To evaluate the functional results of the orthopaedic treatment of midshaft clavicle fractures with a minimum follow-up of 15 years.
Materials and methodsA retrospective study was conducted on 40 patients, mean age 35 years (18–64) with a non-surgically treated clavicle fracture. The mean follow-up was more than 22 years (15–32). The clinical evaluation was performed with the Disability of Arm, Shoulder and Hand score (DASH), Constant Shoulder Score test (CSS), EVA score, and a subjective assessment of the final result. Fractures were classified according to Neer's criteria. The radiological evaluation was performed with an anteroposterior and 45° cephalic anteroposterior oblique X-ray.
ResultsA mean DASH score 2.17 points (0–20.82), the mean CSS score was 98.2 (79–100), the mean EVA score was 0.42 (0–6), and 100% patients were satisfied, with good or excellent results. The control X-ray showed 39 healed fractures (97.5%) with a mean shortening of 6.4mm (0–20).
ConclusionsThe presence of comminution and/or shortening of 15mm or more had the worst functional and radiographic results. Despite this, non-surgical treatment showed excellent functional and radiographic results, and a high personal satisfaction.
Evaluar el resultado funcional del tratamiento ortopédico de las fracturas de tercio medio de clavícula con un seguimiento mínimo de 15 años.
Material y métodosEstudio retrospectivo de 40 pacientes adultos, edad media 35 años (18–64), afectos de fractura de tercio medio clavícula tratadas ortopédicamente con seguimiento medio de 22 años (15–32). La evaluación clínica se realiza con la escala Disabilities of Arm, Shoulder and Hand (DASH), el test de Constant Shoulder Score (CSS), la escala visual analógica (EVA) del dolor y una valoración subjetiva respecto al resultado final. La evaluación radiográfica se realiza mediante proyección anteroposterior (AP) simple y oblicua con 45° de inclinación cefálica.
ResultadosLos resultados de la escala DASH muestran un valour medio de 2,17 sobre 100 (0–20,82), el test de CSS medio es de 98,2 sobre 100, la escala EVA 0,42 sobre 10 (0,6) y el 100% de resultados fueron buenos o excelentes de manera subjetiva por parte de los pacientes. En radiología de control se observan 39 fracturas consolidadas (97,5%) con acortamiento medio de 6,4mm (0–20).
ConclusionesLa presencia de conminución y/o acortamiento igual o mayor a 15mm obtienen peores resultados funcionales de forma estadísticamente significativa. A pesar de ello, el tratamiento ortopédico de las fracturas de tercio medio de clavícula obtiene un buen resultado funcional y radiográfico, y una alta satisfacción subjetiva.
Fractures of the clavicle represent approximately 4% of all fractures and 35% of the fractures of the pectoral girdle.1 Despite their great incidence, there is no consensus about what is the most suitable treatment.
Until a few years ago, conservative treatment was considered the option of choice for the vast majority of fractures. There are currently studies2–6 showing a variety of complications such as a high incidence of delays in consolidation and pseudoarthrosis, loss of function and strength in the upper limb, paresthesias and aesthetic defects. Due to these complications associated with conservative treatments, open reduction and osteosynthesis are nowadays recommended in an ever-greater proportion of fractures of the clavicle.
The complications described with surgical treatment are superficial and profound infections, delays in consolidation, pseudoarthrosis, refractures and hypertrophic scarring, among others.7–11
The study hypothesis is that orthopaedic treatment of midshaft fractures of the clavicle offers a satisfactory long-term functional and radiographic outcome.
Materials and methodsRetrospective observational study of patients diagnosed as having a midshaft fracture of the clavicle at our hospital centre between 1979 and 1994 and treated orthopaedically. The inclusion criteria were: midshaft fracture of the clavicle in patients over 18 and under 65 years of age, with a minimum follow-up of 15 years. The exclusion criteria were: surgical intervention on a fracture of the clavicle, bilateral fracture of the clavicles, associated chest trauma, patients currently deceased, absence of the initial X-ray from the case history, patients with degenerative neurological diseases and little ability to collaborate or refusal to participate in the study.
Surgical treatment was initially indicated in those patients with midshaft fractures of the clavicle displaced by more than 20mm or with severe associated comminution. The kind of stabilization used depended on the preferences of the main surgeon. Nowadays we tend to operate surgically on more clavicle fractures than in the past, as the current decision-tree protocol used at our department includes a larger number of fractures in the surgical area. Fractures with smaller displacements and less comminution are included, and more operations are performed on young patients of employment age or sports people requiring a speedy return to their habitual activities.
According to the hospital statistics, 212 midshaft fractures of the clavicle were diagnosed and treated during this period. Of these, 44 met the inclusion and exclusion criteria. Finally, 40 completed the study (4 patients declined to take part in it when they were contacted by telephone, arguing that the injury occurred a long time ago and they were currently asymptomatic).
Fractures were deemed to be comminuted if there were more than 3 fragments greater than 1cm each.
The orthopaedic treatment applied consisted in immobilization with a sling or a figure of 8 bandage for 4–6 weeks until radiographic consolidation of the fracture, followed by rehabilitation for an average of 4 weeks.
Information was recorded on gender, age, follow-up time, location and dominance, after obtaining the informed consent of the subjects who agreed to take part in the study.
Fractures were assessed from a functional perspective using the Disabilities of Arm, Shoulder and Hand (DASH) scale, with scores ranging from 0 (best result) to 100 (worst result). This scale assesses the subjective ability to perform multiple activities of daily life, the intensity of symptoms, and the impact on the patient's working and sporting life. The Constant Shoulder Score (CSS) test gives a score between 8 (worst result) and 100 (best result). It assesses the presence of pain, the ability to perform certain activities and, objectively, the active mobility of the shoulder and its strength with respect to the contralateral shoulder. The visual analogue scale (VAS) rates pain between 0 (absence of pain) and 10 (maximum pain possible) and, finally, a nominal subjective valuation of the patient's final outcome (poor, so–so, good or excellent).
The questionnaires and the clinical and radiological examinations were performed at our hospital centre at the end of the follow-up, during the months of April and May, 2010.
The radiological study comprised simple and oblique anteroposterior (AP) X-rays of both clavicles with a 45° cephalic inclination, assessing the consolidation of the fracture and the degree of shortening with respect to the healthy clavicle.
The database and statistical analyses were performed using SPSS® v.18.0 software (SPSS Inc., Chicago, IL, USA), with values of p<0.05 being considered significant.
ResultsThe patients meeting the inclusion and exclusion criteria numbered 40, all of whom suffered a unilateral midshaft fracture of a clavicle with conservative treatment between 1979 and 1994, The patients were 23 males (57.5%) and 17 females (42.5%) with a mean age of 35.1 years (18–64), with a mean follow-up time of 22.1 years (15–32); the fractures were 21 on the right side (52.5%), 19 on the left side (47.5%), with 22 in the dominant limb (55%) and 18 in the non-dominant limb (45%).
A total of 9 comminuted fractures were observed (22.5%). All of them corresponded to medium- or high-energy fractures following traffic accidents (33.3%), sports accidents (55.6%) or work-related accidents (11.1%).
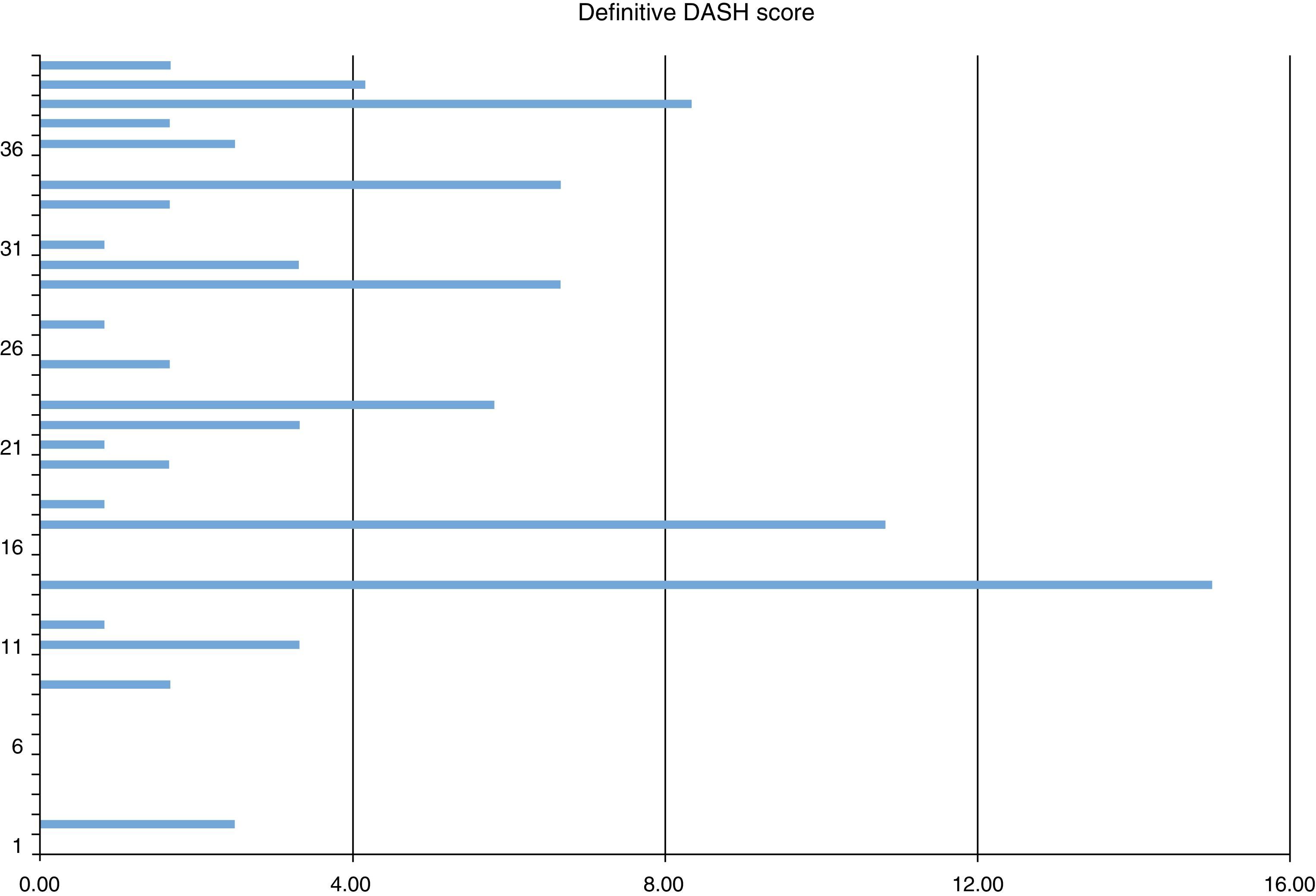
The mean functional outcome on the DASH scale was 2.17 (0–20.82) (Fig. 1); the mean CSS test score was 98.2 (79–100); the mean VAS score was 0.42 (0–6); and the definitive subjective valuation of the final outcome obtained was good in 2 patients (5%) and excellent in 38 patients (95%).
Bone consolidation was achieved in 39 cases (97.5%) and one case of comminuted fracture of the clavicular diaphysis evolved to pseudoarthrosis. In order to evaluate this consolidation, the last radiological study described (the presence or absence of bony bridges between the two clavicular fragments) was examined along with the absence of mobility on the focus of the fracture by means of the physical exploration effected by a single surgeon during the examination conducted for the study. There were no associated complications following the cure, except for the final shortening observed.
In the case of the pseudoarthrosis, which coincided with the case with the greatest shortening (20mm) and associated comminution, surgical treatment was proposed but the patient rejected it out of phobia. The same conservative treatment was applied as in the protocol described above. He is now able to engage in his previous work activity without any problems and controls the occasional mild discomfort with analgesia on demand (2–3 days a month) (Fig. 2).
The mean shortening was 6.4mm (0–20) with respect to the healthy clavicle. In 5 cases the shortening was equal to or greater than 15mm. The results on the DASH and VAS scales tested in these 5 patients are lower than in the group with less than 15mm of shortening, a statistically significant result (p<0.05) (Table 1), except for the CSS test that showed no differences (p>0.05).
The 9 patients with comminuted fractures present a significant reduction on the DASH scale, but not on the other scales evaluated (Table 2).
No clinical alterations were seen during the physical examination of the acromioclavicular joint in any of the cases. Radiologically, cases of ipsilateral acromioclavicular arthrosis were observed in 33 cases, and contralateral acromioclavicular arthrosis in 29 cases, coinciding with the eldest patients.
DiscussionFractures of the clavicle have classically been candidates for conservative treatment in view of the good results obtained, regardless of the initial shortening or comminution. Studies such as those by Rowe12 and Neer13 have shown worse results with surgical treatment and pseudoarthrosis in less than 1% with conservative treatment, so the latter has been considered the treatment of choice for some time. More recent studies have continued to corroborate this option, with good definitive outcomes.14
The type of conservative treatment used (figure of eight bandage or sling) showed no differences in the rate or time of consolidation, although the sling was shown to be more comfortable and was associated with fewer neurovascular complications.15
Currently, however, several studies2–6,16,17 have highlighted complications with this option in a higher percentage than that published to date. Most refer to delays in consolidation and pseudoarthrosis, loss of function and strength in the ipsilateral shoulder, paresthesias and even an aesthetic defect. Significant shortening and the presence of comminution at the focus of the fracture were considered as factors indicative of a poor prognosis3,9,10,18 in the short and medium term. In addition, fractures of the medial and distal third undergo greater torsion stresses so the reduction to be achieved has to be more precise. For all these reasons, initial treatment nowadays tends to be more aggressive.
Our study describes the clinical and functional results in patients who suffered a conservatively treated fracture of the clavicle and were followed up for more than 22 years. This allows us to observe their current status and if there are any sequelae associated with the application of this treatment after such a long time.
Today, the absolute indications for surgical treatment are considered to be those fractures presenting an initial shortening of greater than 15–23mm (depending on the author consulted), comminuted fractures and fractures with a third fragment displaced in the Z axis.19,20 Female gender and advanced age are relative indications.11
Several methods of surgical treatment, such as external fixation, endomedullary pinning, osteosynthesis plates, Kirschner needles, cannulated screws or elastic titanium needles have been proposed. The choice between one and another has been justified in terms of the type of fracture and the surgeon's preferences, although the most popular surgical treatment is osteosynthesis using a low-profile anatomical plate. This system has provided good functional outcomes and a low incidence of pseudoarthrosis.6,21
In all the cases treated surgically, the good outcome rates achieved have been close to 95–100%. Various recent studies3,4,9–11,18,19 have compared 2 different treatment groups (conservative versus surgical) in displaced fractures of the clavicular diaphysis and have observed higher short-term scores in patients treated surgically, as well as a shorter consolidation time, greater functionality and satisfaction, and even a lower definitive cost of treatment. As time goes by, in the medium term, the results tend not to show any great variation between the two groups and they may even be the same in some cases.5,22
This surgical treatment is not without complications: some studies6–8,11,21,22 have reported an incidence of up to 35%, mostly superficial infections, delays in consolidation, pseudoarthroses, refractures or discomfort with the osteosynthesis material.
There are no studies on the long-term outcomes of surgical treatment such as in the present paper, with most studies showing periods of less than 10–15 years of follow-up.23–25
The results of our series show that surgical treatment achieved excellent objective and subjective functional outcomes with follow-up in excess of 22 years. The conservative treatment applied in clavicular fractures with less than 15mm of shortening and the presence of a single focus for the fracture, without comminution, has resulted in an excellent definitive clinical outcome. Only in cases with more than 15mm of shortening and the presence of comminution is there a worse final functional outcome, although this is also satisfactory for patients and has not prevented the practice of a totally normal life without limitations on their physical or work-related activities.
The fact that differences have been observed on the DASH scale and not on the CSS test is attributed to the low number of patients included in the present study. A trend towards a statistically significant difference has been observed between the outcomes of both groups in all the questionnaires and on the VAS although, as we explained earlier, this does not entail any disability or other unsatisfactory results for patients.
This study has certain limitations: it is a non-randomized retrospective study on a sample of 40 patients with a midshaft fracture of the clavicle with certain specific characteristics. In most cases, it was opted to apply a conservative treatment since they were fractures with scant shortening and no comminution. Even so, they include 5 cases with greater shortening in which a surgical approach was proposed but the patients in question rejected this for personal reasons. In addition, 5 cases were lost to the follow-up because they did not wish to take part in the study on the grounds that the lesion occurred a long time ago and they do not currently wish to go to hospital to perform any tests as they are asymptomatic.
Nonetheless, our paper describes the result of a series of fractures of the clavicle all treated conservatively and with a long follow-up not previously seen in any other paper in the scientific literature.
ConclusionsOn the basis of the statistical analysis, we can conclude that the long-term outcome of orthopaedic treatment of fractures of the clavicle is very acceptable for both patients and professionals. There is, however, a slight statistically significant difference with a trend towards worse outcomes, albeit still acceptable, in cases of fractures with initial shortening in excess of 15mm or comminution at the focus of the fracture.
It would be necessary to conduct a comparative study between patients treated orthopaedically and those treated surgically on fractures with similar characteristics (shortening of more than 15mm and/or presence of comminution at the fracture focus) in order to be able to establish priorities for one or other treatment in these fractures.
Level of evidenceLevell of evidence III.
Ethical responsibilitiesProtection of persons and animalsThe authors declare that no experiments have been conducted on human beings or on animals for this research.
Data confidentialityThe authors declare that no patient details appear in this article.
Right to privacy and informed consentThe authors declare that no patient details appear in this article.
Conflict of interestThe authors have no conflict of interests to declare.
Please cite this article as: Sirvent-Díaz E, Calmet-García J, Capdevila-Baulenes J. Fracturas de clavícula tratadas conservadoramente tras 22 años de seguimiento: resultados funcionales y estéticos. Rev Esp Cir Ortop Traumatol. 2014;58:108–113.