A radiographic study was carried out to investigate the relationship between proximal sacral sagittal anatomy (either kyphosis or lordosis) and either isthmic or degenerative spondylolisthesis. In addition, we studied whether there is a relationship between proximal sacral kyphosis and the grade of such listhesis in the case of L5 isthmic spondylolisthesis.
Lateral standing X-rays were used from 173 patients, 90 of whom had degenerative spondylolisthesis L4–L5, and 83 an isthmic spondylolisthesis of L5 (67 low-grade and 16 high-grade) and compared with a control group of 100 patients adjusted by age and gender, without any type of spondylolisthesis. Listhesis was graded using Meyerding's classification and the proximal sacral kyphosis angle (PKA) was measured between S1 and S2 posterior walls, according to Harrison's method.
In our series, there was a proximal sacral kyphosis in both types of spondylolisthesis, greater in the lytic type. By contrast, the control group had a proximal sacral lordosis. The differences were statistically significant.
Therefore, we concluded that there was a proximal sacral kyphosis in patients with both degenerative and isthmic lytic spondylolisthesis, but with our results, we were not able to ascertain whether it is a cause or a consequence of this listhesis.
Se realiza un estudio radiográfico para investigar la relación entre el alineamiento sagital de la anatomía sacra proximal (ASP) y la espondilolistesis, ya sea lítica ístmica o degenerativa. Por otra parte, se estudia si en el caso de la espondilolistesis ístmica lítica de L5 existe relación entre el grado de la listesis y dicha ASP.
Se revisaron las imágenes laterales del sacro (radiografías de columna lumbar en bipedestación generalmente) de 173 pacientes, de los cuales 90 tenían una espondilolistesis degenerativa L4 y 83 una espondilolistesis ístmica lítica de L5 (67 de bajo grado y 16 de alto grado) y se compararon con un grupo control de 100 pacientes ajustado por edad y género, sin ningún tipo de espondilolistesis. Se definió el grado listesis según la clasificación de Meyerding y el ángulo de ASP, medido según el método de Harrison, mediante el ángulo entre las líneas tangentes a los muros posteriores de S1 y S2.
En nuestra muestra existe una cifosis sacra proximal en ambos tipos de espondilolistesis, siendo mayor en la ístmica lítica, especialmente en las de alto grado. Por el contrario, el grupo control presentaba una lordosis sacra proximal. Las diferencias en la ASP fueron estadísticamente significativas entre controles y espondilolistesis, tanto ístmica lítica L5 como degenerativa L4, así como entre ambos tipos de espondilolistesis y, entre las ístmicas líticas, las de alto y bajo grado.
Por lo tanto, se puede afirmar que en los pacientes de nuestro estudio la cifosis sacra proximal está relacionada con espondilolistesis degenerativa y la ístmica lítica, sin poder discernir claramente si es una causa o una consecuencia de la misma.
In recent years several studies have demonstrated that spinal and pelvic parameters are related to spondylolisthesis and its progression. Spondylolistheses with a high grade of dysplasia are more likely to progress and a high grade of dysplasia includes, among other parameters, lumbosacral kyphosis.1 Other authors have demonstrated the existence of the relationship between L5-S1 spondylolisthesis development and its grade, with pelvic incidence, sacral gradient, sacral inclination, lumbar lordosis and thoracic kyphosis.2,3 These studies suggest that these parameters could be factors related to the pathogeny of spondylolisthesis.
Focussing on the sacrum, it has been noted that the anatomy of the sacrum varies considerably from one individual to another overall sacral curvature is minimal in newborns and progressively increases during adolescence.4 Later spine curvatures appear and, together with them, patients with lytic isthmic spondylolisthesis develop a curved sacrum.5 The lumbar sacral angle increases from birth up to 5 years of age, and remains the same in adulthood in healthy patients.
Different sacral parameters are significantly related to spondylolisthesis, such as the sacral plate angle which corresponds to the angle between posterior wall of S1 and the upper plate of S1.6,7 There is also a direct relationship between the lateral curvature of the sacral body8 or its S1–S4 kyphosis measured by the Cobb9 method and L5-S1 isthmic spondylolisthesis and its grade. Similarly, S1 kyphosis (measured by S1 index) has been related with lumbosacral kyphosis, slippage grade and ease with which L5 over S1 was reduced in L5 lytic isthmic spondylolisthesis.10–12 No standard has been defined within the parameters of sacral anatomy with regards to shape, as has been commented on previously, and the variability of measurements referred to in the literature considerably hinders the comparison of outcomes between the different studies.
However, it has not been proven that these anatomical changes are the cause of listhesis or are merely secondary changes, although there have been suggestions, in the sense of a secondary sacral shaping in sacral plate angle studies in patients with serialised images throughout their lives.13 Also, the majority of studies are focused on L5-S1 lytic isthmic spondylolisthesis with less attention paid to degenerative spondylolisthesis.12–17
We therefore feel able to theorise that the anatomy of the sacrum itself, regardless of spinal and pelvic parameters, is different in patients affected by spondylolisthesis, probably as a reflection of a trunk imbalance which leads to formation of the sacrum on its fixed attachment to the pelvis: the sacroiliac joint.
Hypothesis: patients with spondylolisthesis, understood to be the result of an anterior imbalance of the trunk, have a sacrum with greater kyphosis in their region proximal to the sacroiliac joint, i.e. segment S1–S2.
It is to be expected that cases with L5 lytic isthmic spondylolisthesis, because they present with greater trunk imbalance, have this kyphotic deformity to a higher degree than patients with L4 degenerative spondylolisthesis, although both patient groups will suffer from it, compared with the population with no spondylolisthesis.
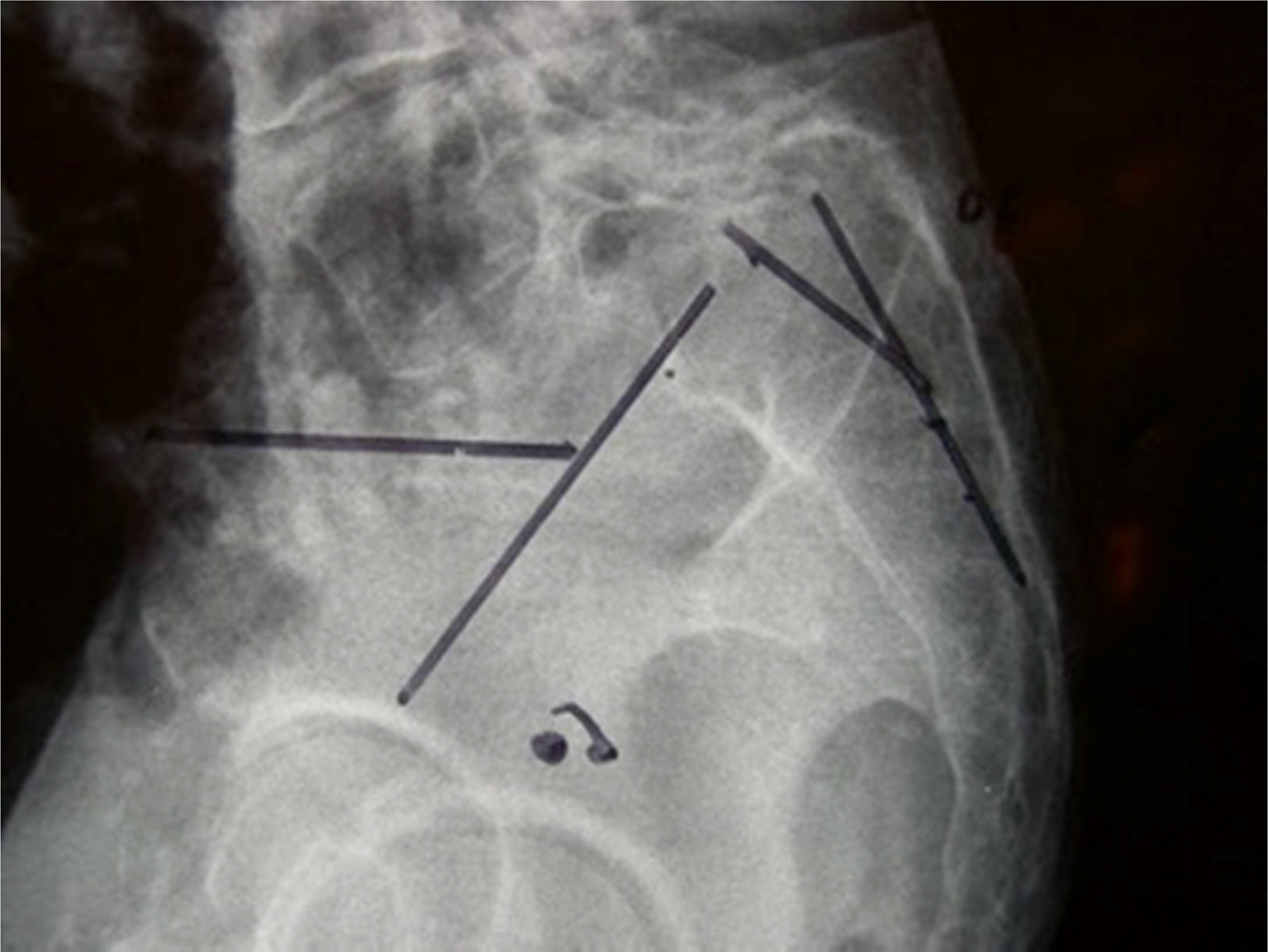
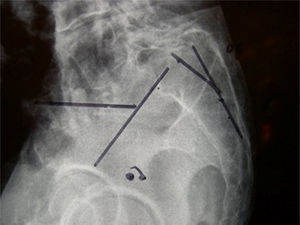
Material and methodsA radiographic study was carried out to investigate the relationship between a tendency to proximal sacral kyphosis and spondylolisthesis, be it L5 lytic isthmic or degenerative (on S1) (Fig. 1) or L4 degenerative (on L5).
In addition, we studied whether there was a relationship between proximal sacral kyphosis and the grade of such listhesis in the case of L5 isthmic spondylolisthesis.
Our sample comprised 273 people, with a control group (group 0), composed of 100 personas with no spondylolisthesis or known vertebral disease, with a similar age and gender distribution to groups 1 and 2. Group 1, of 90 patients with L4–L5 degenerative spondylolisthesis and group 2, of 83 patients with L5-S1 lytic isthmic spondylolisthesis. Group 1 comprised 22 males and 68 females, aged between 43 and 92 years (mean: 68) whilst group 2 comprised 35 males and 48 females aged between 12 and 90 years (mean: 46). In group 2 the listhesis was low grade in 67 patients and high grade in 16.
Inclusion criteriaPatients with anterior L5-S1 spondylolisthesis from isthmic lysis or L4–L5 degenerative spondylolisthesis, assessed in our centre between 1st January 2006 and 31st December 2014.
Images with a clear view of the proximal sacrum: lateral standing radiographies in patients and radiographies or sagittal CAT slices in the middle sacrum line, in the control group.
Exclusion criteriaA background of trauma, tumour, metabolic or infectious disease which could involve deformation of the sacrum.
The radiological variables were studied in digitalised images in the SECTRA visor (IANUS programme). The said variables were: (a) grade of listhesis, in accordance with Meyerding classification, considering types I and II as low grade and type III or above as high grade (50% or more slippage); and (b) proximal sacral kyphosis angle (PKA): angle formed by the straight lines defined by the posterior walls of S1 and S2 (Harrison method18).
The SPSS 21.0 statistical programme and the R statistical package was used, in collaboration with the hospital's epidemiology service. Parametric tests (ANOVA) were selected once normal distribution of the variables in the different groups had been confirmed, with an accepted significance level of p<0.05.
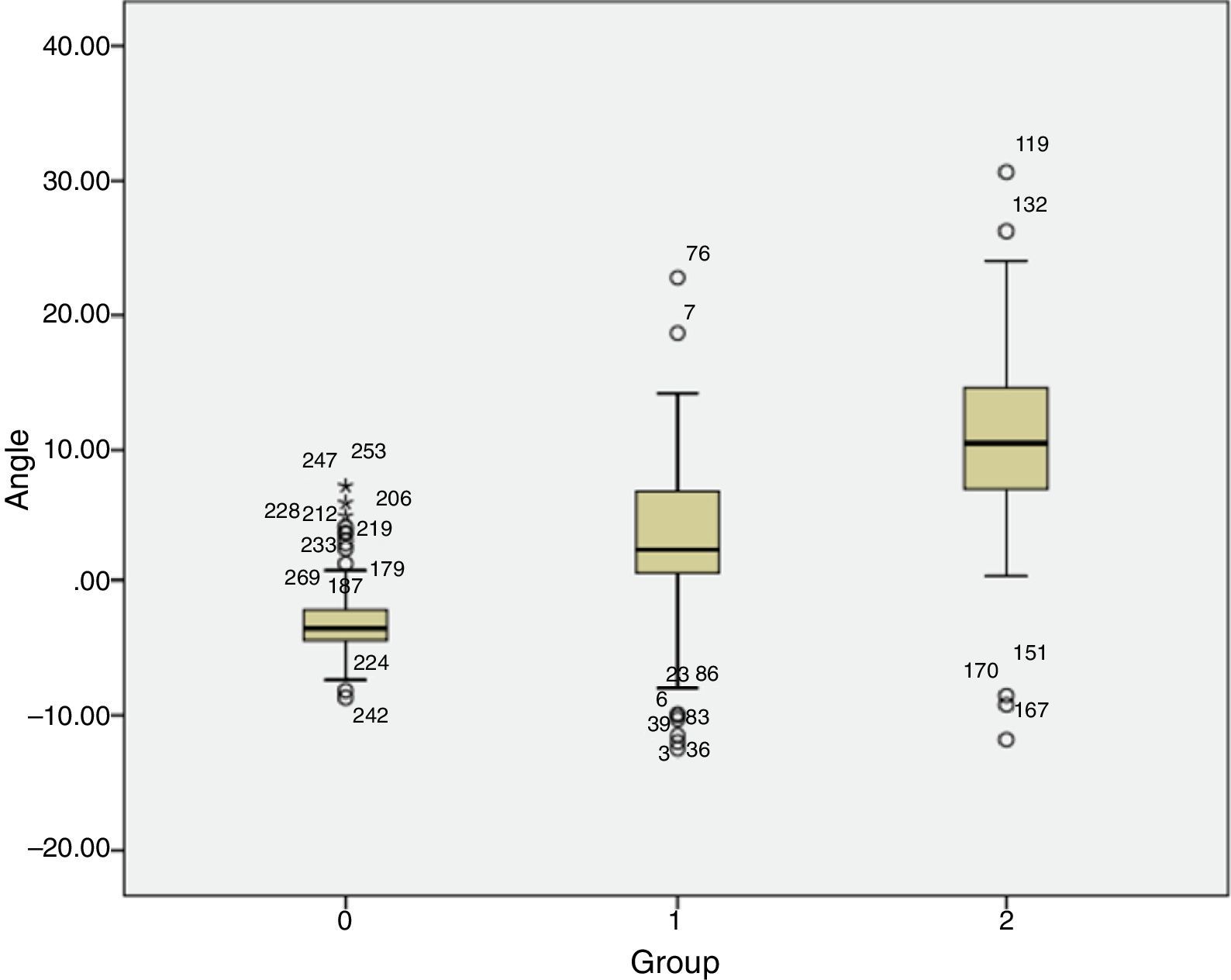
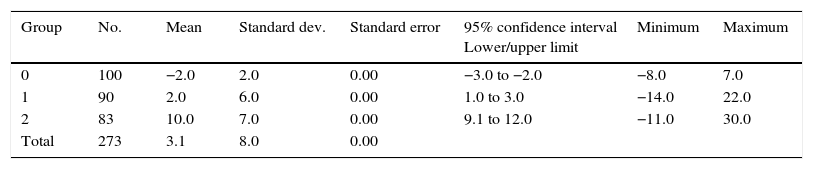
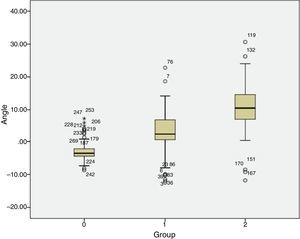
ResultsThe PSA found was lordotic in the control group (−2°±2°; minimum −8° and maximum 7°), whilst in group 1 (L4 degenerative spondylolisthesis) it was kyphotic (+2°±6°; minimum −14° and maximum +22°), so too in group 2 (L5 lytic isthmic spondylolisthesis), where it was also kyphotic (+10°±7°; minimum −11° and maximum +30°). Differences were found between the lytic isthmic spondylolisthesis group (group 2) between patients with low grade (+10°; minimum −11° and maximum +30°) and high grade (+15°; minimum +5° and maximum +26°) (Fig. 2 and Table 1).
S1S2 angulation values.
| Group | No. | Mean | Standard dev. | Standard error | 95% confidence interval Lower/upper limit | Minimum | Maximum |
|---|---|---|---|---|---|---|---|
| 0 | 100 | −2.0 | 2.0 | 0.00 | −3.0 to −2.0 | −8.0 | 7.0 |
| 1 | 90 | 2.0 | 6.0 | 0.00 | 1.0 to 3.0 | −14.0 | 22.0 |
| 2 | 83 | 10.0 | 7.0 | 0.00 | 9.1 to 12.0 | −11.0 | 30.0 |
| Total | 273 | 3.1 | 8.0 | 0.00 |
Positive values indicate kyphosis, negative lordosis. Harrison method.
Groups: group 0 are control groups; group 1: patients with L4 degenerative spondylolisthesis; and group 2 patients with L5 isthmic lytic spondylolisthesis (ANOVA).
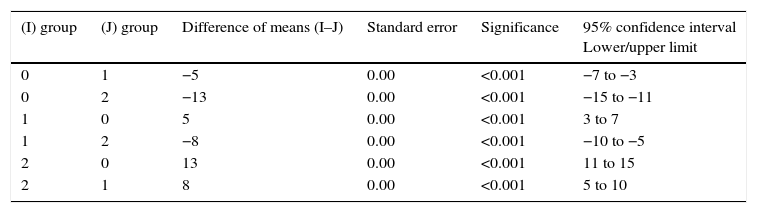
Differences between groups 0 and 1, 1 and 2, and between 0 and 2 are statistically significant: p<0.001 (Table 2). The differences between the low grade and high grade subgroup are also the same, with a significance level of p<0.01.
Comparative study of the 3 groups 2 to 2.
| (I) group | (J) group | Difference of means (I–J) | Standard error | Significance | 95% confidence interval Lower/upper limit |
|---|---|---|---|---|---|
| 0 | 1 | −5 | 0.00 | <0.001 | −7 to −3 |
| 0 | 2 | −13 | 0.00 | <0.001 | −15 to −11 |
| 1 | 0 | 5 | 0.00 | <0.001 | 3 to 7 |
| 1 | 2 | −8 | 0.00 | <0.001 | −10 to −5 |
| 2 | 0 | 13 | 0.00 | <0.001 | 11 to 15 |
| 2 | 1 | 8 | 0.00 | <0.001 | 5 to 10 |
Same distribution of groups as in Table 1. Multiple comparisons. Dependent variable: angle. Test: Scheffe.
Pelvic incidence determines the position of the upper sacral plate. The body balances the pelvic incidence through lumbar lordosis. The tensions which the lumbosacral joint withstands depends on its spatial orientation. The more vertical it is the greater they are. A higher pelvic incidence implies lower pelvic tilt and higher sacral gradient, leading to higher verticalisation of the lumbosacral hinge. Pelvic incidence is therefore significantly related to the progression of listhesis. Pelvic incidence is a constant parameter in the adult,14 although it increases with age during development, suggesting that its increase may be due to adaptive changes in the standing position which could increase in patients with isthmic spondylolisthesis.2,3 However, the sacral plate angle (between the posterior wall and the S1 cranial plate) is similar in young and adult patients,7,17 which could lead us to thinking that a reduced angle could be an etiological factor of spondylolisthesis. This was recently disproved13 in a study where no difference in said angle between patients with isthmic spondylolisthesis and a control group was found. The appearance of sacral kyphosis could therefore be the result of bone shaping of the sacrum rather than one of the original causes of anterior imbalance of the trunk.
It has also been suggested5 that the sacrum in patients with spondylolisthesis, even low grade, is more curved than in that of the general population, and even specifically at S1–S2 level, although the author measured using the Cobb method, of lower reproducibility than the Harrison method which we used. In fact, the same author acknowledges the limitations of the Cobb method used in this region.5 After evaluating the different methods used to measure sagittal alignment, we decided to use the Harrison method17 because we considered it the most reproducible and least susceptible to bone shaping of them all, and our opinion is shared by other authors.19
Why level S1–S2? Since spine curvatures are acquired by the human when he or she begins to stand up, and that the sacrum forms part of the spine, it is understood that the sacroiliac joint is the fulcrum from which the sacrum curves. It is the area of load transmission between the lumbar spine and the pelvis, and a point which may be considered as fixed. This joint is at S2–S3 level, i.e. immediately below the area we chose to measure in this study.
The study of kyphosis of this S1–S2 segment with this methodology has not been published as of yet, and all comparisons with other works may always have an intrinsic component in measurement methodology.
The idea that the sacral anatomy may predispose one to listhesis in the case of L4–L5 segment degeneration we find suggestive. However, this would probably be the consequence of the shaping of a sacrum in growth in the case of patients with L5 lytic isthmic lesions. In other words, it would be a consequence in the case of the development of spondylolisthesis and a cause in the case of acquired spondylolisthesis (in accordance with the criteria of Marchetti and Bartolozzi).
It is an academic digression since S1–S2 kyphosis existing to a lower extent in L4 degenerative spondylolistheses could also be a consequence of a shaping of the sacrum during a person's lifetime, with the lower amount being explained by less bone plasticity than during growth. The distinction requires the study of the sacrum of these patients in early bone maturity (20–30 years of age) before the degenerative processes appear. Notwithstanding, there are works which also suggest a change in the spinal and pelvic parameters in patients with this disorder.20
As an initial step to trying out this thesis we will try to demonstrate that the proximal sacrum is effectively found in kyphosis, in a more marked form than in the population with no type of deformity due to anterior trunk imbalance (spondylolisthesis), regardless of whether said spondylolisthesis is associated with a lysis in the L5 pars interarticularis, or adaptive degenerative changes in the L4–L5 surfaces. It is expected that the first situation leads to an ambiance which is biomechanically more likely to lead to the appearance of deformities, due to the posterior bone structure impairment.
An increase of the proximal sacral kyphosis would be expected to be related to an increase in the probability of suffering from anterior vertebral slippage.4,12–17 Each patient has his or her particular morphology of the sacrum, which includes the proximal sacral kyphosis angle, and this does not vary with regards to the patient's spatial position. It therefore makes no difference to measure radiographies standing up (the standard in our regular practice for studies for patients with vertebral symptomology) or CAT sagittal sections (in prone positioning but performed on patients with problems unrelated to any diseases of the spine). Due to all of the above we believed this to be a variable susceptible to study with reproducibility and reliability in the control group, without the need for a disease of the spine (and therefore without standing spine radiology in several cases).
In healthy humans lumbosacral fusion is lordotic,4 which would correspond to our data by extension (lordosis S1–S2 of −2°). In people with spondylolisthesis this proximal sacral lordosis disappears, and becomes kyphosis, statistically more acute in patients with lytic spondylolisthesis compared with degenerative, and even more so in cases of high grade. This fits in with common sense: the greater the imbalance the greater the shift and this anterograde imbalance is even reflected inside the sacral bone.
According to the Hueter–Volkmann law of physeal growth anatomic changes of the sacrum and particularly sacral kyphosis in patients with spondylolisthesis, are secondary to an axial compression of the anterior sacral plate due to L5 anterior shift over S1, reducing enchondral bone growth in this area and increasing it abnormally in the posterior part of the S1 body, because it is less subject to pressure. Moreover, if the pars interarticularis does not break, it pulls on the elements posterior to S1, boosting this growth posterior to the proximal vertebrae of the sacrum, leading to kyphotic curvature of the proximal sacrum. Other anatomical changes of the sacrum, such as the dome shaped proximal sacrum plate or the cradling of L5 are thought to be adaptive changes secondary to listhesis.3–9
It has been seen in a young population (6–20 years of age) with lytic L5-S1 spondylolisthesis that the sacral plate and sacral kyphosis are significantly changed in these patients, compared with a control group with no listhesis. They measured the overall sacral kyphosis according to the Ferguson angle, which forms the line that goes from the midway of the upper plate of S1 to the midpoint of its lower plate, with the line which passes between the mid points of the lower plates of S2 and S4. They observed a mean sacral kyphosis of 26° in healthy subjects and one of 43° in patients with spondylolisthesis. However, they did not find any difference with regards to the kyphosis between low and high grade spondylolisthesis. These authors also measured the proximal sacral kyphosis, but unlike our study, they used the super S1 angle (angle between that perpendicular to the upper plate of S1 and the line which links the mid points of S1 plates) and the lower S2 angle (angle between the line which joints the midpoints of the S1 plates and that perpendicular to the lower S2 plate). They found that the upper S1 angle was considerably superior in patients with spondylolisthesis, and that the lower angle of S2 was considerably inferior in these patients. Other authors did not confirm these findings of the sacral plate in patients with spondylolisthesis,13 and the sacral deformity was therefore due to a shaping of the same: appearance of S1–S2 kyphosis as we saw in our series.
Pelvic incidence was not affected by the surgical reduction and fixation of the spondylolisthesis, whilst the lumbosacral angle and the lumbar lordosis was. Pelvic tilt and sacral gradient are modified by surgery, but to a lesser degree. With regards to the therapeutic relevance of sacral kyphosis Schroeder et al. reported several good results regarding the reduction of the lumbosacral slippage angle and improvement in the SRS questionnaire in patients with high grade isthmic spondylolisthesis who had undergone surgery involving L4-S1 arthrodesis, prior to reduction of the L5 listhesis, which was redirected towards cranial and posterior.16 Sagittal balance was improved as a result of reducing the lumbosacral kyphosis, despite the fact that the degree of listhesis was not changed to any great significance. Although this technique did not directly change the sacral kyphosis, it did underline the importance of the sacral kyphosis in the spondylolisthesis and suggests that a reduction of the same would improve the prognosis of these patients.
Regarding L4–L5 degenerative spondylolisthesis we chose this level, since it was the most common in our environment (72% of all degenerative spondylolistheses diagnosed during the 2006–2014 period). The fact that proximal sacral kyphosis is statistically higher in these degenerative spondylolistheses compared with the population without listhesis suggests that sacral deformity could also be a pathogenic factor in this nosologic entity. In the case of these L4–L5 spondylolistheses, which did not present with listhesis at level L5-S1, it is more difficult to think that the sacral deformity is due to vertebral slippage, and that it is more likely to be an anatomical characteristic of the sacrum, a possible etiological factor of future spondylolisthesis.
However, the fact that the ASP is more kyphotic in lytic spondylolisthesis than in degenerative spondylolisthesis, and that within the lytic that it is greater in high grade than in low grade, suggest to us that proximal sacral kyphosis could also be a consequence of listhesis, with the sacral deformity developing as the vertebral slippage progresses, as previously explained. This hypothesis is backed up by the fact that patients with isthmic spondylolisthesis usually start presenting with the disease at an early age, when the skeleton is still immature and is therefore more likely to suffer from deformities with growth.
The bias of our study may be the lack of similarity regarding the age of the patients with degenerative spondylolisthesis and those with lytic spondylolisthesis. This is difficult to avoid, since the pathological processes appear at very different ages. Since the patient group with lystic spondylolisthesis was not divided into young people and adults we cannot know whether anatomical sacral changes are present at a young age or in adulthood. Neither can we obtain this data in the group with degenerative spondylolisthesis since early age radiographies of the patients who later developed listhesis were not available to us.
ConclusionProximal sacral kyphosis exists in patients with spondylolisthesis, both lytic isthmic L5 and degenerative L4, and is greater in patients with isthmic lysis of L5 and, among these, in those of high grade listhesis.
Level of evidenceLevel of evidence III.
Ethical disclosuresProtection of human and animal subjectsThe authors declare that no experiments were performed on humans or animals for this investigation.
Confidentiality of dataThe authors declare that no patient data appears in this article.
Right to privacy and informed consentThe authors declare that no patient data appears in this article.
Conflict of interestsThe authors have no conflict of interests to declare.
Please cite this article as: Gallego-Goyanes A, Barahona-Lorenzo D, Díez-Ulloa MA. Deformidad sacra proximal: elemento común a la espondilolistesis ístmica lítica de L5 y a la degenerativa del segmento L4-L5, 2 entidades de etiopatogenia muy diferente, aparentemente. Rev Esp Cir Ortop Traumatol. 2017;61:343–348.