We evaluated the radiographic and clinical functional results of K-wire fixation in the treatment of displaced lateral condyle fractures of the humerus.
Materials and methodsA prospective longitudinal study was undertaken in our hospital during the period December 2010•December 2014. A total number of 85 children (18 girls and 67 boys) mean age 7.76 years; range 2•13 years with displaced (>2mm) lateral condyle fractures of the humerus. All the patients were treated by close reduction and internal fixation with two K-wires for three weeks. The fractures were classified according to the criteria by Milch and Badelon and functional results were evaluated according to the criteria by Hardacre et al. The mean follow-up period was 24 months (range 20•28 months).
ResultsAll children achieved union in a mean time of 3 weeks (range from 2.5•6 weeks). Functional results were excellent in 91.75% children and good in 7.05% children. Full range of elbow motion was achieved in all the patients. None of the patients had instability postoperatively. Post-operatively, 5.88% children got pin tract infection, which was superficial and healed after removing pins and oral antibiotic administration.
ConclusionPercutaneous K-wire fixation is an effective treatment for unstable displaced lateral condylar fractures of the humerus in children. If fracture displacement after closed reduction exceeds 2mm, open reduction and internal fixation is recommended.
Evaluamos los resultados radiográficos y funcionales clínicos de la fijación del alambre K en el tratamiento del desplazamiento de fracturas de cóndilo lateral del húmero.
Materiales y mèc)todosSe realizó en nuestro hospital un estudio prospectivo longitudinal durante el periodo diciembre 2010-diciembre 2014, incluyendo a un total de 85 niños (18 niñas y 67 niños) con una edad media de 7,76 años y un rango de 2 a 13 años con desplazamiento (>2mm) del cóndilo lateral del húmero. Se trató a todos los pacientes con reducción cerrada y fijación interna mediante 2 alambres K durante 3 semanas. Las fracturas se clasificaron con arreglo a los criterios de Milch y Badelon, y se evaluaron los resultados funcionales conforme a los criterios de Hardacre et al. El periodo de seguimiento medio fue de 24 meses (rango de 20 a 28 meses).
ResultadosSe logró la unión en todos los niños en un tiempo medio de 3 semanas (rango de 2,5-6 semanas). Los resultados funcionales fueron excelentes en el 91,75% de los niños, y buenos en el 7,05% de ellos. Se logró el rango completo del movimiento del codo en todos los pacientes. Ninguno de los pacientes reflejó inestabilidad postoperatoria. A nivel postoperatorio, el 5,88% de los niños padeció infección del tracto del clavo, de manera superficial, que se resolvió tras la extracción del mismo y la administración de antibióticos orales.
ConclusiónLa fijación percutánea del alambre K constituye un tratamiento efectivo para el desplazamiento de las fracturas de cóndilo lateral del húmero en niños. En casos en que el desplazamiento de la fractura tras reducción cerrada excediera de 2mm, se recomienda reducción abierta y fijación interna.
Pediatric lateral condylar elbow fractures account for 15 percent of elbow.1,2 The peak age of injury is six years.3 It is the second most common fracture about the elbow in children. This diagnosis may be less obvious both clinically and radio logically. A poorly treated lateral condylar fracture is more likely to result in a substantial functional loss of elbow motion.4 Several reports have recommended open reduction and internal fixation as the effective procedure for unstable fractures to prevent further displacement, nonunion, and malunion.4•6 However, only a few reports have focused on closed reduction and internal fixation of lateral condylar humeral fractures.7,8 We believe that satisfactory reduction and secure fixation of a lateral condylar fracture of the humerus in a child can often be achieved by means of closed reduction and internal fixation without the need for open reduction. We prospectively studied the use of closed reduction and internal fixation as the initial treatment for a group of displaced unstable lateral condylar humeral fractures.
Material and methodsThis prospective study was carried out at orthopedics department from December 2010 to July 2014. It was approved by institutional medical ethics committee. A written informed consent was obtained from all the patients (by their parents). A total of 85 children (18 girls and 67 boys) with fractures lateral condylar of humerus who were followed-up were included in this study. The patients were aged between 2 and 13 years with the mean age of 7.76 years.
Inclusion criteria
- 1
Age between 2 and 13 years.
- 2
The mean follow-up period was 24 months (range 20•28 months).
- 3
All cases unilateral and close fracture.
- 4
Displaced >2mm, unstable with or without rotation.
- 5
Failure of conservative treatment.
- 6
Late cases of unsatisfactory deformity with poor functional results.
Exclusion criteria
- 1
Age more than 13 years.
- 2
Open fractures
- 3
Cases with polytrauma.
- 4
Fractures manageable by immobilization alone which were stable.
- 5
Multiple bones fracture involving the same elbow.
- 6
Fractures with dislocation of elbow.
Following anesthetic assessment, all patients with a displaced lateral humeral condyle fracture were consented and listed for close reduction and percutaneous fixation with Kirschner wires (K-wires) in the operating theater. A single dose of intravenous prophylactic antibiotics was administered at the anesthetic induction, as per hospital policy, and tourniquet was used. The reduction was stabilized with two divergent K-wires that were left outside the skin. Subsequently, an above elbow plaster of paris (POP) in neutral position was applied. Patients were followed up weekly until radiological union of the fracture was evident after three weeks and thereafter, the wires and the POP were removed in the outpatient department without the use of general or local anesthetic. Following the removal of plaster, all patients were mobilized with intensive physiotherapy focusing on elbow full range of movement (ROM), mainly with active movement exercises.
The final clinical and radiographic examinations of cases were performed after two year in average. All injuries were associated with low-energy traumas, resulting from falls. No primary neuro-vascular injury was observed following the fracture. Left elbow was involved in forty five patients and right elbow in forty patients. Other injuries were present in addition to the lateral humeral condyle in eight patients. For evaluation of fractures, Milch and Badelon classifications were used.8•11 In the Milch classification, anatomical position of the fracture and its relation with capitello-trochlear groove are evaluated. A Milch type I fracture extends through the ossification center of the lateral condyle and exits at the radiocapitellar groove whereas a Milch type II fracture exits at the medial of the capitellotrochlear groove. In Type II fractures, angulations as well as lateral translation of the olecranon and upper fragment of the radius are present. In the Badelon classification, degrees of displacement are evaluated. A Badelon type I fracture is undisplaced, and a type 2 fracture is displaced <2mm, and a type 3 fracture is displaced >2mm. A type 4 fracture is completely disconnected, and mostly displaced; even the fragment may be rotated. Patients were evaluated after a two-year monitoring period since it has been reported that bone remodeling and improvement in motion of joints are completed in two years in the elbow injuries of children.8•14 During the final examinations, all patients were interviewed and a thorough examination was performed. Clinical outcomes were evaluated according to the criteria by Hardacre et al.12 for the lateral humeral condyle fractures as well as the radiographic criteria. The results were rated as excellent, good and poor. The mean follow-up period was 24 months (range from 20 to 28 months).
Radiographically, full lateral and full anteroposterior images of both elbows were obtained for all patients. Healing of fracture and potential complications were evaluated. Radiographic indication of healing is the visualization of the callus tissue around the fracture on the anteroposterior and lateral views of the elbow. Avascular necrosis, presence of non-union and malunion, and status of the lateral condyle growth plate were also taken into consideration during the evaluation of functional results. Radiographs of the elbow were also evaluated in terms of rotational or angular deformities, and heterotopic ossification. Based on these observations, deformities of elbow were classified as normal, relatively cubitus varus, cubitus varus, pseudo cubitus varus and cubitus valgus. The carrying angle of the injured elbow is reduced in the relatively cubitus varus compared to the other elbow; but still above 0 degrees while in cubitus varus, the carrying angle is below 0 degrees. In pseudo cubitus varus, the lateral condyle is very prominent in the elbow and it is similar to cubitus varus; but the carrying angles are the same at both elbows. In cubitus valgus, the carrying angle is increased compared to the other elbow.
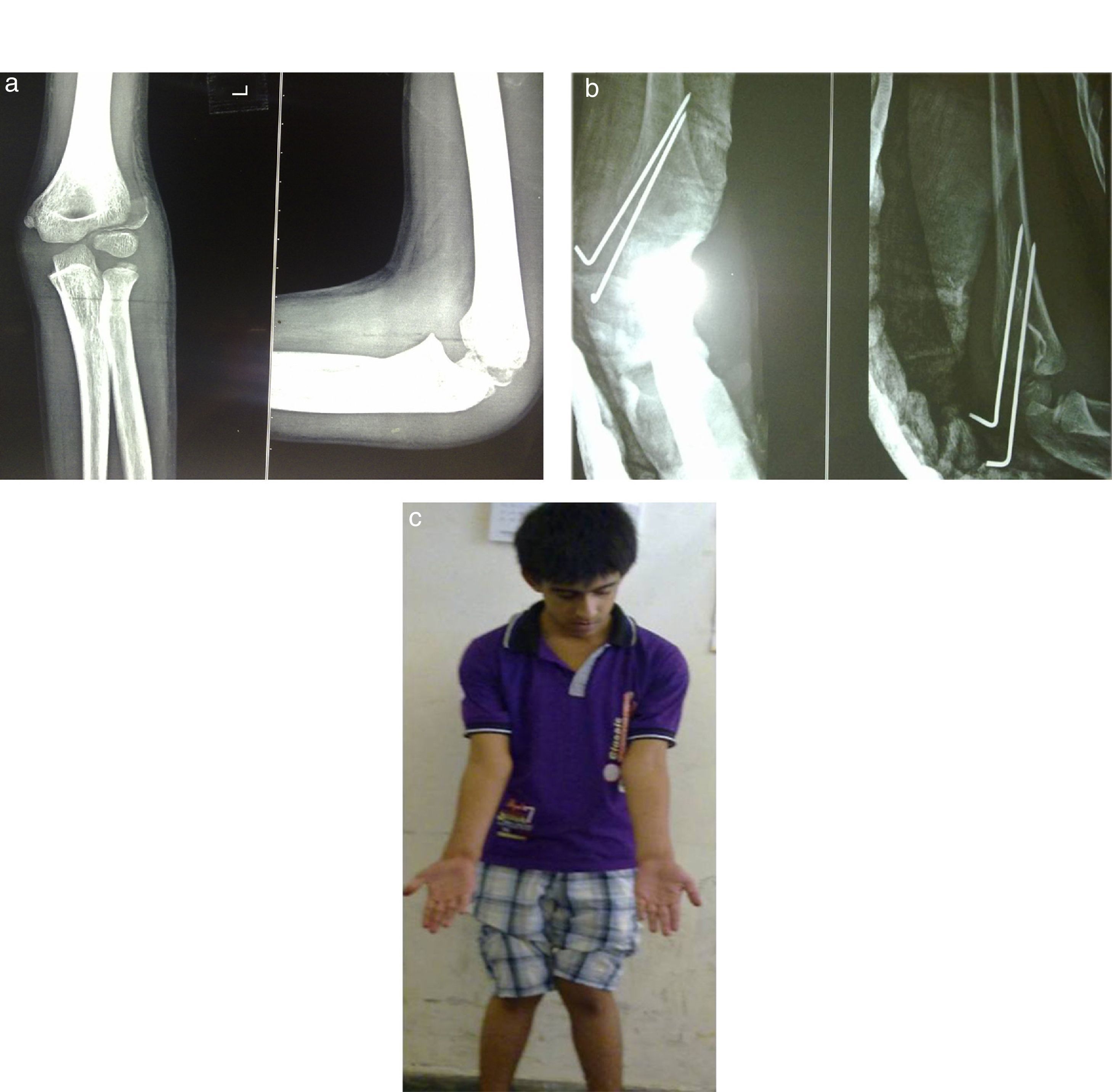
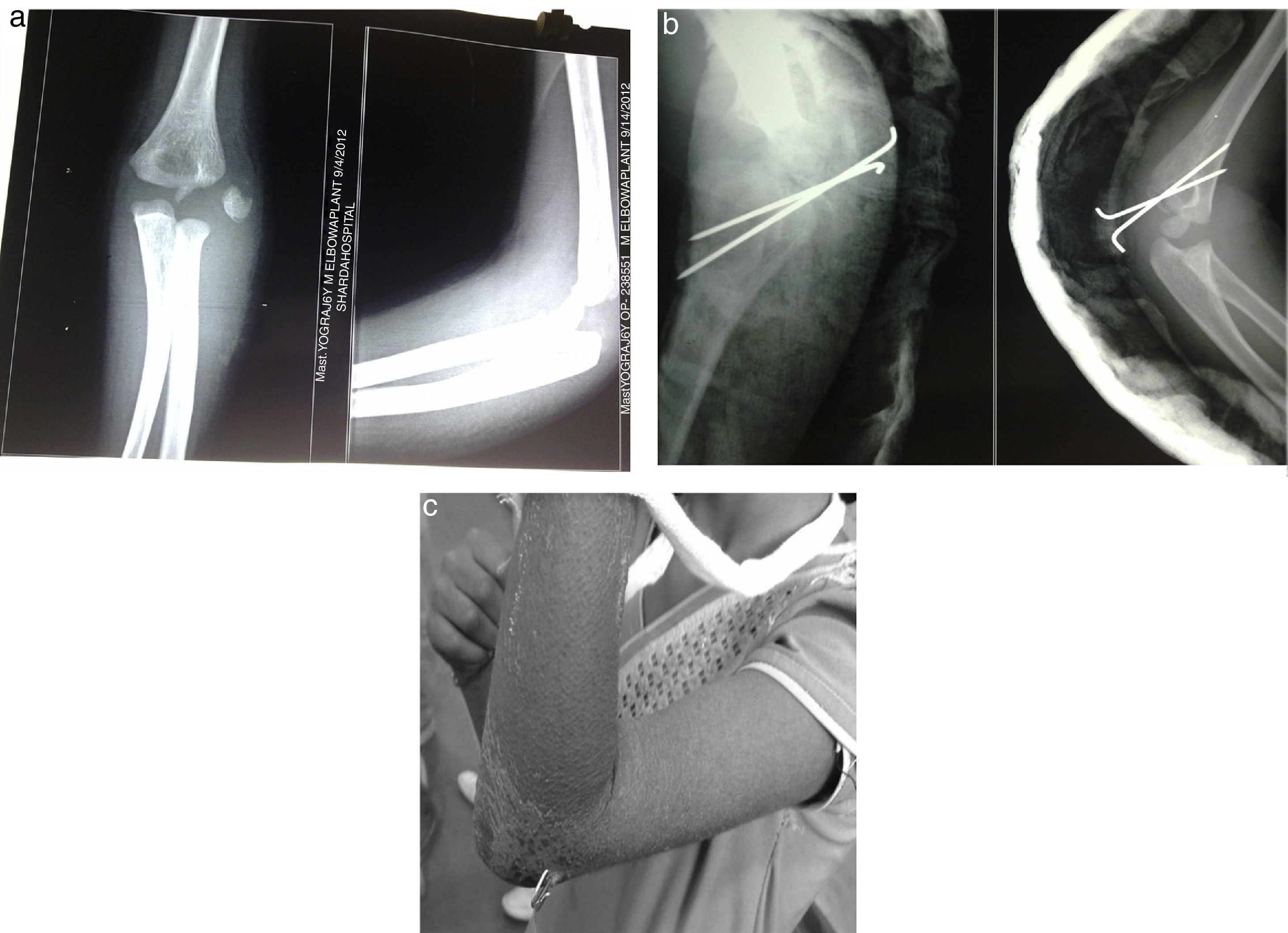
ResultsThere were 85 children in this study, 67 children were male and 18 children were females. The children were aged 2 years to 13 years. There were 45 left sided and 40 right-sided fractures. 54 children had injury during playing, 24 children had met with a road traffic accident and 7 had a fall from a height. All were closed fractures. All the 85 cases were treated by two lateral parallel or divergent K-wires. According to the Milch classification, the fracture was of type 1 in five cases, and type 2 in 80 cases. According to the degree of displacement, 15 of fractures were Badelon type 3 and 70 were Badelon type 4. Close reduction and internal fixation with K-wire were performed on the day of trauma in 57 patients, one day later in 18 patients, within 2•7 days in seven patients and after one week in three patients. Cases treated within 2•7 days were late referrals to our institute. One of the patients who underwent surgery following the first week was treated by closed reduction and long-arm cast; he/she was operated at day 13 due to displacement determined in the fracture. The other two were late referrals. Two K-wires were used for lateral humeral approach and fixation in all cases; placed percutaneously, and the fixation time was limited to three weeks. Percutaneous K-wires were removed without any need for clinical anesthesia at the end of the specified period. After 3 weeks (immobilization time), all patients were mobilized with intensive physiotherapy focusing on elbow full range of movement (ROM), mainly with active movement exercises. No complication was observed during early period. The mean carrying angle in the fractured elbow was 8° (range from 0 to 15°), and 7.8° (range from 5 to 11°) in the other elbow during the late monitoring period. These values had no significant difference. The carrying angles of both elbows were equal in 67 (78.82%) patients (Fig. 1a•c), with a mean difference of 5° in 17 patients (20%). Eight of these cases (9.41%) had relative cubitus varus, three (3.52%) had cubitus valgus. Only one patient (1.17%) had a difference of 11° in the carrying angle between the affected elbow and the other, who had cubitus varus. The intraoperative views showed that the reductions were anatomically performed and maintained. Following the removal of K-wires, no malunion or any arrest of growth in the lateral humeral growth plate was observed. According to Hardacre criteria, the functional results were excellent in 78 fractures (91.75%), good in 5 fractures (5.88%), fair in 2 fractures (2.35%). No poor result was obtained (Fig. 2a•c). Lateral humeral condyle was clinically and radiographically more prominent in 33 patients (38.82%) due to formation of new and extra bones. Review of early radiographs demonstrated that the bone spicules are elevated from the lateral condyle. The spicules were probably osteoperiosteal flaps, and the lateral prominence was depending on the formation of bone between spicule and lateral condyle, the lateral prominence was associated with deformity of pseudo cubitus in the elbow in 11 patients (12.94%). The mean humeroulnar range of motion was 135° for both elbows. The humeroulnar range of motion was similar for both elbows in 64 patients (75.29%), with a difference of 5° in 21 patients (24.70%). A scar tissue wider than 2mm was evident in 35 patients (41.17%); however, patients did not have any complaints. During follow-up, we did not found secondary displacement of wires and loss of reduction. Post-operatively, five (5.88%) patients got pin tract infection, which was superficial and healed after removing pins and oral antibiotic administration. Callus formation was seen in all patients at the three week post-operatively before removing the K-wires. The fracture united in all cases at the three week post-operatively. All patients were followed at eighth weeks, 16 weeks 24 weeks 12 months, 18 months and 24 months. Postoperatively 68.23% had excellent, 29.40% good, 1.17% fair and 1.17% poor results at eight weeks which was improved to 91.75% excellent, 7.05% good, 1.17% fair and no poor result at the final follow-up. In my study, there was an inappropriate fixation in one case where two pins, which is too close and work as one pin, though reduction was maintained and union had occurred without deformity. Child was kept in close follow-up. During this study, complications like vascular injury, compartment syndrome, myositis ossifications, significant mal-union and non-union were not seen.
(a) Pre-operative anteroposterior and lateral view of displaced fracture lateral condyle of humerus in 10 years of old boy. (b) Post-operative A•P and lateral view of fracture lateral condyle of humerus showing fracture fixation with two K wires. (c) Two years follow-up case of fracture lateral condyle of humerus.
(a) Pre-operative anteroposterior and lateral view of displaced fracture lateral condyle of humerus in 7 years of old girl. (b) Post-operative A•P and lateral view of fracture lateral condyle of humerus showing fracture fixation with two K wires. (c) Three weeks follow-up case of fracture lateral condyle of humerus.
This study shows that bone union and good clinical results can be achieved in children with a lateral condylar fracture, and that lateral overgrowth (38.82%) and cubitus varus (9.41%) are the most common residual deformities. Furthermore, these residual deformities persisted at a mean 24 months post injury. However, nonunion, avascular necrosis, fishtail deformity and ROM (range of motion) limitations, which are known to be complications after treating lateral condylar fractures, were not observed in this series.11 Bone healing was achieved in all cases without any limitation in range of motion.
Three patients with delayed union achieved union after 6 months of follow-up. Three cases (3.52%) of cubitus valgus, which was reported to be common after nonunion were found but no corrective surgery was required because the fractures were eventually healed, the patients had no disability, and their parents did not want further surgery. The fishtail deformity was not seen in our study. However, this study did not add any confirmatory information about the fishtail deformity because 2 year of follow-up and the incomplete ossification of distal elbow in the mean 6.5 years old patients were not enough to detect fishtail deformity. Some recent studies have reported that lateral overgrowth and cubitus varus are the most common residual deformities after lateral condylar fracture and our results concur.15,16 Varus deformity has been reported to be the most common complication and to occur regardless of fracture displacement. Some authors said that varus deformity is mainly caused by overgrowth of the lateral humeral condyle and others reported that the fracture gap might contribute to the cubitus varus deformity.12 Even though it is not entirely understood, it is believed to be secondary to a combination of lateral condylar physeal stimulation or inadequate reduction. In our series, radiographic carrying angle showed 5.0 (±4.6) degrees of decrease versus contralateral sides, and clinically 8 patients showed cubitus varus. Although no differences were observed between treatment methods or fracture types and a decrease in carrying angle or the development of clinical cubitus varus, the prominence of the lateral side of the elbow was more obvious in the 33 (22.3%) patients with lateral overgrowth and a decreased carrying angle. The additional corrective surgeries were not needed to treat cubitus varus or a reduced carrying angle in this study, more attention might be needed. In addition, these cubitus varus deformity can be the reason for corrective surgery and refractures of the upper extremity might occur in children with the history of lateral condylar fracture and cubitus varus deformity. In this study, clinical overgrowth of the lateral condyle was observed more commonly for Jakob type II and III fractures than for type I fracture. Lateral approach to avoid violating the posterior blood supply was used. Extensive soft tissue stripping and damage to cartilage or growth plate was avoided. Incomplete anatomic reduction rather than extensive soft tissue stripping was accepted. Probably all these efforts could contribute to the good results in our study. All the lateral condylar fractures were treated by single surgeon using consistent treatment protocols. Radiographic analysis of carrying angles, lateral overgrowth, and osteophyte development and clinical evaluations of cubitus varus and lateral elbow prominence were conducted. These lateral condylar fractures are easily missed and when not managed appropriately can displace. Missed fracture is a common cause of nonunion and deformity; thus, a high index of suspicion and adequate clinical and radiographic evaluation are required. Displaced fractures are associated with a high rate of nonunion. Nondisplaced fractures or those displaced ≤2mm are managed with cast immobilization and frequent radiographic follow-up. Fractures displaced >2mm are managed with surgical fixation. Successful outcomes have been reported with closed reduction, open reduction, and arthroscopically assisted techniques. Complications associated with pediatric lateral condylar fracture include cubitus varus, cubitus valgus, fishtail deformity, and tardy ulnar nerve palsy. In our series, 85 cases were displaced fracture of >2mm and all these cases were treated with close reduction and percutaneous K wire fixation. All the fractures were fixed with 2 K-wires. Non union was not encountered in this study. Fractures can be classified by various methods. Among all, Milch and Badelon classifications are easy to use and simple. According to the Milch classification, the fracture was of type 1 in five cases, and type 2 in 80 cases. According to the degree of displacement, 15 of fractures were Badelon type 3 and 70 were Badelon type 4. Diagnosis for lateral condyle fractures of the humerus is made by means of anteroposterior, lateral and oblique radiographs of the elbow as well as attentive clinical examination. Although arthrogram is helpful in more precise diagnosis, it may not be necessary in cases other than very young children as the lateral condyle of the humerus is ossified after two years of age. Sometimes intra-operative findings and radiographic images may be inconsistent. Radiographs and clinical evaluations were adequate to make diagnosis in our cases; and no unexpected finding was observed during the operation. An undisplaced fracture may be treated in a long-arm cast for 3 weeks. If this treatment is used, however, close observation every 5•7 days is necessary. Good radiographs out of plaster should be made at each visit for 6•8 weeks to determine the status of the fracture. This may require considerable time and effort. Launay et al. showed displacement in 5 of the 17 fractures treated by cast immobilization; four of them required surgery at a later date.6 Some authors suggest that screw fixation also promotes the union of fracture without significant complications.17 Close reduction with percutaneous pin fixation is recommended for fractures with less than 2mm of displacement and others that can be anatomically reduced with residual gap or step of less than 2mm. This may be performed in the operating room under image intensification only in fresh cases.15,18 The problems and the resulting complications may not be as bad when the patient presents within 12 weeks of the injury, as careful dissection and modifications in the surgical technique can provide a satisfactory reduction without compromising the blood supply.19 Overgrowth of the lateral condyle has been noted by some authors.16 Generally, there has been uniform agreement regarding the need for open reduction and internal fixation of displaced fractures of the lateral condylar physis.8•11 Because it is difficult to maintain the reduction of a displaced lateral condylar fracture and because of the high prevalence of poor functional and cosmetic results associated with closed reduction and casting, open reduction and internal fixation has become the most widely advocated method for the treatment of unstable fractures with Jakob stage-2 or 3 displacement.5 However, even patients who are managed with open reduction and internal fixation may have development of malunion because of a lack of intraoperative confirmation of the reduction status or osteonecrosis caused by excessive soft-tissue dissection. The elbow joint coordinates movements of the upper extremity, facilitating the execution of activities of daily living in areas such as hygiene, dressing, and cooking. When the distal humerus is injured, elbow joint function can be impaired.20 Operative management is required in type I fractures that demonstrate delayed displacement or instability. Fragment stabilization is most frequently performed using 2 percutaneously placed smooth Kirschner wires (K-wires).21,22 All type II and III fracture patterns require open reduction and fragment stabilization.23 Only a few reports have focused on percutaneous pin fixation of these fragments. Mintzer et al. reported good results after percutaneous pin fixation of twelve lateral condylar fractures with displacement in excess of 2mm.7 They believed that the method is appropriate for selected fractures with 2•4mm of displacement and an arthrographically demonstrated congruent joint space. Foster et al. reported that percutaneous pin fixation of nondisplaced and minimally displaced fractures is an acceptable alternative in any situation in which close clinical and radiographic follow-up cannot be ensured.8 It was often our personal experience that many fractures that were treated with open reduction and internal fixation could be reduced by closed means. Because it appeared that open reduction and internal fixation was not always necessary for these displaced fractures. However, even patients who are managed with open reduction and internal fixation may have development of malunion because of a lack of intraoperative confirmation of the reduction status or osteonecrosis caused by excessive soft-tissue dissection. Only a few reports have focused on percutaneous pin fixation of these fragments. We conducted the present study. The present study showed a high success rate (73%) in association with closed reduction and pin fixation for the treatment of unstable displaced fractures. While others have reported that closed reduction and internal fixation is not recommended for the treatment of Jakob stage-3 displaced and rotated lateral condylar fractures. We acknowledge that the number of cases is small and that additional prospective studies are needed to further evaluate this approach for the treatment of fractures with an unstable and rotated fragment. It is our impression that the reasons for our high success rate with closed reduction and internal fixation were (1) the accurate interpretation of the direction of fracture displacement (mainly posterolaterally, not purely laterally) and the amount of displacement of the fracture (2) routine intraoperative confirmation of the reduction on both anteroposterior and internal oblique radiographs, and (3) maintenance of the reduction with two parallel percutaneous Kirschner wires. However, this study is inherently weakened by its short follow-up. Furthermore, as growth and remodeling potentials of the distal humerus are relatively small, a mean follow-up of 24 months may have been insufficient for a comprehensive evaluation of outcome. The measurement of radiographic carrying angle and possible measurement bias was another weakness of our study. The small amount of rotation, especially with the lack of full extension could have a dramatic effect on the measurement of radiographic carrying angle.
ConclusionsWe conclude that the two lateral K-wires fixation in divergent fashion provided good fracture stability, good union rate with excellent functional and cosmetic outcome with minimum complication rate and virtually no nonunion in management of displaced lateral condylar fracture of humerus in children.
Conflict of interestNone.
None.