Congenital knee dislocation is a very rare entity, characterised by deformity in genuine recurvatum present at birth, and there is currently no consensus on the optimal treatment. The aim of the present study is to analyse the functional results and long-term complications after the application of a protocol of therapeutic action for the management of congenital knee dislocation (CKD) created in a reference centre for child orthopaedics.
Materials and methodsRetrospective descriptive study of patients with congenital dislocation of the knee who followed CRPL between January 1997 and December 2010. Demographic variables, type of treatment, functional outcomes at the end of the follow-up, complications and relapses were studied. The conservative treatment consisted of serial casts, leaving the surgical treatment for cases in which passive flexion was not achieved above 30° or the conservative treatment failed.
Results9 patients (11 knees) met the inclusion criteria. The 66.7% were girls and the average follow-up was 15 years (9-22). In all cases, conservative treatment was initiated. Of the 11 knees treated, less than half (36%) required surgery. The average Lysholm questionnaire was 90.3 points, the WOMAC pain 0.4 (0–1), WOMAC stiffness 1.8 (0–6) and WOMAC function 3.8 (1–12).
ConclusionsThe existence and application of the PLCR protocol in a pathology as rare as congenital knee dislocation suggests good long-term functional results with few complications and no recurrences.
La luxación congénita de rodilla es una entidad muy infrecuente, caracterizada por la deformidad en genu recurvatum presente al nacimiento, no existiendo en la acutalidad consenso sobre el tratamiento óptimo. El objetivo del presente estudio es analizar los resultados funcionales y complicaciones a largo plazo tras aplicación de un protocolo de actuación terapéutica para el manejo de luxación congénita de rodilla (PLCR) creado en un centro de referencia de ortopedia infantil.
Materiales y métodosEstudio descriptivo retrospectivo de pacientes con luxación congénita de rodilla que siguieron el PLCR entre Enero de 1997 y Diciembre de 2010. Se estudiaron variables demográficas, tipo de tratamiento, resultados funcionales al finalizar el seguimiento, complicaciones y recidivas. El tratamiento conservador consisitió en yesos seriados, dejando el tratamiento quirurgico para los casos en los que no se consiguió una flexión pasiva mayor a 30º o fracasó el tratamiento conservador.
Resultados9 pacientes (11 rodillas) que cumplieron los criterios de inclusión. El 66.7% fueron niñas y el seguimiento medio fue de 15 años (9-22). En todos los casos se inició tratamiento conservador. De las 11 rodillas tratadas, en menos de la mitad (36%) se precisó realizar cirugía. El cuestionario Lysholm medio fue de 90,3 puntos, el WOMAC dolor 0,4 (0-1), WOMAC rigidez 1,8 (0-6) y WOMAC función 3,8 (1-12).
ConclusionesLa existencia y aplicación del protocolo PLCR en una patología tan infrecuente como la luxación congénita de rodilla sugiere unos buenos resultados funcionales a largo plazo con escasas complicaciones y sin recidivas.
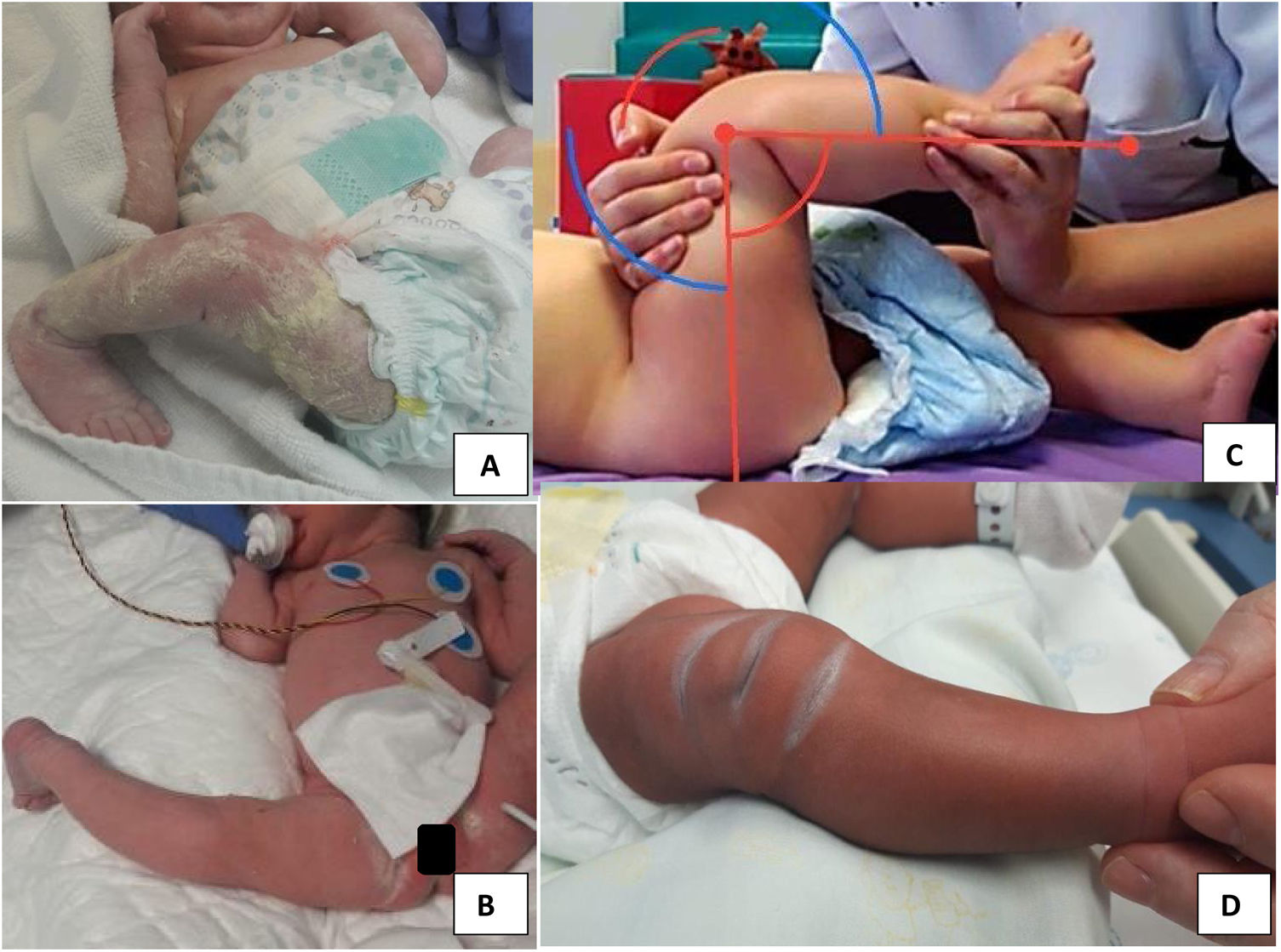
Congenital knee dislocation (CKD) is a very rare condition, with an estimated incidence rate of 1 per 100,000 live births,1 originally described by Chatelaine in 1822 and characterised by a genu recurvatum deformity present at birth (Figs. 1 and 2).
It can present in isolation or due to muscle imbalances in the context of other syndromes such as arthrogryposis, myelomeningocele or Larsen syndrome. It is frequently associated with other musculoskeletal anomalies such as hip dysplasia, clubfoot, congenital vertical talus and congenital dislocation of the elbow.2
Diagnosis is made soon after birth by physical examination, and plain radiography is helpful in some cases to establish level of severity.3
There are multiple therapeutic options, ranging from conservative measures, such as physiotherapy, serial casting, bracing and traction, to surgical options. To our knowledge, there is currently no clear consensus on the optimal treatment of this condition at present.3 Different studies indicate that a high percentage of cases will require surgery (capsulotomy, quadriceps lengthening or femoral shortening, among other techniques) after failure of conservative treatment.4,5
The aim of the present study is to analyse the functional outcomes and long-term complications after implementation of a protocol for congenital knee dislocation (PCKD) for the management of this disease created in a paediatric orthopaedic referral centre.
MethodsFor the present investigation we undertook a retrospective descriptive study of case series of patients with congenital knee dislocation who followed the PCKD between January 1997 and December 2010 in the same paediatric orthopaedic referral centre, and with a minimum follow-up of 9 years.
All patients with a diagnosis of congenital knee dislocation born between January 1997 and December 2010 and treated in the same paediatric orthopaedic centre were included. Exclusion criteria were the presence of congenital rotational or lateral dislocation of the knee, inability to walk due to associated malformations, and non-completion of follow-up.
Different variables were analysed such as demographics (sex and age), affected limb, associated diseases and deformities, type of treatment according to the PCKD, age at which surgical treatment was performed, functional results at the end of follow-up (measured using the WOMAC6 and Lysholm7 questionnaires), complete or incomplete mobility of the knee compared with the contralateral knee if healthy, or considering extension at 0° and flexion at 120° in the case of bilateral involvement, and possible complications or recurrences.
Description of the protocol for the management of congenital knee dislocationThe protocol of action carried out in the sample under study was as follows:
- 1
Clinical assessment: examination of the entire lower limb to determine degrees of passive flexion. Quantification of the axis of both lower limbs, as well as the neurovascular status of the affected leg. Rule out other associated congenital anomalies.
- 2
Radiological assessment: useful to confirm the diagnosis and to classify according to severity. X-rays are not routinely performed. They are taken in cases of diagnostic doubt, late diagnosis beyond 6–12 months or deformity clinically compatible with knee subluxation or dislocation, to classify stage, follow up and observe the evolution of this deformity.
- 3
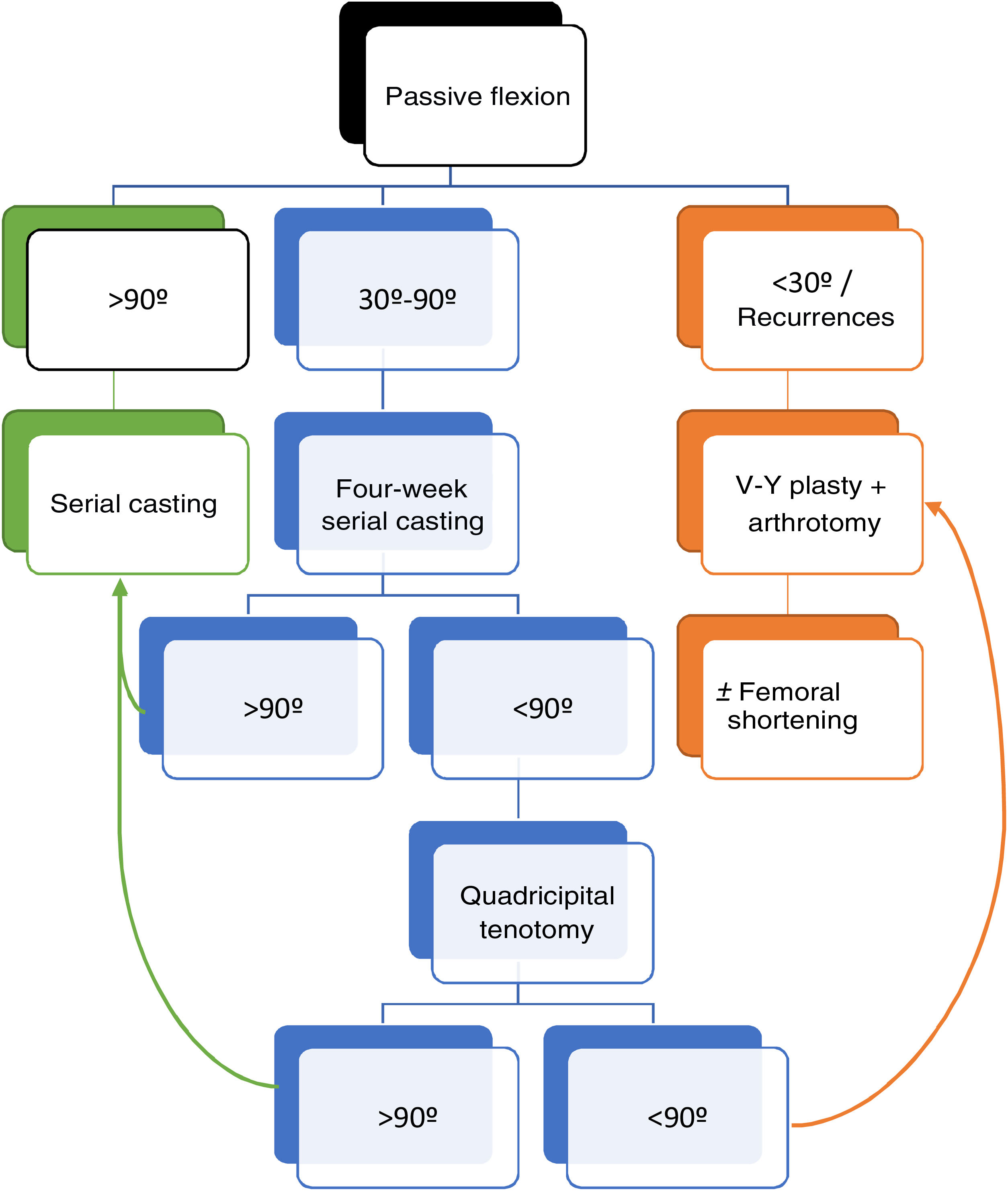
Treatment (Fig. 3): Treatment is started at the time of diagnosis. The degree of contracture of the quadriceps will determine the possibilities for reduction and should be based on the degrees of passive flexion achieved by flexion and decoaptation of the joint.
- -
If>90° of passive flexion is achieved, treatment will be with serial casting and maintained for 2–4 weeks. Immobilisation is carried out under fluoroscopic control without maintained traction.
- -
If flexion is from 30° to 90°, initial treatment is weekly casting, and mobility is re-evaluated after 4 weeks. If >90° is achieved, conservative treatment with casts is maintained, while a quadricipital tenotomy is recommended if flexion after 4 weeks is still <90°.
- -
If flexion is still less than 90° after tenotomy, V–Y plasty combined with arthrotomy is recommended.
- -
If more than 30° passive flexion is not achieved, and if there is recurrence, V–Y plasty combined with arthrotomy is performed to release the displaced ligamentous structures anteriorly.
- -
If this is not sufficient, femoral shortening is performed to avoid complications from quadricipital scarring.
If surgery is necessary, it is performed at around 8–16 months of age in an individualised and non-protocolised manner depending on the results of conservative treatment, associated deformities and expectations.
In cases where other musculoskeletal disorders coexist, it is recommended that the knee be treated first, as good knee position is essential for the management of hip dysplasia or clubfoot to maintain an adequate posture.
The post-surgical and rehabilitative protocol conducted varied depending on the needs of the individual patient. As a general rule, closed casts were used to increase flexion every week for 4–6 weeks, and then those able to walk were allowed to weight bear and caregivers were taught exercises (knee flexion-extension) to recover mobility and for muscle strengthening.
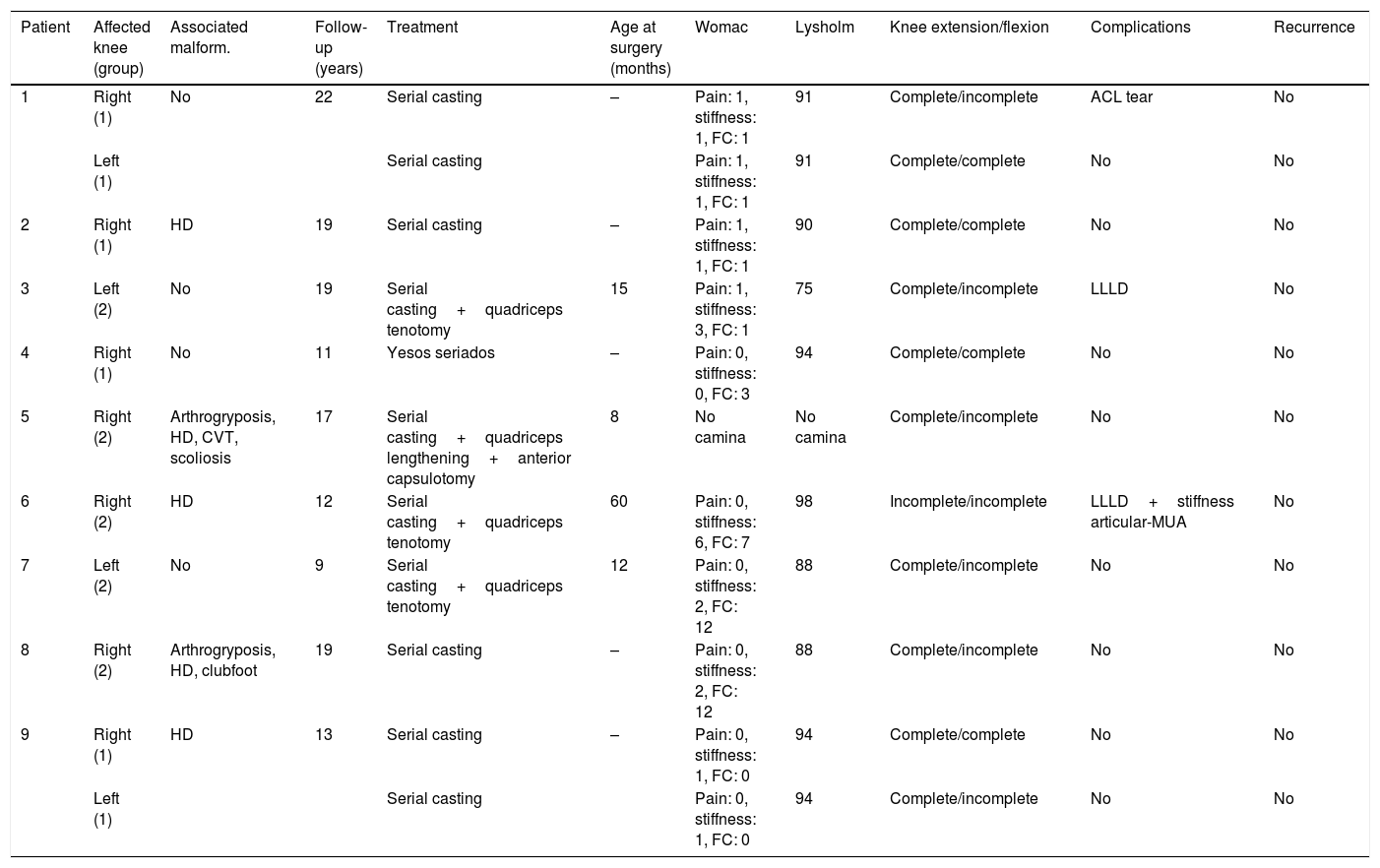
ResultsFrom a total of 12 patients diagnosed with congenital knee dislocation, one patient was excluded due to the presence of congenital lateral knee dislocation and two patients did not complete follow-up. The final sample size analysed was 9 patients (11 knees) who met all inclusion criteria and the minimum follow-up, of whom 67% were girls (n=6) (Table 1).
Characteristics of the sample under study.
| Patient | Affected knee (group) | Associated malform. | Follow-up (years) | Treatment | Age at surgery (months) | Womac | Lysholm | Knee extension/flexion | Complications | Recurrence |
|---|---|---|---|---|---|---|---|---|---|---|
| 1 | Right (1) | No | 22 | Serial casting | – | Pain: 1, stiffness: 1, FC: 1 | 91 | Complete/incomplete | ACL tear | No |
| Left (1) | Serial casting | Pain: 1, stiffness: 1, FC: 1 | 91 | Complete/complete | No | No | ||||
| 2 | Right (1) | HD | 19 | Serial casting | – | Pain: 1, stiffness: 1, FC: 1 | 90 | Complete/complete | No | No |
| 3 | Left (2) | No | 19 | Serial casting+quadriceps tenotomy | 15 | Pain: 1, stiffness: 3, FC: 1 | 75 | Complete/incomplete | LLLD | No |
| 4 | Right (1) | No | 11 | Yesos seriados | – | Pain: 0, stiffness: 0, FC: 3 | 94 | Complete/complete | No | No |
| 5 | Right (2) | Arthrogryposis, HD, CVT, scoliosis | 17 | Serial casting+quadriceps lengthening+anterior capsulotomy | 8 | No camina | No camina | Complete/incomplete | No | No |
| 6 | Right (2) | HD | 12 | Serial casting+quadriceps tenotomy | 60 | Pain: 0, stiffness: 6, FC: 7 | 98 | Incomplete/incomplete | LLLD+stiffness articular-MUA | No |
| 7 | Left (2) | No | 9 | Serial casting+quadriceps tenotomy | 12 | Pain: 0, stiffness: 2, FC: 12 | 88 | Complete/incomplete | No | No |
| 8 | Right (2) | Arthrogryposis, HD, clubfoot | 19 | Serial casting | – | Pain: 0, stiffness: 2, FC: 12 | 88 | Complete/incomplete | No | No |
| 9 | Right (1) | HD | 13 | Serial casting | – | Pain: 0, stiffness: 1, FC: 0 | 94 | Complete/complete | No | No |
| Left (1) | Serial casting | Pain: 0, stiffness: 1, FC: 0 | 94 | Complete/incomplete | No | No |
Affected knee group: 1) initial flexion>90°; 2) initial flexion between 30° and 90°.
ACL: anterior cruciate ligament; CVT: congenital vertical talus; FC: functional capacity; HD: hip dysplasia; LLLD: lower limb length discrepancy; MUA: mobilisation under anaesthesia.
Hip dysplasia was the most frequent associated musculoskeletal malformation, present in 5 patients (55%), followed by foot malformations (bilateral congenital vertical talus and bilateral clubfoot in 2 patients [22%] and arthrogryposis [n=2, 22%]).
The CKD was bilateral in 2 patients (22%), the remaining 7 were unilateral, the right lower limb was affected in 71% of the patients (n=5) and the left in 29% (n=2).
Of the 11 knees included in the study, 6 achieved more than 90° flexion at the time of diagnosis, and 5 fell into the 30°–90° flexion group. Conservative treatment with serial casting was started in 100% of the patients. Of the 5 knees in group 2 (flexion 30°–90°), 4 required quadriceps tenotomy after failing to achieve flexion of 90° after 4 weeks of conservative treatment with casts, and were counted as treatment failure. In one of the cases, despite tenotomy, flexion of more than 90° was not achieved, and therefore V–Y plasty combined with capsulotomy was performed. The mean age at surgery was 24 months (8–60 months), as shown in Table 1.
The mean follow-up was 15 years (minimum 9–maximum 22 years). In terms of functional outcomes, one patient could not be included due to underlying disease (arthrogryposis) he was not a walker and had associated diseases that impaired the knee functionality studies (bilateral congenital hip dislocation, bilateral congenital vertical talus and scoliosis). The mean Lysholm7 score of the 8 walkers (10 knees) was 90.3 points, WOMAC6 pain score 0.4 (0–1), WOMAC stiffness score 1.8 (0–6) and WOMAC function score 3.8 (1–12).
After completion of treatment the range of motion was full for extension (0° extension when the contralateral knee was affected or full extension compared to the healthy contralateral knee) in 9 knees (90%) and for flexion (120° flexion when the contralateral knee was affected or full flexion compared to the healthy contralateral knee) in 4 knees (40%).
On separate analysis of the knees that underwent conservative (n=7, 70%) and surgical (n=3, 30%) treatment, excluding the non-walker patient who underwent surgery, a mean Lysholm score of 92 was obtained in the unoperated knees. The only sequela during follow-up of these patients was a lower limb-length discrepancy due to shortening of the affected lower limb by 1.6cm. In the operated knees, the mean Lysholm7 score was 87, with sequelae or complications being anterior cruciate ligament (ACL) tear in one patient at 13 years of age that did not require surgery, a 1.8cm length discrepancy and one patient who required mobilisation under anaesthesia for mild knee stiffness having undergone percutaneous quadriceps tenotomy 2 years earlier.
No cases of recurrence were reported.
DiscussionThe aim of the present study was to evaluate the functional results and long-term complications of an implemented PCKD, given the lack of therapeutic consensus for a condition as rare as congenital dislocation of the knee.
The classification used by Oetgen et al. for staging the severity of this disease defines 3 grades according to residual congruence of the knee joint on x-ray3:
- -
Grade I, hyperextension with joint continuity.
- -
Grade II, anterior dislocation of the tibia on the femur.
- -
Grade III, anterior and proximal dislocation of the tibia on the femur.
In the protocol described above, plain knee x-rays were not routinely performed, diagnosis in most cases being primarily clinical, as it is very difficult to take radiographs with pure projections in this type of patient (Fig. 4). “Continuous" fluoroscopy was used during cast immobilisation.
The initial treatment decision was made depending on the degree of passive flexion achieved and not achieved according to the initial deformity classification. In the present study, no differences were found with respect to function at the end of follow-up, with good final results in all patients, those who underwent surgery and those who did not, which suggests good selection in the indication and correct follow-up according to the protocol.
The main limitation of this study is the small sample size, and the work must continue to obtain a larger sample so that further differences can be demonstrated.
Comparison with published studies is difficult, as the available series have a small sample size because the disease is so rare, and there are disparities in indications, classifications and surgical techniques.
In their protocol, Rampal et al.4 initially operated on 4 of the 51 knees analysed. As in the present study, the authors opted for conservative treatment by means of physiotherapy, casting, or immobilisation for 7 days with traction, external rotation and flexion, controlling reduction of the tibia with fluoroscopy. Only irreducible type III dislocations and/or failures after conservative treatment were included in the surgical group. In case of intervention, V–Y quadricipital plasty or quadricipital tenotomy was performed with or without arthrolysis and fixation of the dislocation with K-wires. The results were good or excellent in 82% of type I CKDs, good in 68% of type II CKDs and poor in all type III CKDs in the opinion of the authors. A limitation of this study was that functional questionnaires were not included.
Abdelaziz et al.8 proposed a protocol similar to that presented in this study, with the difference that they included percutaneous tenotomy from the outset in diagnosed patients older than 1 month. Of the 21 knees analysed they presented 12 cases with excellent results (57%), 7 cases with good results (33%) and 2 cases with poor results (10%) based on flexion range, extension power, instability and pain. In comparison, in our study 90% achieved full flexion compared to 57% of their cases; none of our patients had pain and only one case had instability due to anterior cruciate ligament tear during long-term follow-up. Their study had a 48-month follow-up, compared to our results with a 15-year follow-up, which shows the future repercussions and complications of treated patients, such as lower limb length discrepancy.
Shah et al.9 studied 8 patients (16 knees) proposing conservative treatment at the outset and minimally invasive quadricipital tenotomy if 90° flexion was not achieved or the tibia was not reduced radiographically over the femur by 6° or 7° by weekly casting. Additionally they performed Achilles tendon tenotomy to reduce equinus, and anterior capsulotomy and lateral retinacular release if the first gesture was not sufficient. Finally, 13 knees were operated (81%), and there were 2 failures at the end of follow-up (12.5%), extension deficit in 5 cases (31%) and 2 fractures due to plastic deformity in the tibia (12.5%). In our protocol, with a much lower surgery rate (36%), we obtained 90% of cases with full extension and no fractures at the end of follow-up.
Oetgen et al.,3 in a study of 7 patients (9 knees) with grade III dislocation who underwent primary surgery, showed good results, comparing quadricepsplasty and femoral shortening, with respect to mobility and functional scales with some long-term instability (follow-up 12+6 years).
Other authors5,10 have proposed percutaneous surgical treatment as an alternative with satisfactory results. Our results coincide with those of Youssef et al.,5 recommending conservative treatment from the outset, leaving surgery for unsatisfactory results. In a study of 13 patients (22 knees), they achieved satisfactory results with conservative treatment in 6 knees, with the remaining 16 cases undergoing surgery and achieving good or excellent results at the end of follow-up. On the other hand, Patwardhan et al.10 evaluated the results of performing percutaneous needle quadriceps tenotomy as a first therapeutic step in a study of 12 patients (20 knees), 9 patients achieving good results and 3 fair results. The present study suggests that treatment from the outset with casting achieves similar results with a less invasive procedure.
Klein et al.2 advocated external fixator treatment as an alternative to surgery in severe cases of type III CKD. They believe that quadricipital or shortening surgery has major complications such as bleeding, scarring, infection or extensor deficits compared to external fixation. It could be an alternative, but not without morbidity.
Tercier et al.11 made modifications to the quadricepsplasty techniques described by Curtis and Fisher, encountering fewer complications and range of motion.
There were only minor complications at the end of follow-up in the present series, suggesting that the protocol implemented provides safe long-term management.
ConclusionsThe existence and application of the protocol for CKD in such a rare condition as congenital knee dislocation suggests good long-term functional results, with few complications and no recurrences.
Correct selection of patients for the different therapeutic decisions is essential for a good result.
Ethical responsibilitiesThe authors declare that they obtained the informed consents of the subjects under study for publication of the data.
Level of evidenceLevel of evidence IV.
Conflict of interestThe authors have no conflict of interests to declare.
Please cite this article as: Salvador Marín J, Miranda Gorozarri C, Egea-Gámez RM, Alonso Hernández J, Martínez Álvarez S, Palazón Quevedo Á. Luxación congénita de rodilla. Protocolo terapéutico y resultados funcionales a largo plazo. Rev Esp Cir Ortop Traumatol. 2021;65:172–179.