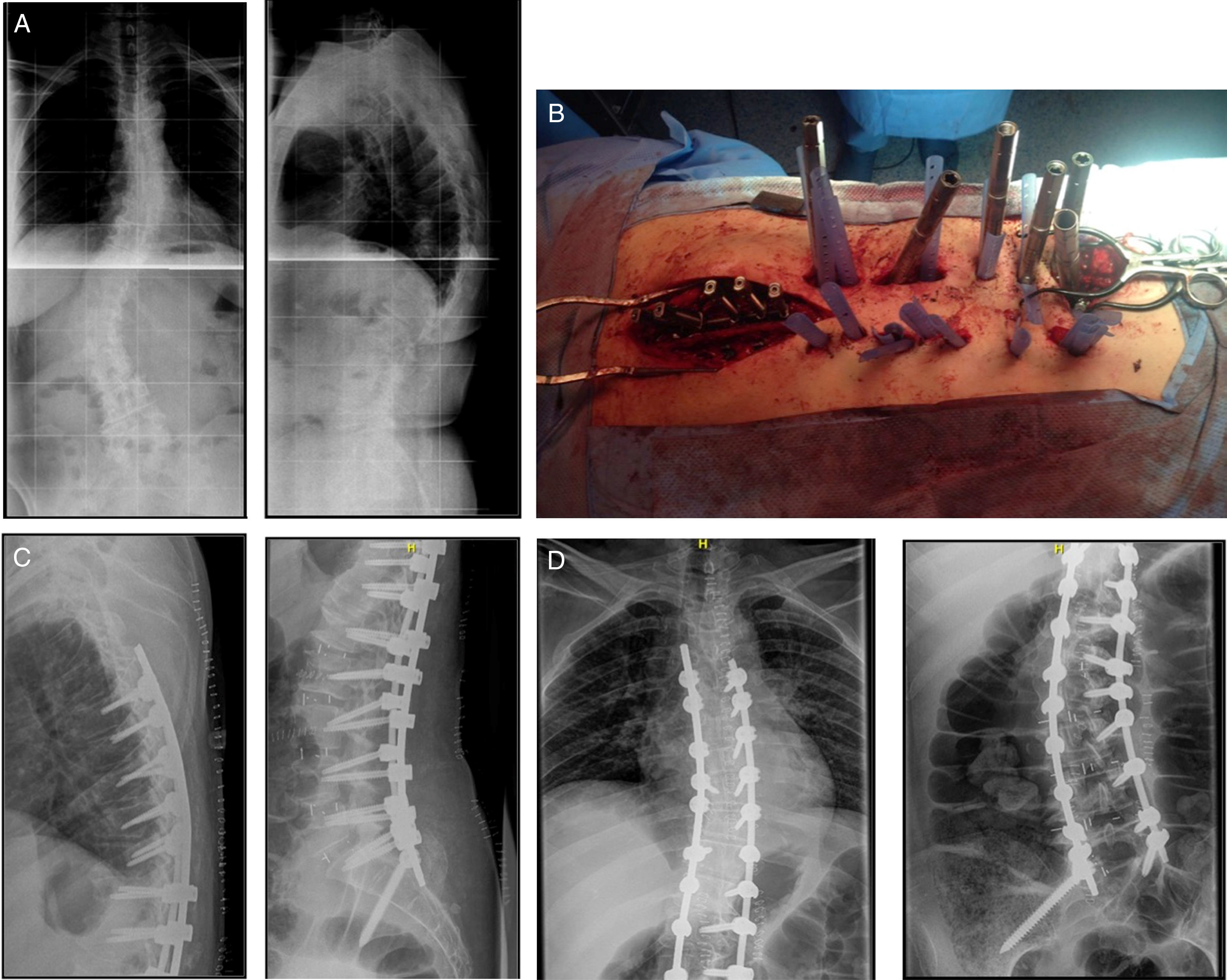
The distribution by sex was: 23 females and 2 males. The mean age was 70 (54–84). Preoperative sagittal vertebral alignment was 5cm, becoming 2cm postoperatively. The preoperative Cobb angle was 31 degrees, becoming 6 degrees postoperatively. This angle remained constant over time. The lumbar lordosis went from 18 degrees preoperatively to 38 degrees after the operation (Fig. 4).
All the patients were classified as type or class II according to Mummaneni et al.9
All the patients underwent posterior instrumentation except 2, who underwent a lateral approach with “single” cages, and lateral plates were used in another 2. Likewise, all the patients underwent an MIS TLIF at level L5-S1 except 2. The mean lateral cages implanted were 3.5. Fixation to the ilium was performed in 13 patients by AIS2 screw. Instrumentation extended to the thoracic area on 3 occasions.
There was no persistent motor lesion in this series. However, there were 10 sensory lesions with paresthesia and dysesthesia in the proximal third of the thigh and ipsilateral groin on the side where the XLIF technique had been performed, which resolved during the following 6 months.
There were 4 complications (16%) that we classified as major or minor, depending on whether reintervention was necessary or not. One patient with junctional kyphosis, another with movement of a lumber pedicle screw, one urinary tract infection and one movement of the cage placed in L5-S1 by MIS TLIF. Only the latter case required reoperation due to a major postoperative radiculopathy. The implant was removed and a cage of greater height and length was placed. Surgical reintervention was not necessary in the other 3 cases.
DiscussionAdult spine deformity is a condition defined as a deformity in the major coronal plane of 20 degrees in a skeletally mature patient.
The incidence of this disorder increases exponentially as time passes, therefore it is estimated that in 2050 the number of patients with ASD will be 8.3% of the world population.2
Surgical correction of the deformity, especially in the sagittal plane, provides clear clinical improvement in patients who undergo the procedure.3–5
However, a major rate of complications occurs in the surgical treatment of ASD.6,7 Thus, Glassman et al.,3 in 434 patients operated for ASD, obtained a complication rate of 24.9%. Schwab et al.13 report 80 patients with at least one complication out of 953 patients operated, which constitutes 8.4%. Charosky et al.14 present 13.7% of medical complications in a retrospective series on 306 patients. Blamoutier et al.15 present a medical complication rate of 16.1% in a series of 180 patients with ASD. Soroceanu et al.16 in 2016 reported an incidence of complications of 26.8%. We can conclude that in general terms, half of the patients operated for ASD will present a complication.
The risk factors for the onset of a complication in the surgical treatment of ASD have been examined by different authors. Transfusion of more than 21 litres of blood, the approach and presence of more than 3 comorbidities are factors that, along with age, have been presented as directly associated with the appearance of a complication.17
Since the publication by Ozgur et al.18 of the XLIF technique in 2006 to date, many papers have advocated the use of this technique for different spinal disorders. With regard to adult spinal deformity, several authors report very promising results. The aim of treating adult spinal defomity by MIS techniques should be the same as that of conventional surgery, namely: decompression of the neurological elements and realignment of the spine, both on the coronal and the sagittal plane. Although further studies are required to establish which patients might benefit from MIS for ASD, it seems clear that the rate of complications in patients who have undergone this type of intervention has significantly reduced.
In 2008 Anand et al.19 reported their first 12 patients diagnosed with ASD and treated with the cMIS technique going from a preoperative COBB angle of 18.93 degrees to 6.19 degrees. They do not report complications although they presented 4% motor lesions and 25% sensory lesions.
In 2010 there were 4 articles reporting the authors’ experiences in patients with ASD who underwent MIS surgery. Dakwar et al.20 present 25 patients who underwent cMIS going from a Cobb angle of 27.9 degrees to 6.4 degrees postoperatively. Major complications of 8% presented in their series and 16% minor complications. No case of motor lesion presented, and there were 12% sensory lesions.
Tormenti et al.21 report 8 hybrid cases, with a Cobb angle that went from 38.9 to 13.4 and lumbar lordosis from 47.4 to 41.8. They also report 12.5% persistent motor lesions and 65% sensory lesions.
Wang and Mummaneni22 report their results in 23 patients who underwent cMIS. The Cobb angle went from 31.4 to 11.5 and lumbar lordosis from 37.4 to 45.5. The patients presented a rate of major and minor complications of 26%, with 12% persistent motor lesions and 26% transient sensory lesions.
Finally, Anand et al.23 report 28 patients treated with cMIS. The Cobb angle went from 22 degrees to 7. There was a major complication rate of 21% and 61% for minor complications. Persistent motor lesions comprised 7% and 61% of the patients presented sensory lesions.
In 2011 Acosta et al.24 reported 36 patients who underwent cMIS. These authors report an improvement of lumbar lordosis, going from an angle of 42.1 to one of 46.2.
Marchi et al.25 in 2012 presented 8 patients treated by cMIS with an improvement of lumbar lordosis from 14.9 degrees to 40 and a rate of major complications of 12.5%.
Anand et al.,26 in 2013, reported the results obtained in 71 patients diagnosed with adult spinal deformity and operated by XLIF and various types of posterior fixation techniques, with a follow-up of 2–5 years. The mean improvement of Cobb angle on the coronal plane went from 25 to 10 and sagittal balance improved from 32 to 11mm. The patients required a mean of 412ml and the complication rate was 22%.
Phillips et al.,27 in 2013, reported 107 patients with ASD operated with the XLIF technique. The mean age was 68 years and the predominant symptoms were lumbar and radicular pain. The complication rate was 24%. Thirteen percent presented a major complication.
Wang et al.28 and Tempel et al.29 report their patient series operated in 2014. The former presented 85 patients with single cages, cMIS and hybrid, with a clear improvement of Cobb angle, especially in the hybrid constructions (from 43 degrees to 15). They presented a complication rate of between 29% and 40%. Tempel et al. present 26 patients, all treated with a hybrid approach, with an improvement in Cob angle of 41.1–12 and a complication rate (major and minor) of 65%. These authors also report a rate of motor deficits of 19% and sensory deficits of 12%.
In 2015, Park and La Marca30 reported 105 patients treated with cMIS and hybrid construction. Improvement in Cobb angle was very significant, from 22.1 to 8.6. The major complications, of the cMIS and the hybrid technique together, were 67%.
In 2016, Kanter et al.31 performed a review of the literature on MIS technique in the surgical treatment of ASD. They analysed 39 articles; 30 covered MIS techniques. Six of them describe details about MIS techniques, and 3 cover treatment of ASD in general. They conclude that MIS techniques are effective in terms of achieving adequate correction of the deformity, reducing the complications that present in conventional surgery.
In 2017 Uribe et al.32 performed an observational study on 2 patient cohorts operated for ASD. One underwent open approaches and the other minimally invasive approaches. Each group comprised 84 patients; they compared the results in clinical and radiological terms and reached the conclusion that MIS techniques in patients operated for ASD reduced extension of the interbody fusion, reduced the reoperation rate, the need for blood transfusion and hospital stay without affecting the final outcomes.
We must insist that MIS techniques cannot be used for all types of deformity. Mummaneni et al.9 have developed an algorithm taking pelvic parameters, deformity and sagittal imbalance into account. They classify patients into 3 class types, those in class II will benefit more from minimally invasive techniques. With the increased experience using the XLIF technique, the development of associated techniques of anterior release by lateral approach and the use of hyperlordotic cages (>20 degrees) the use of MIS techniques has extended even to patients with more rigid deformities, who could be classified as patients with class III ASD.
This study presents the radiological outcomes and complications that arose in a retrospective series of 25 patients with ASD treated by MIS.
Twenty-three of the 25 cases underwent a MIS L5-S1 TLIF. The choice of this technique compared to an ALIF at this level was made due to the good behaviour of the implant at this level in long fusions. The rate of potentially fatal complications with the L5-S1 ALIF procedure (2.5% vascular injury), along with the demonstrated fact that TLIF achieves better correction of deformity with a shorter operating time and shorter hospital stay, made us opt for this technique rather than ALIF for patients who needed fusion of the L5-S1 space.33
As can be observed, the outcomes presented by the different outcomes are variable, but coincide in 2 points that are worth highlighting.
Firstly, both the clinical and radiological outcomes are very satisfactory; our own experience corroborates this. The radiological improvement is more significant in the coronal plane that the sagittal plane, where, although it clearly increases with the XLIF procedure, the improvement is not directly proportional to the number of boxes used. The introduction of hyperlordotic cages and anterior release of the spine using a lateral approach are providing very satisfactory results.5
Secondly, the abovementioned authors, although not all of them, report the rate of complications after MIS techniques. As can be seen, the outcomes vary greatly. Our experience could be added to what we highlight here, a number of complications greater than 4% and less than 12% with an incidence of sensory changes of 40% with no motor changes. Although the rate of complications may seem high, it has to be said that these complications are relatively simple to resolve, without putting the patient's life at risk in any way. Bear in mind that the incidence of infection, cerebrospinal fluid fistula and radicular injury was nil.
Thirdly and finally, the low incidence (4%) of junctional kyphosis in our series is worth noting. We define this event according to Kim and Sravisht34: (1) a proximal junctional sagittal Cobb angle greater than 10 degrees, and (2) at least 10 degrees greater than the preoperative measurement. This complication is frequent in surgical treatment of ASD. Its estimated incidence is between 20% and 40%.34 Various factors have been considered responsible for the onset of this complication. One is undoubtedly injury to the posterior soft tissues in the course of the operation. Although there is no consensus on this point, we consider like Kanter et al.31 that MIS techniques respect these structures more than the hybrid and/or open procedures, and therefore a lower incidence of this complication is to be expected with these techniques. However, the case in our series with junctional kyphosis had undergone cMIS. It is true that the patient was older than 55, with a high body mass index, marked osteoporosis and upper instrumented vertebra in the lower thoracic column, factors that are highly associated with this complication. As indicated, the incidence of this complication in our series is low (4%), although similar to that reported by authors with wide experience in the treatment of ASD using MIS techniques.35
Conclusions- •
Adult spinal deformity is a disorder of increasing in incidence in the developed countries.
- •
Surgical treatment of ASD improves these patients’ quality of life.
- •
Treatment of ASD by MIS obtains results similar to those obtained by conventional surgery, with a lower rate of major complications.
- •
Further studies with a greater level of evidence are required to conclusively determine the advantages of MIS techniques in the surgical treatment of ASD.
Level III.
Ethical responsibilitiesProtection of people and animalsThe authors declare that the research was carried out according to the ethical standards set by the responsible human experimentation committee, the World Medical Association and the Helsinki Declaration.
Confidentiality of dataThe authors declare that they have followed the protocols of their centre of work regarding the publication of patient data
Right to privacy and informed consentThe authors have obtained the informed consent of the patients and/or subjects referred to in the article. This document is held by the corresponding author.
Conflict of interestsThe authors have no conflict of interests to declare.
Please cite this article as: Domínguez I, Luque R, Noriega M, Rey J, Alía J, Urda A, et al. Deformidad del adulto tratada mediante cirugía mínimamente invasiva. Técnica quirúrgica, resultados radiológicos y revisión de la literatura. Rev Esp Cir Ortop Traumatol. 2017;61:419–426.