Perthes disease often produces a congruent nonspherical coxa. The most widely accepted cause is initial bone collapse, but some authors refer to physeal injury as the cause of this deformity. We analyze this elliptical process in cases of congruent nonspherical Perthes.
MethodsRetrospective case-control study of 49 unilateral class III–IV Perthes cases that were not operated on. Results were compared with 49 healthy contralateral hips. The following radiological variables were determined both in AP and lateral projection, and at 4 points in time of the disease: ovalization index (OI), arthrotrochanteric distance, intraphysial angle, physeal narrowing, presence of double epiphyseal reosification nucleus, physeal length and Reimers index.
ResultsThe initial OI was 1.7 in the early reosification phase and final OI was 2.07 at physeal closure. The OI in the control cases was invariably 1.4. There was a direct relation between a high index and the initial appearance of a double epiphyseal ossification nucleus, asymmetric physeal effacement and the increase of the intraphyseal angle in both radiographic projections.
ConclusionsThe elliptical process of the femoral head occurs progressively throughout the disease and not only during bone collapse. It starts in the reosification phase and ends when growth stops. The initial risk signs found were the appearance of the double nucleus of reosification, the progressive angulation of the physis and the progressive increase in the rate of ovalization.
Level of evidenceIII control cases.
La enfermedad de Perthes produce frecuentemente una coxa anesférica congruente. La causa más ampliamente aceptada es el colapso óseo inicial, pero algunos autores hacen referencia a la lesión fisaria como causante de esta deformidad. Nos proponemos analizar este proceso de ovalización en casos de Perthes anesféricos congruentes.
MétodosEstudio retrospectivo de casos-control de 48 casos unilaterales de Perthes clase III-IV que no fueron operados. Los resultados se compararon con las 48 caderas contralaterales sanas. Se determinaron las siguientes variables radiológicas tanto en proyección AP como en lateral, y en 4 momentos del curso de la enfermedad: índice de ovalización, distancia artículo-trocantérica, ángulo intrafisario, borramiento fisario, presencia de doble núcleo de reosificación epifisario, longitud fisaria e índice de Reimers.
ResultadosEl IO inicial fue de 1.7 en la fase de reosificación precoz y final de 2.07 al cierre fisario. El IO en los casos control fue invariablemente de 1.4. Hubo una relación directa entre un índice alto y la aparición inicial de un doble núcleo de osificación epifisaria, borramiento fisario asimétrico y el aumento del ángulo intrafisario en ambas proyecciones radiográficas.
ConclusionesEl proceso de ovalización de la cabeza femoral se produce de forma progresiva a lo largo de la enfermedad y no solo durante el colapso óseo. Se inicia en la fase de reosificación y finaliza al cesar el crecimiento. Los signos de riesgo iniciales encontrados fueron la aparición del doble núcleo de reosificación, la angulación progresiva de la fisis y el aumento progresivo del índice de ovalización.
Nivel de evidenciaIII casos control.
Legg-Calvé-Perthes’ disease is also known as “flat coxa”, and it causes final Stulberg class III or IV1–3 congruent aspherical morphology in more than 30% of cases.1 The final shape of the femoral head will depend on the degree of bone collapse caused in the first phases of necrosis/fragmentation, and the altered growth in the head physis that gives rise to evolving deformities during the re-ossification/remodelling phases.4–8
Unlike the collapse of bone that can be recovered, necrosis of the layer of physis basal cells is not recoverable. Asymmetric or incomplete necrosis of the epiphyseal cartilage causes irregular plate growth. This commences in the re-ossification stage and increases during the remodelling phase, once the necrotic phase has cured.7–11 This aspherity was described by Nelson3 in the “Deformity Index”, and he described it as the process of cephalic widening and flattening. He did not detect any predictive signs that would anticipate its development.
Although a physeal lesion is hard to detect using radiological means, it may be inferred once the logical consequences have appeared. These include progressive alterations in the shape of the proximal end of the femur, which include excessive growth of the greater trochanter, a wide short neck, physeal erasure, an inferior epiphysis and a discrepancy in the length of the inferior limbs.5–8
We propose to study this process of ovalisation of the femoral head caused in cases of congruent aspherical heads (Stulberg classes III and IV). We also attempt to determine which factors may be present at the start, so that they can be labelled as risk factors for the appearance of an oval flat coxa.
Material and methodsAll of the cases of Legg-Calvé-Perthes that had been seen by the authors and followed up until the end of growth were reviewed retrospectively. Bilateral cases and those which had been treated surgically were ruled out. The inclusion criterion was the presence of a Stulberg class III or IV congruent aspherical femoral head.1,2 Cases without a complete clinical and radiological follow-up from diagnosis until skeletal maturity were ruled out.
The series that was analysed included 48 patients (48 hips), 25 of which were Stulberg class III and 23 of which were Stulberg class IV. The healthy side of the hip was taken as the control group. The average age at diagnosis was 3.9 years (range 2.2–6.1). The total duration of the disease was evaluated.
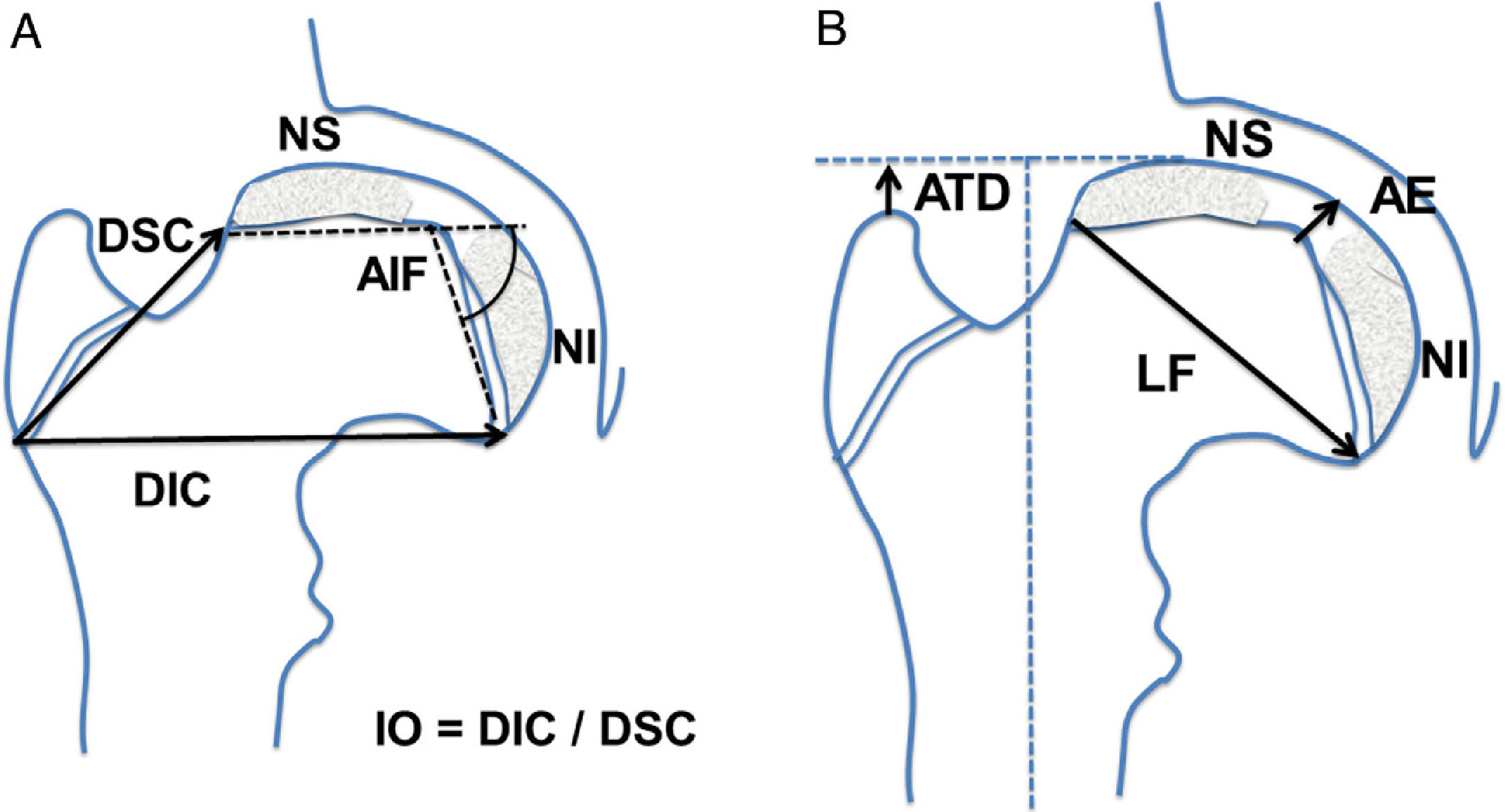
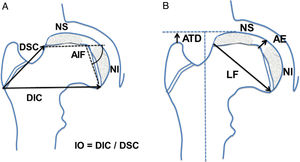
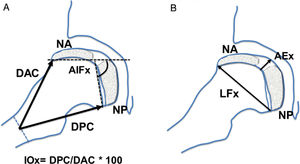
The following radiographic measurements were determined in anteroposterior hip projection: article-trochanter distance (ATD), superior distance of the neck, inferior distance of the neck, central epiphysis height, intraphyseal angle, physeal length, presence of a dual epiphyseal re-ossification nucleus and physeal narrowing or erasure. The amount of extruded head was also quantified, together with the intruded head and Reimers’ extrusion index. The ovalisation index was calculated as was the coefficient between the inferior distance of the neck divided by the superior distance of the neck (Fig. 1).
Diagram showing the measurements taken in anteroposterior hip projection. (a) AIF: intraphyseal angle; DIC: inferior distance of the neck; DSC: superior distance of the neck; IO: ovalisation index; NI: inferior re-ossification nucleus; NS: superior re-ossification epiphyseal nucleus. (b) AE: epiphyseal height in the centre; ATD: article-trochanter distance; LF: physeal length or cephalic diameter; NI: inferior re-ossification nucleus; NS: superior epiphyseal re-ossification nucleus.
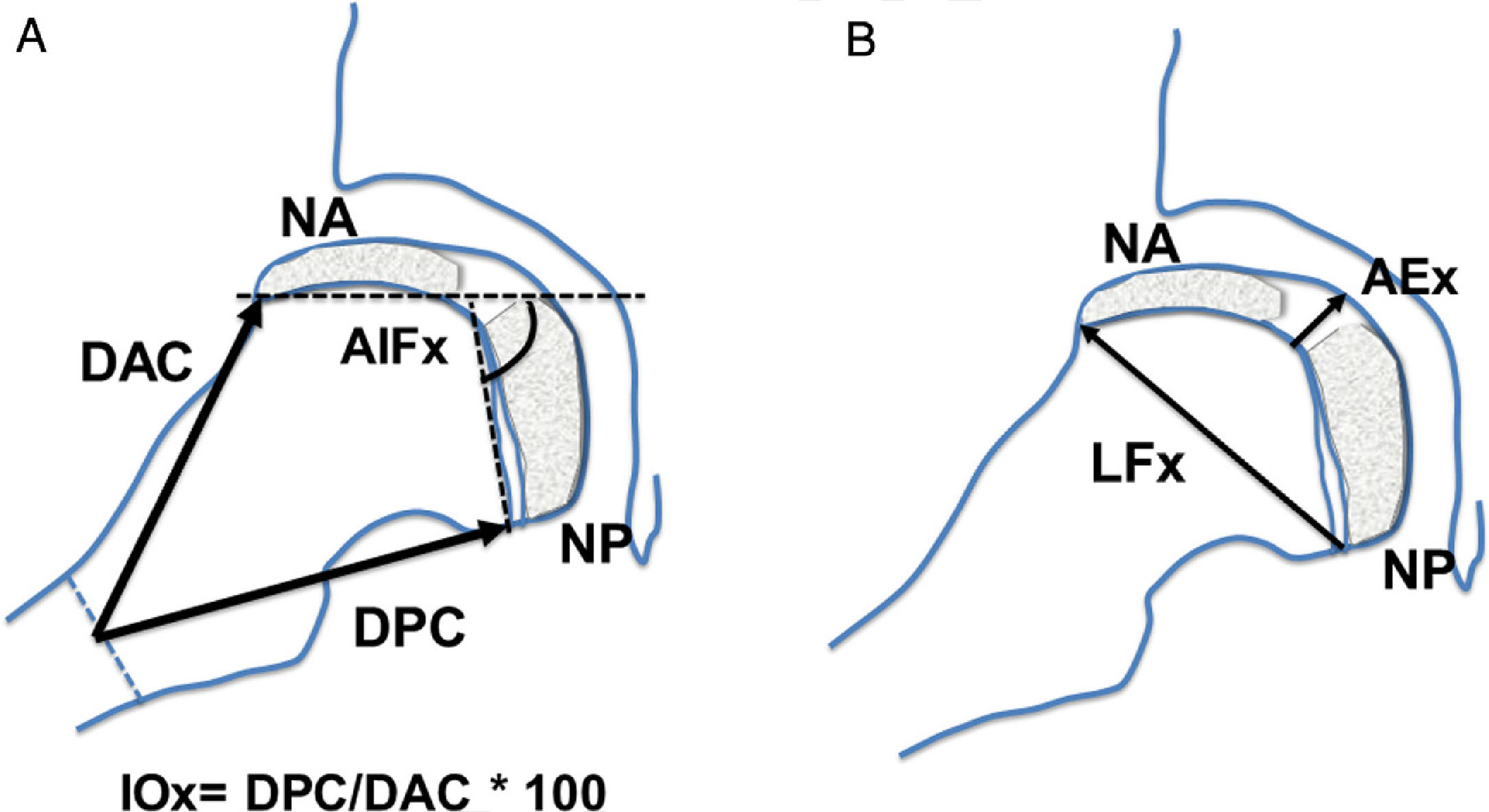
The following measurements were determined in frog leg or Löwenstein lateral projection: anterior distance of the neck, posterior distance of the neck, central epiphyseal height, intraphyseal angle, physeal length, presence of double epiphyseal ossification nucleus and physeal narrowing (Fig. 2). The axial ovalisation index was calculated, as was the coefficient between the posterior neck measurement and the anterior neck measurement multiplied by 100 (Fig. 2).
Diagram showing the measurements taken in lateral, frog leg or Löwenstein hip projection. (a) AIFx: axial intraphyseal angle; DAC: anterior distance of the neck; DPC: posterior distance of the neck; IOx: axial ovalisation index; NA: anterior re-ossification epiphyseal nucleus; NP: posterior re-ossification nucleus. (b) AEx: axial epiphyseal height in the centre; LFx: physeal length or axial cephalic diameter; NA: anterior re-ossification epiphyseal nucleus; NP: posterior re-ossification nucleus.
All of these radiographic measurements were taken at 4 different moments during the evolution of the disease. The first took place one year after the start of re-ossification, at the age of about 6 years, and the last took place at the end of growth after physeal closure (at about the age of 16 years). The other 2 radiographic checks were performed at equidistant moments between them, i.e., at 9 and 12 years old. The size and length of the femoral head was thereby monitored throughout infancy, including the period corresponding to the disease and the remodelling phase. The DICOM real time imaging system was used (DICOM 3.0 Conformance Statement system, IRE Store Channel® version 4; Philips).
The SPSS program was used for the statistical study (version 15; IBM, Chicago, IL, U.S.A.). The statistics included the comparison of quantitative variables using the Student t-test after checking for normalcy and variance homogeneity. The ANOVA test was used to compare quantitative variables, together with post hoc Tukey analysis. We applied the Wilcoxon test in cases of non-homogeneous variances. The contingency test was used to compare qualitative variables. The level of significance was P < .05.
ResultsIn the series studied the onset of the disease occurred at an average age of 3.9 years and lasted for an average of 7.4 years (range 3.8–12.1 years), and the process ended at 11.3 years old.
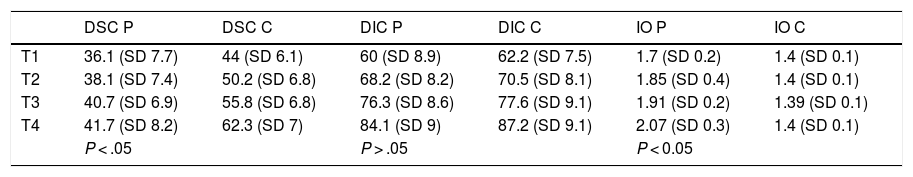
The results of measurements in anteroposterior projection of the neck and ovalisation indexes are described in Tables 1–3, together with physeal length, ATD and Reimers’ index.
Results obtained respecting the inferior and superior neck distances. This also shows the result of the ovalisation index of the control and disease cases.
| DSC P | DSC C | DIC P | DIC C | IO P | IO C | |
|---|---|---|---|---|---|---|
| T1 | 36.1 (SD 7.7) | 44 (SD 6.1) | 60 (SD 8.9) | 62.2 (SD 7.5) | 1.7 (SD 0.2) | 1.4 (SD 0.1) |
| T2 | 38.1 (SD 7.4) | 50.2 (SD 6.8) | 68.2 (SD 8.2) | 70.5 (SD 8.1) | 1.85 (SD 0.4) | 1.4 (SD 0.1) |
| T3 | 40.7 (SD 6.9) | 55.8 (SD 6.8) | 76.3 (SD 8.6) | 77.6 (SD 9.1) | 1.91 (SD 0.2) | 1.39 (SD 0.1) |
| T4 | 41.7 (SD 8.2) | 62.3 (SD 7) | 84.1 (SD 9) | 87.2 (SD 9.1) | 2.07 (SD 0.3) | 1.4 (SD 0.1) |
| P < .05 | P > .05 | P < 0.05 | ||||
T1, T2, T3, and T4 are the 4 moments when the variables were measured.
IO C: ovalisation index in the controls; IO P: ovalisation index in Perthes cases; DIC C: inferior neck distance in the control cases; DIC P: inferior neck distance in the Perthes cases; DSC C: superior neck distance in the control cases; DSC P: superior neck distance in the Perthes cases; SD: Standard Deviation.
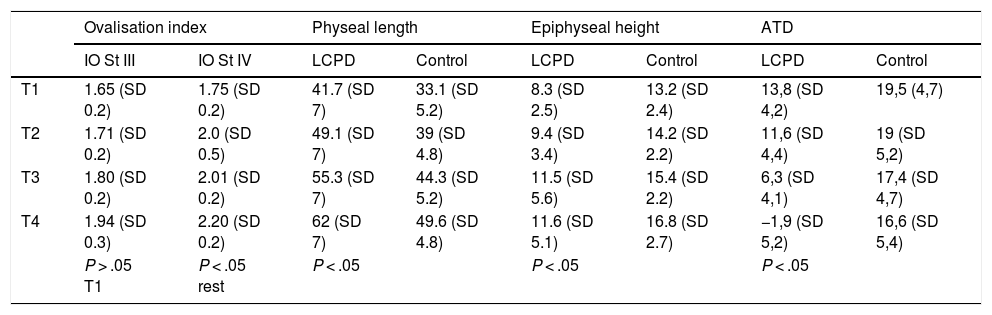
Results of the variables: ovalisation index according to Stulberg grades, physeal length, epiphyseal height and article-trochanter distance.
| Ovalisation index | Physeal length | Epiphyseal height | ATD | |||||
|---|---|---|---|---|---|---|---|---|
| IO St III | IO St IV | LCPD | Control | LCPD | Control | LCPD | Control | |
| T1 | 1.65 (SD 0.2) | 1.75 (SD 0.2) | 41.7 (SD 7) | 33.1 (SD 5.2) | 8.3 (SD 2.5) | 13.2 (SD 2.4) | 13,8 (SD 4,2) | 19,5 (4,7) |
| T2 | 1.71 (SD 0.2) | 2.0 (SD 0.5) | 49.1 (SD 7) | 39 (SD 4.8) | 9.4 (SD 3.4) | 14.2 (SD 2.2) | 11,6 (SD 4,4) | 19 (SD 5,2) |
| T3 | 1.80 (SD 0.2) | 2.01 (SD 0.2) | 55.3 (SD 7) | 44.3 (SD 5.2) | 11.5 (SD 5.6) | 15.4 (SD 2.2) | 6,3 (SD 4,1) | 17,4 (SD 4,7) |
| T4 | 1.94 (SD 0.3) | 2.20 (SD 0.2) | 62 (SD 7) | 49.6 (SD 4.8) | 11.6 (SD 5.1) | 16.8 (SD 2.7) | −1,9 (SD 5,2) | 16,6 (SD 5,4) |
| P > .05 T1 | P < .05 rest | P < .05 | P < .05 | P < .05 | ||||
T1, T2, T3, and T4 are the 4 moments when the variables were measured.
ATD: article-trochanter distance; IO St III and IV: ovalisation index according to Stulberg grades III and IV; LCPD: Legg-Calvé-Perthes’ disease; SD: standard deviation.
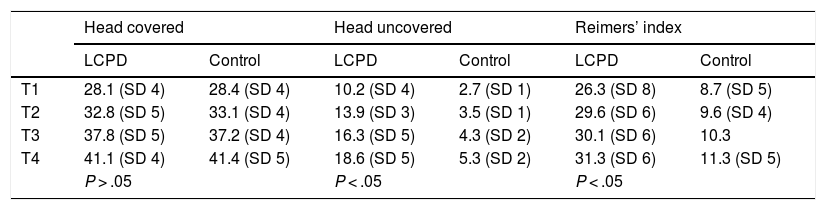
Results of the variables femoral head extrusion according to Reimers’ index: amount of head covered /head uncovered *100.
| Head covered | Head uncovered | Reimers’ index | ||||
|---|---|---|---|---|---|---|
| LCPD | Control | LCPD | Control | LCPD | Control | |
| T1 | 28.1 (SD 4) | 28.4 (SD 4) | 10.2 (SD 4) | 2.7 (SD 1) | 26.3 (SD 8) | 8.7 (SD 5) |
| T2 | 32.8 (SD 5) | 33.1 (SD 4) | 13.9 (SD 3) | 3.5 (SD 1) | 29.6 (SD 6) | 9.6 (SD 4) |
| T3 | 37.8 (SD 5) | 37.2 (SD 4) | 16.3 (SD 5) | 4.3 (SD 2) | 30.1 (SD 6) | 10.3 |
| T4 | 41.1 (SD 4) | 41.4 (SD 5) | 18.6 (SD 5) | 5.3 (SD 2) | 31.3 (SD 6) | 11.3 (SD 5) |
| P > .05 | P < .05 | P < .05 | ||||
T1, T2, T3, and T4 are the 4 moments when the variables were measured.
LCPD: Legg-Calvé-Perthes’ disease; SD: Standard Deviation.
In the Legg-Calvé-Perthes disease group, the presence of an epiphyseal re-ossification dual nucleus was found in 43 cases in the first measurement (90% of cases). In 33 hips it was possible to detect its presence in at least 2 successive measurements (69% had this during 6 years). The presence of a dual epiphyseal re-ossification nucleus in more than 2 measurements was significantly more frequent in Stulberg class IV cases (P < .05). No case had a hip with a dual epiphyseal nucleus in the control cases.
In respect of physeal loss, there were 34 partial physeal losses in the first measurement in the 48, and in the second measurement there were 47 cases with physeal loss. In the final measurement the cases as well as the controls had complete loss of the physis. No physeal loss was present in the control group until the end of growth.
In anteroposterior projection the epiphyseal height in the cases of Perthes was 7.8 mm (SD 2.1) in the first measurement, in the second it was 8.8 mm (SD 2.4), in the third it was 8.9 mm (SD 2.4) and at the end of growth it was 10 mm (SD 4.2). In the control group it was 12.2 mm (SD 2.3) in the first measurement, in the second it was 14 mm (SD 2.1), in the third it was 15.6 mm (SD 1.9) and at the end of growth it was 16.6 mm (SD 2). Significant differences were detected between them (P < .05). The final difference in height between a healthy head and one with Perthes was that the latter was 6.6 mm inferior.
All of the diseased hips shows some type of physeal angle in anteroposterior projection, with an intraphyseal angle of 43.3° in the first measurement, 58.1° in the second, 63.3° in the third and 72.5° at the end of growth (P < .05). No type of angle was detected in the control group.
With regard to the axial or lateral Löwenstein projection, we obtained an axial ovalisation index in the patients of 104 (SD 6.1) in the first measurement, 106.6 (SD 8) in the second, 108.9 (SD 8) in the third and 112.7 (SD 8.6) in the last measurement. Comparison of the indexes between the cases and controls showed a P of < .05. The ovalisation index of the controls was 99.6 (SD 3.5) in the first measurement, 98 (SD 3.8) in the second, 98.3 in the third (SD 5.1) and 97.6 (SD 4.7) in the fourth measurement.
The axial physis length in cases of Perthes at the 4 times of measurement was 39.6 mm (SD 10), 48.5 mm (SD 7.4), 55.9 mm (SD 6.2) and 62 mm (SD 7.3), while in the control group it was: 34 mm (SD 5.5), 39.2 mm (SD 4.7), 45 mm (SD 5.1) and finally 49.3 mm (SD 5). The difference in length of the physis head between the cases and controls was 8.6 mm in the first measurement (P < .05), 10.1 mm (P < .05), 11 mm (P < .05) and finally 12.4 mm (P < .05). At the end of the follow-up physeal length was 12 mm longer in Perthes cases than it was on the healthy side, which is equivalent to having a head that is 25% wider (49.6 vs 62).
The axial physeal angle was 47.3° (SD 24) in the first measurement, 57.5° (SD 25.5) in the second, 63.5° (SD 27) in the third measurement and 67.4° (SD 30) at the end of growth. The control hips never showed any physeal angle.
DiscussionBone necrosis at both sides of the cephalic physis necessarily causes necrosis of the growth plate,4,6,8 especially in cases of massive necrosis.8,12–15 The necrotic lesion of the germinative layer would be within expectable limits due to its terminal irrigation7,8,16 and the fact that the blood reaches it through the epiphyseal bone.6 Involvement of the physis is associated with a poor final prognosis,5,8,12,16–19 and some authors estimate that 30% of Perthes cases suffer physeal arrest.11
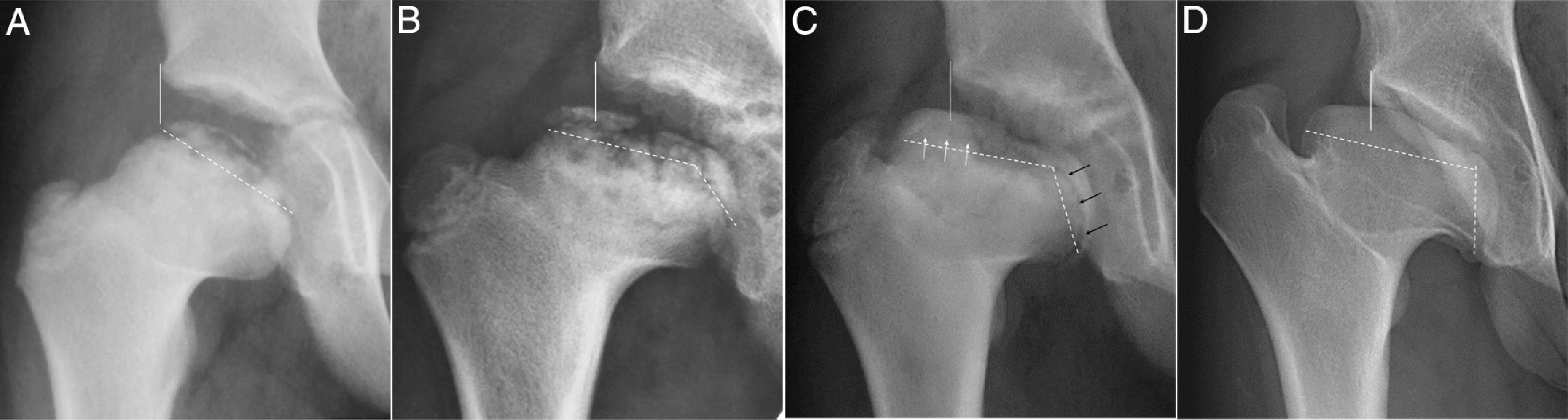
The direct radiological signs of physeal lesion are hard to detect at the start of the process.8,10,12 The earliest signs include narrowing and loss of the early physis or the existence of bone metaphyseal-epiphyseal bridges10,16 which function as anchorage points and slow growth.15 There may also be a fall in the number of germinal cells, although all of them will not be lost, so that their cellular multiplication power will be reduced.6,17 Tests such as NMR are not able to detect the physeal necrotic lesion in the initial period of fragmentation. In more advanced phases it is able to detect the presence of physeal bridges, W or M wave-shaped deformities or the presence of epiphyseal-metaphyseal bone cysts.8,20 Nevertheless, NMR is unable to really show the residual capacity of the physis for growth21 or to determine germinal cell loss. The actual power of growth may only be detected a posteriori, when secondary bone alterations occur such as maintained reduced growth of the femoral head. These alterations include femoral length discrepancy, which may amount to 5 cm,5,10,12,19,22 relative excessive growth of the greater trochanter12,22–25 or the progressive deformity of the head during the reconstruction phase,5 with flattening and extrusion6,8 (Figs. 3 and 4). Several authors23,24 found that ovoid heads had a physeal lesion that caused the deformity. They therefore described ovoid heads (classes III and IV) that were larger and underwent irregular growth.
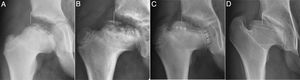
Series of X-ray images of a cases of Perthes with onset at 4 years old. (a) Early re-ossification phase developing over 18 months. Continuous vertical line or Perkins’ line. The discontinuous line marks the cephalic physis. (b) Start of the physeal angulation and the incipient appearance of 2 epiphyseal re-ossification nuclei. (c) Note the greater extrusion, physeal closure of the lateral nucleus with white arrows and productive physis in the medial nucleus with black arrows. A chondral zone without ossification is visible between both nuclei. (d) Final result at 16 years. Coxa magna, flat and extruded. Showing maximum physeal angulation, cephalic extrusion and trochanter overgrowth. Stulberg grade IV.
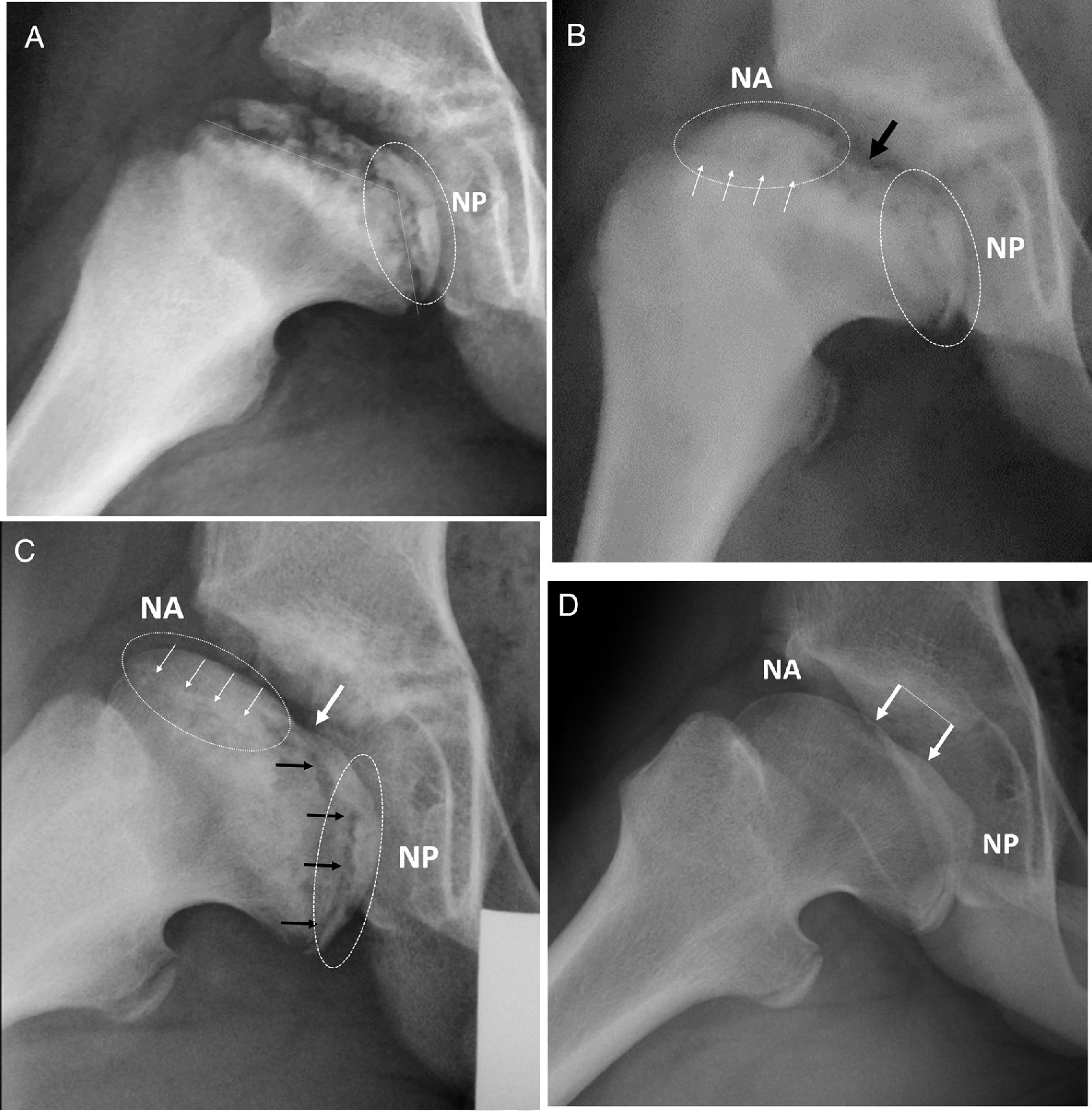
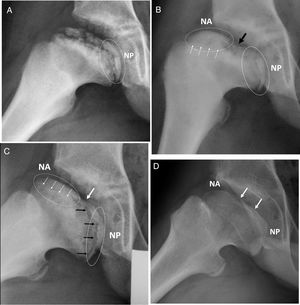
Series of X-ray images of the previous case in lateral projection. (a) Re-ossification phase after 2 ears’ development from the start. Note the physeal angulation under the discontinuous line. NP: epiphyseal re-ossification nucleus in posterior location. (b) The anterior (NA) and posterior (NP) re-ossification dual nuclei are now visible. The black arrow indicates the central zone without re-ossification between both nuclei. The white arrows indicate loss or early physeal closure. (c) Note the physeal asymmetry with closure of the anterior hemiphysis (white arrows). The posterior hemiphysis is still productive and growing (black arrows). Progressive ovalisation with both epiphyseal nuclei moving apart. (d) Final result, Stulberg IV. The arrows indicate the central flat ossified zone after growth of the posterior nucleus.
Our observation of the most ovoid cases, Stulberg class IV, showed that the gradual flattening and ovalisation of the epiphysis may be caused by asymmetric growth that is surely due to the irregular growth of the physis.6 In the same way that the greater trochanter grows, the part of the head where the physis was not affected may also grow. This could be described as excessive growth relative to the posteroinferior quadrant of the femoral head. Bowen4 described 2 types of physeal arrest: one in the lateral zone and the other in the central zone of the physis. He found that only the lateral lesion caused an ovoid head, thereby explaining that the physis is the cause of the final oval shape. The results of our series also corroborate that this partial physeal arrest, caused in an isolated part of the head, and more specifically in the anterolateral quadrant, is the cause of the oval shape. Its final extension varies from one patient to another, and this would explain why similar degrees of bone necrosis seen in hip X-ray images cause different ovoid morphologies. 3 dimensional imaging studies as well as the examination of human anatomical specimens show that there is a zone of greater deformity and flattening in the anterolateral quadrant of the femoral head.11 On the contrary, the posteromedial zone is not damaged and it is this zone that finally grows and protrudes during the final phase of re-ossification.6
The data reported here are conclusive, and they show the alteration in cephalic growth when the inferior and superior lengths of the femoral neck are compared. The harmonious growth of both lengths together with the normal growth in height of the epiphysis leads to a spherical head. In cases of Legg-Calvé-Perthes disease, the anterolateral physeal lesion prevents the growth of the superior distance of the neck, which hardly increases during the process, while it does grow on the healthy side (P < .05). On the other hand, the physis underlying the posteroinferior quadrant remains intact and grows at a normal velocity, with increases in the inferior distance of the neck that are similar to those in the control group (P > .05). This cephalic growth asymmetry means that the ovalisation index increases throughout infancy, even beyond the necrotic process. Meanwhile, the ovalisation index of the control group remains close to 1.4 because both lengths grow harmoniously, the inferior distance of the neck and the superior distance of the neck (Fig. 1).
The same occurs in the lateral projection, where the index always remains below 100 in the control cases. These healthy femoral heads with symmetrical growth show similar increases in the anterior distance of the neck and in the posterior distance of the neck. On the contrary, the heads with Perthes have an index in progression from the initial 104 up to 112 at the end of growth. The physeal arrest in this projection arises in the anterior hemiphysis of the femoral head. The result of this is less growth of the anterior distance of the neck while the posterior length remains intact (the posterior distance of the neck) as the posterior hemiphysis is healthy (Fig. 1).
The ovalisation indexes vary when we compare Stulberg classes III and IV. Although in the first measurement the indexes are the same in both groups (flattening due to bone collapse), as the disease progresses the indexes increasingly diverge, and it is higher in class IV (ovalisation due to physeal growth).
The length of the physis is equivalent to cephalic diameter, and it too progressively increases in the cases. The most logical explanation is that the medial physis, which is undamaged, grows normally or in a way that is increased by the hypervascularisation of the process. We observe that in the initial phase the difference in diameter between the heads of the control group and those of the Perthes amounted to 8.6 mm, while at the end of growth the Perthes’ heads were 12 mm, 29% less (P < .05). As may be seen in the data, the differences gradually increased, even after the necrotic process in the reconstruction phase had ended. This finding would be an unmistakable sign that the physis, at least in its posterior and medial zone, continued to grow. It was also found that the epiphysis is lower at its central point, and at the end of growth it is 6.6 mm lower in Perthes’ cases. Thus the head at the end of growth in ovalised Perthes’ cases is 12 mm broader and 6.6 mm lower.
The radiographic image of a healthy physis is that of a more or less irregular translucent line, although it has a spherical shape and inferior concavity.6 Its appearance is similar in both projections. As several authors have also described, in this series we found a central angle that produced an angular image with the central vertex8,20 (Fig. 3). This has been said to be associated with a poor final prognosis in terms of sphericity,6 and this agrees with our results. Study of the intraphyseal angle shows a gradual increase as ovalisation progresses. This angle is consistently associated with the closure of the anterolateral hemiphysis, which thereby seems to become more horizontal. Physeal curving also occurs in the lateral projection, and the hemiphysis that closes early in the anterior half. The posterior part continues to grow normally, deforming the epiphysis and causing gradual ovalisation, while in the most intense case it also causes central flattening. This flattened zone corresponds to the part of the epiphysis located where the angle is maximum, or the central zone between both physeal hemibranches. The final results is a Stulberg class IV head.
The majority of authors describe better results in patients with early onset of the disease, due to the advantage of having an open physis that was able to remodel the deformities of a necrotic head. Nevertheless, this is true in cases with a physis that grows regularly and symmetrically.5,25 In cases with an asymmetric physeal lesion the result will necessarily be the contrary. The younger the patient, the greater the final deformity. This fact was found in our series, where in spite of a very young average age of 3.9 years, the results consisted of congruent aspherity. Thus Bowen5 described how the 100 cases in his series with a physeal lesion had poor results in spite of having commenced prior to the age of 6 years, and he also stated that the cause would have to be a physis with altered growth.
The appearance of a dual epiphyseal re-ossification nucleus at some time during the disease is a radiological sign that has not been previously described. We were only able to observe this in the ovalised cases (Figs. 3 and 4). Both nuclei develop in parallel and independently, merging only in the final moments of development. However, in some cases they leave a central zone without re-ossification, and this coincides with the point where the physis is at the greatest angle. Finally, this central unossified zone leave a radiological image of osteochondritis. The dual re-ossification nuclei was found in 90% of the cases of ovalised hips. This radiological sign is strongly associated with the most ovalised cases, where it is also detected more persistently over time. 70% of these Perthes’ cases keep it after the 6 years of development, and it is more common in Stulberg grade IV cases.
While in anteroposterior projection an external nucleus and another medial one can be seen, in lateral X-ray imaging the nuclei are in the anterior and posterior parts. When both projections are combined we can conclude that there are only 2 re-ossification nuclei, and that they are located in the anterolateral and posteromedial quadrants of the cephalic sphere, and it was possible to confirm this in checks using NMR imaging. While the anterolateral quadrant of the physis suffers loss and early closure, the posteromedial quadrant of the physis continues to be productive. They behave like two tectonic plates of the earth which are moving apart. The epiphyseal tissue between both nuclei is chondral tissue and is the last to re-ossify. This is the zone of the head which undergoes the most flattening.
The data show that the excessive size of the head causes its extrusion beyond the acetabular limit. The Reimers’ index gradually increases during the illness, so that the head will be extruded as its anomalous growth continues. The surface of the head that is covered by the acetabulum is similar in both groups, the cases of disease and the controls. This means that the increase in the size of the head causes it to protrude due to excessive size rather than because of subluxation, and some studies16 show that the shape of the acetabulum flattens at the end of the disease. We hypothesize that in the final phases of growth the acetabulum, once the head has r-ossified, takes on the flat shape of the head. The initial rule is the opposite, where the necrosed femoral head takes on the spherical shape of the acetabulum, in the theory of containment.
Many authors have studied the intra- and inter-observer reproducibility of radiographic hip measurements,3,8,16,24,26–28 even in cases of studies using NMR.8 Measurements of the width, length and sphericity of the femoral head, or measurements of the acetabulum, have shown a high degree of correlation between observers. The results of these studies therefore offer sufficient statistical support for validations in similar measurements, such as the present study. This work has omitted to repeat the said reproducibility studies, and we carried out the radiographic measurements directly.
To conclude, we are able to say that Perthes’ cases which undergo a gradual increase in the ovalisation index greater than 1.4 run the risk of developing congruent aspherical heads, especially if they also show physeal loss in the anterolateral zone, progressive intraphyseal angulation and the presence of dual nuclei.
These 4 radiological findings together may be taken as signs of a poor prognosis, with the risk of developing Stulberg class III and IV oval heads.
Further studies are necessary to determine whether hemiepiphysiodesis of the posteromedial quadrant, which would be the cause of asymmetrical overgrowth of the femoral head, could prevent ovalisation.
Level of evidenceLevel of evidence III, control cases.
Conflict of interestsThe authors have no conflict of interests to declare.
Please cite this article as: Abril JC, Montero M, Ismael MF. Enfermedad de Legg-Calvé-Perthes. Estudio de la anesfericidad congruente causada por la lesión fisaria. Rev Esp Cir Ortop Traumatol. 2021;65:116–123.