Pigmented villonodular synovitis (PVS) is a synovial proliferation disorder of uncertain aetiology, with some controversy as regards its proper treatment. The purpose of the study was to evaluate the functional outcome and recurrence rate in a series of patients diagnosed with both the diffuse and the localised types of PVS and treated by arthroscopic resection.
Material and methodsTwenty-four patients diagnosed with PVS were retrospectively assessed. There were 11 cases with the diffuse type, and 13 cases with the localised type of PVS. They were followed-up for a median of 60 months (range, 34–204). They underwent arthroscopic synovectomy, and were functionally evaluated with IKDC, WOMET, and Kujala scores.
ResultsThere was recurrence in 8 out of 13 (61.5%) cases with the diffuse type of PVS. Two of these patients were treated with radiation. One patient underwent surgical resection with an open procedure due to extra-articular involvement. The remaining 5 patients underwent a second arthroscopic resection, and no recurrence was subsequently observed. Cases with localised PVS did not recur after a single arthroscopic resection. IKDC, WOMET and Kujala scores improved by 30.6, 37.4 and 34.03 points, respectively.
DiscussionPigmented villonodular synovitis treated by arthroscopic resection showed good functional results at mid-term follow-up. A single arthroscopic resection was sufficient to treat the localised PVS, whereas the diffuse type of PVS required a second arthroscopic resection in most cases, due to its high rate of recurrence.
La sinovitis villonodular pigmentaria (SVP) es un trastorno de la proliferación sinovial de etiología incierta, con un tratamiento controvertido. El objetivo del estudio es valorar los resultados funcionales y la tasa de recurrencia en una serie de pacientes diagnosticados de SVP de rodilla, tanto en su forma difusa como en su forma localizada, tratados mediante resección artroscópica.
Material y métodosEstudio retrospectivo de 24 pacientes diagnosticados por resonancia magnética de SVP local/difusa entre 1996 y 2011. Se trataron 11 casos de forma localizada y 13 de forma difusa. Tras un seguimiento medio de 60 meses (rango: 34-204). Se intervinieron mediante sinovectomía artroscópica y se valoraron funcionalmente en el postoperatorio con los test IKDC, WOMET, Kujala y Tegner.
ResultadosOcho pacientes afectados de SVP difusa recidivaron (un 61,5% de las formas difusas). De ellos 2 requirieron radioterapia, uno cirugía abierta por afectación extraarticular y 5 nueva resección artroscópica sin detectarse posteriormente nueva recidiva. En 6 pacientes se observaron lesiones asociadas (en 3 meniscopatía y en 3 lesiones condrales). No hubo recidivas en la forma localizada. El IKDC mejoró de media 30,6 puntos, el WOMET 37,4 puntos y Kujala 34,03 puntos.
DiscusiónLa SVP resecada mediante técnica artroscópica presenta buenos resultados funcionales y curativos a medio plazo con una baja morbilidad. La forma difusa de la SVP requiere con frecuencia una segunda intervención quirúrgica por su alta tasa de recidiva tras su resección artroscópica.
Pigmented villonodular synovitis (PVNS) is a disease of the synovial membrane characterised by the proliferation of mononuclear cells. It is an infrequent and benign entity, which typically affects the knees of young adults (<40 years).1
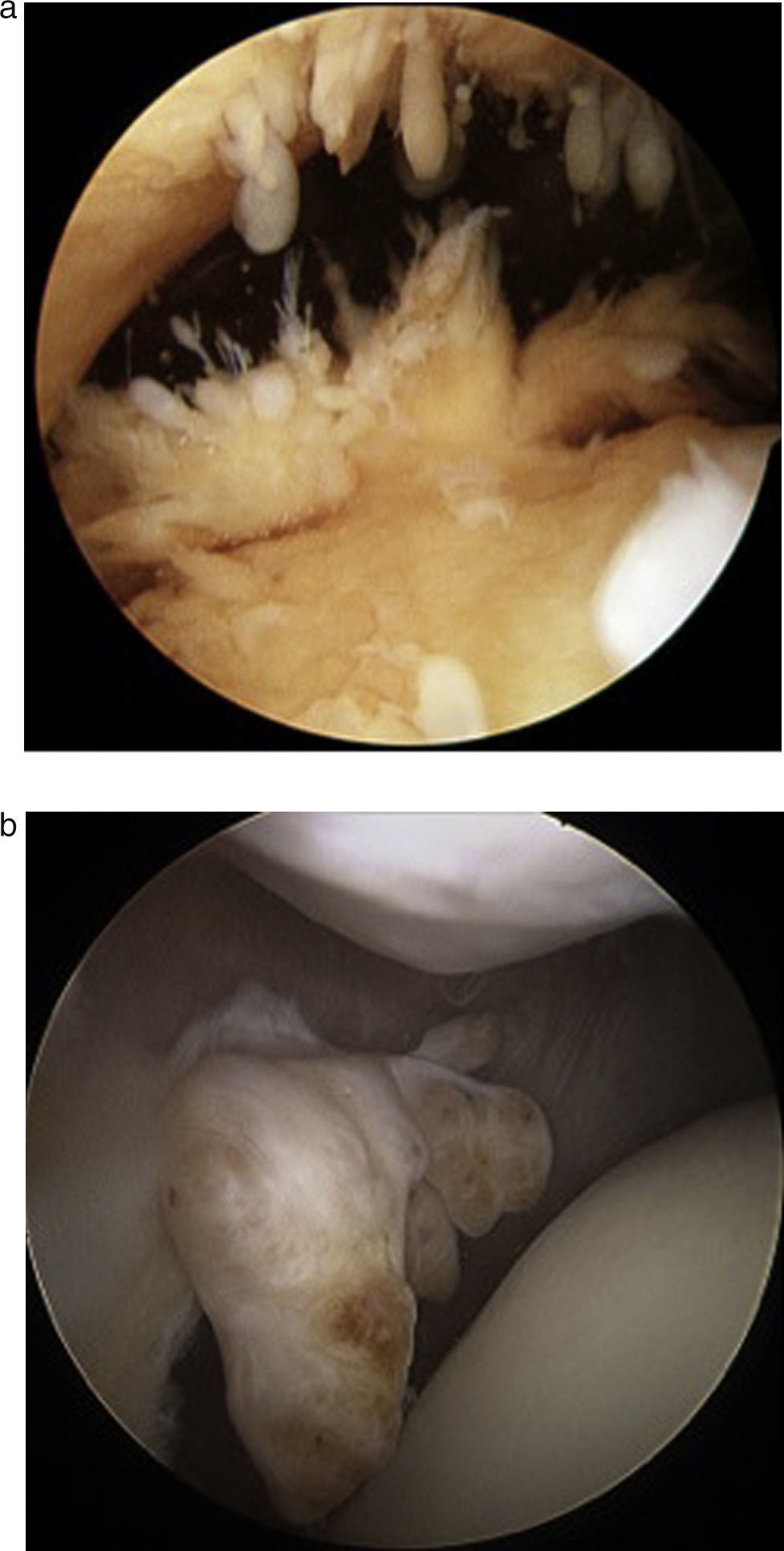
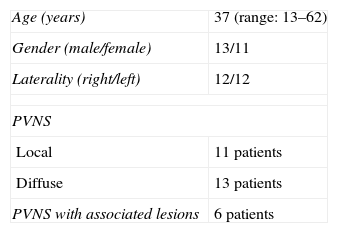
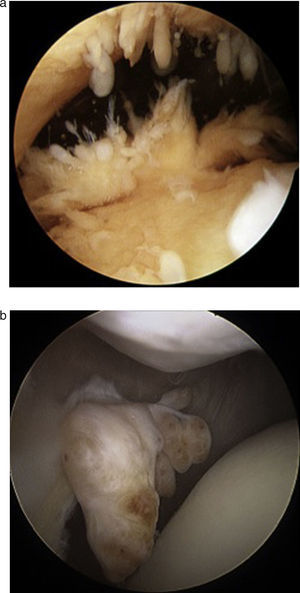
The literature distinguishes 2 forms of presentation of PVNS, diffuse (DPVNS) (Fig. 1a) and localised (LPVNS) (Fig. 1b). The localised form is characterised by lobular and pendulous lesions from the synovium, which usually present in the femoropatellar region. On the other hand, DPVNS is characterised by involvement of all or most of the joint synovium.2
Although the treatment of PVNS is generally considered to consist in a full excision of the affected synovium, there is no consensus regarding the surgical technique to employ. While some authors advocate resection through open surgery,1–6 others report similar rates of recurrence through total arthroscopic synovectomy.3,7–9 Arthroscopic synovectomy enables a better preservation of knee functionality, with few complications, and an acceptable rate of recurrence, although the latter could depend on the form of PVNS. Complementary therapies with external radiotherapy or isotopic synoviorthesis have been proposed as alternatives in partial or incomplete resections as coadjuvant treatment, with the aim of improving local disease control. There have been no reports of success with a second surgical resection upon recurrence of PVNS.2–14
The objective of this study was to evaluate the functional results and rate of recurrence in a series of patients diagnosed with PVNS, both the diffuse and localised forms, who were treated though arthroscopic resection.
Material and methodsWe selected patients diagnosed with PVNS between the years 1996 and 2011 out of a database including all patients who underwent knee surgery through an arthroscopic technique at our centre.
The inclusion criteria were: (1) patients with knee pain; (2) full preoperative study with a presumptive diagnosis of PVNS by magnetic resonance imaging (MRI); (3) intervened through arthroscopic technique; (4) with confirmation of PVNS by pathological anatomy; and (5) with a monitoring period over 24 months.
We excluded patients with intraosseous PVNS lesions.
A total of 6006 knee arthroscopies were conducted at our centre between 1996 and 2011. Of these, 24 (0.4%) fulfilled the inclusion criteria of our study. A total of 6 cases (0.1%) were excluded due to intraosseous lesions. The group of patients presented a median follow-up period of 60 months (range: 34–204 months) with no losses during follow-up. The demographic results are shown in Table 1. A total of 13 patients suffered DPVNS, while the remaining 11 presented LPVNS, all of them diagnosed intraoperatively. Out of these cases, 7 presented lesions in the posterior compartment of the knee, whilst the 4 remaining patients did so in the femoropatellar compartment.
For each patient we registered the clinical and functional condition, both preoperatively and during the last postoperative assessment, using the IKDC test,15 Western Ontario Meniscal Evaluation Tool (WOMET)16 (assessment scale for meniscal involvement, evaluating physical and recreational symptoms, lifestyle and emotions), Kujala17 (subjective and functional evaluation test for patellofemoral conditions) and Tegner test.18 The range of mobility obtained in each case was also recorded.
Radiographic assessmentPatients underwent a radiographic study through telemetric radiography of the lower limbs under load, a profile radiograph, an axial radiograph of the patella and a Rosemberg projection (posteroanterior at 45° flexion, under load) of both knees in the preoperative period, at 6 months and at 2 years postoperatively, always following the same protocol. We used the Ahlbäck classification to study the grade of arthrosis, both in the preoperative telemetric radiographs and in the control images obtained 2 years after the intervention. In addition, we obtained an MRI scan of the affected knee, in order to diagnose the lesion and its location during the preoperative period (Fig. 2).
Surgical techniqueAll the interventions were conducted by 4 surgeons specialising in the knee, through 4 routine arthroscopic portals: 2 anterior (anterolateral and anteromedial) to access the femoropatellar compartment and 2 posterior (posterolateral and posteromedial) to access the posterior compartment. A total synovectomy was performed with a 5.5mm incisional terminal (Gator, ConMed Linvatec, Largo, FL, USA) in oscillating mode, and any existing associated lesions were treated. We also obtained a biopsy of synovial tissue in all cases, placing a number 10 intraarticular drainage for the first 24h.
In the postoperative period, we established prophylaxis with low molecular weight heparin for a period of 15 days, along with a rehabilitation protocol which enabled full load on the limb and muscular strengthening according to tolerance.
Associated lesionsIn our series, 6 (25%) patients presented associated lesions, diagnosed through the preoperative MRI scan: 3 of them suffered meniscopathy and 3 chondral lesions. The meniscopathies affected the medial compartment. One was treated through suture and the other 2 through a partial meniscectomy. Regarding the chondral lesions, 2 were grade III and were treated through microfractures, whilst the third was a grade IV at the level of the trochlea, and did not require any treatment. The postoperative controls did not show any worsening of the associated lesions or any arthritic changes in the radiographs.
Pathological anatomyThe analysis was conducted by an anatomopathologist specialising in musculoskeletal tumours. In all cases, the diagnosis was obtained after observing the presence of villi and brown nodules formed by groups of histiocytes with a fibrous stroma, deposits of hemosiderin, giant cells and foam cells7 in the intraoperative sample.
Statistical analysisThe categorical variables were described through frequencies and percentages, whereas the quantitative variables were described using the mean and standard deviation or the median and 25 and 75 percentiles. The pre- and postoperative differences between patients in the IKDC, WOMET, Kujala and Tegner tests were described using a nonparametric Wilcoxon test, whilst the differences in the presence of associated lesions were analysed using the Mann–Whitney U test. We considered as statistically significant values of P<.05 and the statistical analysis was carried out with the statistics software package SPSS 18.0 (SPSS Inc., Chicago, IL, USA).
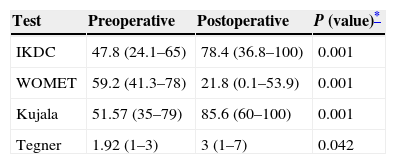
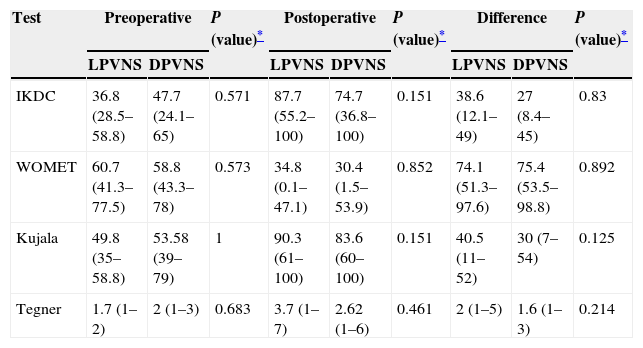
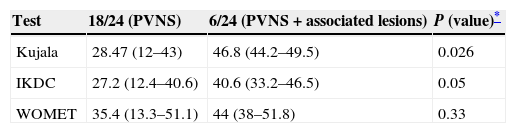
ResultsFunctional resultsThe results of the functional test revealed an improvement of 30.6 points in the IKDC (P=.001), 37.4 points in the WOMET (P=.001) and 34.03 points in the Kujala (P=.001) (Table 2) tests for the overall series of patients. No differences were found in any of the tests after the sample of patients was divided into those suffering LPVNS and DPVNS (Table 3). When studying the results divided into 2 groups (patients with PVNS and patients with PVNS plus associated disease), we observed a greater improvement in the IKDC of 40.6 points (P=.05) and in the Kujala of 46.8 points (P=.026) among those presenting concomitant diseases (Table 4).
Test results in the preoperative and postoperative periods.
| Test | Preoperative | Postoperative | P (value)* |
|---|---|---|---|
| IKDC | 47.8 (24.1–65) | 78.4 (36.8–100) | 0.001 |
| WOMET | 59.2 (41.3–78) | 21.8 (0.1–53.9) | 0.001 |
| Kujala | 51.57 (35–79) | 85.6 (60–100) | 0.001 |
| Tegner | 1.92 (1–3) | 3 (1–7) | 0.042 |
Results of the test in preoperative period, postoperative period and mean thereof in LPVNS and DPVNS.
| Test | Preoperative | P (value)* | Postoperative | P (value)* | Difference | P (value)* | |||
|---|---|---|---|---|---|---|---|---|---|
| LPVNS | DPVNS | LPVNS | DPVNS | LPVNS | DPVNS | ||||
| IKDC | 36.8 (28.5–58.8) | 47.7 (24.1–65) | 0.571 | 87.7 (55.2–100) | 74.7 (36.8–100) | 0.151 | 38.6 (12.1–49) | 27 (8.4–45) | 0.83 |
| WOMET | 60.7 (41.3–77.5) | 58.8 (43.3–78) | 0.573 | 34.8 (0.1–47.1) | 30.4 (1.5–53.9) | 0.852 | 74.1 (51.3–97.6) | 75.4 (53.5–98.8) | 0.892 |
| Kujala | 49.8 (35–58.8) | 53.58 (39–79) | 1 | 90.3 (61–100) | 83.6 (60–100) | 0.151 | 40.5 (11–52) | 30 (7–54) | 0.125 |
| Tegner | 1.7 (1–2) | 2 (1–3) | 0.683 | 3.7 (1–7) | 2.62 (1–6) | 0.461 | 2 (1–5) | 1.6 (1–3) | 0.214 |
DPVNS, diffuse pigmented villonodular synovitis; LPVNS, localised pigmented villonodular synovitis.
Mean results of the test comparing patients only with PVNS vs patients with PVNS plus associated lesions.
| Test | 18/24 (PVNS) | 6/24 (PVNS+associated lesions) | P (value)* |
|---|---|---|---|
| Kujala | 28.47 (12–43) | 46.8 (44.2–49.5) | 0.026 |
| IKDC | 27.2 (12.4–40.6) | 40.6 (33.2–46.5) | 0.05 |
| WOMET | 35.4 (13.3–51.1) | 44 (38–51.8) | 0.33 |
PVNS, pigmented villonodular synovitis.
There was no extension deficit in any case and the final mean flexion observed was 127° (range: 120–140°). No preoperative or postoperative complications were noted in relation to the surgical technique, such as deep vein thrombosis, infection, rigidity or haemarthrosis.
Radiographic resultsWhen the radiographs were analysed by means of the Ahlbäck classification in patients suffering PVNS, no significant arthritic changes were observed comparing the preoperative radiographs with those at the end of the monitoring period, neither in cases of LPVNS nor cases of DPVNS (P=.001).
Disease recurrenceIn total, 8 of the 24 patients (33%) presented recurrence of PVNS, with a mean period of 56.9 months (range: 23–168 months) between the first intervention and the recurrence. All the cases corresponded to the diffuse form of PVNS. Two of them underwent external radiotherapy, 5 underwent an arthroscopic resection and another case underwent open surgery through a posterior access route (Trickey approach) to complete the resection of the diseased tissue affecting the extraarticular region of the popliteal space. Until the last control, patients in this group were asymptomatic both clinically and radiographically after a minimum follow-up of 21 months after recurrence.
DiscussionThe main finding of this study was that a single arthroscopic resection in the localised form of PVNS produced good functional results and a medium-term cure. However, the percentage of patients who presented disease recurrence in the diffuse form was considerably high. In any case, the association of a second arthroscopic resection or some other coadjuvant procedure in such cases managed to control the disease, at least in the short term, in 87.5% of the patients. Likewise, after a mean follow-up period of 5 years, De Ponti et al.8 observed that the risk of recurrence was 20% in the case of DPVNS treated through arthroscopic technique with no adjuvant treatment. In addition, Zvijac et al.9 reported a 14% rate of recurrence of DPVNS in patients treated arthroscopically after a mean follow-up period of 3.5 years.
On the other hand, Colman et al.19 studied the risk of recurrence of DPVNS with different techniques and observed a lower recurrence with the mixed technique (arthroscopic/open) compared to the arthroscopic or isolated open alternative: 9% vs 62% vs 64%, respectively. Flandry et al.4 reported a series of patients operated through open technique with multiple approaches in which they only found 2 recurrences in a group of 23 patients with a mean follow-up period of 58 months.
There have also been reports of deficits in postoperative mobility. The studies by Johansson et al.5 and Flandry et al.4 observed a limitation of the range of movement in knees operated through open technique, with a mean 0–15° extension and 90–130° flexion, in 24% and in 50% of patients, respectively. On the other hand, the present study observed that resection through an arthroscopic technique resulted in full extension in all cases and a mean flexion of 127°.
From the standpoint of functional scales, we observed an improvement regardless of whether the patients suffered DPVNS or LPVNS. Gu et al.20 compared DPVNS treated arthroscopically vs open surgery and saw an improvement in IKDC from a mean 56.3 points preoperatively to 89.4 points 3 years after the surgery in patients treated arthroscopically (P<.001) and from a mean 58.2 points in the preoperative period to 72.1 points 3 years after the intervention among those treated by an open technique (P<.001). In the present work, we also observed a functional improvement in that scale, which went from 47.8 to 78.4 points. Similarly, the study by Aurégan et al.21 noted good functional results and levels of activity with significant improvements, without finding any differences between LPVNS and DPVNS.
One of the worst consequences of PVNS is early degenerative changes in otherwise healthy and young patients. Flandry et al.4 reported a 48% rate of advanced degenerative changes following open synovectomy. During the monitoring period of patients included in the present study, we did not observe any cases with advanced arthrosis secondary to the intervention. This could be attributed to the arthroscopic technique, which is obviously less invasive and aggressive.
The main limitation of the present work lies in being an observational and retrospective study with a limited sample of patients and without a control group of patients who had undergone open surgery, with a median of 60 months follow-up.
ConclusionPVNS resected through an arthroscopic technique presents good functional and curative results in the medium term, along with low morbidity. The diffuse form of the PVNS often requires a second surgical intervention, due to its high rate of recurrence following arthroscopic resection.
Level of evidenceLevel of evidence IV.
Ethical responsibilitiesProtection of people and animalsThe authors declare that this investigation did not require experiments on humans or animals.
Confidentiality of dataThe authors declare that this work does not reflect any patient data.
Right to privacy and informed consentThe authors declare that this work does not reflect any patient data.
Conflict of interestsThe authors have no conflict of interests to declare.
Please cite this article as: Isart A, Gelber PE, Besalduch M, Pelfort X, Erquicia JI, Tey-Pons M, et al. Alta recidiva y buenos resultados funcionales tras la resección artroscópica de la sinovitis villonodular pigmentaria de la rodilla. Rev Esp Cir Ortop Traumatol. 2015;59:400–405.