Post-traumatic cortical defect appears 3 months after greenstick or torus fractures in children. This entity is asymptomatic and usually located just proximal to the fracture site. The most frequently affected bone is the distal radius. The pathogenesis of this lesion remains unclear but it seems to be caused by an intramedullary fat and blood accumulation beneath a intact periostium. Its diagnosis is based on CT and MR images and no treatment is needed, because its resolution is the rule. There are only 25 cases reported in English literature, we present another one after an epiphisiolysis in the distal radius.
El defecto cortical postraumático aparece 3 meses después de una fractura en tallo verde o un rodete en niños. Esta entidad es asintomática y se suele localizar proximal a las fracturas. El hueso más afectado suele ser el radio distal. Su patogénesis es controvertida, aunque parece que se debe a la acumulación de una mezcla de sangre y grasa intramedular debajo del periostio íntegro. Su diagnóstico se basa en estudios de imagen de TC y RM, y no necesitan ningún tratamiento; su resolución espontánea es lo habitual. Hay solamente 25 casos publicados en la literatura inglesa y nosotros en este trabajo presentamos uno más tras una epifisiólisis tipo ii de radio distal.
Posttraumatic cortical defect is a rare lesion which occurs in children after a slightly displaced or non-displaced fracture and which is usually located in the distal radius. It can sometimes be confused with a pathological lesion, but its evolution is benign and it disappears spontaneously. The Anglo-Saxon literature contains 25 cases. In our work we describe 1 case and carry out a literature review on this subject.
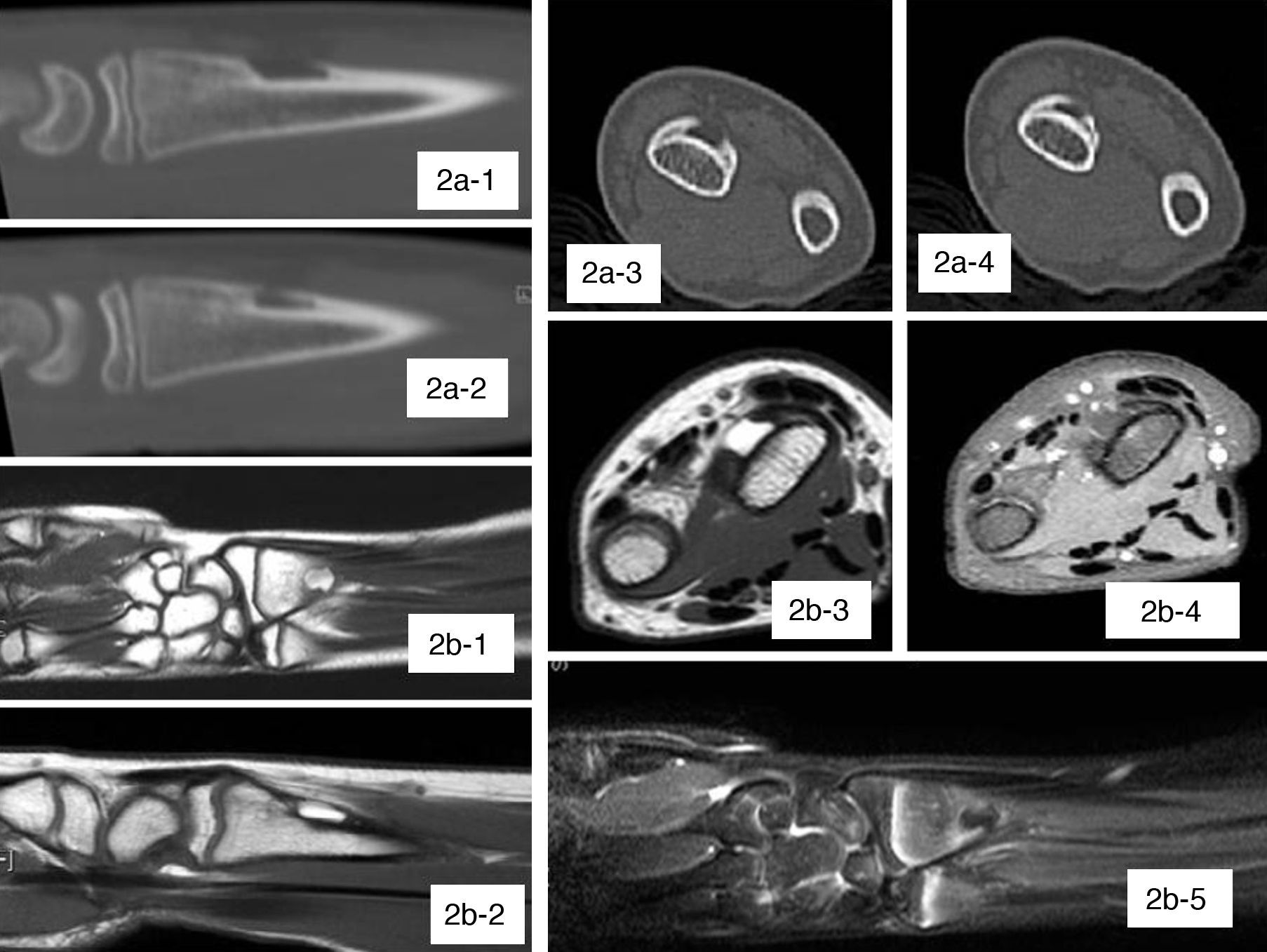
Case reportThe patient was an 11-year old girl, with no relevant history, who attended the Emergency Traumatology Service at our hospital following upper limb trauma due to a fall. Physical examination found pain, swelling and loss of function at the level of the right shoulder and wrist. The radiological study revealed a type II epiphysiolysis in the right proximal humerus and a type II epiphysiolysis in the right distal radius (Fig. 1A). The first was treated with a sling and the second was reduced by traction and immobilised with a forearm cast. The sling was removed at 3 weeks and the cast at 4 weeks. The patient did not present pain in any of the 2 fracture foci. Shoulder and wrist mobility were normal at 3 months of the fracture and the radiographs showed complete consolidation and remodelling of the fractures. However, an osteolytic lesion appeared at the level of the diaphysio-metaphyseal distal radius (Fig. 1B), proximal to the location of the fracture. It had well-defined although not sclerotic edges, was approximately 1.5cm in diameter and appeared to affect the dorsal cortical. The differential diagnosis considered an infection or a tumour, such as an aneurysmal bone cyst, osteoblastoma or fibrous cortical defect. She underwent computed tomography (CT) and magnetic resonance imaging (MRI) studies (Fig. 2). The former showed a cortical lesion measuring 10×3.6×6mm within a cortical thickening, probably secondary to a calcified subperiosteal haematoma, which presented an area with loss of the cortical without soft tissue mass and a very low attenuation coefficient, similar to fat. The MRI showed a hyperintense lesion on T1 and T2-weighted sequences, with complete loss of signal in fat suppression sequences, thus confirming its fatty nature. In addition, there was a fine cortical line between the lesion and soft tissues, and no significant soft tissue mass or other signs of radiological aggressiveness were observed. The final diagnosis was post-traumatic cortical defect, so we decided to adopt a waiting attitude. At 10 months of the fracture we performed a new radiological control of the wrist which showed the disappearance of the lesion along with a small, dorsal, cortical thickening of the radius.
Plain radiographs. (A-1 and A-2) Anteroposterior and lateral radiographs of the wrist at the time of fracture. We can see a type II epiphysiolysis in the distal radius. (B-1 and B-2) Anteroposterior and lateral radiographs at 3 months of the fracture. We can see a geographical, osteolytic image in the metaphyso-diaphyseal area of the distal radius, at the level of the dorsal cortical.
(A) CT images. (A-1 and A-2) Sagittal sections. (A-3 and A-4) Axial sections. We can see an intracortical defect of the distal radius at the dorsal level, with no extension to soft tissues. (B) MRI images. (B-1) T1 coronal section. (B-2) T1 sagittal section. (B-3) T1 axial section. (B-4) DP axial section. (B-5) Fat-suppression coronal section. In these images we can see the subperiosteal lesion with fat content.
Post-traumatic cortical defect is a very uncommon lesion which occurs in children from 2.5 to 15 years of age, 2–4 months after a greenstick or buckle/torus fracture. The first report in the literature took place in 1969 by Levine et al.,1 regarding the fibula of a 13-year old boy. At present, the literature contains 25 reported cases. The largest series published to date is that of Pfister-Goedeke et al.,2 which describes 9 cases. Of the 25 reported cases, 20 were located in the distal radius, 3 in the distal tibia, 1 in the femur and 1 in the fibula. Therefore, the distal radius is the most frequently affected bone. It usually occurs at the level of the concave cortical of the fracture (opposite to the apex of the fracture), proximal to it and usually measuring about 1cm in diameter. There is some controversy regarding the pathophysiology of these lesions, especially with regard to their content. Some authors have demonstrated the existence of clotted blood in their interior through biopsies.1 Phillips and Keats3 attributed the lesion to an intraosseous haemorrhage which was subsequently reabsorbed and formed the cyst. On the other hand, others like Malghem and Maldague4 reported the content of these cysts to be intramedullary fat included in the subperiosteal haematoma at the time of fracture, but which was only seen on the radiograph when the surrounding haematoma became calcified. In a subsequent work, Malghem et al.5 used CT studies to demonstrate the presence of fat within the cyst. This could come from the intramedullary red marrow being converted into small fat droplets. Dürr et al.6 and Davids et al.7 supported this fact by using MRI studies. Ball et al.8 reported that the fat was mixed with the haematoma, so when the latter was reabsorbed it became possible to see the lesion radiologically. Roach et al9 likened the content of the cyst to lipohaemarthrosis containing blood and fat droplets. The lesion occurs in slightly displaced or non-displaced fractures, at the level of the most concave cortical, in which the periosteum remains intact and favours the accumulation of the haematoma with intramedullary fat. Therefore, the fracture must be severe enough to break the cortical in its entirety and allow the exit of intramedullary content, but not excessively, so the periosteum remains complete. As the fracture heals, a new cortical is formed from the periosteum, which is separated from the original cortical. A cavity is formed between them which corresponds to the lesion described. It is totally asymptomatic and does not seem to interfere with healing of the fracture or increase the risk of pathological fracture.
The diagnosis of the lesion is based on imaging studies. Being asymptomatic, it is usually an incidental finding which appears in control radiographs of the fracture or in some cases in new radiographs obtained for other reasons. Plain radiographs show a non-expansive, intracortical, osteolytic lesion, approximately 1cm in diameter, with well-defined edges, located at a proximal level with respect to the fracture. It may be single or multiple. CT and MRI studies show an intracortical, cavitated, circumferential lesion, with fatty content10 and without soft tissue extension. A biopsy is not necessary to confirm the diagnosis. Healing is spontaneous and patients just need to be observed. Follow-up radiographs show a slight proximal displacement, away from the physis,9 due to bone growth, as well as resolution within 1 or 2 years. Differential diagnosis should include simple bone cysts, fibrous cortical defect, eosinophilic granuloma, aneurysmal bone cyst and infectious processes, such as subacute osteomyelitis.
ConclusionPost-traumatic cortical defect is a rare lesion which occurs in children who suffer fractures that break the cortical, but which retain the periosteum. They appear due to an accumulation of haematoma and intramedullary fat within the periosteum. The most common location is the distal radius. The lesion is asymptomatic and the diagnosis is based on imaging studies, with biopsies being totally unnecessary. Its resolution is spontaneous, without affecting the healing process of the fracture or increasing the risk of pathological fracture.
Level of evidenceLevel of evidence IV.
Ethical responsibilitiesProtection of people and animalsThe authors declare that this investigation did not require experiments on humans or animals.
Confidentiality of dataThe authors declare that they have followed the protocols of their workplace on the publication of patient data and that all patients included in the study received sufficient information and gave their written informed consent to participate in the study.
Right to privacy and informed consentThe authors declare having obtained written informed consent from patients and/or subjects referred to in the work. This document is held by the corresponding author.
Conflict of interestsThe authors have no conflict of interests to declare.
Please cite this article as: Valverde Villar AM, Salcedo Montejo M. Defecto cortical postraumático. A propósito de un caso. Rev Esp Cir Ortop Traumatol. 2012;56:482–5