Actually there is a controversy about the treatment of hip fractures on older patients with high risk of dislocation. Our study is focus on report clinico functional and radiographic results in this population treated with total hip replacement using a dual mobility system after a minimum follow up of 2 years.
Material and methodsIn the period from January 2015 to January 2016 patients assisted at the Emergency Unit at the participant hospital were recluted for participation. A total of 137 patients were assisted and 41 fulfilled the inclusion criteria and accepted to participate. All patients received a total hip replacement with a dual mobility system (cemented or uncemented). The patients were evaluated with the Mini-Mental State Examination, walking distance test, preop and postop at 3 and 6 weeks, 3 months, 6 months, one year and subsequent years. Radiographic evaluation was scheduled with clinico-functional review.
ResultsForty-one patients included, follow up average 2.4 years (range 2–3.2 years). Mean age 85.2 (range 80–96 years). Four patients died during follow up due to causes not related to the total hip replacement and the implant was functioning. One case have an infection and was revised in one stage procedure. One case have an infection at 8 months follow-up and was revised in one stage procedure. There were no dislocations.
ConclusionThe use of dual mobility system in this high dislocation risk population has shown good clinical and functional results, and support the sistematic indication in our services.
En la actualidad continúa la controversia respecto al tratamiento quirúrgico más adecuado de la fractura de cuello femoral desplazada en pacientes añosos o con alto riesgo de luxación. En nuestro estudio nos enfocamos en reportar resultados clínicos, funcionales y radiográficos de este tipo de pacientes tratados con artroplastia total de cadera usando sistema doble movilidad con un seguimiento mínimo de 2 años.
Materiales y métodosEn el periodo de enero de 2015 a enero de 2016 los pacientes con fractura del cuello femoral desplazada asistidos en las centrales de emergencia de los hospitales que participaron en el estudio fueron seleccionados. De 137 pacientes, 41 cumplían con uno o másde los criterios de inclusión y aceptaron la indicación terapéutica recomendada. Los pacientes fueron sometidos a artroplastia total de cadera utilizando prótesis con sistema de doble movilidad (cementada o no cementada). Todos los pacientes fueron evaluados con el Mini-Mental State Examination y la distancia de caminata en el preoperatorio, a las 3 y 6 semanas, a los 3 y 6 meses, al año y en años subsecuentes. Las evaluaciones radiográficas fueron programadas a tiempos similares.
ResultadosSe evaluaron 41 pacientes, con un seguimiento promedio de 2,4 años (rango 2 a 3,2 años). La media de edad fue de 85,2 (rango 80 a 96 años). Cuatro pacientes fallecieron en el periodo de seguimiento por causas no asociadas a la cirugía, con el implante funcionando. Hubo un solo caso de infección a los 8 meses de la cirugía, tratado con una revisión en un tiempo. No se reportaron casos de luxación en esta serie.
ConclusiónLa utilización de sistema doble movilidad para tratamiento de fractura fracturas del cuello femoral desplazadas en pacientes con alto riesgo de luxación y añosos ha demostrado buenos resultados clínicos y radiológicos que fundamentan la indicación sistemática de uso en nuestros servicios.
Total hip arthroplasty (THA) instability remains one of the most feared complications and a frequent cause of revision surgery, both in the United States (22%) and in the Australian Registry of Arthroplasties; it is even more common than infection.1,2
For patients with displaced femoral neck fractures (FNF), the reported rates are 1.4%–2.8% within the first postoperative year, even after implementing different strategies such as larger heads, reinsertion of the short rotator plane and capsule or changing to the direct anterior approach.3–5
With the increase in life expectancy worldwide, it is expected that more patients will suffer a hip fracture and may present risk of dislocation (RD) after THA.
There are multiple factors that contribute to increased RD, such as the experience of the surgeon, the number of operations performed by the surgeon, the type of approach used and the type of implant placed.6 Risk of dislocation mainly inherent to the patient include age over 75 years, cognitive deficit, neurological diseases, alcohol abuse, and a body mass index greater than 30.3,7,8
The concept of THA with a dual-mobility system (DM) was introduced in Europe more than 3 decades ago by Dr Bousquet in France and has shown excellent long-term results.4 In our setting and in the United States, it has recently rapidly gained in followers with the use of 2 joint surfaces. This implant system comprises 2 joint surfaces, one provided by the acetabular cup, with a large polyethylene insert, the other composed of polyethylene and the head is fixed by a capture mechanism, which allows both surfaces to move freely, thus improving the stability of the implant by increasing the jump distance.8–10
In most of the current reports the system is used to reduce dislocation rates in revision surgeries.9
In our study we focussed on patients who, due to their conditions had RD, with a minimum of 2 years’ clinical, functional and radiographic follow-up.8,11,12
Material and methodsA prospective, non-randomised study. After obtaining the approval of the Research and Ethics Committee of the respective hospitals, the use of a DM system in patients with one or more risk factors was systematised. All the patients included, or their guardians, were asked to sign the corresponding informed consent.
In the period from January 2015 to January 2016, patients with FNF treated at the emergency centres of the Italiano-San Justo, Centro Médico Fitz Roy and CEMIC hospitals were invited to participate in the study if they met the inclusion criteria.
Inclusion criteria: FNF (Garden 3 or 4), patients over 80 years of age, Parkinson’s disease, Alzheimer’s disease, neurological deficit, dementia and abductor system deficiency.13
Exclusion criteria: previous surgery on a fractured hip, metastatic oncological disease.
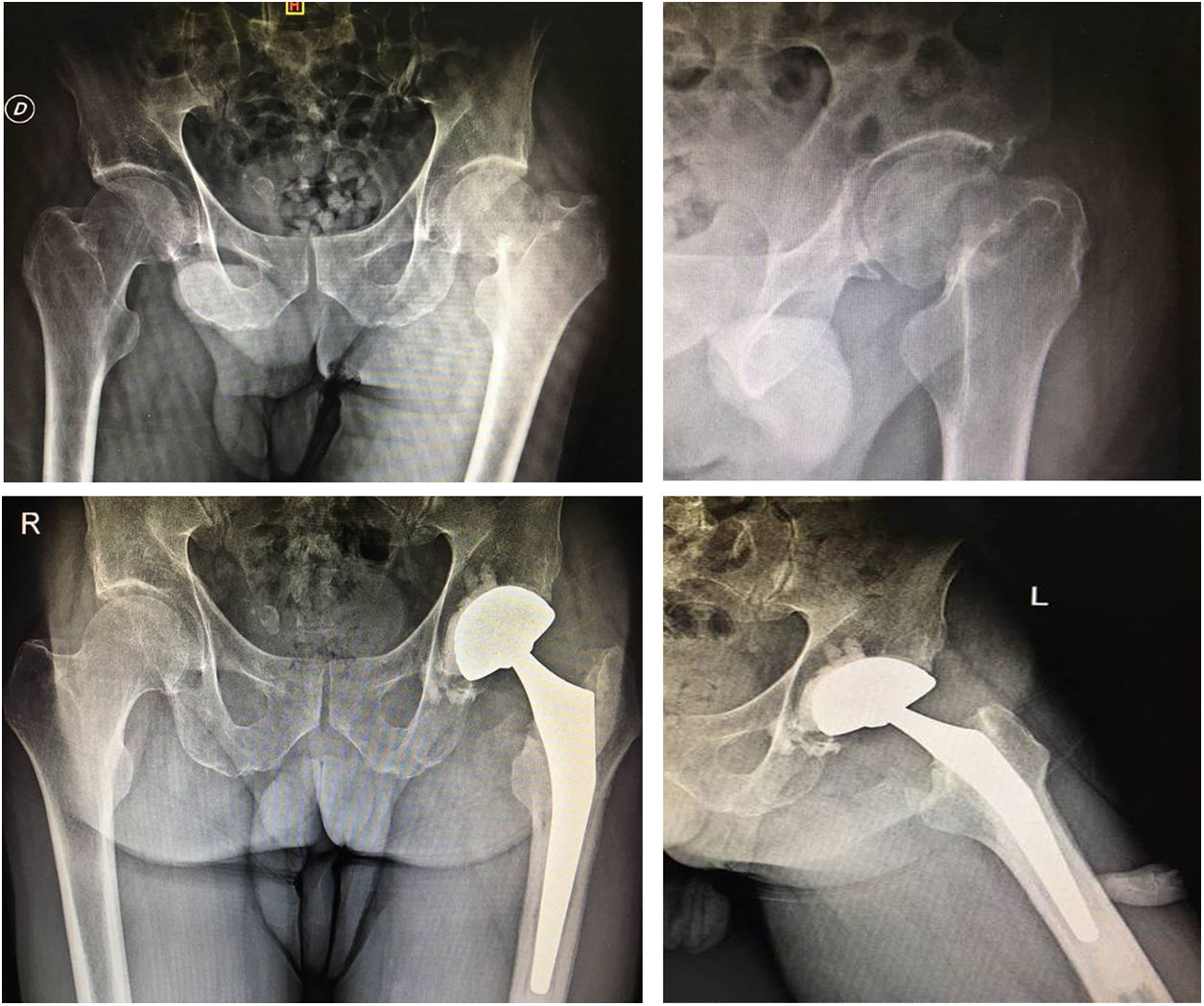
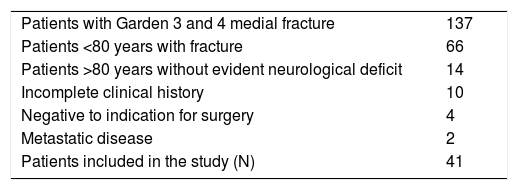
A total of 137 patients had suffered FNF, of which 45 met one or more of the inclusion criteria; in 4 cases the relatives did not accept the recommended therapeutic indication (Table 1).
All the procedures were performed by surgeons specialising in arthroplasty, using the posterolateral approach (routine approach in the department for all hip arthroplasties), with pyramidalis and posterior muscle retention, and capsular insertion according to the technique described by Pellicci.
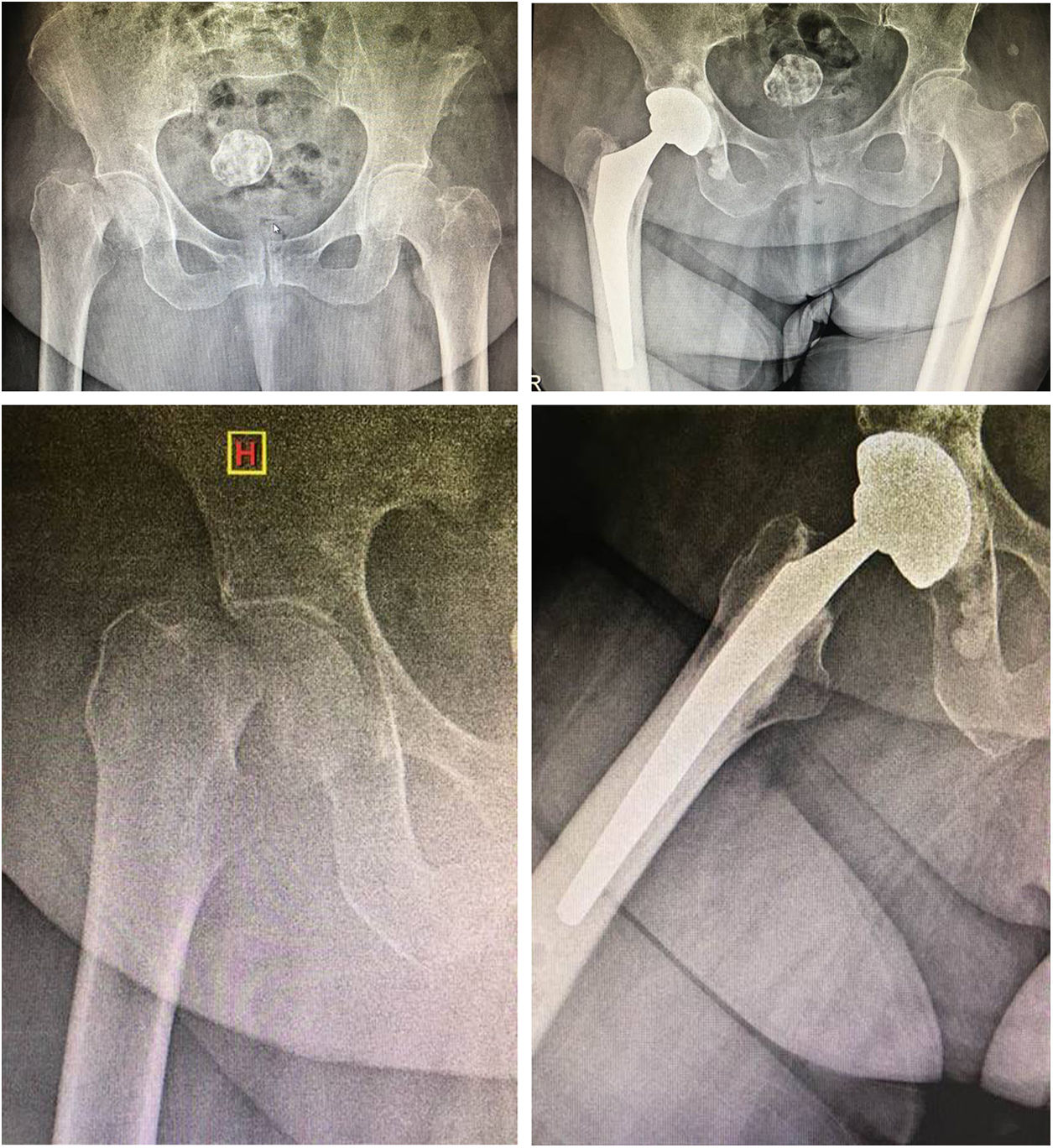
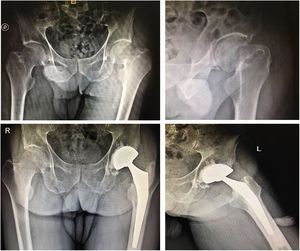
The acetabulum was prepared with gradual reaming with placement of an acetabular insert of 2 mm, smaller in the case of the cemented version and line-to-line in the cementless tripod version. Orientation was sought within the Lewinnek Safe Zone (inclination 30° to 50°; anteversion 5° to 15°)14 (Fig. 1).
The femoral canal was reamed due to impaction, a distal plastic plug was placed in the canal and cement gun retrograde cementing and antibiotic loading (vancomycin) was performed as routine.
A DM Hip’n Go prosthesis was used, which includes a cemented or cementless tripod acetabular cup version, and cemented mirror polished stem (FH Orthopaedic, Quimper, France).
The cognitive status of the patients was assessed with the Mini-Mental State Examination by Folstein et al.15 Data were collected on the usual daily walking ability of the patient and their relatives.
Radiographic evaluation of the acetabular cup included angle of inclination and anteversion with the Auckland method and the Lewinnek Safe Zone, and the femoral stem cementation was evaluated using the Barrack system.14,16
Complications during surgery and hospitalisation were recorded.
Follow-up was at 3 and 6 weeks, 3 and 6 months, at one year and annually thereafter.
ResultsThe study evaluated 41 patients and the average follow-up was 2.4 years (range 2–3.2 years). The average age was 85.2 years (range 80–96 years). The ratio of women to men was 2:3.
The initial reported walking distance ranged from .5 to 3.7 km (average 1.2 km).
The pre-surgical Mini-Mental State Examination had a range of 21–28 (mean 23.5) on a 30-point scale.
The average length of surgery was 72 min (range 50−93 min).
Anaesthesia was spinal in 38 cases and general in 3 cases.
Cemented acetabular inserts were placed in 35 patients, and cementless tripod inserts in 6 cases.
Intraoperative complications detected: oxygen desaturation during cementation, a calcareous fracture and a greater trochanter fracture (both treated with cerclage wires and without changes to the rehabilitation protocol); there were no complications at the time of the acetabular component placement.
Transfusion was required in 27 cases (65%), with an average of 2 units (range 1–4 units).
No patient died during the surgical procedure or during hospitalisation.
Postoperative radiographic evaluation with acetabular cup in a range of 38°–51° (average 43°) in 37 (97%) patients. Anteversion was found in a range of 0°–15°; in 40 patients (97.6%) no retroverted acetabular inserts were found. Non-progressive radiolucent lines without clinical manifestation were found in 5 cases (12%) of the series (2 cementless and 3 cemented) during follow-up controls. Evaluation of femoral cementation according to the Barrack system was A in 35 cases (85.3%) and B in 6; in 4 cases separation was identified in the shoulder of the prosthesis, due to radiolucency at the cement-bone interface less than 2 mm, with no clinical manifestation.
In the postoperative assessment, an average discrepancy of 5 mm was detected, with a range of −2 to 15 mm.
No episodes of dislocation were found during the follow-up period; one-stage revision of an implant was required due to infection at 8 months postoperatively, where the implant was replaced in one stage.
Four patients died in the follow-up period from causes not associated with the THA, with the implant working.
At the 2-year follow-up, 47% of the patients assessed maintained their level of ambulation and 23% required a cane to walk.
The reported walking distance decreased to an average of .8 km, with a range of .2–2 km, and the Mini-Mental State Examination showed an average of 20.9 points, with a range of 16–25 points.
DiscussionThe concept of DM was introduced in 1974 by Bousquet (surgeon) and Rambert (engineer), who combined the principle of Charnley’s low friction arthroplasty with the use of large McKee–Farrar heads.
Despite the changes in surgical technique, such as joint capsule repair, the use of large heads and the anterior approach, the incidence of dislocation in high-volume surgery centres has dropped to 1%; however, there is a group of high-risk patients, these are cases of hip FNF that have a 5% risk according to multiple reports.
Patients over 75 years of age worldwide present 1.6 million fractures per year, and this number will increase in the coming decades.17
As a consequence of increased life expectancy, one third of patients over 85 years of age display some form of cognitive impairment. Patients with dementia show a 2.7 times higher risk of hip fracture than those of a similar age in control studies.18
In all the patients we used the posterolateral approach, which is preferred by the surgeons, who consider it faster, more reproducible, with less comorbidity and better exposure of the acetabulum, bearing in mind that these are patients with fragile bones. Ritter et al. compare a number of patients operated by this approach versus direct lateral and expose a higher proportion of clinically demonstrable Trendelenburg sign in the Hardinge approach.19 Pellicci et al. demonstrated that capsule repair, added to heads of 32 mm, reduces the dislocation rate to less than .8%, equalling the direct lateral and anterior approach.20
Parkinson’s disease has a prevalence of 1% in patients over 60, with an exponential increase per decade, causing progressive deterioration with tremor, rigidity and akinesia.21 Bloem et al. concluded that falls are disabling and common in early Parkinson’s disease and dementia, and predictive of long-term disability.22 In the study, 4 patients died (9%), which is similar to the data found in other morbidity and mortality studies at 1-year follow-up post hip fracture, and given the progressive deterioration of the patients, as well as the increase in concomitant diseases at 5 years of follow-up, a mortality rate of 38% is to be expected.23,24
Thus, in a US national registry-based study by Jämsen et al. dislocation was the main cause in patients with Alzheimer's disease.25 In order to test the theoretical advantage of avoiding dislocation, patients treated with DM versus hemiarthroplasty (HA) in risk patients were compared with favourable results without statistical significance.26
It has been widely demonstrated that the use of bipolar components for HA dramatically decreases the rates of prosthetic dislocations by allowing the use of large femoral head sizes.27,28 However, Cho et al.29 compared the use of these prosthetic models with THA in very elderly patients with functional independence and the results were very favourable for THA, where functional and pain scores decreased in the medium and long term with the use of bipolar hemiarthroplasty. In our study group, we chose THA for patients with high functional demand, but combined with a DM cup due to RD, obtaining the result of 0% dislocations at an average 2.4 years of follow-up (Fig. 2).
Like those evaluated in our series, Guyen et al. do not report dislocations in patients at high risk of dislocation with the use of a tripolar component.8
Kaiser et al., in a retrospective study in which a DM system (Medacta) was used in patients with RD over a minimum follow-up period of 2 years, found no dislocations in 1046 cases, a similar result to our series, with a hemispheric cup similar to the design we used.30
Similar results are reported by Luthra et al. in a group of 30 patients identified as high risk, in a follow-up of 5 years on average using DM Advance.11
There are reports of intraoperative dislocation associated with attempts to reduce the polyethylene component embedded in soft tissue and with traction for reduction by a bottle- opener mechanism that uncouples the head.31,32
In our series, no wear or dislocation was observed, historically associated with the use of large heads and multiple joint surfaces with early failure with the first DM generation, which should not be seen with the current generation, which has a highly cross-linked polyethylene component and a small neck stem.33
In terms of functional results, we followed the line of care already reported with the help of orthogeriatrics and specific rehabilitation. It is known that less than half of the patients over 80 years of age recover their ability to walk after a medial hip fracture, and 40% maintain their activities of daily living.23
It is our belief that in this type of patient, given the expected survival rate, the evaluation of surgical results should be based on function and quality of life obtained rather than on implant survival.34
The study lacks randomisation or comparison with other types of systems (hemiarthroplasty, THA), although it is a specific sub-group of high-risk patients, with multiple confounders. The strength of the study is that it was able to identify the patients, their functional and cognitive evaluation, using a standardised surgical technique performed by prosthetic surgery specialists and a single brand implant in order to avoid deviations. (Figs. 1 and 2)
ConclusionThe use of the DM system in elderly patients with high RD with a minimum follow-up of 2 years has demonstrated good clinical (even in patients with progressive cognitive and functional impairment) and radiological results that support its systematic indication for use in our departments.
Studies with larger numbers of patients and longer-term follow-up are required to assess component wear. However, it could be said that with the current materials, the implant should survive the patient.
Level of evidenceLevel of evidence IV.
Conflict of interestsThe authors have no conflict of interests to declare.
Please cite this article as: Godoy-Monzon D, Garcia-Mansilla A, Buljubasich M, Cid-Casteulani A, Valentini R. Sistema de doble movilidad. La solución francesa en pacientes añosos con fractura intracapsular de cadera y alto riesgo de luxación. Rev Esp Cir Ortop Traumatol. 2020. https://doi.org/10.1016/j.recot.2020.03.003