Ribbing disease is a rare benign sclerosing bone dysplasia. It presents with an increased bone density at the diaphysis with cortical endosteal/periosteal thickening and affects predominantly the lower extremities. We report a case of a 28-year-old woman with a condition in her tibia that occluded the medullary cavity, with severe pain that could not be relieved with anti-inflammatory therapy. Several cases have been published on pain relief after intramedullary reaming. We performed this treatment with the surgical steps to avoid complications such as a fracture or false route that may occur due to the difficulty in piercing the closed medullary cavity. Pain improved immediately after surgery, and the patient is asymptomatic after one year. The natural progression of ribbing disease is to stabilize, but there are no data published with long term follow-up after intramedullary reaming.
La enfermedad de Ribbing es una displasia ósea esclerosante benigna poco frecuente. Se presenta con un incremento de la densidad ósea a nivel diafisario con engrosamiento cortical endo/periostal que predomina en extremidades inferiores. Presentamos una mujer de 28 años con una lesión de éstas características a nivel tibial que llega a obstruir por completo el canal medular y con dolor muy intenso no controlable con analgésicos habituales. Está publicado en varios casos cómo el fresado endomedular alivia de forma notable los síntomas. Aplicamos dicho tratamiento detallando los pasos quirúrgicos empleados para evitar una fractura y falsa vía que puede producirse por la dificultad de traspasar el tapón óseo escleroso. La paciente mejoró inmediatamente en el postoperatorio encontrándose asintomática al año de la intervención. En su evolución natural la enfermedad tiende a estabilizarse, no hay datos a largo plazo en los pocos casos publicados con fresado endomedular.
The patient was a 23-year-old woman from Morocco, who presented with constant pain in the left leg over the previous year, with a feeling of tiredness and heaviness that gradually increased throughout the day and got worse at night. She presented limitations in walking normally; analgesic and anti-inflammatory drugs gave her little relief. She classified her pain on the visual analog scale (VAS) as between severe and very severe (9/10). Simple X-ray of the left tibia showed diaphyseal fusiform endosteal and periosteal sclerosis without metaphysis and epiphysis involvement, with another similar lesion in the distal fibula (Fig. 1A and B). Computer-assisted tomography scan revealed that the lesion obstructed the intramedullary canal (Fig. 1C and D).
Simple radiograph of the left tibia. Fusiform diaphyseal endosteal and periosteal sclerosis sparing the metaphysis and epiphysis could be seen, with another similar lesion in the distal fibula (a, b). The computer-assisted tomography image revealed that the lesion obstructed the intramedullary canal (c, d). The bone scintigraphy series revealed smaller, asymptomatic sclerotic intramedullary lesions in these locations (e).
Bone scintigraphy also showed increased uptake in the distal area of both femurs and fibulas, but the greatest activity was in the middle third of the left tibia. The bone X-ray series revealed smaller, asymptomatic sclerotic intramedullary lesions in these areas (Fig. 1E). Routine blood analysis returned normal values (hemogram, biochemistry, sedimentation rate and C-reactive protein, alkaline phosphatase, parathyroid hormone, vitamin D levels of 1.25 and 25).
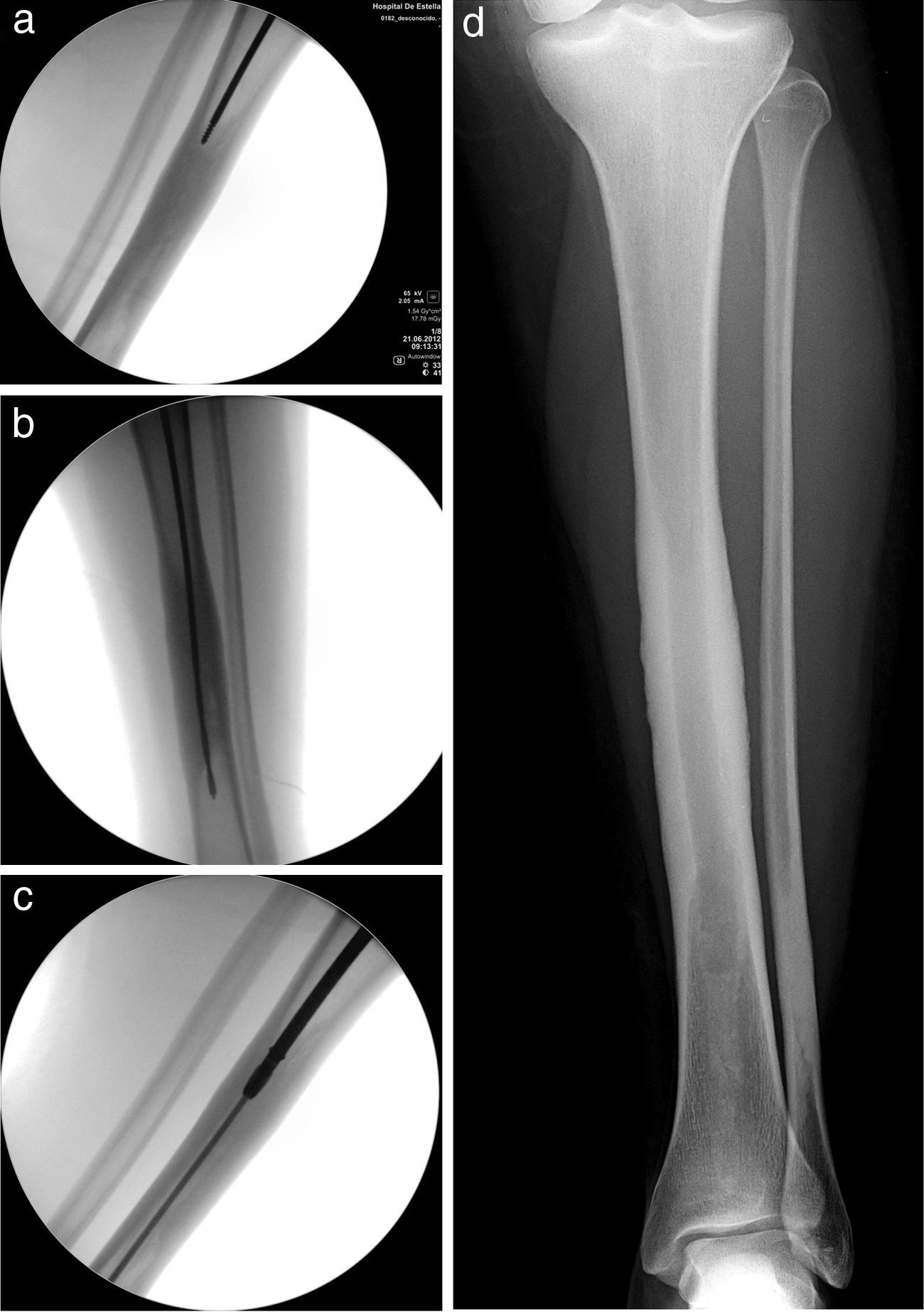
The differential diagnosis contemplated in the face of a lesion having these features is shown in Table 1, but it is mainly with Camurati–Engelmann disease, a similar entity having childhood onset that is progressive and genetically transmitted. A few cases have been described in which surgical reaming to remake the intramedullary canal was very effective in relieving intense pain. Suspecting Ribbing disease, we decided to apply this treatment. The main problem is performing it in a centered fashion to avoid taking a false route, fracturing the tibia and making the surgical objective more complicated. As the canal was entirely occupied, it was not possible to pass a standard knotted reamer guide. The lesion area was penetrated using a sufficiently long threaded wire under alternative anterior/posterior–lateral scope control (Fig. 2A). After removing the threaded wire, a bit (Fig. 2B) and manual reamer of a larger diameter were passed sequentially until it was possible to introduce the knotted guide; this was then used to perform a standard progressive reaming, widening the canal to 9.5mm (Fig. 2C). Samples of the reaming-obtained tissue were sent for histological study and culture. Results showed normal bone with absence of bacterial growth. One week after surgery, the patient reported a pain level of 0 in the VAS scale and she remained totally asymptomatic 12 months following the intervention (Fig. 2D).
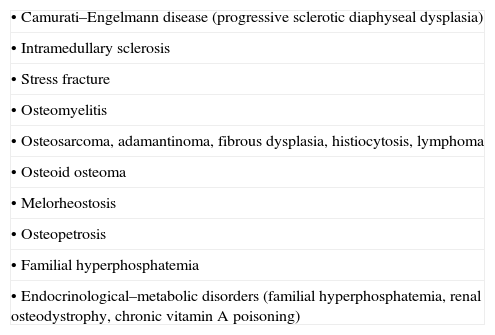
Differential diagnosis of sclerotic bone lesions.
| • Camurati–Engelmann disease (progressive sclerotic diaphyseal dysplasia) |
| • Intramedullary sclerosis |
| • Stress fracture |
| • Osteomyelitis |
| • Osteosarcoma, adamantinoma, fibrous dysplasia, histiocytosis, lymphoma |
| • Osteoid osteoma |
| • Melorheostosis |
| • Osteopetrosis |
| • Familial hyperphosphatemia |
| • Endocrinological–metabolic disorders (familial hyperphosphatemia, renal osteodystrophy, chronic vitamin A poisoning) |
The lesion area was penetrated using a sufficiently long threaded wire under alternative anterior/posterior–lateral scopy control (a). After withdrawing the threaded wire, a bit (b) and manual bur of a larger diameter were passed sequentially until a knotted guide wire could be inserted; this was used to perform standard progressive reaming, widening the canal to 9.5mm (c). The patient reported a pain level of 0 (VAS scale) 1 week after surgery and remained totally asymptomatic 12 months after the intervention (d).
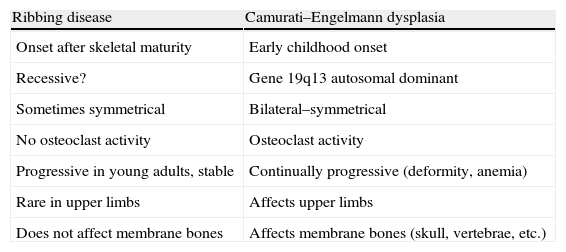
In 1949 Ribbing1 described 4 cases of diaphyseal sclerosis of the long bones among 6 siblings and his name was given to this rare disease. Greenspan's2 review on sclerosing bone dysplasia included those that evolve with intramedullary ossification. Of these, the most characteristic is Camurati–Engelmann disease, with autosomal-dominant inheritance (gene 19q13), with which differential diagnosis is necessary (Table 2). At present, according to Makita et al.,3 Ribbing disease may represent a phenotypic variation of the same disorder and may have recessive inheritance. Affecting young adults, the disease produces a sclerosis with progressive endosteal/periosteal cortical thickening especially in the lower limbs (above all, in tibia and femur), while sparing the metaphysis and epiphysis. The series of Seeger et al.4 and Beals et al.5 together add up to a total of 18 patients (13 women and 5 men), including 15 tibias (12 bilateral), 7 femurs (5 bilateral), and 2 fibula cases. Our patient had bilateral involvement of femurs and fibulas, as well as the left tibia (symptomatic). The remaining cases published are generally isolated, with involvement of the femur or tibia. Due to the radiological characteristics, Ribbing disease can be mistaken for chronic osteomyelitis, stress fracture, or other disorders as shown in Table 2. Its natural progression is unclear, normally stabilizing with age. It is characterized by variable intense pain, of uncertain origin; Rubin6 attributed the pain to blood vessels being trapped between bones, while Gaeta et al.7 proposed the bone edema detected in magnetic resonance as the cause. Bisphosphonates have been used as a treatment, but there is a published case of symptoms getting worse after administering intravenous pamidronate.8 Disease progression can obstruct the medullary canal. In cases of unbearable pain, Beals et al.,5 Matas et al.,9 and Öztürkmen and Karamehmetoğlu10 have published instances of complete relief following intramedullary reaming based on observations by Fallon et al.,11 as there were patients who improved after intramedullary scraping to obtain samples for anatomopathological study. Zhang et al.12 reported a case with improvement with isolated perforations in a femur, but without publishing radiological images. In the series of Seeger et al.4 (6 patients), biopsy showed thickened reactive bone of normal characteristics with a greater number of osteocytes per surface unit and smaller Haversian canals or non-specific reactive changes. In our case, the material obtained from the reaming was reported to be normal bone. We show a case similar to that of Matas et al.,9 indicating the surgical steps used to avoid the possible complication of fracture and false route that can arise due to the difficulty in penetrating the sclerotic bony plug, as occurred in the case of Beals et al.5 We felt that reaming to a diameter of 9.5mm was sufficient; except for the article by Beals et al.,5 which reported having reamed a femur to 13mm, there is no mention published as to the diameter to reach. Matas et al.9 published a case with an evolution of 5 years, as did Öztürkmen and Karamehmetoğlu,10 while that published by Beals et al.5 had an evolution of 3, and our case had 1; all these patients were asymptomatic after follow-up.
Differential diagnosis between ribbing and Camurati–Engelmann diseases.
| Ribbing disease | Camurati–Engelmann dysplasia |
| Onset after skeletal maturity | Early childhood onset |
| Recessive? | Gene 19q13 autosomal dominant |
| Sometimes symmetrical | Bilateral–symmetrical |
| No osteoclast activity | Osteoclast activity |
| Progressive in young adults, stable | Continually progressive (deformity, anemia) |
| Rare in upper limbs | Affects upper limbs |
| Does not affect membrane bones | Affects membrane bones (skull, vertebrae, etc.) |
Source: with permission from Beals et al.5
In summary, Ribbing disease is a rare benign pathology, characterized by endosteal/periosteal intramedullary sclerosis, principally in the lower limbs. If pain is intense, intramedullary reaming has shown to be effective in relieving symptoms. We have shown in detail the surgical steps we follow to avoid fracture/false route complications. How much to widen the canal is arbitrary, and the possibility of recurrence exists. In favor is the fact that the disease stabilizes in adults.
Level of evidenceLevel of evidence 4.
Ethical responsibilitiesProtection of people and animalsThe authors declare that no experiments were performed on human beings or animals for this research.
Data confidentialityThe authors declare that they followed the protocols of their work center on the publication of patient data and that all the patients included in the study received sufficient information and gave their written informed consent to participate in this study.
Right to privacy and informed consentThe authors obtained informed consent from the patients and/or subjects referenced in the article. This document is in the hands of the corresponding author.
Please cite this article as: Noain-Sanz E, et al. Fresado endomedular en la enfermedad de Ribbing. Rev Esp Cir Ortop Traumatol. 2013;57:231–4.