Medial discoid meniscus is a rare entity with a reported incidence of 0.12 to 0.3, although the real incidence may be greater because not all the patients are symptomatic. Like lateral discoid menisci, medial discoid menisci are prone to degeneration that may prompt the presence of mechanical symptoms at early age. We present the case of a 14 year old male patient with bilateral knee symptons of insidious onset without a traumatic event. Magnetic resonance revealed bilateral medial discoid menisci. Arthroscopic medial meniscus remodelling was performed in the right knee and, three months later, in the left knee, due to limitating mechanical symptoms. At the latest follow up – 6 months for the right knee, 3 months for the left knee -, the patient resumed his sports activities.
El menisco discoideo medial es una entidad muy poco frecuente, con una incidencia reportada de 0.12 al 0.3 aunque la incidencia real puede ser mayor ya que no siempre se manifiesta clínicamente. Al igual que el menisco discoideo lateral, el menisco discoideo medial es susceptible a la degeneración meniscal, lo que puede derivar en síntomas mecánicos en edades tempranas.
Se presenta el caso de un paciente varón de 14 años con dolor de ambas rodillas de inicio insidioso sin relación con traumatismo definido que tras estudio de resonancia es diagnosticado de menisco discoideo medial bilateral con degeneración intrasustancia. Debido a la presencia de síntomas mecánicos limitantes para actividades de la vida diaria y deportivas, se realiza remodelación meniscal primero de la rodilla derecha y, a los 3 meses, de la izquierda, con buenos resultados en el tiempo de seguimiento – 6 y 3 meses, respectivamente -, que permiten a paciente el retorno a las actividades deportivas sin restricciones.
The menisci are cartilaginous “C”-shaped cushions, between the femoral condyles and the tibial saucers, and are composed of type 11 collagen, which is circumferential in nature. The functions of the menisci are to evenly distribute joint load force, stabilize contact between the femur and the tibia and aid joint propioception and lubrication.2
The discoid meniscus is an anatomical variant where the meniscus is larger in size, thickness,3 is irregularly shaped and covers a larger surface area of the tibial saucer than a normal meniscus.4 Some authors refer to the fact that it is also associated with a reduction and alteration to the layout of collagen fibres. This condition was described for the first time by Young in 1889 in a cadaveric specimen and Kroiss made it public in 1910, describing the so-called “spring-loaded knee syndrome”3 for the lateral meniscus.
Lateral discoid meniscus is more common with an incidence of between 1.2% and 5.2% whilst that of medial discoid meniscus is between .12% and .3%. Bilateral presentation is still highly unusual. The real incidence for bilateral medial discoid meniscus is difficult to determine since an unknown percentage of patients are asymptomatic,3 but an incidence of .012%2 has been reported. Discoid meniscus is more common in the Asian population.5
Medial discoid meniscus was first described by Cave and Staples in 1941.4,6 In 1956 Murdoch described the first bilateral case.7 As previously described, incidence is very low and even more so for bilateral cases. A ratio of 3 to 1 has been reported for its presentation, being more frequent in men and 65% of patients are over 18 years of age.8 In the bilateral cases the two menisci usually present with the same type in up to 99% of cases, whether this be type 1 or complete, or type 2 or incomplete, according the Watanabe9 classification with the type 3 or Wrisberg-ligament variant6 being added only in the case of lateral discoid meniscus.
The aetiology of the discoid meniscus has not yet been clarified. In 1948 Smillie et al. postulated that the discoid shape of the meniscus was normal in the embryo, and later the lack of reabsorbing of the central section which persists during the foetal phase leads to a “congenital discoid meniscus”. In 1957 Kaplan proposed that lateral discoid meniscus developed from abnormal mobility caused by the absence of posterior tibial fixation,4 although no author to date has found any presence of discoid meniscus in foetuses or embryos.10–14
For the medial discoid meniscus, the cause was not well defined either. Different studies were made in which it was proposed that the cause in the medial meniscus was the lack of separation between the medial meniscus and the anterior cruciate ligament, the embryonic origin of which are in the same tissue and they normally separate between the ninth and tenth weeks of gestation.15 In 2014 Raheel and McKay8 reported a family case of medial discoid meniscus with meniscal tears in 3 members of the same family, which, although it has not been proven, suggests a probable association between discoid meniscus and a genetic anomaly.4
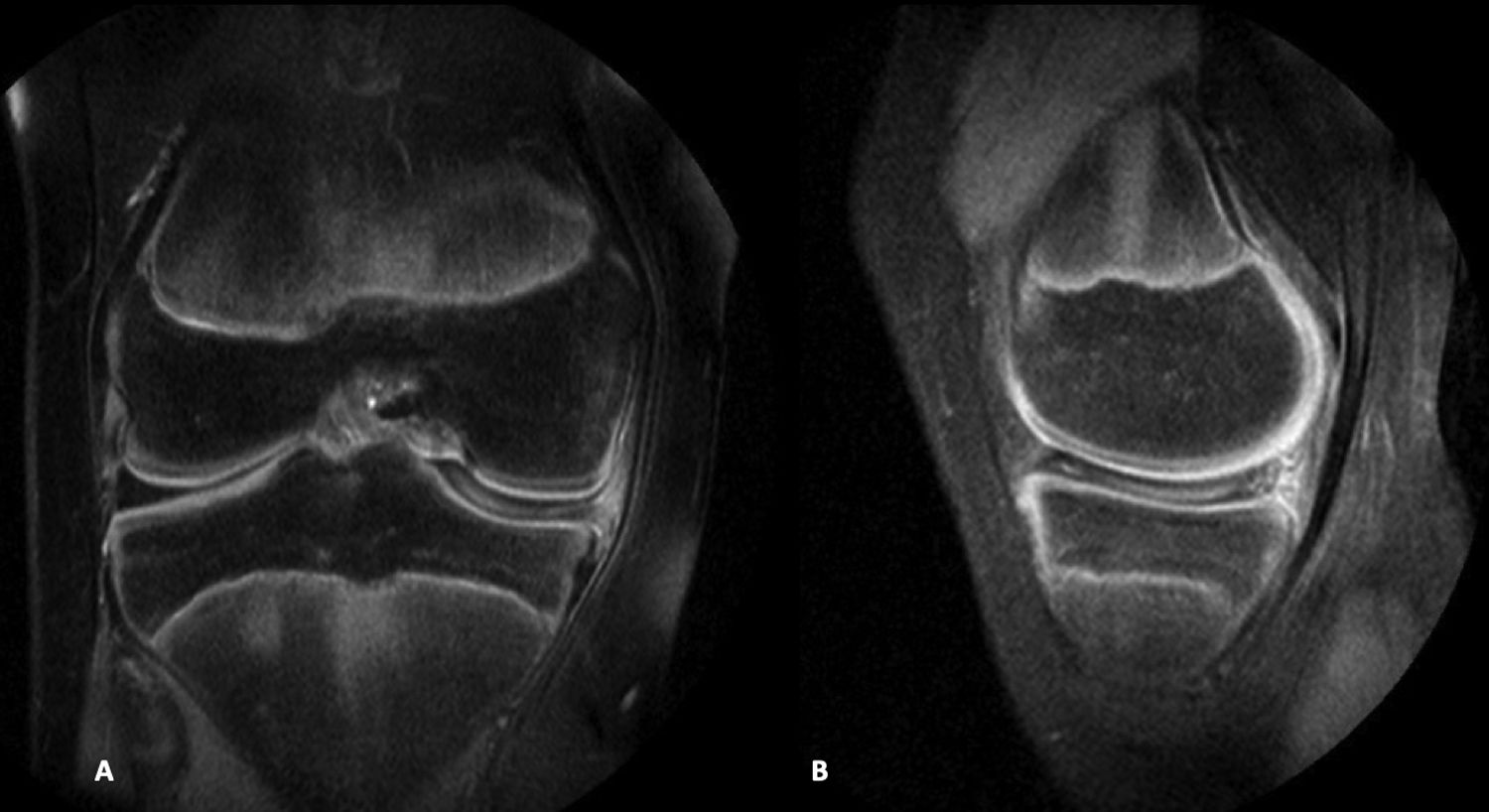
Clinical caseA male, 14-year-old patient presented for consultation due to pain in both knees of insidious onset and predominantly in the right knee, intermittently of 5-year duration. He played basketball and tennis but was frequently in discomfort during the sports activities and had resorted to the use of non steroid anti-inflammatories to be able to practice these sports. On examination pain presented in the medial joint line, with a positive McMurray sign, a negative Lachman sign, without any tears or swelling, with flexion of 140° and extension of 0°, and the remainder of the examination resulting normal. A magnetic resonance of the right knee (Fig. 1) was requested where the integrity of the cruciate and collateral ligaments was observed, the external meniscus of normal morphology and appearance, with no rupture lines. The medial meniscus was discoid with intrameniscal deterioration, with no clear rupture opening to the joint surfaces. According to the Watanabe9 classification (which divides the discoid menisci into complete, incomplete and Wisberg-ligament variant) this was a complete discoid meniscus. The joint cartilage of the kneecap showed no remarkable anomalies. Magnetic resonance was carried out on the left knee where an medial discoid meniscus of similar characteristics to that of the right knee was observed, with no other findings. In both knees the same medial discoid meniscus presented with intrasubstance deterioration, was complete, and the morphology was block-shaped not tapered. A block-shaped morphology of the discoid meniscus makes it more vulnerable to deterioration and rupture, according to Ayala et al.16
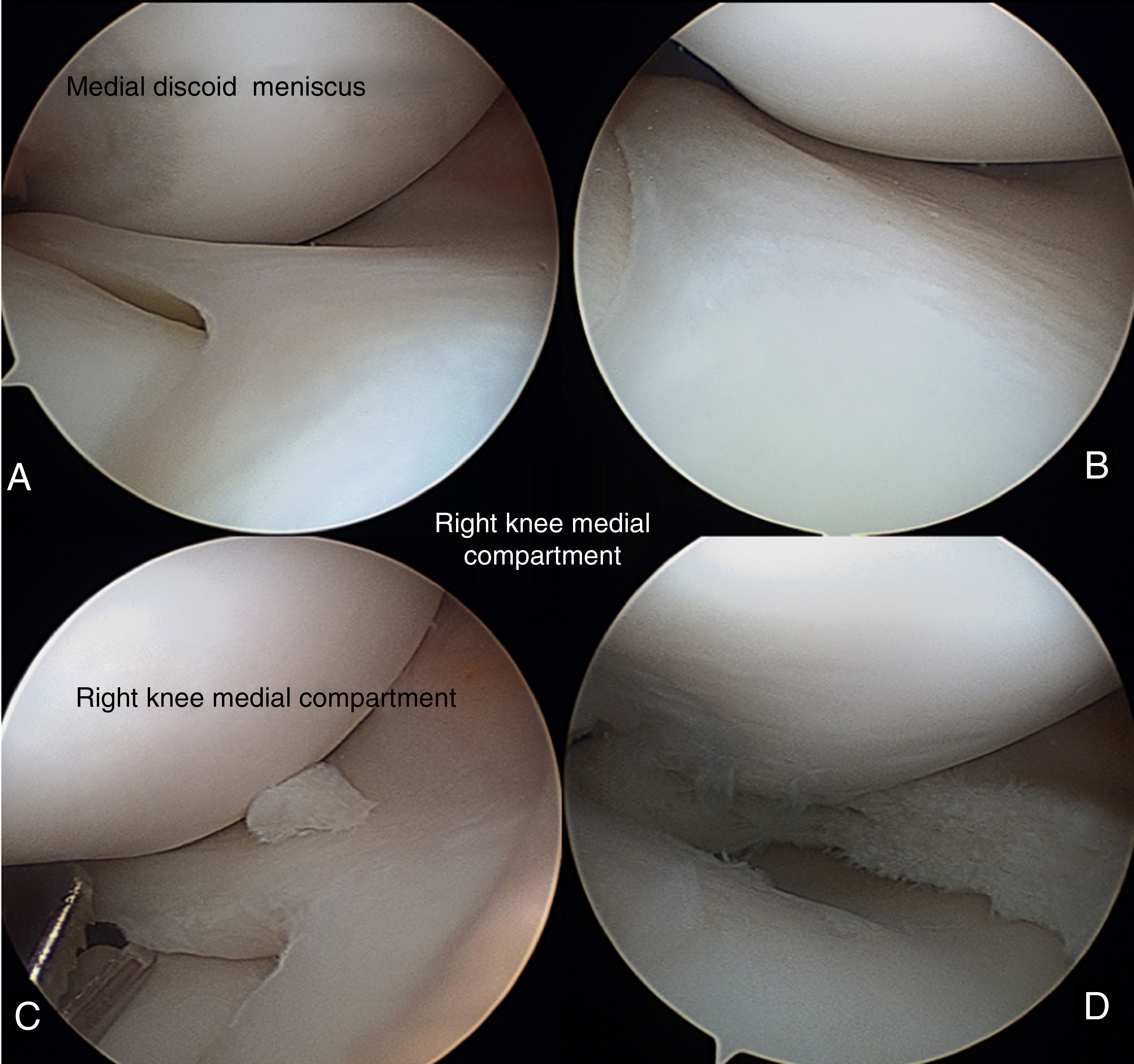
The patient was recommended physiotherapy and to limit his sporting activities, but the pain persisted and he went for a check-up after 11 months with further symptoms in the right knee. Due to non-improvement after one year of modifying his sports activity and treatment of symptoms, it was decided to perform arthroscopy of the right knee, where the following was found: synovial tear, cartilage without changes, complete medial discoid meniscus according the Watanabe9 classification, no rupture, and occupation of the whole medial joint space. Medial meniscus remodelling was performed until a normal meniscus shape was achieved, approximately 1cm from capsular insertion up to the new free edge (Fig. 2).
Evolution was favourable with no postoperative complications. Six weeks after the operation, the patient had moderate swelling, flexion of 120°, extension of 0° and slight hypotrophy of quadriceps. The same surgical procedure was performed in the left knee 3 months later, with no complications, and with favourable evolution.
ResultsIn the last check-up, 13 months after the arthroscopy of the right knee and 10 months after the arthroscopy of the left knee, evolution was favourable, the patient was able to do physical activity and lead a normal life. Flexion and extension of both knees was complete, with no joint tear and on the Tegner Lysholm Knee Score scale the score rose from 58/100 = 58-0% preoperatively to 94/100 = 94.0% 13 months postoperative. The postoperative magnetic resonance of both knees showed a residual medial meniscus with no signs of rupture.
DiscussionWe believe it was pertinent to present this case of complete bilateral medial discoid meniscus with intrasubstance deterioration because it is a highly rare cause of knee pain and sports limitation in the general public, with very few cases having been described in the literature, and that evolved in a satisfactory manner after medial meniscus remodelling in both knees.
According to Last, the menisci follow the tibial saucers in flexion and extension but the femur during rotations and they move over the tibia. The medial meniscus, because it is more fixed in its tibial and capsular insertions, is subject to greater tensions in rotation movements and is more likely to injure, unlike the lateral meniscus, which is more mobile. The medial meniscus of discoid morphology, due to its abnormal shape and thickness, is even more susceptible to injury during rotational movements.
Papadopoulos et al. proposed that discoid injury is a structural rather than a morphological variant. In their histological study they observed a disorganization of circumferential collagen fibres in the discoid meniscus structure. These histological changes associated with poor vascularisation and on occasions impaired peripheral capsular insertion predispose the discoid meniscus be more easily injured.3
The symptoms of a rupture of a medial discoid meniscus are normally similar to those caused in a rupture of a normal meniscus.4 In the case we present, the patient complained of pain in the medical joint line which increased, thereby limiting sports activity.
Medial discoid meniscus may be asymptomatic, and bilateral magnetic resonance should therefore be performed to rule out the presence of medial discoid meniscus and so that the patient can take the necessary precautions to avoid presenting with a contralateral knee injury. Plain X-rays of the knee may be useful, as they may show an enlargement of the medial joint line or hollowing out of the medial tibial saucer. In magnetic resonance, if signs of meniscal winding are found in 3 sagittal slices, the presence of discoid meniscus is suggested. In the coronal plane, when the proportion of the minimum meniscal width to the maximum tibial width is greater than 20% a diagnosis of discoid meniscus may be established. However, arthroscopy continues to be the gold standard for discoid meniscus diagnosis.4
In the majority of cases horizontal injuries present,3,8 with a greater incidence of meniscal injuries with type I or complete discoid meniscus and those with a greater height or thickness,3 which correspond to the block-shaped menisci, according to Ayala et al.16
For treatment, several authors recommend partial menisectomies in patients with complete discoid meniscus due to the high risk of developing injuries, although ideally surgery should be indicated in patients with sufficient mechanical symptoms, with or without meniscal injury, as they validate intervention. Patients with complete discoid meniscus may function satisfactorily without the need for surgery. However, partial menisectomy may be highly favourable in the short term, but follow-up studies of 11 years have been reported, of which 37% required further surgery and 42% presented with basic or poor functional results.3 Treating asymptomatic patients in this way is therefore a risk that future procedures will increase and the function of the affected knee will diminish.
There are morphological differences between the medial and the lateral meniscus which lead to different surgical treatment, because it is difficult to remove the posterior horn due to the limited space in the compartment and the obstruction caused by the anterior cruciate ligament and the intercondyloid eminence of the tibia. Wang et al.15 and Kim and Seo4 developed a technique for facilitating partial meniscectomy and complete resection of the discoid meniscus through 3 arthroscopic portals, thus leading to improved functional results and reducing the risk of presenting with postoperative loose bodies.17
To conclude, the bilateral medial discoid meniscus is a very rare entity, and is therefore difficult to determine. Reported incidence is from .12% to .3%; in bilateral cases an incidence of .012% has been reported, with symptoms being present in 62%-65% of cases.15 The incidence may be higher due to the number of undiagnosed asymptomatic cases. Bilateral presentation has been demonstrated in a high percentage of cases, and magnetic resonance must therefore be used to rule out the presence in the contralateral knee.
There is no consensus at present regarding the ideal management of this anatomical variant, particularly in asymptomatic patients who practise sports who have a higher susceptibility to present with injuries. It is therefore of vital importance to identify the injury to be able to advise the patient regarding the ideal sports activity in their individual case.
Partial meniscectomy or meniscus remodelling in symptomatic patients continues to be the treatment most used and with the best short-term outcomes.
Level of evidenceLevel of evidence IV.
Conflict of interestThe authors have no conflict of interests to declare.
Please cite this article as: Chico-Carpizo F, Arauz de Robles S, Alonso-Hernández J. Menisco discoide medial bilateral sintomático tratado con remodelación meniscal artroscópica: caso clínico. Rev Esp Cir Ortop Traumatol. 2020. https://doi.org/10.1016/j.recot.2020.02.005