40%–50% of this septic arthritis occurs in the knee, despite rapid medical surgical treatment, 24%–50% will have a poor clinical outcome. It is not clear which debridement technique, by arthrotomy or arthroscopy, is more effective in controlling infection, or whether or not previous osteoarthritis worsens the outcome. The objective of this study on septic arthritis of the osteoarthritic knee was to analyse which surgical debridement technique, arthroscopy or arthrotomy, is more effective, the clinical and radiographic outcomes of the patients, and how many go on to require a TKR after the infection has healed.
MethodsA retrospective study was performed in 27 patients with native septic arthritis of the knee. Eighteen were men and the mean age was 64.8 years (30–89 years). Fifteen patients were debrided by arthrotomy and 12 by arthroscopy. The effectiveness of debridement in controlling infection, the radiographic progression of the osteoarthritis on the Ahlbäch scale, the need for subsequent replacement, and pain and functional status were analysed using the VAS and WOMAC scales at 52.8 ± 11.2-month follow-up.
ResultsThe infection was controlled in 93% and 92% of the patients, 13% and 42% required 2 or more surgeries for infection control, 18% and 44.4% showed progression of arthritis in the arthrotomy and arthroscopy groups, respectively. One patient in each group required a knee replacement. The VAS score was superior in the arthrotomy group and there were no differences in WOMAC score.
ConclusionDebridement by arthrotomy in the emergency department by non-sub-specialist knee surgeons is more effective than arthroscopic debridement in controlling septic arthritis of the knee. Surgical debridement of septic arthritis in knees with previous osteoarthritis enabled control of the infection with no pain despite the progression of the osteoarthritis.
Un 40%–50% de estas artritis sépticas se producen en la rodilla, a pesar del rápido tratamiento médico quirúrgico, un 24% a 50% van a acabar en un pobre resultado clínico. No está claro que técnica de desbridamiento por artrotomía o por artroscopia es más eficaz para el control de la infección, ni si la artrosis previa empeora o no el resultado. El objetivo de este estudio en artritis séptica de rodilla artrósica es analizar que técnica de desbridamiento quirúrgico, artroscopia o artrotomía, es más eficaz, cual es la evolución clínica y radiográfica de los pacientes y cuantos van a necesitar la implantación de una PTR tras la curación de la infección.
Material y MétodoSe realizó un estudio retrospectivo en 27 pacientes con artritis séptica nativa de rodilla. Dieciocho eran hombres y la edad media 64,8 años (30–89 años), Quince pacientes fueron desbridados por artrotomía y 12 por artroscopia. Se analizó la eficacia del desbridamiento para el control de la infección, la progresión radiográfica de la artrosis en la escala de Ahlbäch, la necesidad de protetización posterior y el dolor y el estado funcional mediante la escala EVA y WOMAC a los 52,8 ± 11,2 meses de evolución.
ResultadosEl 93% y 92% de los pacientes controlaron la infección, un 13% y un 42% requirieron 2 o mas cirugías para el control de la infección, un 18% y un 44.4% mostraron progresión de la artrosis en el grupo artrotomía y artroscopia, respectivamente. Un paciente de cada grupo requirió que se le implantara una prótesis de rodilla. La escala EVA fue superior en el grupo artrotomía y no hubo diferencias en la escala de WOMAC.
ConclusiónEl desbridamiento por artrotomía en el área de urgencias por cirujanos no subespecializados en rodilla es más eficaz que el artroscópico para controlar la artritis séptica de rodilla. El desbridamiento quirúrgico de las artritis sépticas en rodillas con artrosis previa permite controlar la infección con ausencia de dolor a pesar de la progresión de la artrosis.
Septic arthritis in any location has an incidence in Europe of from 4 to 10 patients per 100,000 inhabitants/year. This increases in the case of patients with other comorbidities such as diabetes or rheumatoid arthritis.1 This pathology is characterised by causing rapid destruction of the joint cartilage—from 25% to 50% of patients may have irreversible changes in the affected joint—and it has a mortality rate that varies from 5% to 15%.1,2
40%–50% of these cases of septic arthritis occur in the knee2 and, as is the case in other locations, swift medical-surgical treatment is required to prevent destruction of the joint. Suction of the pus and broad resection of necrotic joint tissue or debridement are the basis of treatment together with the administration of intravenous antibiotics. It is unclear which debridement technique—arthrotomy or arthroscopy—is the most effective in controlling the infection, although it seems that arthroscopic debridement has a lower rate of reinfection and a functional result that is the same or better.3–5
In spite of treatment from 24% to 50% of cases of septic arthritis of the knee will eventually have a poor clinical result.2 In 85% of cases it will require the implantation of a total arthroplasty, while in the remaining 15% another procedure such as arthrodesis will have to be used.2 This is why in patients with knee arthrosis who have septic arthritis some authors2,6 argue that the best treatment option is broad debridement with resection of the joint surfaces and the implantation of a spacer with an antibiotic in an initial operation. Once the infection is under control they recommend implanting a total knee arthroplasty (TKA), as they consider the presence of arthrosis associated with septic arthritis makes it highly probable that pain will persist. However, other authors7,8 argue that debridement of the arthrotic joint and TKA implantation should only be used when pain persists.
In this work we analyse the evolution of treatment using debridement by arthroscopy or arthrotomy of patients diagnosed with septic arthritis of the knee with previous arthrosis. We firstly ask which surgical debridement technique - arthroscopy or arthrotomy - is the most effective. Secondly, we describe clinical and radiographical evolution after surgical debridement, together with the number of patients who will need the implantation of a TKA following cure of the infection.
Material and methodsWe present a retrospective review of patients diagnosed consecutively with septic arthritis of the knee and treated by surgical debridement (arthroscopic or arthrotomic) from 2013 to 2016 and who had a follow-up period of at least one year. This study was approved by the Clinical Research Ethics Committee of our hospital (protocol number PI-18-096), and all of the patients signed the informed consent document. Patients with osteosynthesis material or knee implants were excluded, as were those with non-bacterial infections and those under the age of 30 years old.
The diagnosis of septic arthritis of the knee was established by following modified Newman criteria9 which require the existence of at least of the following four criteria: a) positive culture of fluid from the affected joint; b) positive culture of another sample (haemoculture) when septic arthritis is suspected; c) typical symptoms of arthritis (pain, swelling, erythema, oedema, an increase in local temperature and functional limitation) together with inflammatory joint fluid in a patient who has already received previous antibiotic therapy, and d) pathological synovial anatomy which suggests infection.
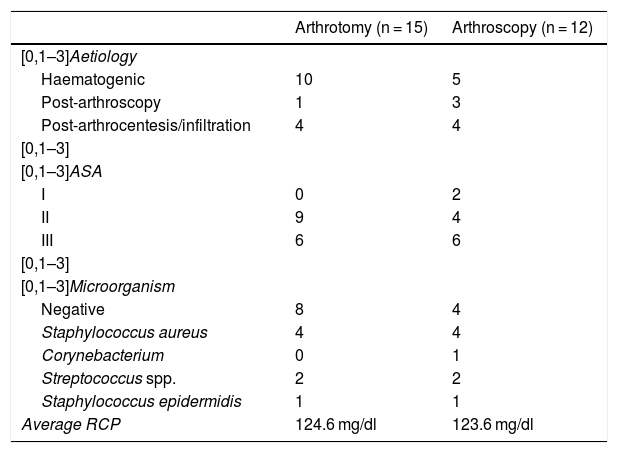
29 patients were found with native septic arthritis of the knee, of whom 27 (18 men [66.6%] and 9 women [33.4%]) fulfilled the inclusion criteria. Average age: 64.8 years (range 30–89 years). Fifteen patients (55%) had a haematogenic cause and 12 (45%) were diagnosed with septic arthritis following a medical intervention (4 after an arthroscopy, 6 after an infiltration and 2 following drainage arthrocentesis) (Table 1).
Epidemiological data for each type of debridement.
| Arthrotomy (n = 15) | Arthroscopy (n = 12) | |
|---|---|---|
| [0,1–3]Aetiology | ||
| Haematogenic | 10 | 5 |
| Post-arthroscopy | 1 | 3 |
| Post-arthrocentesis/infiltration | 4 | 4 |
| [0,1–3] | ||
| [0,1–3]ASA | ||
| I | 0 | 2 |
| II | 9 | 4 |
| III | 6 | 6 |
| [0,1–3] | ||
| [0,1–3]Microorganism | ||
| Negative | 8 | 4 |
| Staphylococcus aureus | 4 | 4 |
| Corynebacterium | 0 | 1 |
| Streptococcus spp. | 2 | 2 |
| Staphylococcus epidermidis | 1 | 1 |
| Average RCP | 124.6 mg/dl | 123.6 mg/dl |
All of the patients had symptoms of a reduction in joint movement, pain and synovitis; 81.5% also had redness at joint level and none of them had symptoms of initial sepsis or cutaneous lesions. Blood samples were taken from all of them for a count and leucocyte formula, together with C-reactive protein determination (CRP). A synovial fluid sample was extracted by arthrocentesis, and this was sent for biochemical study (glucose and proteins), a cell count and culture. At the moment of diagnosis in the emergency department all of the patients had raised CRP, with an average value of 180.8 mg/dl (12.6−533 mg/dl).
Surgical debridement techniqueAll of the patients were treated surgically in the emergency department facility by different on-duty surgeons, some of whom are not knee surgery experts. The selection of the technique to be used, and therefore assignment to the arthrotomy or arthroscopy debridement groups, took place according to the preference of the surgeon. Fifteen patients were debrided by arthrotomy and 12 by arthroscopy. Six patients in the arthrotomy debridement group were men, as were all of the patients in the arthroscopy group. Nine patients were operated on the right knee in the arthrotomy group as were 8 in the arthroscopy group. Both groups had a similar distribution in terms of comorbidities and ASA level (Table 1).
Arthrotomy was performed with ischemia due to elevation of the limb without expression. An anterior longitudinal approach was used, with medial parapatelar arthrotomy followed by synovectomy of the bottom of the subquadricipital sac and lateral recesses and washing with 10 L saline solution (SSF) and closure of the wound in planes with compressive bandage. Surgery using arthroscopic technique also takes place with ischemia due to elevation of the limb without expression; the approach was through an anteromedial and lateral portal. Synovectomy of the bottom of the sac and lateral recesses was performed, washing with 10 L of SSF. Samples were taken for culture and anatomical pathological study in both groups. A Redon drain was left until discharge from the same was <50 cc, although it was never left for longer than 72 h. The limb was immobilised with an orthosis at 10° knee semiflexion until the pain improved and the inflammation reduced, at which time passive and active mobilisation of the joint commenced. Partial loading was permitted during the first 8 weeks with the help of walking sticks, followed by total loading.
Although 53% of the patients in the arthrotomy debridement group had no positive cultures, the biochemistry of their synovial fluid was compatible with septic arthritis of the knee: Staphylococcus aureus was detected in 26.5% and Streptococcus spp was detected in 13.3% of them. In the group treated by arthroscopy 33.3% had no positive culture but did have compatible biochemistry of the knee joint fluid; S. aureus was isolated in 33.3%, as was Streptococcus spp. in 16.6%. In both groups one patient had a positive culture for Staphylococcus epidermidis (Table 1).
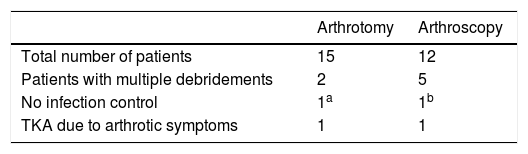
Debridement efficacyThe number of debridements necessary to control the infection was recorded, together with whether or not the infection persisted in each surgical group. We define persistence of the infection—and therefore failure of the debridement—as when signs and symptoms of septic arthritis remain, or when progression of the infection in the bone is detected by simple X-ray imaging or computed tomography. The patients who required multiple debridements but who finally achieved control of the infection were not considered to be cases of persistence of the infection or failure of the treatment. The infection was defined as correctly under control with normalisation of the RCP value, the disappearance or persistence of pain (no pain, some pain or a lot of pain), the absence of signs of inflammation (redness, a high temperature or swelling) and non-progression of the infection in the bone (Table 2).
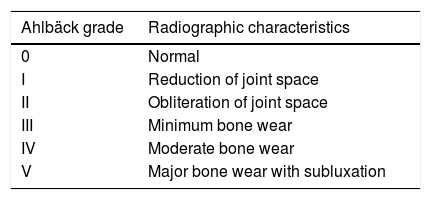
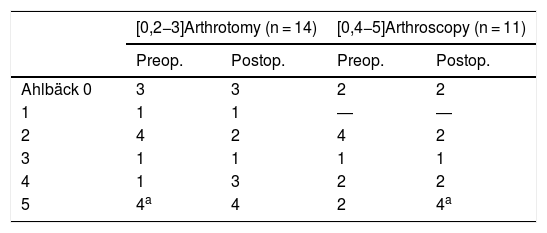
Progression of the arthrosisProgression of the arthrosis was studied in 25 patients by X-ray images of the affected knee in anteroposterior and lateral projection at the moment of admission and 12 months after debridement on Ahlbäck’s scale10 (Table 3). Two patients, one from each type of debridement, showed persistence of septic arthritis and required amputation and initial placement of a prosthesis, so they were eliminated from this analysis.
The need for implantation of a prosthesisThe time that had passed in months was determined from the debridement and implantation of a TKA, together with the number of patients who were implanted with a TKA (Table 2).
Pain and functional stateIn 16 patients (7 in the arthrotomy group and 9 in the arthroscopy group), with an average time of evolution of 52.8 ± 11.2 months and 55.3 ± 10 months after the reference event, respectively, were evaluated telephonically for their degree of pain on the verbal numerical scale (VNS) from 0 to 10 (0: no pain; 10: maximum pain) and the Western Ontario and McMaster Universities scale was determined (WOMAC)11 to evaluate functional state (Table 4).
Ahlbäck classification according to type of debridement and postoperative progression.
| [0,2−3]Arthrotomy (n = 14) | [0,4−5]Arthroscopy (n = 11) | |||
|---|---|---|---|---|
| Preop. | Postop. | Preop. | Postop. | |
| Ahlbäck 0 | 3 | 3 | 2 | 2 |
| 1 | 1 | 1 | ― | ― |
| 2 | 4 | 2 | 4 | 2 |
| 3 | 1 | 1 | 1 | 1 |
| 4 | 1 | 3 | 2 | 2 |
| 5 | 4a | 4 | 2 | 4a |
The qualitative variable data studied was described in terms of frequency or percentage of occurrence, and the quantitative variables were described in terms of their average and standard deviation.
ResultsDebridement efficacy (Table 2)Two (13%) of the 15 patients debrided using arthrotomy required subsequent debridements. One of them had bone involvement (osteitis) and a prosthesis was implanted in two stages. The other patient had correct clinical evolution following the second debridement. In 14 (93%) patients the infection was brought under control.
Five (42%) of the 12 patients debrided using arthroscopy required a second debridement, and all of them underwent correct clinical evolution. One patient had necrotising fasciitis of the limb which required suprachondral amputation. The infection was controlled in 11 (92%) patients: in 6 after the first debridement using arthroscopy and in the remaining 5 following a second debridement.
Progression of the arthrosisProgression of the arthrosis was similar after both types of debridement. Of the 14 patients in the arthrotomy group, 11 (78.5%) had previous arthrosis: 4 (36.3%) had grade V arthrosis. Two (18%) patients showed worsening of their Ahlbäck classification, and the remaining 9 (82%) did not. The 3 (21.5%) patients who had no arthrosis prior to the treatment showed no signs of arthrosis in their evolution.
Of the 11 patients in the arthroscopy group, 9 (81.8%) had previous arthrosis, 2 (22%) with grade Ahlbäck V arthrosis. The arthrosis progressed in four (44.4%) patients, and in the 5 remaining patients (64.6%) it did not progress. Of the 2 (18.2%) patients without previous arthrosis, neither went on to develop arthrosis.
Of the 25 patients studied, 20 (80%) had previous arthrosis. Progression from the initial Ahlbäck grade was detected in 6 cases (24%), with no differences according to the type of debridement, and the average progression was 2 Ahlbäck group points.
The need for a prosthesis (Table 2)In 2 (8%) patients, one in the arthrotomy group and the other in the arthroscopy group, TKA implantation was indicated 12 and 24 months after debridement, respectively. Both patients were Ahlbäck grade V prior to debridement. The other patients had no pain (7 and 4 patients) or had little pain (4 and 3 patients) in the arthrotomy and arthroscopy group, respectively.
Pain and functional state (Table 4)Post-debridement pain in the arthrotomy group (3.1 ± 2.5) in the VNS was higher than it was in the arthroscopy group (1.6 ± 2.2). No differences were found in the WOMAC functional scale between the arthrotomy group (17 ± 15.4) and the arthroscopy group (16.1 ± 15.9).
DiscussionThe most important finding in this study is that although 80% of patients with septic arthritis of the knee had previous arthrosis, and although this progressed in 24% of them, only 8% required the implantation of a TKA because of pain. We therefore advise debridement using arthrotomy in cases of septic arthritis of the knee with arthrosis, and we do not recommend debridement with the implantation of a spacer in a first operation followed by the implantation of a prosthesis in a second operation. Our study is the first to evaluate the progression of arthrosis and the need for implantation of a prosthesis in patients who had recovered from septic arthritis of the knee with previous arthrosis
The increasing incidence of septic arthritis is associated with the increase in infections of prosthetic material, the aging of the population, more invasive operations and an increase in the use of immunosuppressor therapy.12 The aetiology of the infection does not seem to be a factor in a poor prognosis.1,2,13 The study by Geirsson et al.12 found that the risk of septic arthritis are the infiltration of corticosteroids into the joint is 0.04%, while after arthroscopy it is 0.14%. Although our study does not evaluate the risk after these procedures, we found that there was previous manipulation of the knee in 45% of the cases, for infiltration, arthroscopy or arthrocentesis.
Infection microbiology is similar to those published in other series,1,13 and S. aureus is the most common organism (30%), followed by Streptococcus spp. (15%). The rate of negative cultures, at 44%, is also similar to other published figures.1,13
Septic arthritis of the knee is an orthopaedic emergency, and swift diagnosis and treatment is one of the keys to success. Delay in the start of treatment is a major factor in a poor prognosis.13,14 Delay in treatment or inappropriate treatment may lead to permanent harm to the mobility of this joint, and this may affect from 10% to 73% of patients.2,15 Septic arthritis of the knee may also cause destruction of the cartilage and subchondral bone if treatment is delayed.1,14
Infection is controlled in a high percentage of patients with septic arthritis of the knee by debridement using arthrotomy (93%) or arthroscopy (92%). There is currently no consensus as to whether it is better to perform debridement using arthrotomy vs. arthroscopy which, as is the case in our series, seem to be similar in efficacy3–5 in controlling the infection. Nevertheless, the persistence of pain was more prevalent after debridement using arthrotomy, although functioning was similar regardless of debridement type. This agrees with the series of Rodrigo Peres et al.4, although it does not agree with other series3,5 in which arthroscopy gave rise to less pain and better functioning. Although the repeat intervention rate seems to be lower for debridement using arthroscopy,3–5,13,14 this was not the case in our series, where it was lower after debridement using arthrotomy. We believe that this higher rate of repeat interventions in arthroscopic interventions may be explained by the fact that these operations are performed in the emergency department by surgeons who are not specialised in arthroscopic knee surgery.
A factor in a poor prognosis is the need for multiple debridements. Dave et al.,13 in their series of 52 patients with native septic arthritis of the knee show that 25% of patients require multiple debridements (two or more). Our series as a whole shows a similar rate of repeated debridements (7 patients, 26%), although if we analyse the patients treated using arthroscopy separately this percentage rises to 40%. Of the 7 patients with a second debridement, only one progressed to osteitis that required the two-stage implantation of a prosthesis, while the other cases were cured. A second debridement makes it possible to obtain a good result in the majority of cases (85% of our patients), and surely the prognosis becomes worse when it fails and a third debridement is necessary.
The incidence of knee arthrosis in the cases of septic arthritis in our series was high (80%), as it was in other series.3 There is controversy as to whether1 or not3 arthrosis is a risk or poor prognosis factor for septic arthritis. The presence of arthrosis in a knee with septic arthritis may justify the initial treatment of the septic arthritis of the knee by a two-stage TKA, on condition that we are able to argue that the arthrosis will progress and cause pain at an early stage after the septic arthritis. From 90% to 100% of good results have been described after primary6,16 or two-stage implantation6–8 of a TKA to treat the sequelae after septic arthritis of the knee with bone involvement and destruction of the joint.
The arthrosis progressed in 24% of the patients in our series, which is far below the 91% in which it progressed in the study by Chen et al.2 This difference is surely due to the long delay in the start of treatment for the patients in the latter study. In our series, 82.6% of the patients with previous arthrosis of the knee, in spite of the progression of the same, did not describe incapacitating pain after debridement, and they maintained a correct functional condition. Therefore only two patients (8%) required the implantation of a TKA due to worsening joint pain at 12 and 24 months after the septic event, and both were grade V Ahlbäck at the time of the septic arthritis. The remaining 6 patients who were grade V Ahlbäck after the septic arthritis had no intense pain.
When there is a history of knee infection the risk of infection following the implantation of a TKA increases by up to 4%–9.7%, depending on the series,6,9,12 vs 0.2% for primary prostheses.14 It seems that the longer the time which elapses between the septic arthritis episode and implantation of the TKA, the lower the risk of infection.16 It is clinically important to know whether debridement of septic arthritis in an arthrotic knee using arthrotomy or arthroscopy gives good results, as this will make it possible to delay any future prosthetic surgery and increase the time interval between the infection and the prosthesis, which probably reduces the subsequent risk of infection.
This study has limitations. Firstly, it is a retrospective study, with the possible risks of data selection and loss which this type of study involves. Secondly, multiple surgeons took part in this study, reducing its intrinsic validity while increasing its extrinsic validity. Thirdly, the small size of the sample makes it impossible to compare the group averages at a level with statistical significance. Fourthly, we do not know the extent of the synovectomy and debridement undertaken in each operation, as this datum is hard to extract from the information contained in surgical reports.
ConclusionDebridement using arthrotomy in the emergency department by surgeons who are not specialised in knee surgery is more effective than debridement by arthroscopy in controlling septic arthritis of the knee. Surgical debridement of septic arthritis in knees with arthrosis makes it possible to control the infection without pain, in spite of the progression of the arthrosis. This will increase the interval of infection-free time before a prosthesis is implanted.
Level of evidenceLevel of evidence III.
Conflict of interestsThe authors have no conflict of interests to declare.
Please cite this article as: Sabater-Martos M, Garcia Oltra E, Collado Saenz F, Martínez-Pastor JC, Hernandez Hermoso JA. El desbridamiento por artrotomía de la artritis séptica de rodilla artrósica es más eficaz que el artroscópico y retrasa la necesidad de prótesis a pesar de la progresión de la artrosis. Rev Esp Cir Ortop Traumatol. 2021;65:3–8.