The best management of severe bone defects following total knee replacement is still controversial. Metal augments, tantalum cones and porous tibial sleeves could help the surgeon to manage any type of bone loss, providing a stable and durable knee joint reconstruction. Five different types of prostheses have been analysed: one prosthesis with straight stem; two prostheses with offset stem, with and without supplement, and two prostheses with sleeves, with and without stem. The purpose of this study is to report a finite element study of revision knee tibial implants. The main objective was to analyse the tibial bone density changes and Von Misses tension changes following different tibial implant designs. In all cases, the bone density decreases in the proximal epiphysis and medullary channels, with a bone density increase also being predicted in the diaphysis and at the bone around the stems tips. The highest value of Von Misses stress has been obtained for the straight tibial stem, and the lowest for the stemless metaphyseal sleeves prosthesis.
No hay consenso en el tratamiento de elección de los recambios protésicos de rodilla con defectos óseos severos. Las opciones son variadas, cada una con sus ventajas e inconvenientes. Los trabajos clínicos publicados tienen sus limitaciones en cuanto al número de pacientes y el poco seguimiento clínico. Se presenta un trabajo biomecánico con elementos finitos comparativo de 5 diseños de implantes tibiales: vástago recto, con offset con/sin suplemento y vainas con/sin vástago, para poder analizar el comportamiento tanto del hueso tibial como del material a lo largo del tiempo. Dentro de las limitaciones que presenta un modelo matemático hemos podido ver que los implantes con vástago recto producen el mayor valour de reabsorción ósea alrededor del vástago, mientras que la menor reabsorción ósea tiene lugar en el hueso de la diáfisis proximal. Las vainas metafisarias tibiales sin vástago producen una menor reabsorción ósea que el resto en el canal medular.
One of the key factors in prosthetic knee replacement is the bone defect. A preoperative evaluation can be carried out through radiographic and computed tomography (CT) studies, but the type of defect will be defined during the surgical procedure.1–3 If the defect is not contained, that is, an Anderson type 2 or 3, it is possible to use trabecular metal cones or metaphyseal sleeves.4–9 Both provide a mechanical support for the implant, favouring long-term biological fixation, decreasing the complexity of the reconstruction and avoiding possible load transmission problems related to grafts from an organ bank.1,10
The long-term effect of this type of prosthetic knee replacement on tibial bone resorption is not clearly known. There are several computational studies of bone remodelling based on the finite elements method for fixations in the femoral component,11,12 as well as the tibial component, but only for primary implants.13–15
In the present work we conducted a biomechanical study based on the finite elements method to analyse the effect of incorporating a tibial implant after prosthetic knee replacement on the process of bone remodelling. The study compared 5 types of tibial implant designs: straight stem, sleeves with and without stem, offset stem with and without supplement.
The working hypotheses were the following: (a) that metaphyseal sleeves provide better load transmission with less tip effect; (b) that the tip effect is greater in the case of straight stem, since this stem is adjusted to the diaphyseal canal; (c) that the tibial implant with offset may be indicated in selected cases of tibial deformity. The general objectives were: (a) to improve the knowledge of the biomechanical behaviour the tibial implants according to their prosthetic design; (b) to improve the indication of the type of implant for each type of tibia to be treated with prosthetic replacement. The specific objectives were: (a) to analyse the tension supported by each prosthetic design with physiological loads in order to predict the evolution of bone density in the long term and (b) to compare the biomechanical behaviour of the sleeves, combining a short stem and no stem.
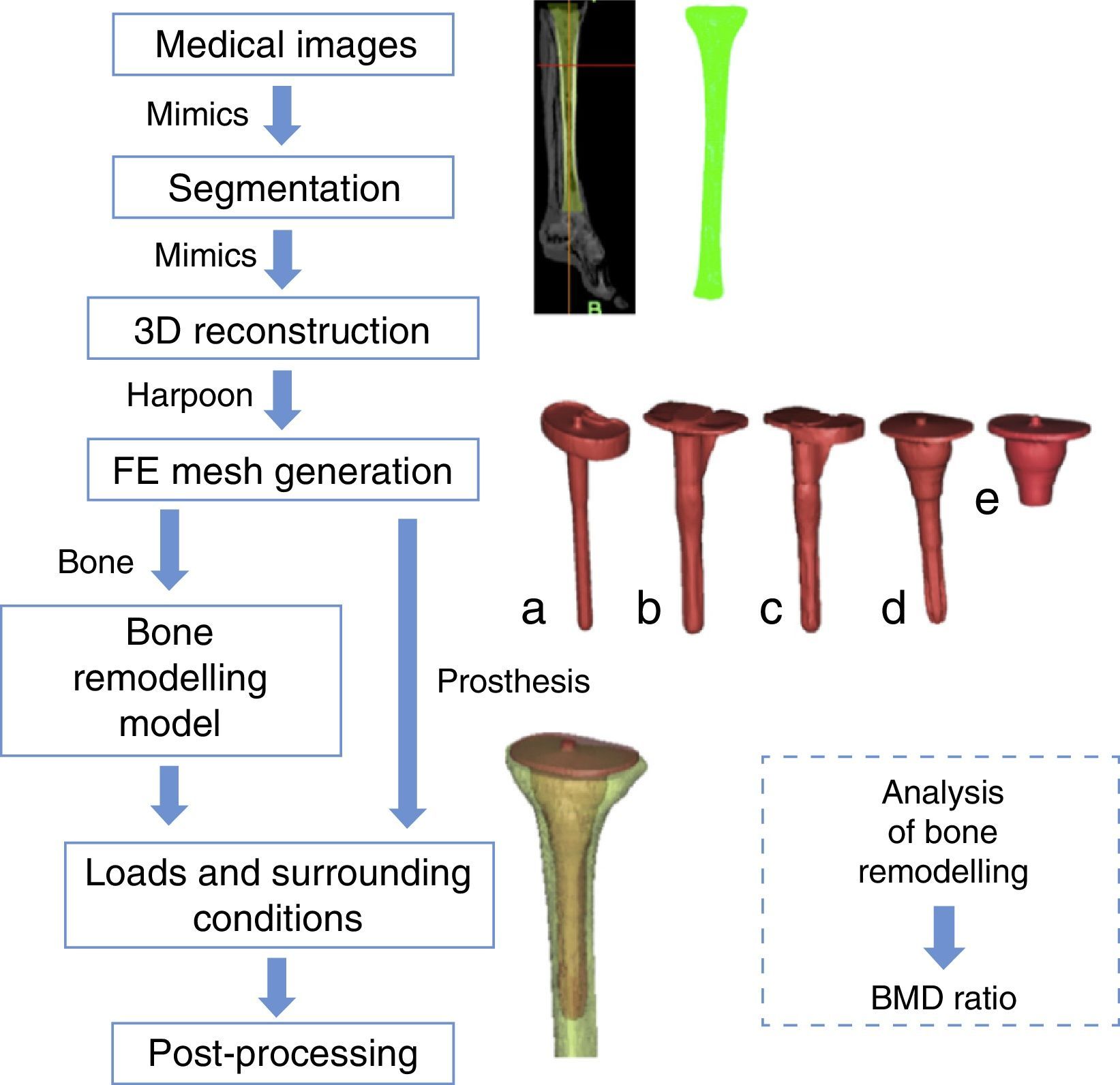
Material and methodsFinite elements modelsFig. 1 shows all the steps followed for a complete reconstruction of prosthesis modelling up to the final analysis of bone remodelling. The starting point were images provided by an axial computed tomography study of the left tibia of a 36-year-old male. The images were acquired through a Brilliance 64 device (Philips Healthcare, The Netherlands) using a current of 257mA and a voltage of 120kV. The spatial resolution was 0.65mm×0.65mm, with a reconstruction matrix of 768×768. The distance between images was 2mm. We analysed 5 different types of knee revision prosthesis models: straight stem, sleeves with stem and without stem (model PFC SIGMA TC3, Depuy, Johnson & Johnson, Warsaw, USA) and offset stem with and without supplement (model NextGen Legacy Constrained Condylar Knee-LCCK, Zimmer, Indiana, USA), (Fig. 1a–e). All 5 models were made of titanium and were uncemented stems, with cement at the surface.
We used the software package Mimics v.11 (Materialise, Louvain, Belgium) to segment and reconstruct the geometric models. The software was used to position the different tibial stems in the correct orientation. The finite elements meshes were generated automatically, with the Harpoon v.2 software package (Harpoon Sharc Ltd, Manchester, UK, 2006) (Fig. 1a–e). The elements comprising the models were tetrahedrons, in order to reproduce the complex geometry of the bone with sufficient precision.
The size of the element used (2mm) is within the asymptotic region of convergence and represents a good balance between numerical precision and computational requirements.
The prostheses were assigned material properties corresponding to titanium. The Young modulus assigned was 80GPa and the Poisson coefficient was established at 0.32.
The bone-prosthesis interface was simulated as completely joined, that is, as if it were perfectly osseointegrated.
Bone remodelling modelBone is a living tissue with mechanical properties that change according to the stimuli received.16 The literature contains various mathematical models which reproduce this behaviour; these models are known as “bone remodelling models”.17–19 The present work used the model by Doblaré and García.20,21
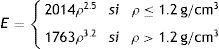
This bone remodelling model, following the work by Doblaré and García,20,21 is based on the principles of continuous damage mechanics, using the theory of damage as a mathematical tool to formulate bone remodelling capacity. The mechanical properties of bone depend on the porosity and the “fabric tensor” H. The “fabric tensor” H includes the distribution of bone mass and the directionality of the structure. The main directions of H are parallel to the direction of bone tissue orthotropy and the influence of porosity (or equivalently, the apparent density, ρ, or the volumetric fraction of bone tissue, vb) are given by:
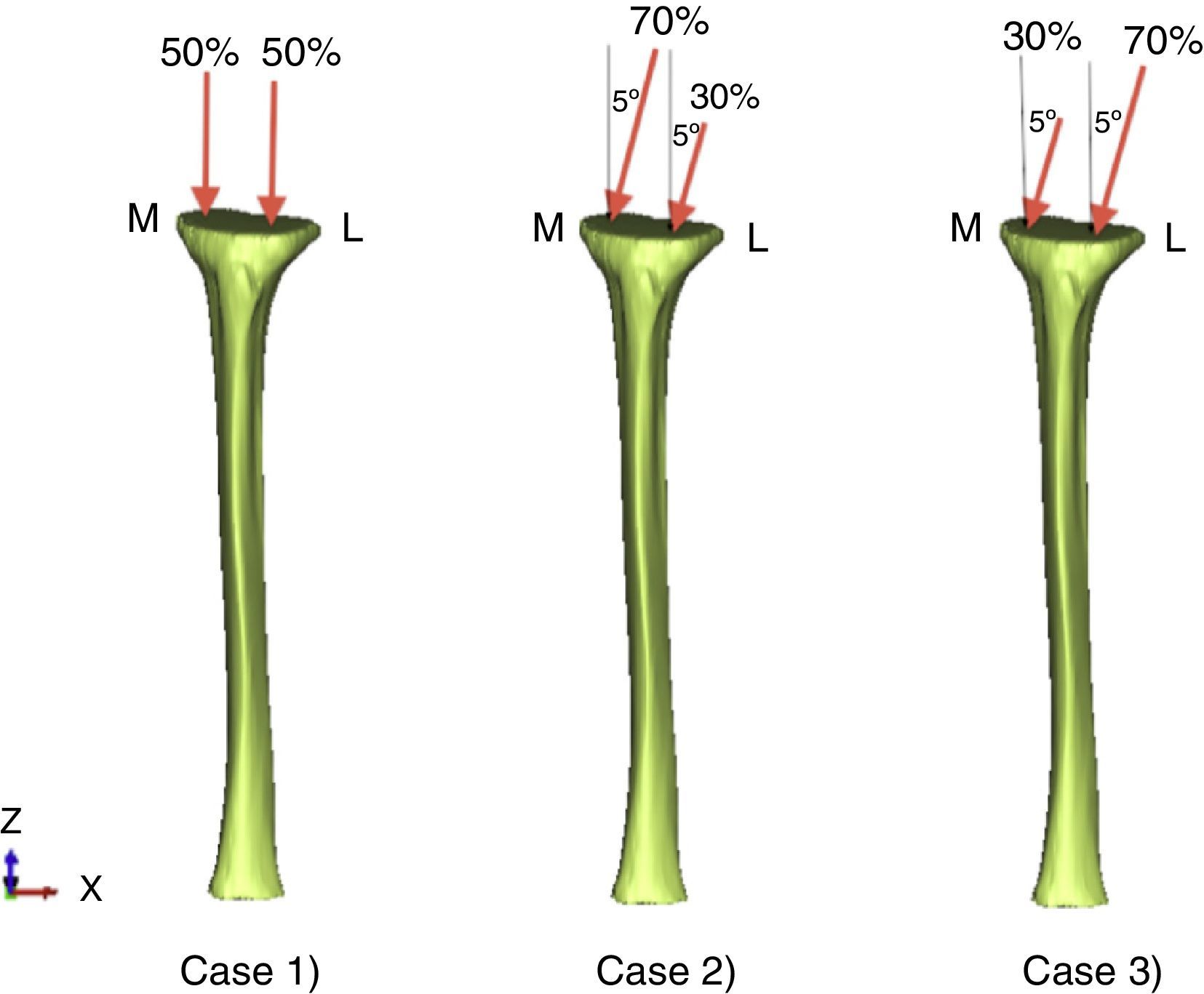
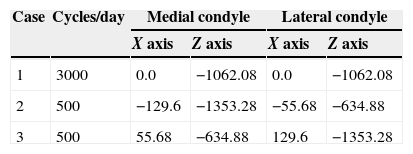
Loads and support conditionsThe lower part of the tibial diaphysis was restricted along the vertical and horizontal axes (Fig. 2). The simulation considered the physiological load conditions corresponding to the 3 most representative stages of the process of walking, including the force of reaction on the condylar surface.22,23 The 3 load cases were (Fig. 2): case 1: the force of reaction on the condylar surface was distributed uniformly to each of the condyles in a perpendicular direction to that surface; case 2: the anterior force was distributed into 70% and 30% in the medial and lateral condyles, respectively, with the force tilted 5° with respect to the vertical, so that the horizontal component of the force pointed in a medial direction; and similarly case 3 corresponded to a symmetric situation to case 2. The load values considered for the tibia have been represented in Table 1.
Numerical simulationThe analysis by finite elements (Fig. 1) was conducted using Abaqus v6.11 (Dassault Systemes Simulia Corp., Providence, RI, USA, 2006). The mathematical model for bone remodelling was implemented in a user subroutine in order to simulate the properties of bone. Specifically, we started from an arbitrary initial situation (uniform density ρ=0.5g/cm3 and isotropic behaviour of the bone), and then applied the loads corresponding to the process of walking. The changes in bone density distribution were calculated over 300 analysis increments corresponding to 300 days of use of a prosthesis (Fig. 1). Among other aspects, we evaluated the density distribution obtained by the simulation, as well as the change in evolution of bone mineral density, called BMD ratio.
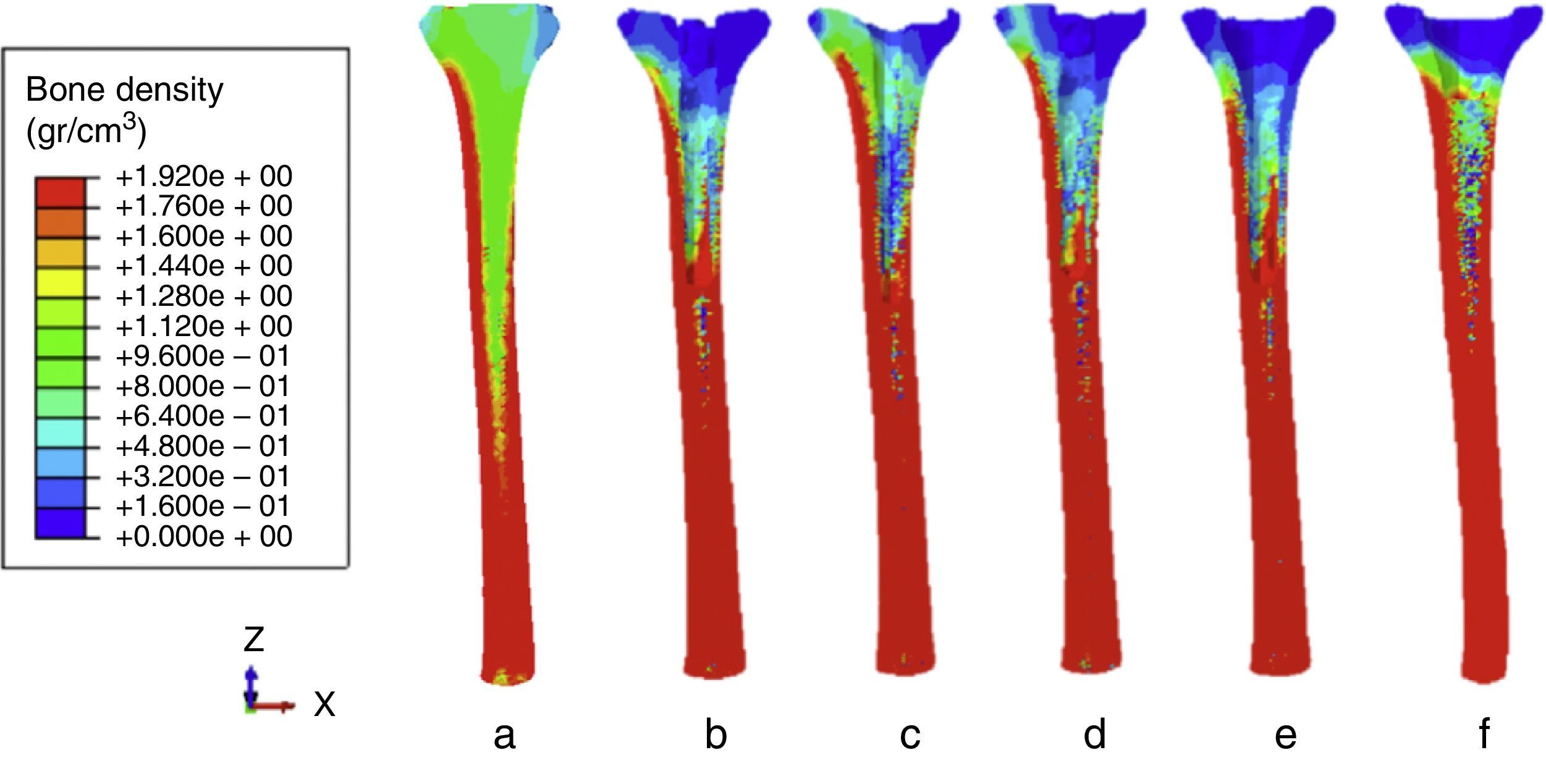
ResultsThe bone density distributions predicted following insertion of the prosthesis are represented in Fig. 3 (after 300 days). In all cases, bone density was reduced in the proximal epiphysis and the medullary canal, and increased in the diaphysis and the bone surrounding the tip of the stems.
Bone density distribution (g/cm3) 300 days after incorporating the prosthesis. (a) Before the implantation. (b) Offset stem with without supplement. (c) Straight stem. (d) Offset stem with supplement. (e) Sleeves with stem. (f) Sleeves without stem. (See different prostheses in Fig. 1.)
Fig. 3 shows how the prosthesis with straight stem produced the greatest bone resorption around the stem, whilst the lowest bone resorption took place in the bone of the proximal diaphysis. The highest value of bone resorption in the proximal diaphysis took place in the case of the prosthesis with sleeves with stem. On the other hand, the sleeves without stem produced less resorption bone than the rest of prostheses. In qualitative terms, the greatest bone resorption was generated by the prosthesis with sleeves with stem and offset without supplement.
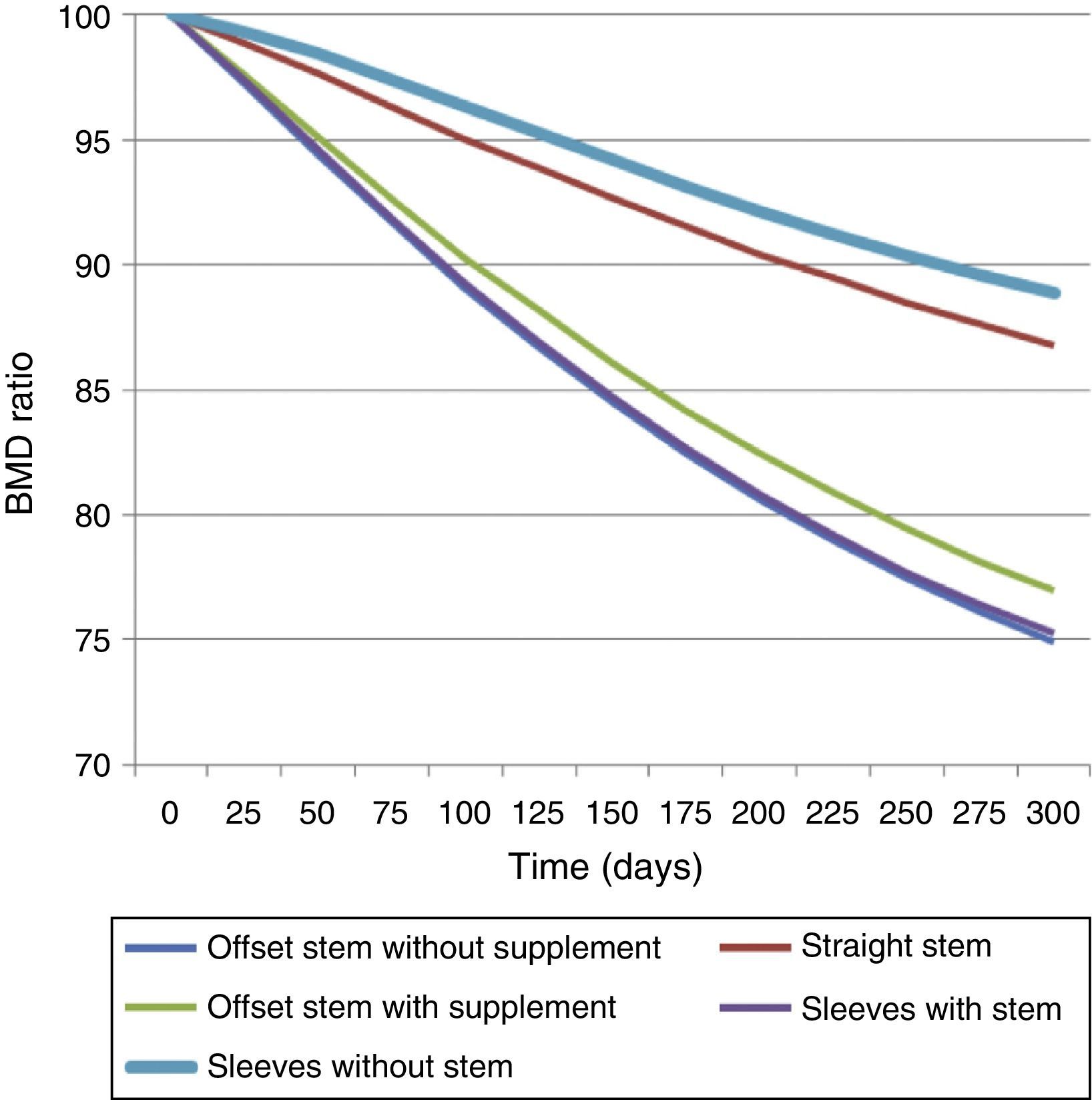
In quantitative terms, Fig. 4 shows the variation of the bone mineral density (BMD) ratio over time for all 5 prostheses. The prosthesis with sleeves without stem was expected to have the lowest bone density variation, followed by the straight stem. On the other hand, the highest level of bone resorption was produced by sleeves with stem and offset stem without supplement. These results supported the observations in Fig. 3.
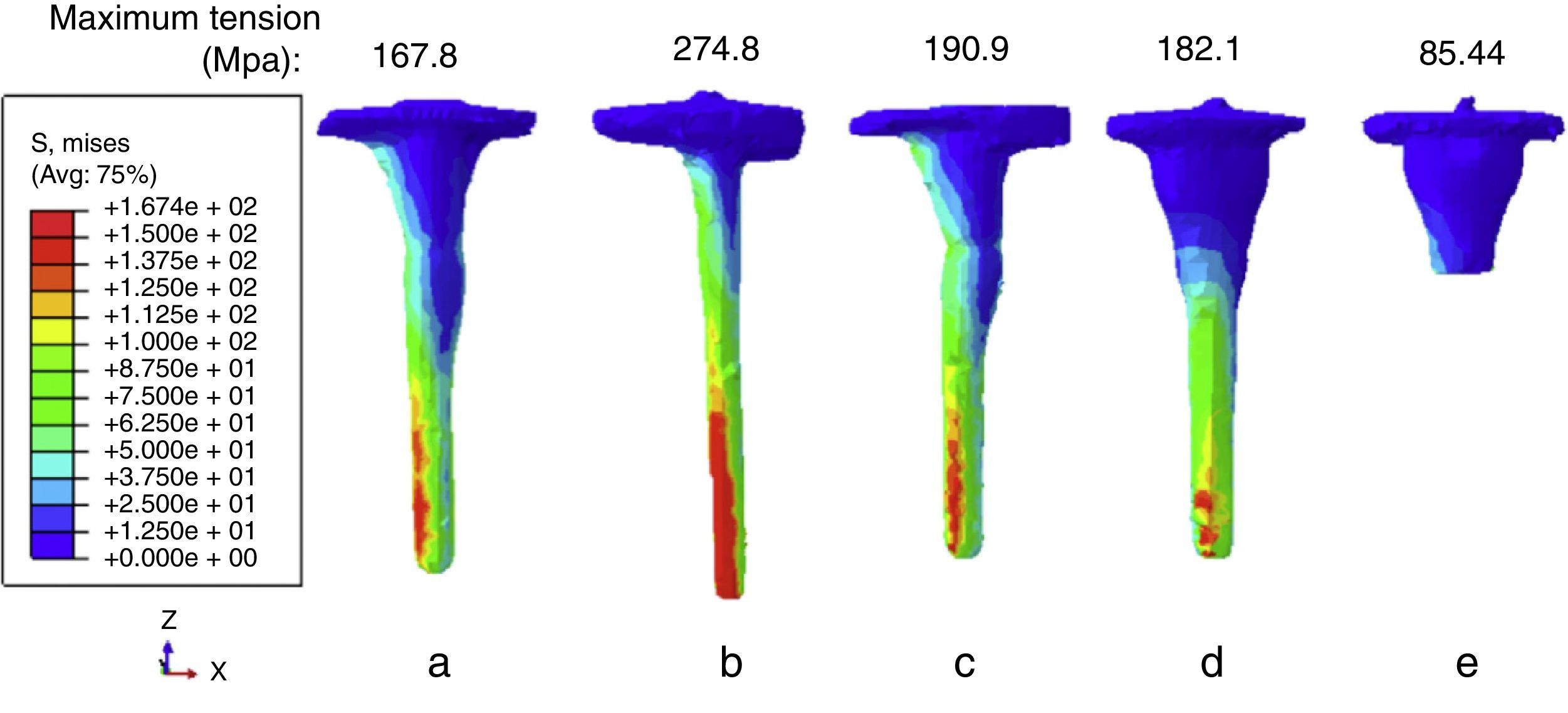
We also analysed the Von Mises tension in the prostheses. None of the prostheses reached its maximum resistance value (450MPa). The distribution of Von Mises tension has been represented in Fig. 5. The highest value was obtained for the prosthesis with straight stem, and the lowest for the prosthesis with sleeves without stem.
DiscussionThe design of knee revision implants has progressed, and the same is true of bone defect management.24 It has been calculated that 82% of patients will require a femoral or tibial increase and 28% will require a bone graft.24
Clinical works show no consensus regarding the treatment of choice in prosthetic knee replacement with severe bones defects. Among the different fixation methods described, sleeves have represented a revolution in terms of implant fixation philosophy. Haidukewych25 argues that stems should be used routinely in replacements, since they unload the epiphyseal area with poor fixation. Schmitz et al.10 highlight the biomechanical advantages of tantalum cones, their low elasticity modulus (3MPa) and high porosity (70–80%), allowing a more uniform transfer of tensions in the tibia. Kindsfater et al.11 highlight the advantages of sleeves without stems: they are simple to place with freedom of rotation, without exceeding the tibial plate and impacted by pressure, with no need for cement, regardless of any tibial diaphyseal deformity; it is not necessary to prepare the tibial canal, thus reducing the risk of intraoperative fissures.
For Agarwal et al.,6 the difference between cones and sleeves is that cones require cementing the implant, whereas sleeves are impacted directly on the tibial metaphysis. Sleeves provide a stable platform and avoid the need for excessive bone resection. Another significant advantage is that they also allow full load immediately.
After analysing all the published clinical works, we considered a series of limitations in relation to sample size and medium/short term follow-up. Agarwal et al.6 presented 103 patients intervened with tibial metaphyseal sleeves and a mean follow-up period of 43 months (range: 30–65 months). The correct size of a sleeve should fill the metaphyseal defect, and it is not necessary to add a metal increase or fill with bone graft. The objective of narrow and short stems is to help centre the implant in the canal, rather than support the load. Osseointegration was studied by conventional radiography, and was defined as good bone apposition in the absence of radiolucency between the sleeve and cancellous bone in 3 interfaces of the 4 existing, measured in the porous proximal third of the sleeve. Osseointegration was good in 102 cases. In 2 cases, the revision was carried out due to aseptic loosening and in both cases the sleeves did not have stem. Alexander et al.7 conducted a retrospective study of 28 knee replacements using the model of uncemented metaphyseal sleeves (model Sigma TC3), in patients with type 2B and 3 intraoperative bone defects, with a follow-up period of 2 years. They did not find any complication regarding the sleeve. Up to 23% referred pain in the tip of the stem, located in the diaphysis. In cases of chronic diaphyseal pain longer than 2 years, the stem was longer than 150mm and with no groove. However, there was no significant relationship with the type of stem (grooved or non-grooved) or its length. Neither were any differences found in relation to the amount of bone in contact with the stem; but the diameter of the stem did have an influence. The sample considered in this work was small, with a loss of 10 patients during follow-up. Barnett et al.12 conducted a retrospective study of 51 cases. In 11 patients they placed a sleeve without tibial stem, to avoid the tip effect described in the work of Alexander.7 In both works, the series were small, with a loss of patients during follow-up. In spite of this, the authors state that sleeves are a long-term option for biological fixation, which allows filling of severe tibial defects, with good clinical results and minimal complications, favouring implant osseointegration without the need for cement. All coincide on the need for long-term clinical works to confirm that this type of implant is a good option.
Jensen et al.26 used DEXA to evaluate changes in bone mineral density in a prospective, randomised study with 40 cases intervened using knee replacements model NexGen (Zimmer Warsaw, USA): 17 cases with trabecular cone and 19 without cone. The stems were with and without offset, both at the tibial and femoral levels. The bone remodelling pattern was very similar in both groups, with no significant differences. The increase in bone resorption throughout the tibial stem at 2 years from the replacement was notable. The finite elements study did not find significant differences when comparing stems with and without offset.
In terms of biomechanical works, there have been several in vitro works with tensional analysis of composite tibial models,27 experimental works13,28 analysing tension distribution in the tibial cortical following the placement of different types of knee prostheses, and mathematical studies with finite elements to analyse pain in the tip in prosthetic knee replacements.29
Completo et al.13 conducted an experimental assessment of synthetic tibias through gauges in 3D, examining tension distribution in the cortical of the proximal tibia with 3 types of knee prostheses: cemented tibial plate, pressure-adjusted stem, and tibial plate alone with short, single-block stem. These authors observed an increase of the tension distribution in the tibia close to the tibial plate with the cemented stem. With the pressure-adjusted stem, the tension distribution was less at the proximal level, but greater throughout the stem. This could generate bone resorption, as observed in the cases analysed in the present study. There is a concentration of tensions in the tip of the stem in both cases, due to proximal physiological bone resorption.
Metaphyseal sleeves are not a new concept in revision surgery, as they were previously used in modular hinge implants. Their current use is possible in less constrained prostheses, and they are a good option to treat extensive metaphyseal tibial bone defects. The work presented coincides with the observations reported by Kindsfater,11 Agarwal6 and Alexander7 in terms of the need to associate a short, grooved, small diameter stem, which facilitates centring of the implant and its long-term evolution.
In all the tibial designs we have observed an increase in bone resorption at the proximal tibial level with an increase of bone density at the diaphyseal level around the tip of the stem, in accordance with clinical observations (Jensen et al.26). Implants with a straight stem presented the highest bone resorption values around the stem, whereas the lowest bone resorption took place in the bone of the proximal diaphysis. Overall, sleeves without stem produced less bone resorption than the rest of models, an aspect to be added to the advantages indicated by Kindsfater et al.11
As limitations of the study we can highlight:
- -
It is a mathematical model with restriction at the level of the distal tibia.
- -
We have only simulated the process of walking, ignoring other, less frequent activities like climbing stairs, for example.
- -
The bone-prosthesis interfaces have been simulated as completely joined, that is, considering that the prosthesis is perfectly osseointegrated. Therefore, we have ignored the initial situation in which the interface is loose, but have not simulated the osseointegration process.
As conclusions we can state that:
- -
The highest tension values are located in the tip of the stem.
- -
The prosthesis undergoing the greatest tensions is the straight stem, which explains the pain in the diaphyseal tip.
- -
The prosthesis with offset and sleeves with stem produced the most bone resorption.
- -
The prosthesis that generated less bone resorption over time was that with sleeves without stem; therefore, it is the one which would produce the best biomechanical behaviour in the long term.
The authors declare that this investigation did not require experiments on humans or animals.
Confidentiality of dataThe authors declare that they have followed the protocols of their workplace on the publication of patient data.
Right to privacy and informed consentThe authors declare having obtained written informed consent from patients and/or subjects referred to in the work. This document is held by the corresponding author.
Conflict of interestsThe authors have no conflict of interests to declare.
Level of evidenceLevel of evidence II.
The authors wish to thank SECOT Foundation for sponsoring this study through a Research Project grant in 2012.
Please cite this article as: Quílez MP, Pérez MA, Seral-García B. Estudio biomecánico de la tibia en el recambio de una artroplastia de rodilla. Rev Esp Cir Ortop Traumatol. 2015;59:365–371.