Computer-assisted surgery application in total knee arthroplasty (TKA) has shown more accurate implant alignment compared with conventional instrumentation and is associated with more homogeneous alignment results. Although longer implant survival and superior clinical outcomes should be expected from navigated TKA, currently available evidence does not support this hypothesis. The aim of this study was to compare navigated TKA with conventional TKA regarding clinical and radiological outcomes after a 3-year follow-up under the hypothesis that navigated TKA would provide better outcomes than conventional TKA.
Material and methodIn a prospective multicentre study, 119 patients underwent navigated TKA and 80 patients received conventional instrumentation. Patients were evaluated at the baseline and at postoperative months 3, 12, 24, and 36. Analysis included the American Knee Society Score (KSS), Western Ontario and McMaster Universities Osteoarthritis Index (WOMAC), Short Form-12 (SF12) Health Survey, and radiographic assessment.
ResultsAll clinical scores improved significantly for all patients during the follow-up but were significantly better in the navigation group.
The percentage of patients showing a mechanical axis between 3° of varus and 3° of valgus was significantly higher in the ATR group (93%) than in the conventional TKA group (71%) (p<.01).
ConclusionsThe use of computer-assisted surgery in TKA provides more accurate mechanical alignment and superior short-term functional outcomes compared to conventional TKA.
La navegación en la artroplastia total de rodilla (ATR) ha demostrado obtener una alineación de implantes más precisa comparada con la instrumentación convencional. Aunque se debería esperar una supervivencia más prolongada de los implantes y resultados clínicos superiores mediante la cirugía navegada, la evidencia disponible no apoya esta hipótesis. El objetivo de este estudio fue comparar los resultados clínicos y radiológicos de la ATR navegada con la ATR convencional tras un seguimiento de 3 años bajo la hipótesis de que la navegación proporcionaría mejores resultados.
Material y métodoEstudio prospectivo multicéntrico de 119 pacientes intervenidos de ATR navegada y 80 pacientes con instrumentación convencional. Todos ellos fueron evaluados preoperatoriamente, a los 3, 12, 24 y 36 meses. El análisis incluyó los cuestionarios Western Ontario and McMaster's Universities Osteoarthritis Index (WOMAC), Knee Society Score (KSS) y Short Form-12 Health Survey (SF-12), además de la evaluación radiográfica.
ResultadosTodas las puntuaciones clínicas mejoraron para todos los pacientes durante el seguimiento, pero fueron significativamente mejores en el grupo de navegación.
El porcentaje de pacientes que mostraban un ángulo mecánico femorotibial comprendido entre 3° de varo y 3° de valgo fue significativamente mayor en el grupo de ATR navegada (93%) que en el grupo de ATR convencional (71%) (p<0,01).
ConclusionesEl uso de la cirugía asistida por ordenador en la ATR proporciona una alineación mecánica más precisa y resultados funcionales superiores a corto plazo en comparación con la cirugía convencional.
Achieving good long-term clinical and functional outcomes after total knee arthroscopy (TKA) depends on various factors; in particular the correct alignment of the implant and appropriate balance of the soft tissue. Imageless computer-assisted surgery (CAS) was introduced in the nineteen nineties as a navigation method to help surgeons plan and perform surgical procedures with more precision without using computerised tomography imaging. A CAS system uses infrared communication to spatially locate the patient's limb and, by calculations performed by the computer, enables the surgeon to plan bone cuts before making them, check them when made and assess the postoperative alignment of the implant components. The purpose of using CAS in TKA is to achieve a standardised technique for more precise positioning and alignment of implants compared to the use of conventional instruments.1 Navigation has shown more homogeneous outcomes in alignment on the sagittal plane with a greater number of implants placed between 3° of varus and 3° of valgus compared to conventional TKA.2–4 However, their efficacy in achieving better sagittal alignment remains controversial.3,4 CAS also enables appropriate balancing of the ligaments and of the flexion and extension gaps using the space balancing technique and sequential soft tissue release.5 Although in theory that could result in longer duration of the implant and better clinical outcomes, the current evidence does not corroborate this hypothesis. A meta-analysis series on implant alignment2–12 concluded that navigation promotes better outcomes. In terms of clinical outcomes, however, there have been controversial reports in the literature, mainly due to the great variety and heterogeneity of questionnaires and measurements used in the studies gathered.7–10 In 2014, Rebal et al.11 published the first meta-analysis that included 21 studies with a level of evidence I, demonstrating that the use of navigation in TKA achieves better alignment of the mechanical axis and improved short and medium term functional outcomes, analysing the Knee Society Score (KSS) questionnaire exclusively.
The aim of this study was to compare, after 3-years’ follow-up, the clinical and radiological outcomes of navigated knee arthroscopies with those of prostheses implanted using the conventional technique, with the hypothesis that navigation provides better outcomes.
Material and methodsSample descriptionIn a prospective multi-centre study performed in 3 hospitals, 199 patients were operated by 3 surgeons, one in each hospital, to implant a TKA. The inclusion criteria for both groups were primary or secondary gonarthrosis where conservative treatment had failed. One hospital used the conventional technique with posterior cruciate-retaining (CR) prostheses in 80 patients, another used navigation and CR prostheses in 29 patients and navigation and posterior-stabilised (PS) prostheses in 41 patients, and the third (49 patients) used navigation and PS prostheses. All 3 surgeons had wide experience in knee arthroplasty, using more than 150 prostheses annually. All the patients included signed their informed consent. One of the patients, from the conventional surgery group, developed a deep infection that led to removal and two-step replacement of their prosthesis. Therefore, 198 patients were eventually suitable for the study. The aetiology was primary arthrosis in 194 cases, 3 cases (2 from the navigated surgery group and one from the conventional group) had secondary post-traumatic arthrosis and one, from the navigation group, had rheumatoid arthritis. In the distribution by sex, there were more females (n=143, 72.3%) than males (n=55; 27.7%). Most of the patients were of advanced age, the range was from 41 to 87 years (mean: 71.4 years; standard deviation [SD]: 7.8 years) and their body mass index (BMI) was 31.8kg/m2. The number of left and right operated knees was 83 (42%) and 115 (58%), respectively. According to Ahlbäck's classification system13 there were 71 grade 1 cases, 79 grade 2 cases, 24 grade 3 cases, 17 grade 4 cases, and 7 grade 5 cases; 156 knees had a varus deformity, 18 a valgus deformity and 24 had a normal axis, which was considered to be a mechanical femorotibial angle of 180°.
InterventionAll the patients were implanted with an Apex® (OMNI lifeScience, East Taunton, MA, USA) total knee arthroplasty using a standard medial parapatellar approach with patellar eversion. All the tibial components were cemented, while the femoral components were cemented in the PS prostheses and not in the CR. The space balancing technique with sequential soft tissue release was used for both the navigated operations and those that were performed with conventional instruments. The Total Knee Surgetics® (PRAXIM SA, La Tronche, France) version 7.9 navigation system was used for all the computer-assisted procedures. This is a closed navigation system, with no previous images, that uses kinematic analysis of the hip, knee and ankle and anatomical mapping of the knee joint surfaces to build a working model. After placing the infrared sensors by bicortical fixation in the distal femoral metaphysis and in the proximal tibial metaphysis and resecting the osteophytes, a tibial cut was made at 90° over the mechanical axis of the tibia on the coronal plane with 4° posterior slope on the sagittal plane and, applying the dependent cut technique by sequential release with a distractor, the femoral cut was calculated to achieve symmetrical extension and flexion gaps of 90° with equal soft tissue tension. The mean surgery time was 78min for the conventional arthroplasty and 83min for the navigated operations (p<.02). All the patients followed the same postoperative rehabilitation regimen, with early mobilisation and immediate weight-bearing.
Follow-up and evaluationThe patients were evaluated at the baseline and at 3, 12, 24 and 36 months after the surgery. The Western Ontario and McMaster's Universities Osteoarthritis Index (WOMAC), KSS and the Short Form-12 Health Survey (SF-12) were completed in all cases. Simple anteroposterior and lateral views were taken for the radiological assessment, and standing telemetry to measure the hip-knee-ankle angle. The measurements were taken digitally on X-rays taken with the lower limbs fully extended, with the anterior tibial tuberosities facing forward and the medial malleoli separated 30cm. The mechanical angle was determined blindly by 2 independent observers connecting the centre of the femoral head, the centre of the knee and the centre of the ankle.
The analysis included zonal assessment of the implant fixation integrity in the areas defined in the Knee Society Total Knee Arthroplasty Roentgenographic Evaluation and Scoring System.14 The radiological assessment of the osteointegration of the implant was classified according to the criteria presented by Engh et al.15
The study was approved by the Regional Ethics Committee (identification number: CP03/2014).
Statistical analysisThe Kolmogorov–Smirnov test was used to check that all the study variables had a normal distribution. The qualitative variables (navigation, alignment ±3° or not) were compared using the Chi-square test. The Student's t-test was used for the total comparisons of means between the 2 groups—navigation and conventional. The outcomes at the different times of the study were evaluated using the general linear model of repeated measurements, where the intrasubject variables were the 7 evaluation scales, KSS (2), SF-12 (2) and WOMAC (3), measured on 2 occasions—preoperatively and at 36 months—and the intersubject factor was whether or not navigation was used. p values <.05 were considered significant.
The statistical analysis of the data was performed using SPSS 2012 (IBM SPSS Statistics for Windows, version 21.0, IBM Corporation, Armonk, NY, USA).
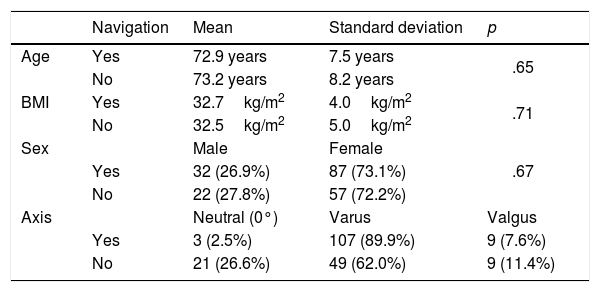
ResultsClinical outcomesThere were no significant differences in the distribution by sex (p=.67), side (p=.68), age (p=.65) and BMI (p=.71) between the 2 groups. The conventional TKA group was characterised by a lower prevalence of preoperative varus alignment compared to the navigated TKA group (Table 1).
Patient characteristics.
| Navigation | Mean | Standard deviation | p | |
|---|---|---|---|---|
| Age | Yes | 72.9 years | 7.5 years | .65 |
| No | 73.2 years | 8.2 years | ||
| BMI | Yes | 32.7kg/m2 | 4.0kg/m2 | .71 |
| No | 32.5kg/m2 | 5.0kg/m2 | ||
| Sex | Male | Female | .67 | |
| Yes | 32 (26.9%) | 87 (73.1%) | ||
| No | 22 (27.8%) | 57 (72.2%) | ||
| Axis | Neutral (0°) | Varus | Valgus | |
| Yes | 3 (2.5%) | 107 (89.9%) | 9 (7.6%) | |
| No | 21 (26.6%) | 49 (62.0%) | 9 (11.4%) |
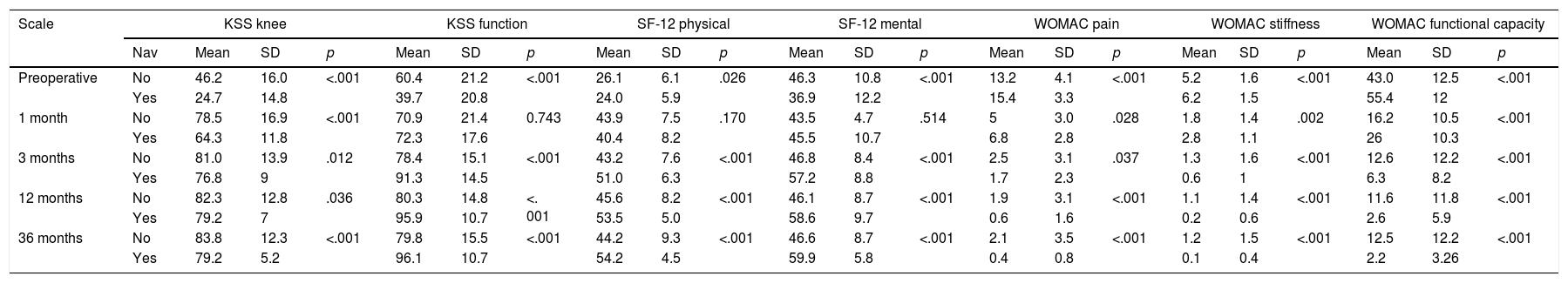
The clinical outcomes are shown in Table 2. There was an improvement in all the clinical parameters measured, which was already significant at the third postoperative month and stabilised in most of the cases at one year's follow-up, and was maintained until the end of follow-up.
Progress of the clinical scales according to surgical technique.
| Scale | KSS knee | KSS function | SF-12 physical | SF-12 mental | WOMAC pain | WOMAC stiffness | WOMAC functional capacity | |||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Nav | Mean | SD | p | Mean | SD | p | Mean | SD | p | Mean | SD | p | Mean | SD | p | Mean | SD | p | Mean | SD | p | |
| Preoperative | No | 46.2 | 16.0 | <.001 | 60.4 | 21.2 | <.001 | 26.1 | 6.1 | .026 | 46.3 | 10.8 | <.001 | 13.2 | 4.1 | <.001 | 5.2 | 1.6 | <.001 | 43.0 | 12.5 | <.001 |
| Yes | 24.7 | 14.8 | 39.7 | 20.8 | 24.0 | 5.9 | 36.9 | 12.2 | 15.4 | 3.3 | 6.2 | 1.5 | 55.4 | 12 | ||||||||
| 1 month | No | 78.5 | 16.9 | <.001 | 70.9 | 21.4 | 0.743 | 43.9 | 7.5 | .170 | 43.5 | 4.7 | .514 | 5 | 3.0 | .028 | 1.8 | 1.4 | .002 | 16.2 | 10.5 | <.001 |
| Yes | 64.3 | 11.8 | 72.3 | 17.6 | 40.4 | 8.2 | 45.5 | 10.7 | 6.8 | 2.8 | 2.8 | 1.1 | 26 | 10.3 | ||||||||
| 3 months | No | 81.0 | 13.9 | .012 | 78.4 | 15.1 | <.001 | 43.2 | 7.6 | <.001 | 46.8 | 8.4 | <.001 | 2.5 | 3.1 | .037 | 1.3 | 1.6 | <.001 | 12.6 | 12.2 | <.001 |
| Yes | 76.8 | 9 | 91.3 | 14.5 | 51.0 | 6.3 | 57.2 | 8.8 | 1.7 | 2.3 | 0.6 | 1 | 6.3 | 8.2 | ||||||||
| 12 months | No | 82.3 | 12.8 | .036 | 80.3 | 14.8 | <. 001 | 45.6 | 8.2 | <.001 | 46.1 | 8.7 | <.001 | 1.9 | 3.1 | <.001 | 1.1 | 1.4 | <.001 | 11.6 | 11.8 | <.001 |
| Yes | 79.2 | 7 | 95.9 | 10.7 | 53.5 | 5.0 | 58.6 | 9.7 | 0.6 | 1.6 | 0.2 | 0.6 | 2.6 | 5.9 | ||||||||
| 36 months | No | 83.8 | 12.3 | <.001 | 79.8 | 15.5 | <.001 | 44.2 | 9.3 | <.001 | 46.6 | 8.7 | <.001 | 2.1 | 3.5 | <.001 | 1.2 | 1.5 | <.001 | 12.5 | 12.2 | <.001 |
| Yes | 79.2 | 5.2 | 96.1 | 10.7 | 54.2 | 4.5 | 59.9 | 5.8 | 0.4 | 0.8 | 0.1 | 0.4 | 2.2 | 3.26 | ||||||||
SD: standard deviation; KSS: Knee Society Score; Nav: navigation; SF-12: Short Form-12 Health Survey; WOMAC: Western Ontario and McMaster's Universities Osteoarthritis Index.
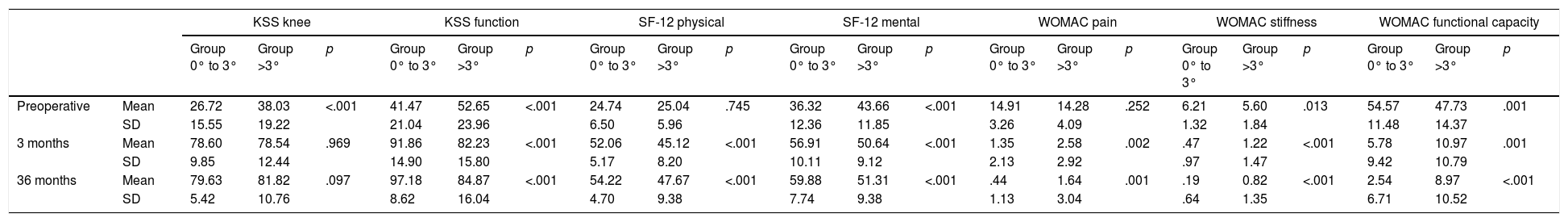
The improvement was significantly greater in the navigated group, which started from poorer mean baseline values on all the scales. At the end of follow-up, the navigated TKA group showed significantly better outcomes on all the scales, with the exception of the KSS specifically for the knee, in which the conventional TKA group obtained higher scores (83.8 vs 79.2 points, p<.01) due to a better range of flexion with a mean of 125° and SD of 10° compared to 110° and SD of 15°, respectively. Regardless of the surgical technique, the patients with a femorotibial mechanical angle between 3° of varus and 3° of valgus had better scores on all the scales throughout the follow-up—apart from the specific KSS, where significant differences were only found preoperatively—than those with alignments outside these values (Table 3).
Progress of the clinical outcomes according to the mechanical femorotibial angle.
| KSS knee | KSS function | SF-12 physical | SF-12 mental | WOMAC pain | WOMAC stiffness | WOMAC functional capacity | ||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Group 0° to 3° | Group >3° | p | Group 0° to 3° | Group >3° | p | Group 0° to 3° | Group >3° | p | Group 0° to 3° | Group >3° | p | Group 0° to 3° | Group >3° | p | Group 0° to 3° | Group >3° | p | Group 0° to 3° | Group >3° | p | ||
| Preoperative | Mean | 26.72 | 38.03 | <.001 | 41.47 | 52.65 | <.001 | 24.74 | 25.04 | .745 | 36.32 | 43.66 | <.001 | 14.91 | 14.28 | .252 | 6.21 | 5.60 | .013 | 54.57 | 47.73 | .001 |
| SD | 15.55 | 19.22 | 21.04 | 23.96 | 6.50 | 5.96 | 12.36 | 11.85 | 3.26 | 4.09 | 1.32 | 1.84 | 11.48 | 14.37 | ||||||||
| 3 months | Mean | 78.60 | 78.54 | .969 | 91.86 | 82.23 | <.001 | 52.06 | 45.12 | <.001 | 56.91 | 50.64 | <.001 | 1.35 | 2.58 | .002 | .47 | 1.22 | <.001 | 5.78 | 10.97 | .001 |
| SD | 9.85 | 12.44 | 14.90 | 15.80 | 5.17 | 8.20 | 10.11 | 9.12 | 2.13 | 2.92 | .97 | 1.47 | 9.42 | 10.79 | ||||||||
| 36 months | Mean | 79.63 | 81.82 | .097 | 97.18 | 84.87 | <.001 | 54.22 | 47.67 | <.001 | 59.88 | 51.31 | <.001 | .44 | 1.64 | .001 | .19 | 0.82 | <.001 | 2.54 | 8.97 | <.001 |
| SD | 5.42 | 10.76 | 8.62 | 16.04 | 4.70 | 9.38 | 7.74 | 9.38 | 1.13 | 3.04 | .64 | 1.35 | 6.71 | 10.52 | ||||||||
SD: standard deviation; KSS: Knee Society Score; SF-12: Short Form-12 Health Survey; WOMAC: Western Ontario and McMaster's Universities Osteoarthritis Index.
At 36 months, the radiological examination confirmed good fixation of the implants in all the patients. The characteristics of radiological osteointegration of the implants were also optimal in all cases, both on the coronal and the sagittal planes, no implant migration or progressive radiolucencies were observed in any of the patients. The percentage of patients who showed optimal postoperative alignment, i.e., a femorotibial mechanical angle between 3° of varus and 3° of valgus, was significantly better in the navigated TKA group at 93% (111 patients), compared to 71% (56 patients) in the conventional TKA group (p<.01). Deviation with respect to the neutral mechanical axis was .77±4.3° in the conventional group and 1.19±5.8° in the CAS group (p=.02).
The complication rates were similar in the 2 groups. There was one seroma in the conventional TKA group and a superficial infection in the navigated TKA group which was resolved with antibiotic treatment. No complications related to the use of screws in the navigated knees were observed. For both surgical procedures, survival at 36 months was 100%, except for the patient who was withdrawn from the study due to a deep infection.
DiscussionCAS has shown advantages as a surgical instrument to improve the accuracy of postoperative alignment and reduce the number of atypical values.2–11 Although some authors have obtained disparate results,16–18 there is general consensus that postoperative coronal alignment is the most important factor towards guaranteeing the survival and prevent aseptic loosening of the knee arthroplasty.19,20 Although the follow-up period of our study was not sufficient to assess the survival of the implants, better clinical outcomes were found on all the scales evaluated when the mechanical axis was within the interval of 3° from the neutral mechanical axis. Although some authors have found that alignment has no influence on clinical outcomes,21 our outcomes coincide with those of Kamat et al.,22 with navigation as well, at 3-year follow-up, but this finding appeared earlier in our series, already manifesting from the third postoperative month. The effect of navigation on the functional outcomes of TKA remains controversial and the outcomes obtained to date are based largely on short term studies with a limited number of cases, like ours. The meta-analyses undertaken to date have reviewed studies that are very heterogeneous in methodology and clinical questionnaires. Bauwens et al.,7 for example, with a view to obtaining an appropriate number of studies, included pseudo-randomised, non-randomised and retrospective studies in their meta-analysis and concluded that navigation offers few advantages over conventional surgery. In 2012, a further 2 meta-analyses were published of controlled and randomised studies,8,9 but neither of them included clinical outcomes. In their systematic review of the success, safety and efficacy of navigated TKA, Zamora et al.10 only included clinical outcomes based exclusively on the KSS, and concluded that navigation did not provide better clinical outcomes.
Rebal et al.11 performed a meta-analysis of the KSS scores in the short and medium term and concluded that the use of navigation provided better functional outcomes, but they included studies with a shorter follow-up time than ours, of a maximum 32 months. These outcomes were consistent with those of the meta-analysis performed by Moskal et al.,12 who found that the use of navigation was associated with better KSS and WOMAC scores. Our study has demonstrated better progress in the objective outcomes obtained on the KSS since, although at final follow-up the specific KSS scores were higher in the conventional surgery group because they had better maximum flexion values, the overall positive change was very much higher in the navigation group, which started from a poorer clinical situation. This lower range of flexion was probably due to the fact that the patients who underwent navigated surgery also started from a lower range of preoperative flexion and is not attributable to selection bias, since the technique used was unique in all of the hospitals. The objective clinical measurements were increasingly considered less representative of the outcomes from the patient's perspective.23 In line with this tendency, now more emphasis is placed on the measurements of outcome reported by the patients (PROMs) to define success after joint replacement surgery.24 Most of the studies performed show navigation to have little or no influence over their outcomes. Roberts et al.,25 in a study that compared the greatest number of prosthesis implanted using navigated surgery versus non-navigated surgery, analysed 3329 and 5725 cases respectively, all of which used the same prosthesis model, taken from the New Zealand Joint Registry, and found no differences in Oxford Knee Score (OKS) at 6 month and 5 year follow-up. Singisetti et al.26 undertook a retrospective study of 351 navigated and non-navigated knee arthroplasties with a follow-up of 2 years, analysing the WOMAC and SF-36 scores, and found significant differences only in the SF-36 scores at one year follow-up. However, they found no significant differences in the SF-36 scores between the 2 groups later on. Finally, Song et al.,27 in a randomised, prospective study comparing navigated TKA with conventional TKA analysed the KSS, WOMAC and Hospital for Special Surgery Scores (HSS) and found no differences after a follow-up of 9 years. In our study, however, the progress of the WOMAC and SF-12 scores was much more satisfactory in the navigated TKA group, with significant differences observed after the third postoperative month. These outcomes would not be attributable to the stability of the implant, as demonstrated by various studies that observed no significant differences in postoperative laxity of the implanted knees or any influence of this laxity on the clinical outcomes according to the type of technique employed.28–30
The limitations of this study included the absence of a controlled process of randomisation and a short follow-up period. The patients underwent surgery in 3 centres performed by 3 different surgeons using 2 types of implants. However, it is unlikely that the use of PS or CR implants implies a bias, since the literature shows no statistically significant differences in clinical and radiological outcomes between either type of prosthesis.31
ConclusionsThe use of CAS in TKA provides more accurate mechanical alignment and superior functional outcomes short term compared to conventional TKA.
Level of evidenceLevel of evidence II. Prospective comparative study.
Ethical responsibilitiesProtection of human and animal subjectsThe authors declare that no experiments were performed on humans or animals for this study.
Confidentiality of dataThe authors declare that they have followed the protocols of their centre of work regarding patient data confidentiality.
Right to privacy and informed consentThe authors declare that no patient data appear in this article.
Conflict of interestsThe authors have no conflict of interests to declare.
Please cite this article as: Martín-Hernández C, Sanz-Sainz M, Revenga-Giertych C, Hernández-Vaquero D, Fernández-Carreira JM, Albareda-Albareda J, et al. Artroplastia total de rodilla navegada versus convencional; estudio prospectivo a 3 años de seguimiento. Rev Esp Cir Ortop Traumatol. 2018;62:282–289.