Evaluation of the surgical management, outcome and complications in patients with pertrochanteric fractures treated with PFNA nail.
Materials and methodsA retrospective study was conducted on 200 patients treated consecutively between April 2010 and February 2012. Radiological assessments were performed before and after the surgery, and during the follow-up (fracture reduction, blade position, consolidation or collapse signs). A clinical evaluation was performed as regards walking capabilities. The results were compared with those of a previous study on 700 patients treated with gamma 3 and TFN nails.
ResultsThe blade position was center–center in 64% of patients, and decreased to 53% in the mechanical complications group. Tip-apex distance was less than 25mm in 91.5%. The average hospital stay was 9.17 days, with a mean post-surgery stay of 5.95 days.
Complications (7.5%): 2 cut out (1%), one cut through (0.5%), 4 cases of helical blade sliding (2%), one failure in distal locking procedure (0.5%), 2 cases with painful fasciae latae (1%), one union delay (0.5%), 2 cases of non-union with hardware failure (1%), one case of intense bleeding related to distal locking of the nail (0.5%), and one case of avascular necrosis (0.5%).
ConclusionsThe PFNA helical blade system seems to reduce the incidence of cut out and cut through in osteoporotic bone. Blade position was one of the main parameters associated with mechanical complications.
Evaluación del manejo quirúrgico, evolución y complicaciones de pacientes afectados por fractura pertrocantérea de cadera tratados mediante enclavado PFNA.
Material y métodoRevisión retrospectiva de 200 pacientes intervenidos entre abril de 2010 y febrero de 2012 de forma consecutiva. Se realiza evaluación radiográfica preoperatoria, postoperatoria y durante el seguimiento (reducción de la fractura, posición de la espiral, consolidación o signos de colapso). La evaluación clínica se realizó en función de la autonomía para la marcha. Se comparan los resultados obtenidos con estudio previo, sobre muestra de 700 pacientes y enclavado gamma 3 y TFN.
ResultadosLa posición de la espiral es centro-centro en el 64% de los pacientes, que disminuye al 53% en el grupo de las complicaciones mecánicas, siendo la distancia punta-vértice menor a 25mm en el 91,5% de los casos. La estancia hospitalaria media se sitúa en 9,17 días con una estancia media postintervención de 5,95 días.
Las complicaciones (7,5%) fueron: 2 casos de cut out (1%), uno de cut through (0,5%), 4 casos de efecto telescopaje (2%), un fallo en el encerrojado distal (0,5%), 2 casos de molestias en la fascia lata (1%), un retardo en la consolidación (0,5%), 2 seudoartrosis que condicionaron la rotura del dispositivo (1%), un caso de sangrado relativo al clavo (0,5%) y un caso de necrosis avascular (0,5%).
ConclusionesEl sistema de espiral cefálica PFNA parece reducir la incidencia de cut out y cut through en el hueso osteoporótico. La posición de la espiral supone uno de los principales parámetros relacionados con las complicaciones mecánicas.
Hip fractures are the most common cause of emergency hospital admission at Traumatology Units among the elderly. About half of such cases are classified as extracapsular and have a high associated mortality.1
Intramedullary nails are one of the most commonly used devices in our country at present and considered superior relative to screw-plate systems for unstable fractures.2–4 However, they are not without complications. Various cephalic anchoring system designs (screw, blade, anti-rotation accessory screw...) seek to reduce the rates of mechanical complications, mainly ‘cut out’3 (collapse of the cervicodiaphyseal angle toward varus and exit of the screw through the femoral head4) and ‘cut through’ (perforation of the femoral head at the central level, with intrusion of the blade within the hip joint, without displacement of the fracture1).The rate of reoperations due to complications caused by these nailing systems is estimated at between 4% and 9%.3,5–9
The aim of our study is to evaluate the results of treatment of pertrochanteric femoral fractures, 31-A in the AO/OTA classification, with a PFNA (proximal femoral nail anti-rotation) nailing system.
Materials and methodsThe study included 200 patients who were consecutively admitted at our center with a diagnosis of pertrochanteric femoral fracture between April 2010 and February 2012. The inclusion criteria were: extracapsular fractures (AO/OTA 31-A), low-energy trauma (falls from standing height) and osteoporosis. The exclusion criteria were: pathological fractures, young patients (<60 years) and high-energy trauma. The series was composed of 56 males and 144 females, with a mean age of 84.74 years (range: 60–98 years). We conducted a retrospective study based on medical records and imaging data collected by the Department of Radiology upon admission and during the evolution. Evaluation of the results was carried out by an independent surgeon, different from the one performing the interventions. We compared the results with those obtained in 2 previous studies conducted at our center, the first of them with 224 patients who underwent gamma nailing10 and the second including 700 fractures intervened by gamma 3 nailing and TFN (trochanteric femoral nail).11
Typically, these patients underwent operations at 36–48h of admission, unless a medical pathology caused a delay in surgery. We conducted prophylaxis for thromboembolic disease with bemiparin. The operation was predominantly performed under subarachnoid anesthesia, occasionally associated to femoral nerve block for pain control. We used 2g of cefazolin (fosfomycin in patients allergic to beta-lactam) as antibiotic prophylaxis, and an orthopedic traction table for reduction. During the procedure, usually performed jointly by a senior surgeon and a resident, radioscopic images were obtained to assess the position of the components.
Except in cases with clinical decompensation of the overall condition, sitting took place at 24h postoperatively, in all cases following an assessment of radiological and analytical postoperative monitoring. Ambulation was allowed approximately 72–96h after surgery in most patients. The indication for early load was determined by previous or present functional condition, but independently of the type of fracture and quality of reduction.12,13
Monitoring was carried out at 1, 3, 6 and 12 months after discharge, during routine outpatient consultations at our center. We performed a comparison of previous ability for ambulation and the improvement achieved during follow-up, assigning patients to one of the following groups14: group 1 (able to walk independently or with a single, simple aid, like a crutch or tripod), group 2 (able to walk with the aid of 2 crutches, walker or frame) or group 3 (unable to walk, requiring a wheelchair for transport). Fractures were classified according to the AO/OTA scale.15
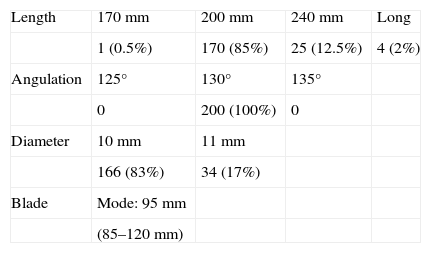
The nail under study16 is marketed in standard lengths of 170, 200 and 240mm, as well as longer versions between 300 and 420mm. The diameters available range between 9 and 14mm. The proximal bolt was a perforated helical blade allowing cementation, with cervicodiaphyseal angulation of 125°, 130° or 135°.
Radiographic evaluation in the immediate postoperative period included an assessment of the reduction (depending on the cervicodiaphyseal angle obtained and the reduction gap, which should be less than 5mm in both projections), and was given a score of “good” if both criteria were present, “acceptable” if only one of them was observed, and “poor” if neither could be recorded.14
The position of the helical blade was evaluated according to the quadrants of Cleveland and Bosworth17,18 (dividing the cephalic circumference into 9 portions, with each being assigned a number from left to right and top to bottom), as well as the Baumgaertner tip-apex distance.4,19
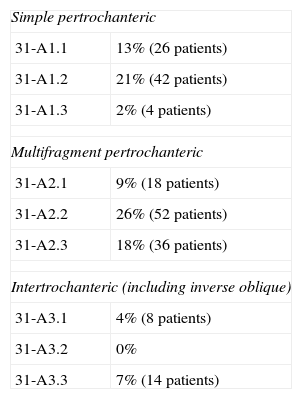
ResultsThe distribution of fracture types can be seen in Table 1, with the most prevalent being 31-A1.2 (21%) and 31-A2.2 (26%).
Distribution of the fracture pattern according to the AO/OTA classification.
| Simple pertrochanteric | |
| 31-A1.1 | 13% (26 patients) |
| 31-A1.2 | 21% (42 patients) |
| 31-A1.3 | 2% (4 patients) |
| Multifragment pertrochanteric | |
| 31-A2.1 | 9% (18 patients) |
| 31-A2.2 | 26% (52 patients) |
| 31-A2.3 | 18% (36 patients) |
| Intertrochanteric (including inverse oblique) | |
| 31-A3.1 | 4% (8 patients) |
| 31-A3.2 | 0% |
| 31-A3.3 | 7% (14 patients) |
The nails used in our study presented the distribution shown in Table 2, with the most commonly used nail having 200mm length, 130° angulation and 10mm diameter. Except for long nails (over 240mm), we performed a dynamic distal block in all cases. The mean surgery time was 42.06min. The quality of reduction was classified as good in 154 cases (77%), acceptable in 40 cases (20%) and poor in 4 cases (2%).
The position of the helical blade according to the Cleveland and Bosworth quadrants showed the following distribution by quadrants: 1 (0.8%), 2 (0%), 3 (0%), 4 (9.4%), 5 (64.1%), 6 (0.8%), 7 (11.7%), 8 (13.2%) and 9 (0%) (Fig. 1). The Baumgaertner tip-apex distance, which should be less than 25mm to decrease the incidence of cut out,1,4,14,19,20 was confirmed in 91.5% of cases, with a mean distance of 17.48mm (range: 5.84–35.88mm).
The mean hospital stay of our patients was 9.17 days (range: 4–35 days), with a mean time prior to surgery of 3.22 days (range: 0–19 days) and a mean postoperative admission period of 5.95 days (range: 3–18 days).
The mean follow-up period was 1.6 years (range: 11–31 months). We recorded 3 losses during follow-up, in addition to cases of exitus letalis.
Regarding the functional capacity of patients, 63% belonged to group 1 (no aid or a single, simple support). Of these, only half (47%) maintained this status in the postoperative period, with the remaining cases presenting a reduction of functional capacity (47% required a walking frame or 2 crutches, and the remaining 6% required a wheelchair). Prior to the fracture, 34% of patients needed 2 crutches or a walking frame for ambulation (group 2), whilst this figure increased to 57% of the sample during follow-up. The percentage of patients who required a wheelchair due to inability for ambulation (group 3) was tripled (from 4% at baseline to 12% during follow-up).
The intrahospital mortality rate stood at 1.5%, whilst the figure during the 1 year follow-up period was 15.6%.
Complications were classified into 3 groups:
- 1.
Intraoperative mechanical complications: 1 case of failure upon insertion of the distal screw (0.5%).
- 2.
Postoperative mechanical complications: 2 cases of cut out (1%), 1 case of cut through (0.5%), 4 cases of helical blade sliding effect (lateral movement of the trochanteric mass due to sliding of the blade and diaphyseal medialization and collapse at the level of the fracture) (2%), 2 cases of discomfort in the fascia lata unrelated to cases of blade retropulsion (1%), 1 case of delayed consolidation which required dynamization (0.5%), 2 cases of pseudoarthrosis (or nonunion) which in both cases led to breakage of the device (1%) and 1 case of avascular necrosis (0.5%).
- 3.
Non-mechanical complications: 1 case of continuous active bleeding related to the intervention (0.5%) and 1 case of deep vein thrombosis (0.5%).
Overall, mechanical complications accounted for 7.5%, although only 3.5% required surgical revision.
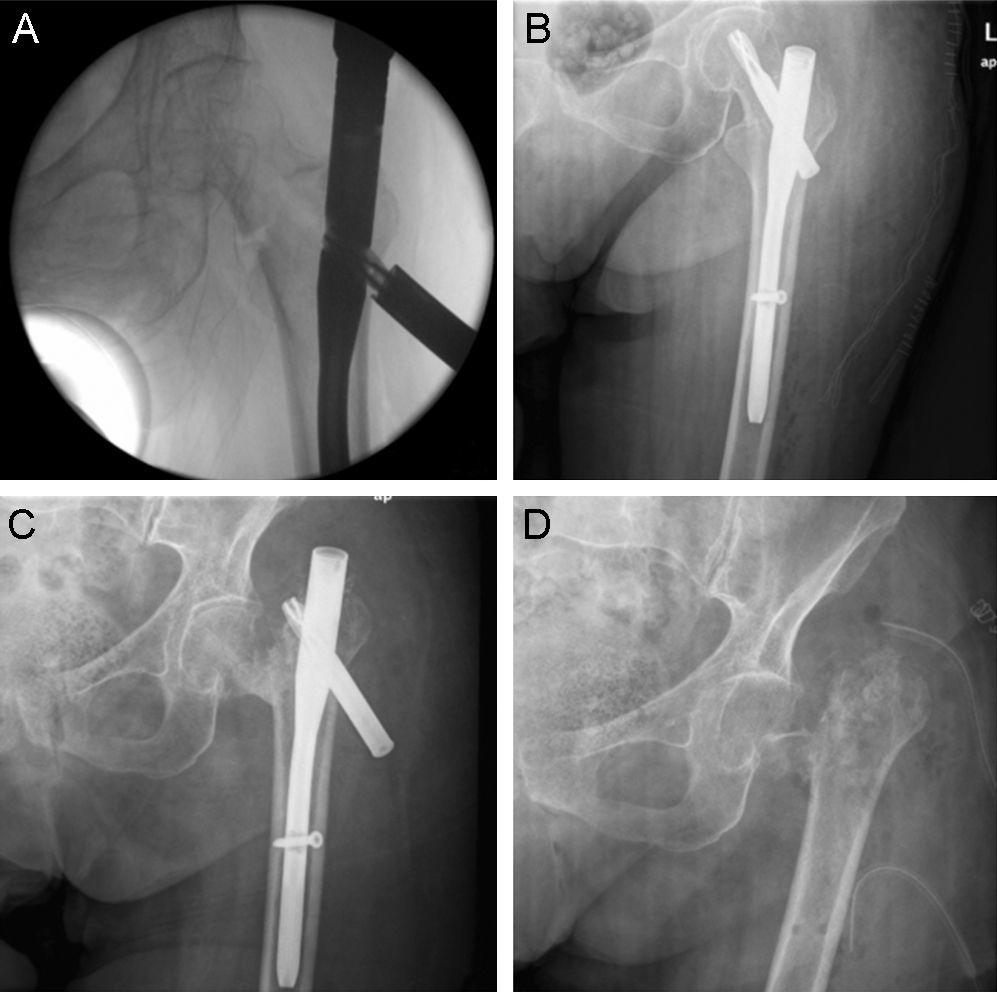
Cut out: we observed 2 cases of cut out. The first case presented concomitant infection in addition to the mechanical complication. Thus, after considering the age, comorbidity and functional capacity of the patient, we decided to extract the osteosynthesis material from the femoral head and neck (Girdlestone technique) in a single surgical action. The patient was able to walk using a walking frame, albeit with relative difficulty (Fig. 2).
Fracture with a basicervical line treated by PFNA nailing. During its introduction, the helical blade reached the subchondral bone so it was partially removed, revealing the channel created by compaction of the trabeculae (A). Postoperative control (B). Cut out (C). Definitive treatment through a Girdlestone procedure (D).
In the other case, a 31-A1.2 fracture, after analyzing the images we observed a delayed union and progressive mobilization of the blade, which resulted in a subcapital fracture at the point of exit of the blade. It was resolved by a Thompson hemiarthroplasty after extraction of the nail, with satisfactory evolution after this intervention and requiring a walking frame for ambulation (Fig. 3).
Pertrochanteric fracture with a simple line treated by PFNA nailing. Postoperative control (A). A slight collapse took place during the evolution, which was consolidated with lateral migration of the blade (B). The point of fracture can be observed at a subcapital level (coinciding with the tip of the blade), along with nonunion. Cut out. (C). We opted for surgical treatment by hemiarthroplasty with a Thompson type cemented prosthesis (D).
Cut through: we proceeded to extract the osteosynthesis material due to the low functional demands of the patient.
Pseudoarthrosis or nonunion: there were 2 cases of nonunion. Both cases were 31-A3.3 fractures with an inverse oblique pattern, showing a gap over 5mm after surgical reduction. In these patients, nonunion conditioned the breakage of the osteosynthesis material. Only 1 patient was surgically reoperated: replacement of a short nail for a long one, together with cementing through the helical blade. In the other case, the considerable morbidity and mortality and good tolerance to the condition led us to choose a conservative treatment.
We stratified patients into 2 groups according to the presence or absence of mechanical complications. Within these groups we analyzed the location of the blade in an ideal position (center–center) or other positions, which were considered “suboptimal”. We observed significant differences regarding the development of mechanical complications between the group with a center–center position with respect to the group with “suboptimal” positions (P=.04) (Table 3). We then analyzed the tip-apex distance in these same 2 groups, and found that the mean tip-apex distance in the group with mechanical complications was 18.03mm (range: 5.84–33.58mm) compared to 17.38mm (range: 5.84–35.88mm) in the group without complications. These values were not statistically significant (P=.897).
Distribution of the position of the helical blade in the Cleveland and Bosworth quadrants within the groups stratified according to presence of postoperative mechanical complications and absence of complications.
| Group with complications (%) | Group without complications (%) | ||||
| 8.33 | 0 | 0 | 0 | 0 | 0 |
| 8.33 | 50 | 8.33 | 9.56 | 66.08 | 0 |
| 16.66 | 8.33 | 0 | 10.43 | 13.91 | 0 |
Finally, we stratified according to the quality of the reduction. In the group with postoperative mechanical complications the quality of the reduction was good or acceptable in 86.6% of cases, whereas in the group without complications this figure rose to 99.46%, resulting in a statistically significant difference (P=.04).
The results of our study were compared with those obtained in another study conducted 1 year earlier at our center with a sample of 700 patients intervened due to hip pertrochanteric osteoporotic fracture using a gamma 3 nail and TFN for 5 years. This study only measured the following mechanical complications: cut out (3.4%), cut through (1.6%), fracture varization (0.5%), helical blade sliding effect (2.5%), decoupling of the system (0%), breakage of the device (0%), failure of the distal screw guide (0.8%) and blade contact at the level of the fascia lata (0.4%), obtaining a total rate of 9.2% mechanical complications derived from the use of a nail, compared to 7.5% obtained in our series (P=.469). Nevertheless, reducing the observation to those complications studied in both works which required reoperation (cut out, cut through and nonunion), we observed that the incidence was reduced from 5% to 2.5% (P=.13).
DiscussionMechanical complications are the most frequent type of complications leading to implant failure and requiring reoperation. The factors which condition such failures can be divided into “modifiable” and “non-modifiable”. The first include bone mineral density and fracture type, whilst the latter are those known as “surgeon-dependent” (Baumgaertner tip-apex distance, position of the blade, fracture reduction and choice of implant). It is on the latter that we can primarily act in order to improve the final results of osteosynthesis.
The development and improvement of new osteosynthesis systems, as well as a meticulous surgical technique, have reduced the rate of surgeon-dependent mechanical complications.
The results of our study are consistent with those obtained by other working groups which observe a reduction in the incidence of mechanical complications among those cases in which the blade was located in the center of the femoral head and neck.1,14 The percentage of patients in the sample with a suboptimal tip-apex distance has been reduced, which may have had an influence on reducing the significant variability in terms of the relationship between this distance and the incidence of complications. Other studies have found similar results regarding the tip-apex distance. The series of Herman et al.14 reported a tip-apex distance of 20.3mm (SD: 6.5) in the group of patients without mechanical complications and 24.0mm (SD: 6.5) in the group of patients with cut out (P=.175). This could raise the point that the position of the blade in the Cleveland and Bosworth quadrants may be of greater importance than the Baumgaertner tip-apex distance. There are very few research works with nail systems using a helical blade, since the original study showed the results in patients treated with screw-sliding plate systems. The first study to assess the tip-apex distance with nailing was conducted by Geller et al.21 with results similar to those of Baumgaertner. Other studies have also been conducted which evaluated measurement using the PACS22 fluoroscopy system during the surgical intervention, allowing placement and correction during surgery until a suitable subchondral position was achieved. In our previous series of 700 patients treated with other types of nails, the mean value of this parameter was 21mm (range: 9–37mm).
We did not carry out a radiographic evaluation of the degree of osteoporosis according to the method of Singh because there is controversy regarding the results of published studies, which associate the Singh trabecular pattern with mechanical complications.14,23 In addition, there is considerable intra- and interobserver variability in the classification of the Singh pattern,24 making this parameter scarcely reliable in establishing whether osteoporosis is a determining factor in the results. There are new studies which attempt to relate the diameter of the medial cortex and the degree of bone fragility, which may become determinant in the future to establish whether or not there is a frank association between osteoporosis and mechanical complications.
Mortality data during the first year of follow-up reflected a survival of 84.4% versus the expected figure of 75% according to other studies.3 This improvement could be the result of a precise coordination between the Departments of Traumatology, Anesthesia and Geriatrics, enabling ongoing medical care, surgical intervention and early ambulation, as well as prevention and treatment of complications arising during hospital stay.
In the analysis of complications we found 4 cases of cut out related to fractures with a single basicervical stroke, which led us to consider alternative causal mechanisms other than the position of the helical blade. One possible explanation lies in cephalic rotation,25–27 conditioned by the absence of muscle insertions which stabilize the fracture line, and cause the head to rotate on the nail, both during insertion of the helical blade and during ambulation. Some new theories suggest that the torsional forces exerted on the blade during ambulation cycles may cause the trabeculae surrounding the implant to rupture, with a subsequent rotation of the femoral head on the blade, causing a “shear” movement on the surrounding bone and initiating a progressive osteolysis during ambulation cycles (“windshield effect”) which will eventually lead to the development of cut out.28 In order to prevent this cascade of events, we are currently employing new technical variants, including the use of anti-rotation screws or cementing through the blade, in certain types of fractures with rotational instability, which could further reduce the rates of mechanical complications. The results have yet to be analyzed.
In our opinion, the first case of cut out could be attributed to an error in the surgical technique since, after inserting the helical blade and conducting the relevant checks with the image intensifier, the surgeon realized that the blade had been introduced too close to the articular cartilage, and conducted a partial extraction and subsequent reintroduction in a position farther from the cartilage. This extraction and subsequent reintroduction of the blade could have caused trabecular impaction, initially beneficial to promote anchoring of the blade, to be lost during reintroduction of the blade through the same channel. This would allow the rotation of the femoral head during ambulation cycles due to the rupture of the trabeculae around the blade. We suggest that cases such as this may be susceptible to cementing through the helical blade or to addition of a cannulated screw in order to block these torsional forces.
As expected, group 31-A3 fractures led to a notable number of delayed consolidations and nonunions compared with other types of fractures (31-A1 and 31-A2), attributable in part to a poor quality of reduction, with gaps greater than 5mm in the point of fracture, and to the high instability thereof, caused by the absence of the lateral wall, which should act as a buttress for blade sliding.
At present, in our center we perform surgical treatment of all these fractures by the intramedullary, proximal femoral nail anti-rotation (PFNA) system. We choose this system because of its improved mechanical properties and lesser inflection compared to the screw-sliding plate system, due to its more medial position. Nailing has shown better results than the screw-plate system for unstable pertrochanteric fractures of the femur.2,29 When comparing with our historical series (based on TFN and gamma 3 nailing), we have observed a decrease in the incidence of these complications, although follow-up periods were shorter. This lower incidence of complications may be due to the fact that the helical blade provided angular and rotational stability by compacting the spongy tissue as it was inserted, thus giving it greater anchoring capacity and allowing sliding, once blocked, which favored fracture point compression.30,31
The strength of the study was, firstly, that the intervention was performed by the same senior surgeon, thus preventing the results from being influenced by technical implementation by different surgeons. Secondly, the scarce losses during follow-up, both due to mortality and to absence from consultation, did not substantially affect the variable being studied. Thirdly, monitoring was always longer than 6 months for all cases studied, thus ruling out belated, undocumented complications, since almost all appeared within that time interval. Lastly, we did not only evaluate the primary, qualitative, dichotomous variable of presence or absence of “complications”, but also secondary variables, like the “functionality” of patients.
The limitations of this study include it being a retrospective study, thus making it impossible to assess certain variables not routinely collected in the evolution forms. In addition, a larger sample size could have provided more statistically significant results, since the study variables were numerous and the rate of complications was low.
ConclusionsNailing is an effective treatment for pertrochanteric fractures of the femur (31-A). The helical blade system of PFNA appears to reduce the incidence of cut out and cut through. Lateral migration of the blade allows impaction of the fracture and consolidation thereof (although it may increase rates of friction with the fascia lata, varus consolidation and shortening). The position of the blade represents one of the main parameters associated with mechanical complications. Although other studies have shown the importance of the tip-apex distance, given the characteristics of our series, we could not observe this fact.
Level of evidenceLevel of evidence III.
Ethical responsibilitiesProtection of people and animalsThe authors declare that this investigation did not require experiments on humans or animals.
Confidentiality of dataThe authors declare that this work does not reflect any patient data.
Right to privacy and informed consentThe authors declare that this work does not reflect any patient data.
Conflict of interestsThe authors have no conflict of interests to declare.
Please, cite this article as: Aguado-Maestro I, et al. Resultados y complicaciones de la osteosíntesis de fracturas pertrocantéreas de fémur mediante clavo endomedular con espiral cefálica (clavo femoral proximal antirrotación) en 200 pacientes. Rev Esp Cir Ortop Traumatol. 2013;57:201–7.