The treatment of trapeziometacarpal osteoarthritis through the implantation of total trapeziometacarpal prostheses is in continuous expansion. The Isis® prosthesis is a trunk-conical threaded anchorage prosthesis. Our objective was to assess the functional results and survival of this implant for at least one year of follow-up.
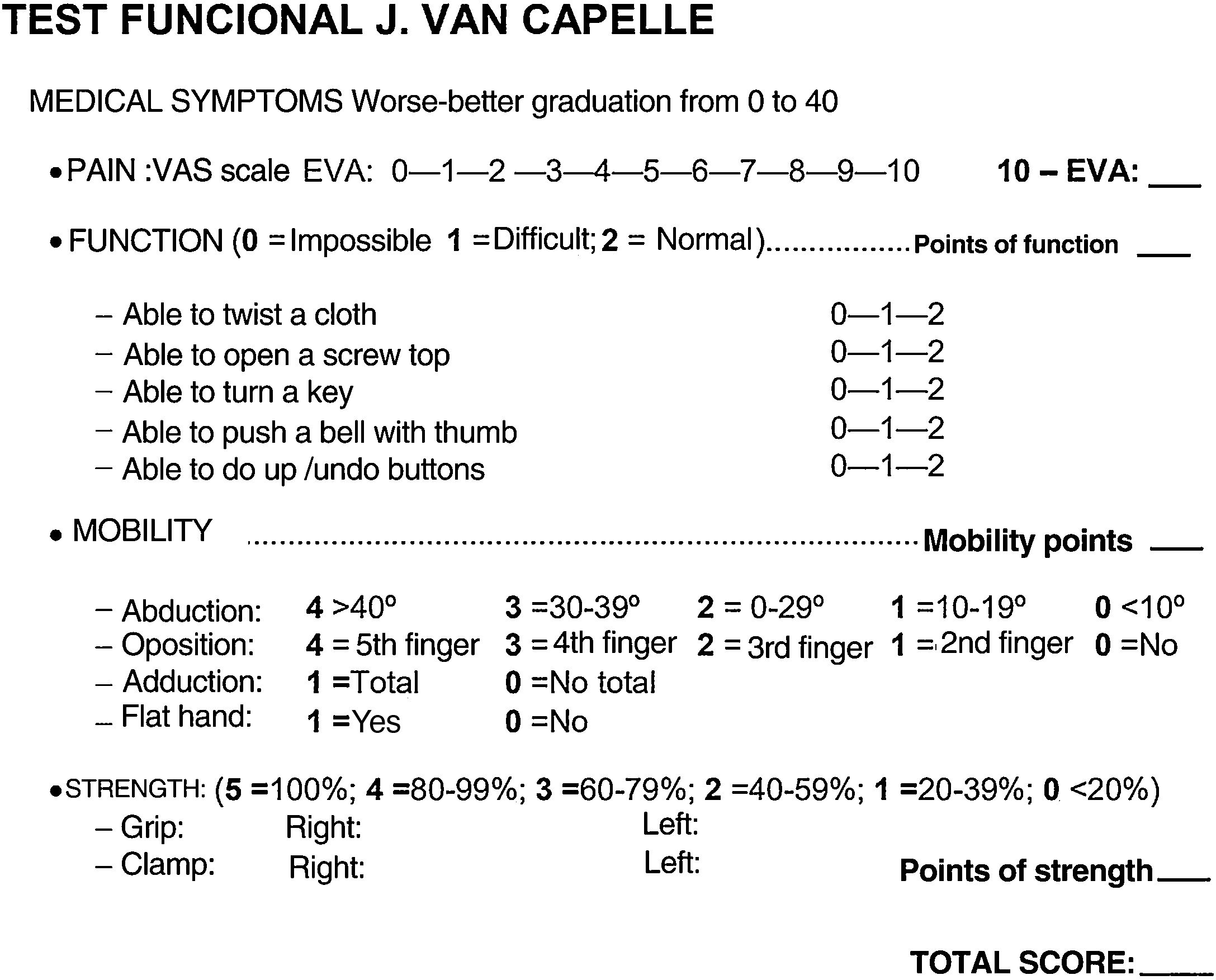
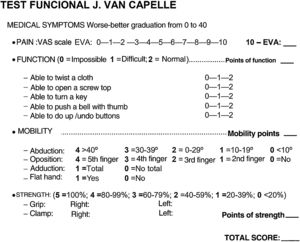
Material and methodProspective study on 53 Isis® prosthesis, implanted from April 2014 to January 2019. The Van Cappelle functional test, pain, strength, mobility, return to previous activity, radiological variables and placement of the trapezial component were evaluated. The surgical technique was performed with a guide wirefocused on the trapezius and control of the scopia. Observed complications were recorded and statistical analysis was performed.
ResultsFifty-one implants (49 patients) were reviewed. Mean follow-up was 2.1 years (1–5.7). Van Cappelle’s test, pain, mobility, and grip and clamp strength improved significantly, as did the distance between the metacarpal head and the trapezius base; 96% of the patients returned in less than 6 months to their activities. Minor complications, 3 De Quervain’s tendinopathy and 2 intra-operative metacarpal and 2 trapezium fractures were recorded, and one carpal tunnel syndrome. There was no dislocation, mobilization, or implant infection.
ConclusionsThe functional results of the Isis® prosthesis are excellent in the short term, far exceeding the first year of 100% of survival. The complications that arose were minor and few. The anchorage and placement of the trapezial component guided by scopia seem to be crucial for the good result.
El tratamiento de la rizartrosis del pulgar mediante la implantación de prótesis totales está en continua expansión. La prótesis Isis® es un implante de cúpula troncocónica de anclaje roscado y semiconstreñida. Nuestro objetivo fue valorar los resultados funcionales y de supervivencia de este implante durante un mínimo de un año de evolución.
Material y métodoEstudio prospectivo sobre 53 prótesis Isis® implantadas entre abril de 2014 y enero de 2019. Se evaluaron el test funcional de Van Cappelle, dolor, fuerza, movilidad, regreso a la actividad, variables radiológicas y colocación de la cúpula. La técnica quirúrgica se realizó siempre con aguja guía centrada en el trapecio y control de escopia. Se registraron complicaciones y se llevó a cabo un análisis estadístico.
ResultadosSe revisaron 51 implantes (49 pacientes) con un seguimiento medio de 2,1 años (1–5,7). El test de Van Cappelle, el dolor, la movilidad y la fuerza de puño y pinza mejoraron significativamente; también la distancia entre cabeza de metacarpiano y base de trapecio. El 96% de los pacientes regresaron en menos de 6 meses a sus actividades. Las complicaciones registradas fueron: 3 tendinopatías de De Quervain, 2 fracturas de metacarpiano y 2 de trapecio intraoperatoriamente, y un síndrome del túnel carpiano. No hubo ninguna luxación, infección ni movilización del implante en el último seguimiento.
ConclusionesLos resultados funcionales de la prótesis Isis® son excelentes a corto plazo, con una supervivencia del 100% tras el primer año de evolución. Las complicaciones surgidas fueron escasas. El anclaje y colocación de la cúpula guiada por escopia parecen ser cruciales para el buen resultado.
Trapeziometacarpal osetoarthritis is a degenerative, limiting disease assiduously faced by hand surgery specialists.1 Patients demand effective, long-lasting treatment once standard conservative treatments have failed. The surgeon should offer an option to restore a joint which is mobile, strong and painless.2 In recent years total trapeziometacarpal prostheses have had highly satisfactory functional outcomes, especially during the first months of evolution, compared with standard treatments such as trapeziectomies with suspension and interpositioning.3,4 With regard to long-term outcomes, the complication which presented with first generation cemented prostheses are being overtaken by the development of second generation prostheses with more anatomical designs and osteointegration contact surfaces, such as porous titanium or hydroxyapatite.5,6 Improvement of the implantation technique, and intraoperative scopia as a guide for cup orientation has also helped to improve the reduction of the major complications of these implants: dislocation and mobilisation.7,8 Load support capacity in medium and light activities and a fast recovery has made this a very attractive option for these patients, whose mean age is usually between 55/60 years, an age when fast functional outcomes are required.
Many models have been developed in recent years, with spherical cups or impacted trunk-conical cups, dual mobility or threaded cups.9
The Isis trapeziometacarpal prosthesis® is a direct evolution of the cementless prosthesis from the Guepar Group.10,11 The main differentiating characteristic from other models is its threaded anchorage cup. There are very few references in the literature regarding the outcomes of this implant.12
The objective of our study was to assess survival during the first few years and the clinical and radiological outcomes of the Isis trapeziometacarpal prosthesis®.
Material and methodA prospective, longitudinal observational study conducted on a consecutive case series at the Hand Unit of our hospital, on primary Isis® trapeziometacarpal implants (Evolutis, Roanne, France) which were implanted from April 2014 to January 2019. The study included patients diagnosed with initial grade III or IV (scaphortrapeziotrapezoid impingement, with no clear bone contact) thumb base rhisarthrosis,13 according to the Easton classification. They were functionally active, with at least one year of postoperative follow-up and had been implanted with a cementless, threaded cup, modular neck and semi-constrained Isis® prosthesis. Patients who met clinical criteria but had a trapezium height under 8 mm, with an intense load activity or evolved grade IV rhisarthrosis of the thumb base were excluded from prosthesis implant. Preoperative and annual postoperative variables were collected in a protocolised manner.
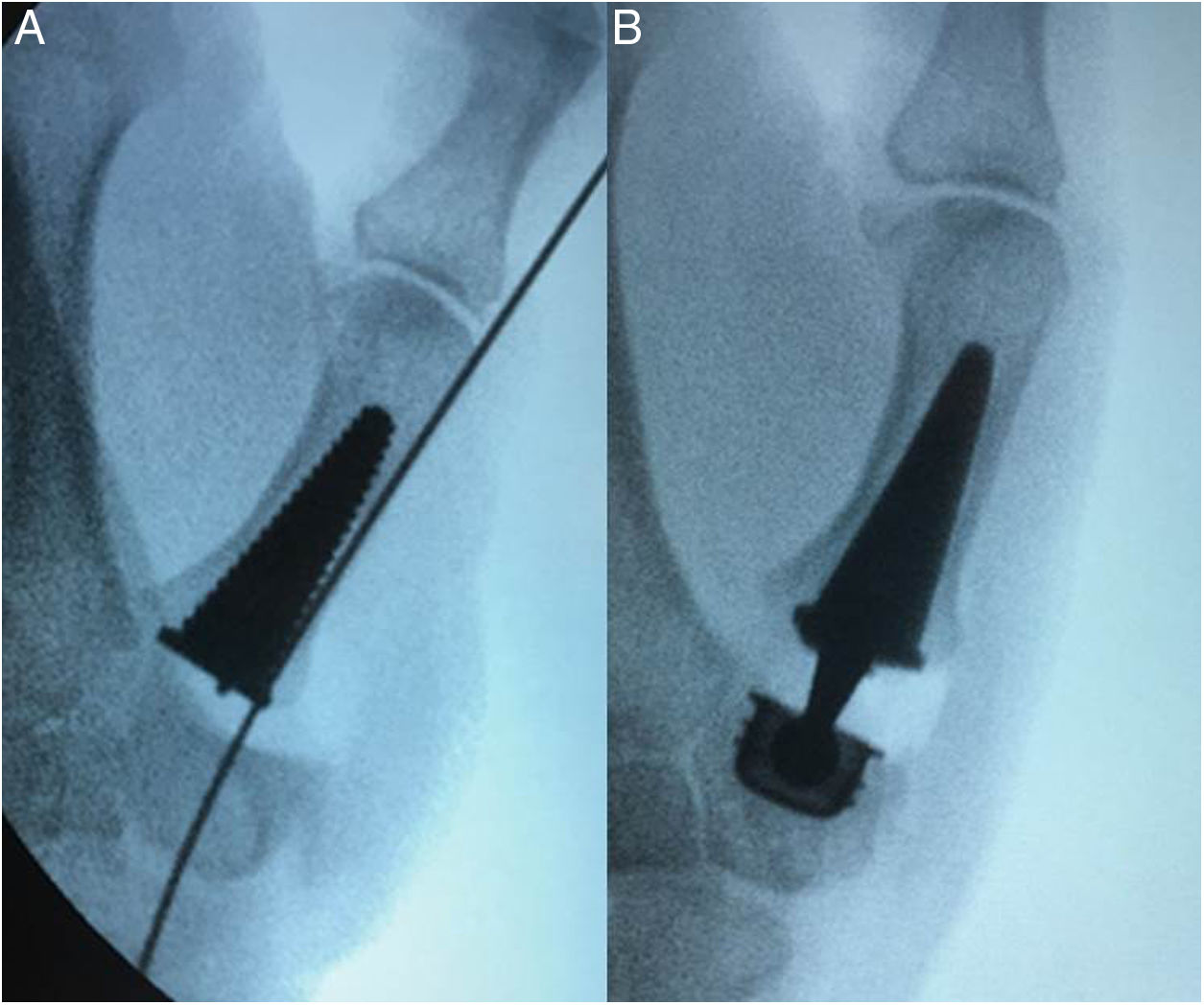
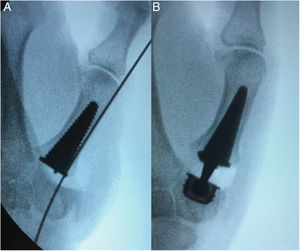
The variables studied were: demographic data, side and dominant hand, in addition to those included in the Van Cappelle14 functional clinical test where scoring was from 0 (poorest score) to 40 (best score) (Fig. 1). Pain, function, mobility, grip and clamp strength were measured to obtain the result. The SAEHAN® (SAEHAN Corporation, S. Korea) hydraulic dynamometer was used: SH5001 for grip strength and SH5005 for clamp strength; the result provided scores according to dominance, sex, and age based on the Torres Coscoyuela et al.15 dynamometric study of the hand and the thumb. The pre and postoperative radiological study comprised 3 projections: posterior–anterior, lateral and the Roberts projection. Radiological variables were collected: the degree of rhisarthrosis of the thumb according to the Eaton scale, the trapezium-head distance of the first metacarpal, the presence of pre-implant radiolucencies, the measurement of the angle between cup orientation and the orientation of the proximal articular surface of the trapezium to assess implantation of the prosthetic threaded cup, in the Roberts projection (Fig. 2). For estimation of radiographic measurements the RIAM Viewer versión 2.5.0 software for observation of medical imaging and diagnostic radiology was used.
Regarding implant characteristics, the Isis® (Evolutis, Roanne, France) trapeziometacarpal prosthesis implant is the direct evolution of the cementless prosthesis by the Guepar Group.10,11 It is a conical trunk threaded anchorage cup prosthesis, titanium and polyethylene lined in the friction region. It is semi-constrained, which limits the risk of dislocation and has a slight surging which reduces restrictions on the trapezium anchorage. It has an articular movement of 68° (superior to the natural one), resulting in a head/neck radius above 2. It presents with 4 modular necks of straight or angled stainless steel, a head diameter of 5 mm and anatomical stem of 5 sizes lined with porous titanium (Fig. 3). Two cemented cups of different diameter are available, to use in cases of salvage surgery.12
Regarding surgical technique, in all cases approach was dorsal, with resection of 5 mm at the base of the first metacarpal, resection of peripheral osteophytes and reaming of the trapezium with guide wire under scopia control focused on all trapezium planes (Fig. 4). We used cannulated motor drills to prevent any swaying effect and to improve reaming precision. The stability of the implant was assessed ensuring lack of rubbing between neck and cup in the maximum ranges of motion.
Technical data of the implanted prosthesis were also collected, such as stem size, neck size and whether it was used straight or angled, together with other procedures used during the same operation. The thumb was immobilised after surgery in a plaster cast for 3 weeks and after this active movement was allowed, according to an established guideline of exercises. Patient satisfaction was assessed according to a scale from 0 to 10, and whether they had returned to previous activities and after how much time. Any complications were recorded.
Statistical analysisThis was performed using the SPSS® 20.0 programme for Windows® (SPSS Inc., Chicago, IL, U.S.A.). Quantitative variables were expressed using means and standard deviation (SD) for those with normal distribution or median and interquartile range (IQR) for variables with non-normal distribution, and categories as percentages. For comparative analysis of pre and postoperative results the Student’s t-test was used for paired data and normal distribution and the Wilcoxon test in cases when the variables did not follow a normal distribution or the Kolmogorov–Smirnov test was not used. In all cases the significant level used was established at p < .05.
ResultsDuring the period described a total of 53 prostheses were implanted in 51 patients. Finally 51 implants in 49 patients formed part of the study, after completing at least one year follow-up and all patients had cementless implants. The 2 excluded patients were implanted with cemented cups because they presented with fragmentation of the trapezium as an intraoperative complication during reaming and the threaded prosthesis could not be used.
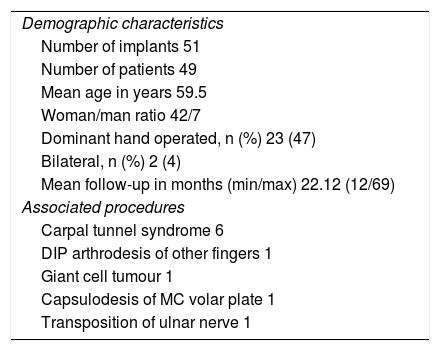
Mean age was 59.5 years (SD 5.6), 42 patients were women (86%). The dominant hand was affected in 23 cases (47%). Mean follow-up was 22.12 months (12–69); 4 implants (7.8%) surpassed the 5 years follow-up, 6 (11.7%) the 4 years, 7 (13%) the 3 years, 14 (27.4%) the 2 years and 20 implants (39.4%) the first year. Surgery associated with prosthesis implantation (Table 1) was also shown. All patients were active, either slightly or moderately.
Demographic characteristics of the simple and the procedures associated with arthroplasty.
| Demographic characteristics |
| Number of implants 51 |
| Number of patients 49 |
| Mean age in years 59.5 |
| Woman/man ratio 42/7 |
| Dominant hand operated, n (%) 23 (47) |
| Bilateral, n (%) 2 (4) |
| Mean follow-up in months (min/max) 22.12 (12/69) |
| Associated procedures |
| Carpal tunnel syndrome 6 |
| DIP arthrodesis of other fingers 1 |
| Giant cell tumour 1 |
| Capsulodesis of MC volar plate 1 |
| Transposition of ulnar nerve 1 |
DIP: distal interphalange; MC: metacarpophalangeal.
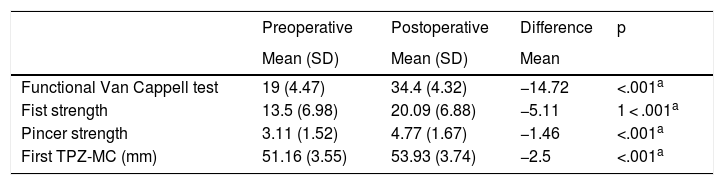
Mean preoperative score of the function Van Cappelle test was 19 points (SD 4.47) and 34.4 (SD 4.32) after the last follow-up, with a mean improvement of 14.72 points having been obtained, which was statistically significant (p < .001). Grip and clamp strength improved significantly, with a mean improvement, respectively, of 5.11 kg (p < .001) and 1.46 kg (p < .001). Regarding the distance between the head of the first metacarpal and the base of the trapezium, we observed an increase in distance of 51.16 mm (SD 3.55) preoperatively to 53.93 mm (SD 3.74) postoperatively (p < .001). A significant improvement was also observed regarding pain relief according to the VAS scale, which passed from 8 (IQE 7−8) to 1 postoperatively (IQR 0–2) (p = .001). Mobility according to the Kapandji test improved from 9 (IQR 8–10) to 10 postoperatively (IQR 10–10) (p = .01). Table 2 shows a summary of the results.
Functional results of the Van Cappelle test in pain, grip strength and clamp strength and XR distance first TPZ-MC.
| Preoperative | Postoperative | Difference | p | |
|---|---|---|---|---|
| Mean (SD) | Mean (SD) | Mean | ||
| Functional Van Cappell test | 19 (4.47) | 34.4 (4.32) | −14.72 | <.001a |
| Fist strength | 13.5 (6.98) | 20.09 (6.88) | −5.11 | 1 < .001a |
| Pincer strength | 3.11 (1.52) | 4.77 (1.67) | −1.46 | <.001a |
| First TPZ-MC (mm) | 51.16 (3.55) | 53.93 (3.74) | −2.5 | <.001a |
| Preoperative | Postoperative | Difference | p | |
|---|---|---|---|---|
| Median (IQR) | Median (IQR) | Median | ||
| VAS pain | 8 (7–8) | 1 (0–2) | 7 | .001b |
| Kapandji test | 9 (8–10) | 10 (10–10) | −1 | .001b |
IQR: interquartile range; TPZ-MC: trapeziometacarpals; SD: standard deviation; VAS: visual analogue scale.
Of the implanted necks, 69% were 8 mm in length (35) and in 82% (42) of cases they were positioned straight.
The mean angle between the prosthetic cup and the proximal articular surface of the trapezium measured in the Roberts projection was 3.8° (SD 2.8). No cases of progressive scaphortrapeziotrapezoid impingement of the joint were observed nor any greater than had existed prior to surgery, nor did any sign of periprosthetic osteolysis appear. The mean score given by the patient regarding their satisfaction with the procedure was 9.4.5–10 Out of the total patients, 47 (96%) returned to their previous activities between the third month (45%) and before the sixth month (49%) of evolution. Two patients did not go back to work. One because of sick leave due to uncontrolled migraines and the other because they presented with invalidating contralateral rhisarthrosis of the thumb pending intervention.
Four intraoperative complications were observed — 2 fragmentations of the trapezium which required the implantation of a cemented cup as salvage surgery and 2 metacarpal fractures which were resolved with cerclage wire (Fig. 5), 3 De Quervain tendinopathies, resolved by medical treatment, one carpal tunnel syndrome and one patient who presented with periprosthetic pain due to the persistence of carpometacarpal osteophytes, which required surgery for osteophytary resection. No major complication such as dislocations, prosthesis mobilisation or infections were recorded. Implant survival has been 100% in all cases since the last follow-up check-up.
DiscussionThe successful results obtained by second generation16 trapeziometacarpal prostheses over the last few years would probably change the concept of “gold standard” for the treatment of thumb rhisarthrosis that we have had to date.3 In the short term better and faster functional outcomes than those of trapeziectomies with suspended arthroplasty have already been published,3,4,17 and this would justify the cost of the implant in functionally active patients. The other battle front to justify its use would be medium to long-term outcomes. Several prosthesis models have presented a high rate of implant survival in the medium term, like in the study by Cootjans et al.13 on the Arpe® prosthesis, where the implant was maintained in 96% of cases, at 6.5 years of evolution, or that of Goubau et al.,18 who reported that at a mean of 5 years, there was a 95% survival rate with the Ivory.® We can also find long-term outcomes, such as those of the study by Martin-Ferrero et al. after 10 years on the Arpe®, with 93% of survival,19 or of the 95% also after 10 years with the Ivory®20 prosthesis of the Tchurukdichian et al. study.
Other more evolved models considered as third generation, with dual mobility, have also reported high medium-term survival, such as in the study on the Moovis® model by Martins et al.21 at a mean evolution of 5 years, with 100% implant survival. Regarding threaded cup prostheses, we believe that they do not enjoy great popularity due to the poor results obtained by the Elektra®, prosthesis, the implant defined as one of those with earlier faults.22,23 According to Thorkildsen et al.24 this is due not just to its design, but also to its metal-on-metal friction which leads to early cup mobilisation. The study by Ganhewa et al.22 evaluated the faults of many currently used implants, with the exception of the cementless Isis®. The latter has been able to impact trust in other different threaded models. Our results shows a 100% implant survival. We believe that this is for 2 essential reasons: on the one hand, the design of the implant itself, and on the other, its placement technique. It has been reported that the correct positioning of the cup is crucial for reducing the risk of major complications, such as dislocation, wear and tear or mobilisation;13,25,26 it should be centred in the trapezium to provide stability and prevent trapezium fracture or contact of the neck with the edge of the polyethylene which leads to wear and tear and displacement. Up until Duerinckx and Caekebeke’s article7 of 2016, there was no clear guideline as to how to orientate the cup. The proximal articular surface of the trapezium is almost flat and may serve as a line of reference. Duerinckx and Caekebeke refer to the fact that the line which represents the centre of mobility forms an angle of 90° with respect to the proximal articular surface of the trapezium (PAST), in the anteroposterior projection and of 83° in the lateral projection. Therefore, the cup should be placed parallel to the articular surface of the trapezium in all planes during surgery, using a neck with 7° angulation to compensate for the 7° inclination presented by the movement axis in the lateral plane compared with the proximal surface of the trapezium. Since providing these 7° of cup inclination would be highly technically complex, according to Brauns et al.,8 the cup should be placed parallel to the PAST to reduce the risk of dislocation, according to the studies by Duerinckx and Caekebeke. The risk of complications was significantly increased when it went past 20°, especially in the mediolateral plane.
In the case of the surgical technique of the Isis® implantation, unlike other models, the cup must be under scopia control and the guide wire centred on all planes. This means that the implant is centred in the trapezium and parallel to the PAST, minimising the risks of dislocation, wear and tear and mobilisation. Goubier et al.27 studied the mobility of healthy trapeziometacarpals and observed that the mean mobility in flexion-extension was 41° and in abduction-adduction it was 51°. The Isis® has a range of motion of 68°; this provides a margin of error in cup alignment which reduces the possibility of impingement between the neck and the cup during a maximum range of motion.
In our casuistic, the mean angle formed by the prosthetic cup and the PAST was 3.8°, in no projection did it surpass 9°, it was always far from the 20° where the risk was significantly raised. This ensured correct alignment of the cup with regard to the axis of movement, with this being a highly important factor in the absence of dislocations or mobilisations in our series. Lerebours et al. carried out a systematic review of all the implants used currently for the treatment of rhisarthrosis of the thumb, published in March 2020, but did not include any study on the Isis® with cementless cup.28 They only referred to a study on this type of implant and with a cemented cup.29
This study was subject to the limitations derived from short follow-up for an implant of this type, and we therefore could not reach any conclusions regarding the risk of long-term loosening. The number of implants is also limited. There is also a lack of a comparative group, but our study is the most extensive series review on this implant, at least up until its redaction.
ConclusionsThe survival and functional outcomes of the Isis® prosthesis in our experience have been excellent in the short term, with a minimum follow-up of one year. They are similar and even better than those reported by other models. We believe surgical technique must be accurate, particularly in the implantation of the trapezium component as this is a key element to reduce the risk of dislocation and mobilisation, which are the major complications of these implants.
Level of evidenceLevel of evidence iv.
Conflict of interestsThe authors have no conflict of interests to declare.
Please cite this article as: Sánchez-Crespo MR, de la Red-Gallego MA, Ayala-Gutiérrez H, Couceiro-Otero J, Rodríguez-Fernández J, del Canto-Alvarez FJ. Supervivencia inicial de la prótesis total trapeciometacarpiana de cúpula roscada Isis®. Rev Esp Cir Ortop Traumatol. 2021;65:416–423.