Hip fracture is a very frequent traumatic pathology in the elderly with high mortality. Different factors have been associated with mortality after surgery (age comorbidities). There are surgical factors that are associated with mortality, but they have not been related to the different mortality rates and medical comorbidities.
ObjectiveTo analyse the surgical parameters with influence on mortality in surgery of extracapsular hip fractures in the elderly patient, as well as the influence of medical comorbidities of these patients on mortality, by means of the Charlson comorbidity index (CCI).
MethodRetrospective review of 187 patients operated on in 2015. Data were collected on age and sex, laterality and type of fracture; surgical delay, surgical time, type of osteosynthesis material, mean stay. The presence of comorbidities was determined using the JRC.
ResultsMean age was 85 years. Regarding the Charlson comorbidity index in brief, 67.4% of patients had a score between 0 and 1, 23.5% of 2, and 9.1% of >2. Mortality at one month and one year after surgery was 5.3% and 14.4% respectively. Forty-three complications were recorded, of which 31 were medical complications. Of the 27 patients who died in the first year, 14 (51.8%) suffered complications, 48.2% of which were medical complications.
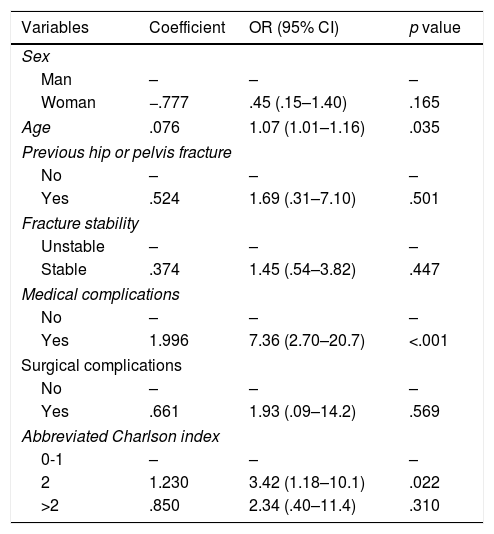
DiscussionMultivariate analysis showed significant differences with respect to age, medical complications and Charlson index abbreviated to 2 with respect to mortality. There is no association between delay and surgical time with increased mortality.
ConclusionsNo association was demonstrated between the surgical parameters studied (surgical delay and time, fracture pattern and stability, reduction criteria, surgical complications) and increased short and long-term mortality. Patients with older age, comorbidities measured with abbreviated CCI and those suffering medical complications have a higher risk of mortality at the month and year of surgery.
La fractura de cadera es una patología traumática muy frecuente en el anciano con alta mortalidad. Diferentes factores se han asociado con la mortalidad tras la cirugía (edad comorbilidades). Hay factores quirúrgicos que se asocian con la mortalidad, pero no se han relacionado con los diferentes índices de mortalidad y comorbilidades médicas.
ObjetivoAnalizar los parámetros quirúrgicos con influencia en la mortalidad en la cirugía de las fracturas extracapsulares de cadera en el paciente anciano, así como la influencia de las comorbilidades médicas de estos pacientes en la mortalidad, mediante el índice de comorbilidad de Charlson abreviado (CCI).
Material y métodoRevisión retrospectiva de 187 pacientes intervenidos en 2015. Se recogieron datos sobre la edad y sexo, lateralidad y tipo de fractura; demora quirúrgica, tiempo quirúrgico, tipo de material de osteosíntesis, estancia media. La presencia de comorbilidades se determinó empleando el CCI.
ResultadosLa edad media fue de 85 años. Con respecto al índice de comorbilidad de Charlson abreviado, 67,4% de los pacientes tenían una puntuación entre 0 y 1, el 23,5% de 2, y un 9,1% > 2. La mortalidad al mes y al año tras la cirugía fue de 5,3% y 14,4%, respectivamente. Se registraron 43 complicaciones, de las cuales 31 fueron complicaciones médicas. De los 27 pacientes fallecidos en el primer año, 14 (51,8%) sufrieron complicaciones, 48,2% de las mismas fueron complicaciones médicas.
DiscusiónEl análisis multivariante mostró diferencias significativas con respecto a edad, complicaciones médicas e índice de Charlson abreviado de dos con respecto a la mortalidad. No existe asociación entre demora y tiempo quirúrgico con el aumento de la mortalidad.
ConclusionesNo se demostró asociación de los parámetros quirúrgicos estudiados (demora y tiempo quirúrgico, patrón y estabilidad de la fractura, criterios de reducción, complicaciones quirúrgicas) con aumento de mortalidad a corto y largo plazo. Los pacientes con mayor edad, comorbilidades medidas con CCI abreviado y los que sufren complicaciones médicas presentan mayor riesgo de mortalidad al mes y al año de la cirugía.
Hip fracture is a very frequent traumatic pathology in the elderly. Osteoporosis and reduction in the neck-shaft angle of the femur with age alters the bone architecture and leads to fracture. However, there are other factors which are not related to bone structures, such as cognitive or somatosensorial changes, heart diseases and changes to movement that also impact hip fractures in the elderly population.1
As the population ages, the number of patients with hip fractures increases. However, due to the growing interest in this population and the development of fall prevention strategies a reduction in the rate of this traumatic pathology is generated.1
This pathology is associated with high morbidity and mortality.2 As such it has become a medical and social problem in the elderly population.3 Optimisation of its management must become a priority from both a medical and a socio-economic perspective,4 since the cost of treatment for a patient with a hip fracture in the U.S.A. is currently estimated to be between $11,844 and $13,805 (€9942 to €11,590 per patient).5
Due to an increase in life expectancy, the risk of suffering from a hip fracture and the associated costs have progressively increased in recent years6; and it is expected that this trend will continue to rise in upcoming decades, from 250,000 procedures per year at present to 500,000 procedures annually in the year 2040.7
Published mortality rates following proximal femur fracture are between 6% and 9% the first month and 26% and 33% the first year.8,9 Different factors have been associated with mortality after hip fracture surgery in the literature and these are essentially the patient's age, sex and medical comorbidities.10–16
Different scoring systems which sum up a patient's overall health status have begun to be used to seek associations between comorbidity and mortality in hip fracture surgery. These include those of the ASA (American Society of Anaesthesiologists), the Elixhauser Index, the Nottingham Hip Fracture Score and the Charlson comorbidity index (CCI) all of which may be useful for decision-making.12
Despite this, the available data for associating the CCI with mortality after extracapsular hip fracture surgery are limited because the majority of studies analyse mortality of hip fracture globally, without differentiating between intra and extracapsular fractures.
There is consensus on the comprehensive assessment of the elderly patient with a hip fracture and it has been observed that by offsetting their pathological status prior to undergoing surgery improves outcomes.17
Due to all of the above the main aim of this study was to analyse whether any relationship was described in the literature between surgical parameters and mortality in extracapsular hip fractures in the elderly patient in the Spanish population (delay until surgery, time in surgery, fracture stability, criteria for intraoperative reduction, complications18–20).
The impact of medical comorbities in mortality following extracapsular hip fracture surgery in the elderly patient was also to be analysed using the abbreviated Charlson comorbidity index.
Material and methodA retrospective review of a case series using medical file analysis was designed.
The population studied included all patients over 65 years of age who had been admitted to our hospital centre with a diagnosis of extracapsular hip fracture and who had undergone surgery during 2015.
Selection criteria were that the patient had undergone extracapsular hip fracture surgery and was over 65 years of age. Pathological fractures and those caused by high energy trauma were excluded from this study.
The list of all these patients was obtained through the medical file archive, using hospital discharge coding.
A review of surgical complications one year after surgery was also undertaken.
The following data were obtained (with prior authorisation from the ethics committee) through review of medical files: age, sex and fracture side as well as whether they had previously suffered from any fractures. Other collected variables were the time period from fracture to surgery (delay to surgery), type of anaesthesia used, time in surgery and type of material used for surgery (Gamma3® [Stryker, Kalamazoo, U.S.A.] or Charfix® [ChM, Juchnowiec Kościelny, Poland]) endomedular nail, together with total time of hospital stay.
The electronic medical file used in the Servicio Galego de Saúde (SERGAS) is available through a computerised system which includes in real time all clinical information of the different care levels, thus providing information on the survival of our patients one month and one year after surgery, both inside and outside the hospital because this information is automatically updated and integrated into the death registration services.
The type of extracapsular fracture of the femur was classified according to the AO classification (Arbeitsgemeinschaft für Osteosynthesefragen), proposed by Müller et al. in 1980–1987 and modified by Meinberg et al.18 in 2018.
The fractures were divided for analysis into two subgroups in accordance with their stability: stable vs unstable, in keeping with the new AO classification.18
Those considered unstable were the ones which have proven to be difficult to manage due to being reverse oblique fractures, or due to fragmentation of the greater trochanter and/or loss of lateral cortical bone since these factors increase their instability and hinder reduction.21
The presence of associated comorbidities was determined by anamnesis on admission and by ongoing clinical review during hospital stay. Comorbidities recorded were those described in the abbreviated Charlson comorbidity index: vascular brain disease, diabetes mellitus, chronic obstructive pulmonary disease, heart failure or ischaemic heart disease, dementia, peripherical arterial disease, chronic kidney failure in dialysis and cancer.
The Charlson comorbidity index (CCI) contains 19 items which aim to study the conditions patients suffer from. Its abbreviated version only includes six items and is easier to handle. Although it may apparently seem less precise than the complete original version its prognostic use in the short term is similar.13
The number of comorbidities in the Charlson comorbidity index were determined for analysis of the impact of medical comorbidities on mortality in surgery of extracapsulares hip fractures, focusing on mortality one month and one year after surgery.
The medical complications suffered during hospital stay were also recorded, including urinary tract infection, respiratory infection, kidney failure, pneumonia, bronchoaspiration, pleural effusion, cardiac complications (auricular fibrillation, congestive heart failure, heart attack), pulmonary thromboembolism, and Olgilvie's syndrome.
Recorded surgical complications (both during hospital stay and during the year after surgery) included infection (superficial or profound) of the surgical wound, the need for reintervention and pseudo-osteoarthritis (defined as failure of fracture consolidation22).
Data were collected from the X-rays of the patients and fracture reduction criteria after surgery according to the modified Baumgaertner index.23
Statistical analysisFirstly, an exhaustive descriptive analysis of the sample was undertaken. For categorical variables a number of absolute cases and percentages were presented. The fit to normality of the continuous variables was contrasted using the Kolmogorov–Smirnov–Lilliefors test. Means and standard deviations were used for variables with fit to normality and in the contrary case, medians and interquartile ranges. This descriptive analysis was combined with graphic analysis.
Bivariate analysis was performed to respond to study objectives. For categorical variables the Chi-squared test was used and for variables not within utility assumptions the Fisher exact test was used.
For continuous variables, when they fitted to normality a mean comparison test (Student's t-test) was performed. If there was no fit to normality the Mann–Whitney U test was applied. Finally, to contrast the impact of each variable on mortality, a joint multivariate analysis was performed, using logistic regression.
All analyses were performed with the statistical software SPSS 19.0 (IBM Corp. Released 2011. IBM SPSS Statistics for Windows, Version 20.0. Armonk, NY: IBM Corp.) and R 3.3.2 (R Core Team (2018). R: a language and environment for statistical computing. R Foundation for Statistical Computing, Vienna, Austria).
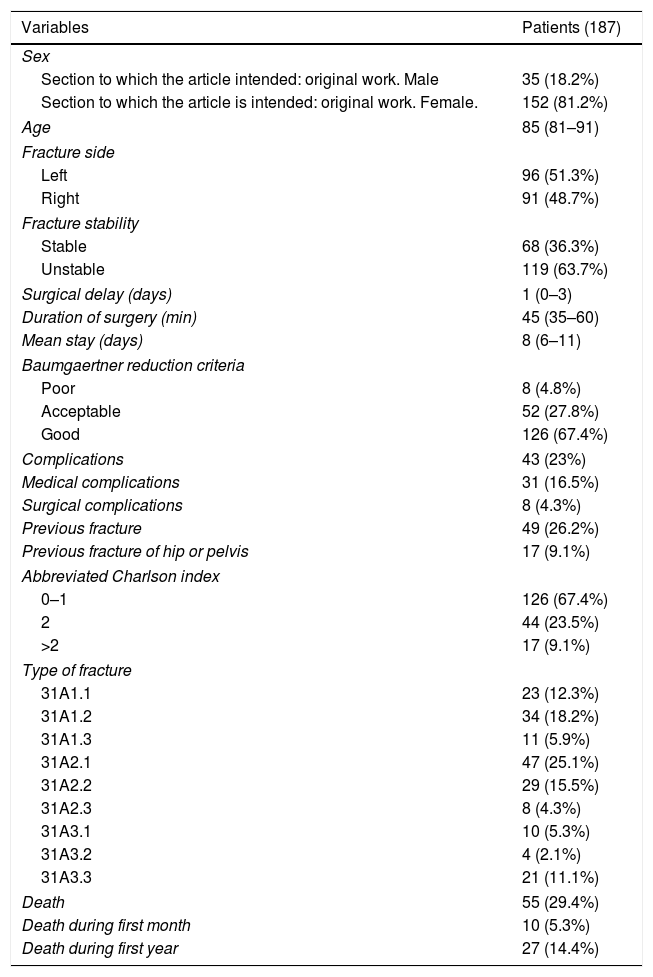
ResultsDuring the study period 187 patients over 65 years of age with extracapsular fracture of the femur, who met with the inclusion criteria were admitted to our service. The general study data are presented in Table 1.
Sample description.
| Variables | Patients (187) |
|---|---|
| Sex | |
| Section to which the article intended: original work. Male | 35 (18.2%) |
| Section to which the article is intended: original work. Female. | 152 (81.2%) |
| Age | 85 (81–91) |
| Fracture side | |
| Left | 96 (51.3%) |
| Right | 91 (48.7%) |
| Fracture stability | |
| Stable | 68 (36.3%) |
| Unstable | 119 (63.7%) |
| Surgical delay (days) | 1 (0–3) |
| Duration of surgery (min) | 45 (35–60) |
| Mean stay (days) | 8 (6–11) |
| Baumgaertner reduction criteria | |
| Poor | 8 (4.8%) |
| Acceptable | 52 (27.8%) |
| Good | 126 (67.4%) |
| Complications | 43 (23%) |
| Medical complications | 31 (16.5%) |
| Surgical complications | 8 (4.3%) |
| Previous fracture | 49 (26.2%) |
| Previous fracture of hip or pelvis | 17 (9.1%) |
| Abbreviated Charlson index | |
| 0–1 | 126 (67.4%) |
| 2 | 44 (23.5%) |
| >2 | 17 (9.1%) |
| Type of fracture | |
| 31A1.1 | 23 (12.3%) |
| 31A1.2 | 34 (18.2%) |
| 31A1.3 | 11 (5.9%) |
| 31A2.1 | 47 (25.1%) |
| 31A2.2 | 29 (15.5%) |
| 31A2.3 | 8 (4.3%) |
| 31A3.1 | 10 (5.3%) |
| 31A3.2 | 4 (2.1%) |
| 31A3.3 | 21 (11.1%) |
| Death | 55 (29.4%) |
| Death during first month | 10 (5.3%) |
| Death during first year | 27 (14.4%) |
Medians and interquartile ranges (continuous variables) or absolute number and percentage (categorical variables).
The mean age of the patients was 85 years (81–89 years). 81.2% (152 cases) were women.
The patients stayed a mean of eight days in hospital (6–11 days). Delay to surgery was one day (median, with interquartile range of 0–3 days). All patients were operated on under spinal anaesthesia.
Regarding the fracture, 68 of them were considered stable (36.3%). According to the modified Baumgaertner reduction criteria, 126 fractures were considered to have good reduction (67.4%), 52 acceptable reduction (27.8%), and eight poor reduction (4.8%). In one fracture no postoperative control was carried out, and therefore no reduction data were obtained.
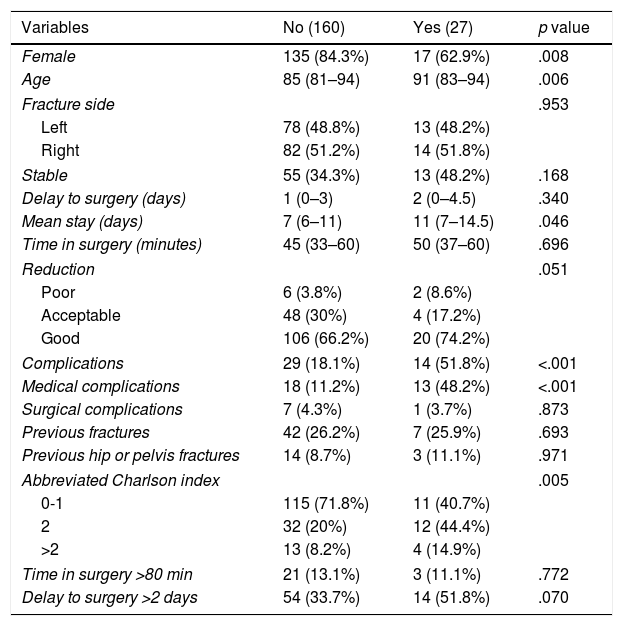
Regarding mortality, 27 patients (14.4%) died during the first year after surgery, 10 (5.3%) of whom died during the first month. The mean age of the patients who died was 91 years. By sexes, 17 were women (62.9%). Of the 27 patients who died during the first year, 14 suffered from complications (51.8%), 13 of which were medical complications (48.2%) and one surgical (3.7%, osteosynthesis material infection). The bivariate analysis regarding death during the first year (Table 2) showed significant differences regarding sex, age, medical complications and abbreviated Charlson index.
Bivariate analysis with regard to death in the first year.
| Variables | No (160) | Yes (27) | p value |
|---|---|---|---|
| Female | 135 (84.3%) | 17 (62.9%) | .008 |
| Age | 85 (81–94) | 91 (83–94) | .006 |
| Fracture side | .953 | ||
| Left | 78 (48.8%) | 13 (48.2%) | |
| Right | 82 (51.2%) | 14 (51.8%) | |
| Stable | 55 (34.3%) | 13 (48.2%) | .168 |
| Delay to surgery (days) | 1 (0–3) | 2 (0–4.5) | .340 |
| Mean stay (days) | 7 (6–11) | 11 (7–14.5) | .046 |
| Time in surgery (minutes) | 45 (33–60) | 50 (37–60) | .696 |
| Reduction | .051 | ||
| Poor | 6 (3.8%) | 2 (8.6%) | |
| Acceptable | 48 (30%) | 4 (17.2%) | |
| Good | 106 (66.2%) | 20 (74.2%) | |
| Complications | 29 (18.1%) | 14 (51.8%) | <.001 |
| Medical complications | 18 (11.2%) | 13 (48.2%) | <.001 |
| Surgical complications | 7 (4.3%) | 1 (3.7%) | .873 |
| Previous fractures | 42 (26.2%) | 7 (25.9%) | .693 |
| Previous hip or pelvis fractures | 14 (8.7%) | 3 (11.1%) | .971 |
| Abbreviated Charlson index | .005 | ||
| 0-1 | 115 (71.8%) | 11 (40.7%) | |
| 2 | 32 (20%) | 12 (44.4%) | |
| >2 | 13 (8.2%) | 4 (14.9%) | |
| Time in surgery >80 min | 21 (13.1%) | 3 (11.1%) | .772 |
| Delay to surgery >2 days | 54 (33.7%) | 14 (51.8%) | .070 |
Values expressed in medians and interquartile ranges (continuous variables) or absolute cases and percentages (categorical variables).
P-values calculated with the Mann–Whitney U test (continuous variables) or Chi-squared test (categorical variables).
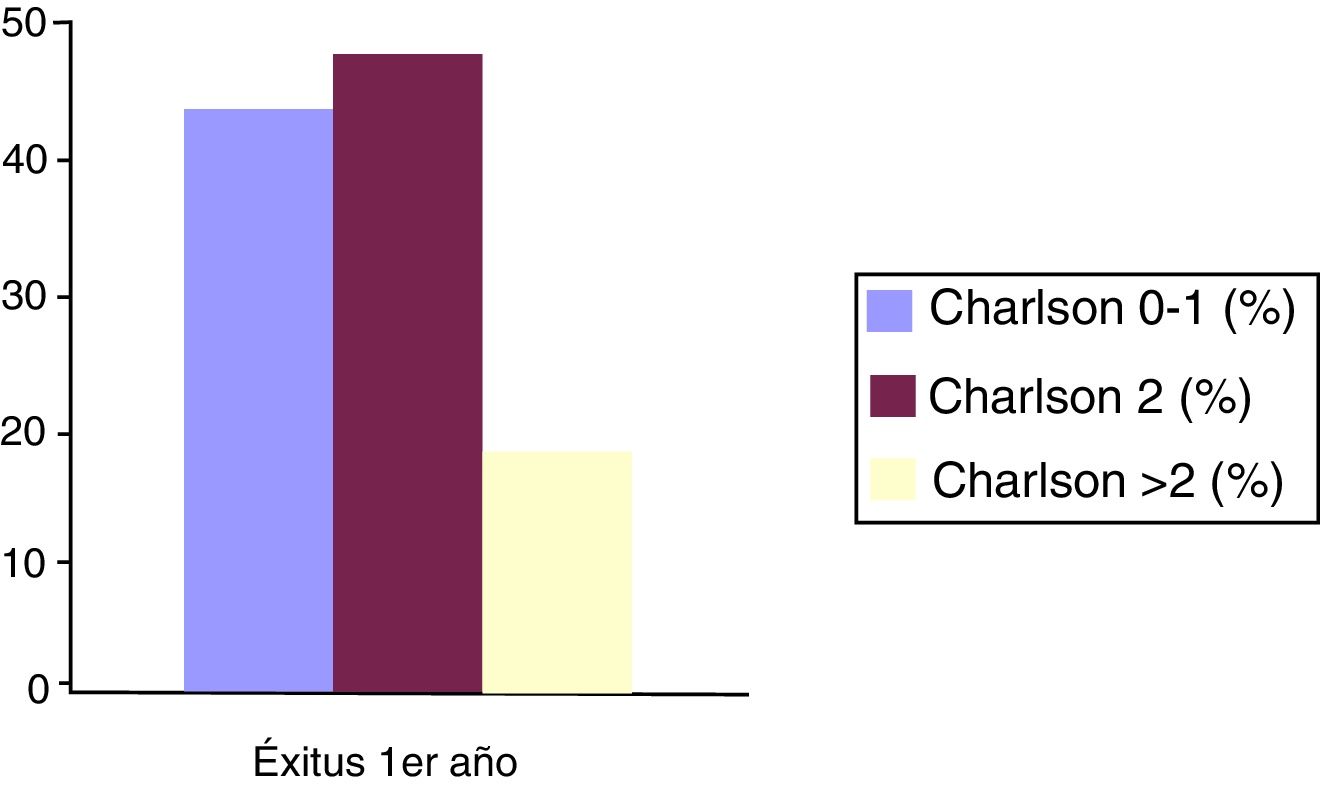
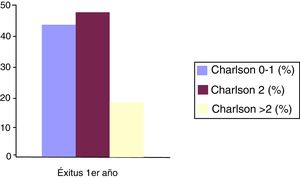
Specifically, regarding the abbreviated Charlson comorbidity index, of the 27 patients who died in the first year, 40.7% had an index between 0 and 1 (absence of comorbidity according to the criteria of said index), 44.4% a score of 2 (low comorbidity), and 14.9% had a Charlson index score higher than 2 points (Fig. 1).
Regarding surgical parameters analysed, no statistically significant association was demonstrated between a greater delay to surgery or time in surgery with increased mortality.
Similarly, no relationship was found between fracture stability (stable vs. unstable) with increased mortality.
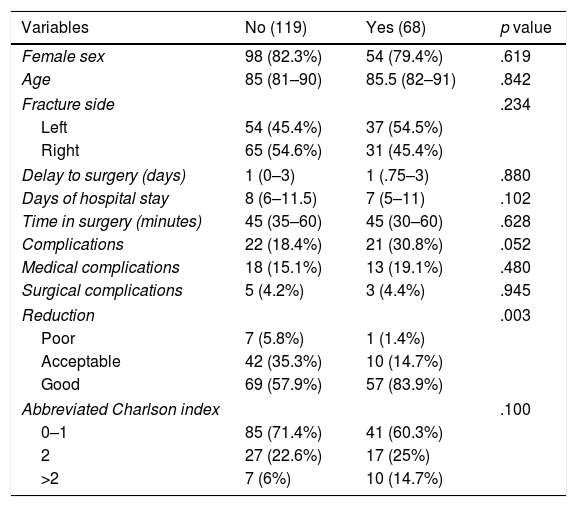
Bivariate analysis was also performed seeking a relationship between fracture stability with regard to the different surgical parameters analysed, but there was no association with any of the parameters studied except with fracture reduction, where a statistically significant association was demonstrated (p .003) between fracture stability and reduction, obtaining better reduction in stable fractures (Table 3).
Bivariate analysis with regard to fracture stability.
| Variables | No (119) | Yes (68) | p value |
|---|---|---|---|
| Female sex | 98 (82.3%) | 54 (79.4%) | .619 |
| Age | 85 (81–90) | 85.5 (82–91) | .842 |
| Fracture side | .234 | ||
| Left | 54 (45.4%) | 37 (54.5%) | |
| Right | 65 (54.6%) | 31 (45.4%) | |
| Delay to surgery (days) | 1 (0–3) | 1 (.75–3) | .880 |
| Days of hospital stay | 8 (6–11.5) | 7 (5–11) | .102 |
| Time in surgery (minutes) | 45 (35–60) | 45 (30–60) | .628 |
| Complications | 22 (18.4%) | 21 (30.8%) | .052 |
| Medical complications | 18 (15.1%) | 13 (19.1%) | .480 |
| Surgical complications | 5 (4.2%) | 3 (4.4%) | .945 |
| Reduction | .003 | ||
| Poor | 7 (5.8%) | 1 (1.4%) | |
| Acceptable | 42 (35.3%) | 10 (14.7%) | |
| Good | 69 (57.9%) | 57 (83.9%) | |
| Abbreviated Charlson index | .100 | ||
| 0–1 | 85 (71.4%) | 41 (60.3%) | |
| 2 | 27 (22.6%) | 17 (25%) | |
| >2 | 7 (6%) | 10 (14.7%) | |
Values expressed in medians and interquartile ranges (continuous variables) or absolute cases and percentages (categorical variables).
P-values calculated with the Mann–Whitney U test (continuous variables) or Chi-squared test (categorical variables).
With regard to the abbreviated Charlson comorbidity index, 67.4% of patients had a score between 0 and 1 (absence of comorbidity), 23.5% had a score of 2 (low comorbidity), and 9.1% had a score over 2 points (high comorbidity), thereby demonstrating the association between high scores on the abbreviated Charlson index and the increased risk of mortality (p .005).
Complications were recorded in 43 (23%) patients, out of which 31 were medical complications and eight were surgical complications (one superficial wound infection, one osteosynthesis material infection, two peri-implant fractures, three cases of cut-out (1.6%) and one osteosynthesis material extraction due to intolerance).
Multivariate analysis showed significant differences with regard to age, medical complications and an abbreviated Charlson index of 2 (Table 4).
Multivariate analysis.
| Variables | Coefficient | OR (95% CI) | p value |
|---|---|---|---|
| Sex | |||
| Man | – | – | – |
| Woman | −.777 | .45 (.15–1.40) | .165 |
| Age | .076 | 1.07 (1.01–1.16) | .035 |
| Previous hip or pelvis fracture | |||
| No | – | – | – |
| Yes | .524 | 1.69 (.31–7.10) | .501 |
| Fracture stability | |||
| Unstable | – | – | – |
| Stable | .374 | 1.45 (.54–3.82) | .447 |
| Medical complications | |||
| No | – | – | – |
| Yes | 1.996 | 7.36 (2.70–20.7) | <.001 |
| Surgical complications | |||
| No | – | – | – |
| Yes | .661 | 1.93 (.09–14.2) | .569 |
| Abbreviated Charlson index | |||
| 0-1 | – | – | – |
| 2 | 1.230 | 3.42 (1.18–10.1) | .022 |
| >2 | .850 | 2.34 (.40–11.4) | .310 |
Results obtained by logistic regression.
OR: odds ratios.
Analysis revealed that mortality one month and one year after extracapsular hip fracture surgery during the year 2015 in our hospital was 5.3% and 14.4%, respectively, with rates being lower than those referred to in recently published studies.24–27 Similar data (mortality of 15.6% at one year) were obtained by Aguado-Maestro,28 where he assessed the surgical complications of these patients. However, in our study we wished to associate mortality with both surgical and medical complications since in previous studies a higher score in CCI13 was related to an increase in both hospital12 rates and at 3014 and 90 days,15 as well as the rate of readmissions and hospital stay.16
Sund24 refers to mortality at 30 days of 9.5% in extracapsular hip fractures and of 26.8% at one year; Kleweno26 reports an annual mortality of 25%, and Holt25 of 7% at 30 days. All of these results are higher than those obtained in our study.
Our results acquire greater relevance as they exclusively involve patients with extracapsular fracture, unlike the series published in the literature where the global outcomes of hip fracture are assessed.
There are other factors which are associated with mortality after hip fracture surgery in the elderly person which do not depend on their previous health status, but on the characteristics of the fracture itself and on the type of treatment: fracture type according to the AO18 classification (stable vs. unstable), type of surgical intervention, delay to surgery, time in surgery, and surgical complications.9
Zuckerman published an increase in mortality after the first year of 15% to 21% when surgical intervention was delayed over 48 hours.19
An increase in surgical time for an osteosynthesis of the hip over 80 minutes was also demonstrated to be associated with an increase in the rate of mortality.20 However, it was not clarified whether these surgical parameters were related to the different mortality and medical comorbidity indexes.
Through further analysis of the different surgical parameters which initially, and according to several existing publications in the literature, may be related to the increase in mortality in extracapsular hip fractures in the elderly patient, we were able to confirm that in our study there was no association between delay to surgery and mortality. This also occurs in the Librero,9 and Kopp29 studies and in recent results published in the Hip Attack30 study.
This association has been demonstrated in other studies such as that conducted by Sánchez–Crespo,11 where a higher delay to surgery than two days was associated with an increase in mortality.
Regarding time of intervention, we have not found there to be a statistically significant relationship between higher surgical duration (over 80min) and an increase in mortality, although this was found to be the case in studies such as that of Roux.20
Regarding fracture stability (stable vs. unstable), this parameter does not appear to be related to mortality. The same occurs with surgical complications, where statistical outcomes of our study reflect that there is no relationship between surgical complication and an increase in mortality, with a follow-up of two years.
Both the presence of comorbidities (calculated using the abbreviated CCI) and medical complications during hospital stay are related to short and long term mortality rates in the patient over 65 years of age with an extracapsular hip fracture. These results are similar to those obtained in the Kopp29 study.
LimitationsThis was a retrospective, observational study. Due to the difficulty of collecting information and its quality this type of study may give rise to biases.
Also, the number of patients recruited in certain analysis groups (e.g. abbreviated Charlson index score >2) is limited, and in statistical analyses we therefore obtained a very broad OR. Results should therefore be interpreted with caution.
Furthermore, the current trend in several studies is to analyse specific types of fracture, so as not to generalise data. In this study, we only analysed one specific type of proximal femur fracture, the extracapsular fracture, due to its different management and outcomes. We were unable to find many studies of this type in the recent literature.
ConclusionIt was not possible in this study to demonstrate the association of any of the surgical parameters analysed (delay to surgery, time in surgery, fracture pattern and stability, reduction criteria, surgical complications) with the increase in short and long term mortality in the elderly patient with an extracapsular hip fracture. Similarly, the length of surgery above 80 minutes, and delay to surgery of over two days did not appear to impact the survival of our patients.
Patients with a higher degree of comorbidity, which was estimated using the abbreviated Charlson comorbidity index and those suffering from medical complications during their hospital stay, presented with a higher risk of mortality after one month and after one year from extracapsular hip fracture.
Level of evidenceLevel of evidence III.
Conflict of interestsThe authors did not receive any financial assistance for conducting this study. Neither was any agreement signed to receive profits or fees from any commercial entity. Furthermore, no commercial entity made or will make payments to foundations, educational institutions or other non-profit-making organisations to which we are affiliated.
Please cite this article as: Coto Caramés L, Codesido Vilar PI, Bravo Pérez M, Mendoza Revilla GA, Ojeda-Thies C, Blanco Hortas A, et al. Influencia de parámetros quirúrgicos en la mortalidad tras cirugía de fracturas extracapsulares de cadera en el paciente anciano. Rev Esp Cir Ortop Traumatol. 2020. https://doi.org/10.1016/j.recot.2020.04.003