To evaluate the clinical results and analyse the complications of total reverse shoulder replacement performed in our centre over an 8 year period.
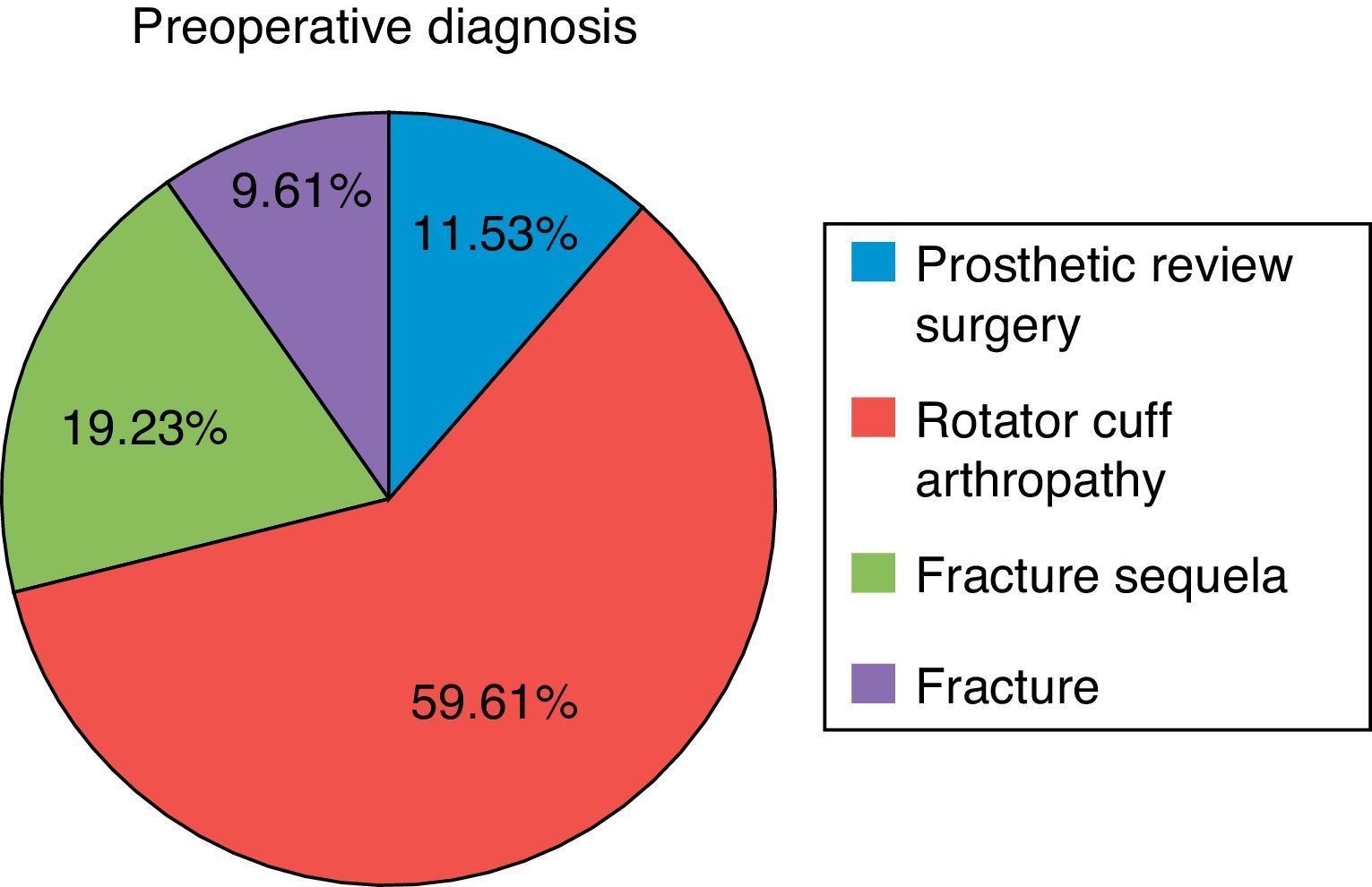
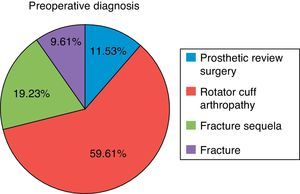
Material and methodA retrospective study was conducted on 50 patients (52 shoulders), with a mean age of 70.15 years (range 51–84 years) between December 2004 and December 2012, who received a total reverse shoulder replacement, all performed by the same surgeon. The results have been evaluated according to clinical data, radiography study, a satisfaction scale, and the Constant scale, with a minimum follow-up of 16 months. Five of the cases (9.62%) had been intervened due to fractures of the proximal end of the humerus, 6 cases (11.53%) as surgical consequence of a prosthesis revision, 10 cases (19.23%) due to fracture sequelae, and 30 cases (59.62%) were patients with arthropathy due to a massive fracture of the rotator cuff.
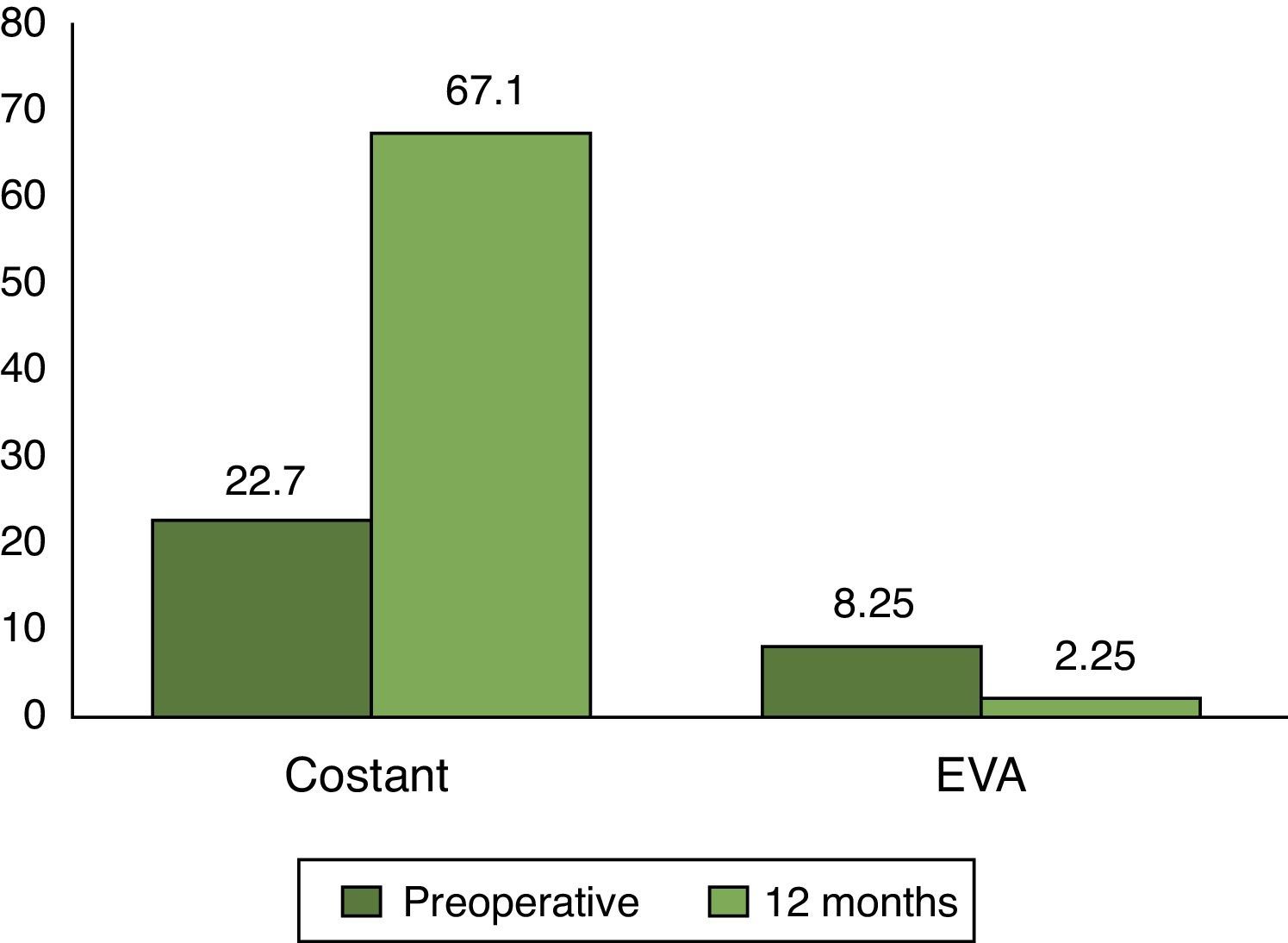
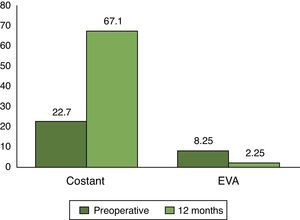
ResultsAfter a mean follow up of 35.78 months (range, 16–82), satisfactory clinical results were obtained in 80% of cases, with a mean preoperative Constant of 27.7 points, and reaching 67.1 points 12 months after the operation. On the visual analogue scale, 8.25 points were obtained before the surgery, which decreased to 2.25 points 12 months later. The complications rate was 15.38%, which were due to an intra-operative fracture (1.92%), deep infection (3.84%), instability (3.84%), and early mechanical loosening (3.84%). Scapular notching was observed in the radiographic study in 9 (17.3%) cases.
Discussion and conclusionsAfter the results obtained, it could be said that total reverse shoulder replacement achieved encouraging results in the short term for the treatment of glenohumeral arthrosis and massive tears of the rotary cuff. On analysing our series, it can be seen that the complications rate is much higher when it is used to treat fracture sequelae in which there is a loss of proximal humerus bone stock.
Evaluar los resultados clínicos y analizar las complicaciones de las prótesis totales invertidas de hombro realizadas en nuestro centro en un periodo de 8 años.
Material y métodoSe ha realizado un estudio retrospectivo sobre 50 pacientes (52 hombros), con edad promedio de 70,15 años en un rango de 51 a 84 años entre diciembre del 2004 y diciembre del 2012, a los que se les ha implantado una prótesis total invertida de hombro, todos intervenidos por el mismo cirujano. Se han evaluado los resultados según la clínica, el estudio radiográfico, la encuesta de satisfacción y la escala de Constant con un seguimiento mínimo de 16 meses. Cinco de los casos (9,62%) se han intervenido por fracturas de la extremidad proximal de húmero, 6 casos (11,53%) como consecuencia de cirugías de revisión protésica, 10 casos (19,23%) por secuelas de fracturas y 31 casos (59,62%) corresponden a pacientes con artropatía por rotura masiva del manguito rotador.
ResultadosTras un seguimiento medio de 35,78 meses (rango 16–82), en los que se han obtenido resultados clínicos satisfactorios en más del 80% de los casos con un Constant preoperatorio promedio de 22,7 puntos y alcanzando los 67,1 puntos a los 12 meses de la intervención. En la escala visual analógica se han obtenido 8,25 puntos en el preoperatorio hasta disminuir a los 2,25 puntos transcurridos 12 meses. La tasa de complicaciones es del 15,38%. Estas corresponden a: fractura intraoperatoria (1,92%), fractura de acromion (1,92%), infección profunda (3,84%), inestabilidad (3,84%) y aflojamiento mecánico precoz (3,84%). En el análisis del estudio radiográfico, se observa notching escapular en 9 casos (17,3%).
Discusión y conclusionesTras los resultados obtenidos, podemos decir que la prótesis total invertida de hombro consigue resultados alentadores a corto plazo para el tratamiento de la artrosis glenohumeral y los desgarros masivos del manguito rotador. Al analizar nuestras series, comprobamos cómo la tasa de complicaciones es mucho más elevada cuando se usa para tratar secuelas de fracturas en las que tenemos una pérdida del stock óseo del húmero proximal.
Shoulders with a deficient rotator cuff present severe biomechanical alterations, causing components of arthroplasties with a conventional design to suffer early complications. These complications are mainly due to a continuous change in the centre of rotation of the joint and eccentric loads on the glenoid component, leading to a loosening thereof.1,2 Due to these two reasons, hemiarthroplasty and bipolar prosthesis techniques have several limitations, both in terms of function and pain relief. The total reverse shoulder replacement (TRSR) technique, in which the humerus is transformed into a concavity and the glenoid into a sphere, solves both problems and provides a stable fulcrum for the glenohumeral joint.3,4
TRSR was approved by the FDA in 2004 and has since proven to be a very effective prosthesis for the treatment of rotator cuff tear arthropathy and other conditions requiring a shoulder arthroplasty due to rotator cuff deficiency.5 However, in other published series, the rate of revision of TRSR was nearly 10%, with instability and infection being the most common causes.6,7 Other studies have shown that aseptic loosening may contribute up to 7% of total complications.7 Since the indications are increasing and the follow-up period is becoming longer, the incidence of aseptic loosening is also likely to increase. Moreover, Guery et al.8 have proven that pain increases in long-term follow-up of temporary replacements (5–10 years). Therefore, in the future, surgeons will be facing difficult decisions when reviewing reverse prostheses, and there is no established optimal management for TRSR complications.
The purpose of our study is to evaluate the results obtained after placement of a TRSR in our centre, in order to improve the quality of healthcare for this specific group of patients.
Material and methodWe conducted a retrospective, descriptive study, from December 2004 until December 2012. A total of 50 patients with a total 52 TRSR (two patients intervened in both shoulders) were reviewed during that period, with the first 30 cases being Delta Xtend™ (DePuy-Johnson & Johnson, Warsaw, IN, USA) and the remaining 22 Aequalis™ Reversed (Tornier, Grenoble, France) units.
The mean age of these patients was 70.15 (SD: 7.767) years, with a range from 51 to 84 years. Of these, 43 were female (84%). Regarding laterality, 34 patients were affected in the right shoulder (65.38%) and 18 in the left (34.61%).
The indications to implant a TRSR are limited, so it is important to take into account several factors allowing us to select a patient who is a true candidate for this process.9–11 The following clinical criteria have been followed to apply the technique: (1) a healthy deltoid with no apparent signs of denervation, (2) arthropathy due to massive rotator cuff tear in Hamada stage IV, (3) non-repairable massive rotator cuff tear, (4) presenting a functionally pseudoparalysed shoulder, (5) revision surgery for anatomical or reverse arthroplasties with non-functional rotator cuff, (6) fracture and fracture/dislocation in 4 fragments with osteoporotic and comminuted tuberosities, and an atrophied rotator cuff with fatty degeneration and (7) clinical situations in which we will foreseeably find a non-functional or potentially damaged rotator cuff, like in cases of glenohumeral arthrosis secondary to rheumatoid arthritis, for example. The age of patients, in this case older than 65 years, is only a relative clinical indication, since we also find young patients who meet some of the clinical criteria described previously. Contraindications for TRSR include: active infection, deltoid dysfunction (neurological or structural), presence of a glenoid bone stock deficit preventing implant placement and young patients (except for rescue procedures).
Our preoperative diagnoses have been ordered from higher to lower frequency: 31 cases (59.62%) of arthropathy due to massive rotator cuff tear, 10 cases (19.23%) of sequelae from fractures, 6 cases (11.53%) of prosthetic revision surgery and 5 cases (9.62%) corresponding to fractures of the proximal humeral joint (Fig. 1).
We analysed the results obtained, according to the preoperative diagnosis, in terms of functionality with the Constant scale12 and pain with a visual analogue scale,13 both assessed preoperatively (in all patients except for fracture cases) and at 12 months from the intervention. We also analysed the radiographic results, any existing complications and asked patients whether they would choose to undergo the procedure again or not, in order to measure the level of satisfaction. This was question number 18 in the UCLA questionnaire14 and is used in research to measure the level of satisfaction regarding a medical procedure or intervention.
All patients underwent a simple radiographic study with at least 2 projections (anteroposterior and lateral) and, in cases of massive rotator cuff arthropathy, a magnetic arthroresonance (arthro-MRI) to confirm the clinical diagnosis prior to the intervention.
Monitoring was conducted through clinical and radiographic controls at 3 and 6 weeks, then every 3 months during the first year and then every 6 months during the second year, continuing with annual reviews thereafter. The measurement of severity of scapular notching was conducted through the Nerot–Sirveaux classification,15–17 which establishes 4 grades, with grade 1 representing a notch contained in the lower column of the neck of the scapula, whilst grade 4 describes the progression of the notch up to the lower surface of the body of the scapula and the central area of the glenoid. In addition, we assessed the presence or absence of radiolucency lines surrounding the stem, as well as cases with component malposition.
It is worth highlighting that all the patients included in the study were surgically intervened by the same orthopaedic surgeon, using a deltopectoral approach and always following the same surgical technique, according to the prosthesis models mentioned previously. There was an attempt to preserve the tuberosities in case of fracture, reanchoring them according to the technique described by Boileau,18 although the supraspinatus was resected and the subscapular, infraspinatus and teres minor muscles were reinserted. Regarding the repair of the subscapular, there was an attempt at reinsertion in all cases except those presenting arthropathy due to massive rotator cuff tear with involvement thereof. Regarding the indication for the use of non-cemented stems, it was reserved only for cases with a preoperative diagnosis of arthropathy due to massive rotator cuff tear where the rotational stability of the stem was verified intraoperatively. Regardless of the preoperative diagnosis, all patients underwent placement of the stem in a neutral position, with 0° retroversion. The BIO RSA system has been used in 28 patients since 2009 in an attempt to reduce medialisation of the centre of rotation and thus the onset of notching.
All cases followed a postoperative rehabilitation treatment. Patients were immobilised with a sling in internal rotation which was progressively removed around the third week. All the rehabilitation protocols were started with passive movements without restrictions between the first and third postoperative weeks. Patients began active mobility between the second and fourth weeks after surgery and muscle strengthening between weeks 3 and 12.
The statistical analysis was carried out using the software package SPSS v.19.0. A descriptive statistical analysis of the study variables was conducted using absolute and relative frequencies in the case of qualitative variables, whereas quantitative variables were described by mean and standard deviation or median and interquartile range depending on whether they followed a normal distribution (following application of the Kolmogorov–Smirnov test) or not, respectively.
We compared the means and/or medians of quantitative variables (Constant and mobility scales) through an ANOVA for variables with a normal distribution or through a Kruskal–Wallis test for variables which did not follow a normal distribution. For qualitative variables we applied the χ2 test or the Fisher exact test in the case of low frequencies. The level of statistical significance was set at P<.05.
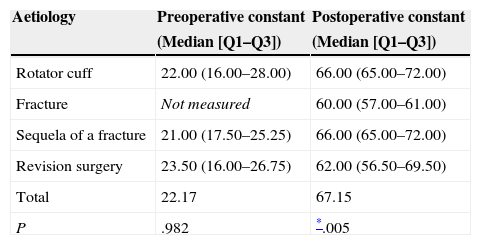
ResultsThe mean preoperative Constant score was 22.7 points, excluding the cases with a preoperative diagnosis of fracture, as the patients could not complete the questionnaire prior to the intervention. The total score at 12 months after the intervention was 67.1 points, including in this mean value the 5 patients intervened due to fractures. After the analysis, a statistically significant difference was observed between the Constant postoperative score of cases which corresponded to the aetiology of massive rotator cuff arthropathy with 66.0 points (range: 65.0–72.0) and that of sequelae of fracture with 60.0 points (range: 57.0–61.0) (Table 1). No statistically significant differences were found when comparing the rest of aetiologies.
Score in the Constant scale according to aetiology.
| Aetiology | Preoperative constant | Postoperative constant |
|---|---|---|
| (Median [Q1–Q3]) | (Median [Q1–Q3]) | |
| Rotator cuff | 22.00 (16.00–28.00) | 66.00 (65.00–72.00) |
| Fracture | Not measured | 60.00 (57.00–61.00) |
| Sequela of a fracture | 21.00 (17.50–25.25) | 66.00 (65.00–72.00) |
| Revision surgery | 23.50 (16.00–26.75) | 62.00 (56.50–69.50) |
| Total | 22.17 | 67.15 |
| P | .982 | *.005 |
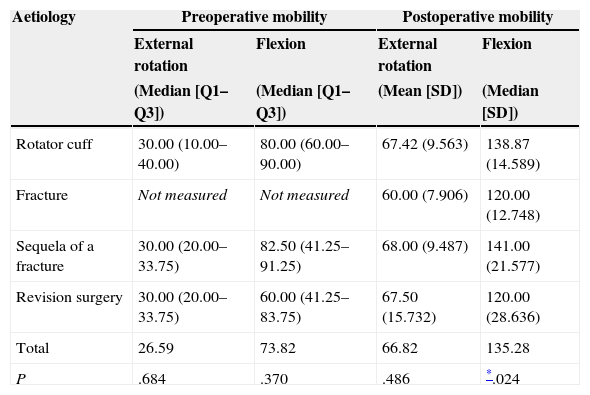
In the mobility study we took into account the preoperative active flexion and external rotation (except in cases of fracture), as well as the postoperative in all cases. The mobility results in terms of measured active flexion were statistically significant when comparing the preoperative results with those obtained 12 months after the intervention, with a mean value of 138° (SD: 14.58) in cases corresponding to prior aetiology of massive rotator cuff arthropathy and 141° (SD: 21.57) in cases with fracture sequelae (Table 2).
Mean mobility results obtained according to aetiology.
| Aetiology | Preoperative mobility | Postoperative mobility | ||
|---|---|---|---|---|
| External rotation | Flexion | External rotation | Flexion | |
| (Median [Q1–Q3]) | (Median [Q1–Q3]) | (Mean [SD]) | (Median [SD]) | |
| Rotator cuff | 30.00 (10.00–40.00) | 80.00 (60.00–90.00) | 67.42 (9.563) | 138.87 (14.589) |
| Fracture | Not measured | Not measured | 60.00 (7.906) | 120.00 (12.748) |
| Sequela of a fracture | 30.00 (20.00–33.75) | 82.50 (41.25–91.25) | 68.00 (9.487) | 141.00 (21.577) |
| Revision surgery | 30.00 (20.00–33.75) | 60.00 (41.25–83.75) | 67.50 (15.732) | 120.00 (28.636) |
| Total | 26.59 | 73.82 | 66.82 | 135.28 |
| P | .684 | .370 | .486 | *.024 |
Regarding the analogue visual scale, we recorded 8.25 points in the preoperative period and a reduction down to 2.25 points after 12 months, with no statistically significant differences being observed (Fig. 2). All the patients reported that they would undergo the procedure again, thus demonstrating a high level of satisfaction.
In the analysis of the radiographic study, we observed scapular notching in 9 cases (17.3%). One of these corresponded to a patient with grade 4 notching who required revision surgery and the rest to grade 1 and 2 notching with no clinical repercussions. We also found 1 case with radiolucency lines corresponding to 1 of the complications described below.
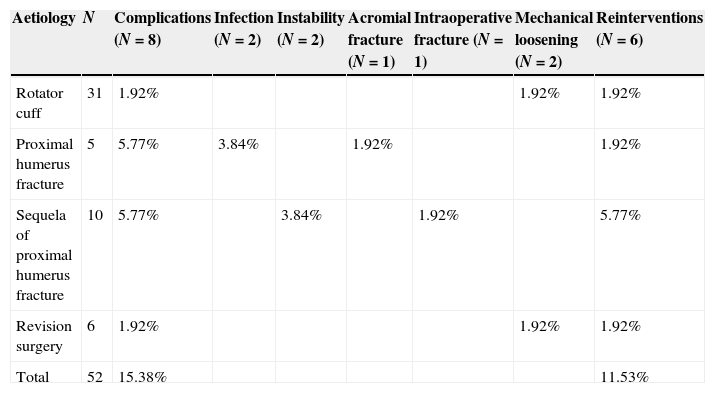
We registered a 15.38% rate of complications, corresponding to 8 cases described below (Table 3).
Summary of complications according to aetiology and reinterventions in patients treated with TRSR.
| Aetiology | N | Complications (N=8) | Infection (N=2) | Instability (N=2) | Acromial fracture (N=1) | Intraoperative fracture (N=1) | Mechanical loosening (N=2) | Reinterventions (N=6) |
|---|---|---|---|---|---|---|---|---|
| Rotator cuff | 31 | 1.92% | 1.92% | 1.92% | ||||
| Proximal humerus fracture | 5 | 5.77% | 3.84% | 1.92% | 1.92% | |||
| Sequela of proximal humerus fracture | 10 | 5.77% | 3.84% | 1.92% | 5.77% | |||
| Revision surgery | 6 | 1.92% | 1.92% | 1.92% | ||||
| Total | 52 | 15.38% | 11.53% |
There were 2 cases of deep infection (3.84%). The first was an 80-year old female patient who underwent implantation of a TRSR due to a fracture in 4 fragments. Subsequently, 15 months after the placement of the prosthesis, a fistula appeared in the anterior side of the arm, which was confirmed by a fistulography reporting contact with the anterior cortical of the humerus. There was no radiographic evidence of implant mobilisation. Staphylococcus aureus (S. aureus) was isolated in the cultures, with no significant clinical repercussions for the patient, so prosthetic revision was ruled out and we decided to excise the fistulous segment, along with a suppressive antibiotic treatment. After 82 months of follow-up since the TRSR implantation, the patient maintained good shoulder functionality with a fixed and stable prosthesis allowing her to carry out a normal life.
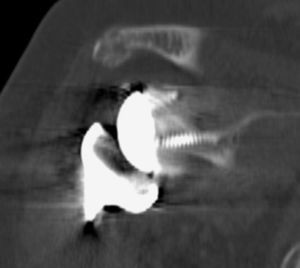
The other case of deep infection corresponded to a 70-year old female patient who also presented, as preoperative diagnosis, a fracture in 4 fragments of the proximal humerus. The surgical wound had a torpid evolution, and serial cultures and a computed tomography scan with contrast were all negative, with no evidence of collections. The evolution showed radiolucency lines around the stem in radiographs, so we decided to carry out prosthetic replacement in 2 stages, considering aseptic loosening of the TRSR. We took intraoperative samples and isolated S. aureus, which was effectively treated with antibiotics. After a follow-up period of 39 months, the patient achieved an external rotation of 60° and an active flexion of 85° obtaining a score of 49 points on the Constant scale 24 months after the intervention.
There was 1 case of intraoperative fracture (1.92%) of the glenoid which affected the primary stability of the metaglene, so we decided to reconvert into a hemiarthroplasty in the same surgical action. The previous aetiology was a sequela from a proximal humeral fracture treated with osteosynthesis in a 77-year old patient.
Two cases of instability (3.84%), both requiring open reduction and revision of the stem due to an orientation defect. Both cases presented sequelae from proximal humerus fractures.
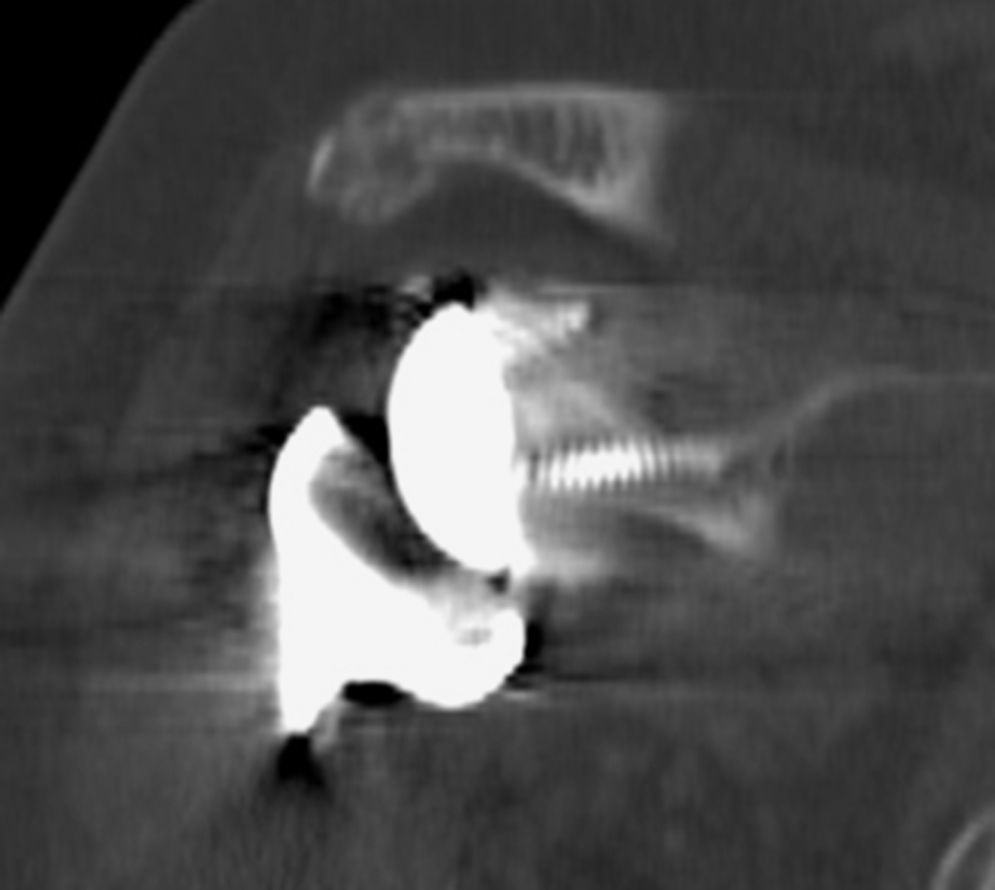
There was 1 case of acromial fracture in the late postoperative period which was treated conservatively (1.92%). The patient was an 81-year old female who presented inability for active elevation 2 months after TRSR implant due to a fracture in 4 fragments. A CT scan confirmed the diagnosis of non-displaced acromial fracture which, as commented, was treated conservatively, regaining shoulder functionality 6 weeks after rehabilitation (Fig. 3).
In addition, we also had 2 cases of early mechanical loosening of the metaglene (3.84%), 1 of them due to disassembly of the glenosphere and the metaglene which caused grade 4 notching and a loss of fixation of the former, which led to a surgical revision of the prosthesis. Intraoperatively, we observed polyethylene wear with the glenosphere and the metaglene loose and with a wrong orientation in the vertical plane. After verifying the stability of the stem, we added a structural, iliac crest autogenous graft, placing a new metaglene in the correct orientation and subsequently achieving a stable prosthetic reduction.
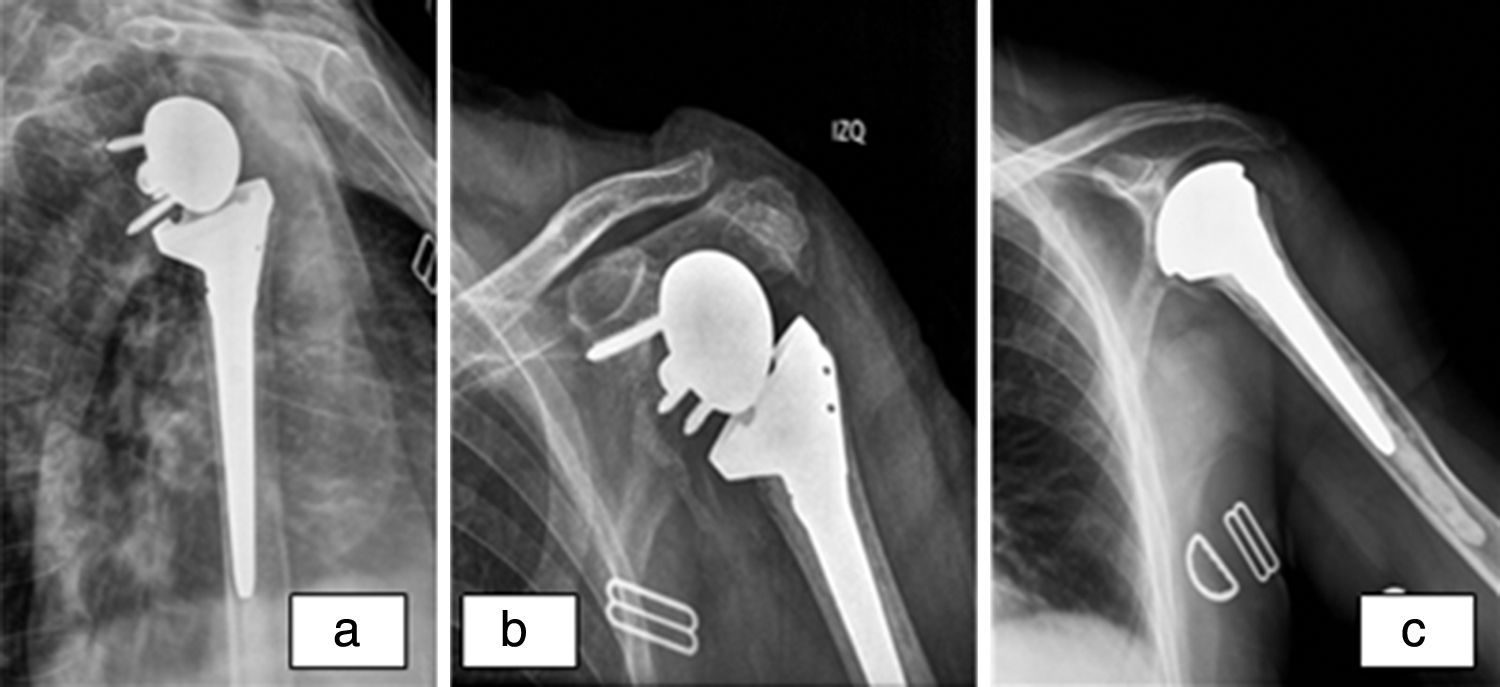
The second case was the only complication in a TRSR implanted due to a preoperative diagnosis of arthropathy due to massive rotator cuff tear. The patient was an 80-year old female in whom we observed loosening of the metaglene due to inferior impingement. We opted for surgical revision in which, after observing the osteolysis caused in the glenoid by 2 of the screws and the poor bone quality, we removed the TRSR and reconverted to hemiarthroplasty (Fig. 4). The patient currently presents a pseudoparalysed arm, albeit with no pain at rest.
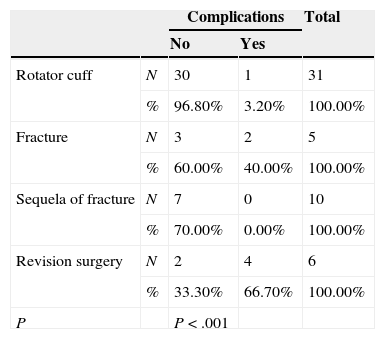
Patients in whom a TRSR was implanted for revision surgery presented a significantly (P<.005) higher incidence of complications compared to the primary use of prosthesis in the frame of a rotator cuff arthropathy (Table 4).
DiscussionTRSR has generated a deep change in the concept of arthroplasty in this joint.19,20 The changes in design,21–23 applied in the mid-80s, transformed the low performance of anatomical prostheses into great successes in shoulders in which the rotator cuff was ineffective and which were in a final phase of pseudoparalysis (Table 4).24–27
Several series have shown promising short and medium-term results with this system, including the one by Boileau et al.28,29
Despite the wide dissemination that this type of implants is reaching, it is not a simple procedure nor one free from complications.7,8,11,30,31
The rate of complications in our series (15.38%) was under the mean rate in the literature (24–44%).7,19 A clinical series of 60 TRSR published by Frankle et al.32 observed a total of 13 complications in 10 patients (17%), including 3 acromial fractures and 1 scapular, as well as 5 cases of loosening of the metaglene, including tear of a screw, with subsequent disassembly. A systematic review published by Zumstein et al.7 found 347 problems and 188 complications, representing an overall rate of complications of 24%. Of these, 24 cases were intraoperative problems, with the remaining 164 cases being postoperative problems, of which the most frequent was scapular notching. The incidence of this problem identified in our series was 9 cases (17.3%), whilst the incidences published in the literature varied between 0% and 96%.7,17,19,20 Some studies have demonstrated a correlation between the onset of scapular notching and poor clinical results, whilst others have not found such association.
The most frequent complication in the study conducted by Zumstein et al.7 was instability, which appeared in 37 cases (4.7%), followed by infection in 30 cases (4%). If we compare the incidences in our series with those in this study, we find that cases of instability (3.84%) were slightly less, whilst the number of cases of infections, both deep and superficial, were very similar. However, the reviewed literature contained a rate of infections between 1% and 15%, which was over 7% in revision cases.17,19,20,30,33
Regarding instability, it is difficult to analyse its causes due to the variability in the published studies. Some have reported that the deltopectoral approach seems to have a negative effect on the incidence of instability.34 However, incomplete release of the subscapular can predispose towards an inadequate orientation of both the humeral and glenoid components. Therefore, the subscapular seems to be vitally important and should be repaired and protected whenever possible, although its influence in implant stability continues to be a point of controversy.19,26
Another complication which appeared in our series was intraoperative fracture, with 1 case of glenoid fracture. Crosby et al.35 conducted a review of a series of 400 TRSR over a period of 4.5 years seeking scapular fractures and found 22 cases of such fractures. In general, intraoperative fractures of the humerus or glenoid are due to errors in the surgical technique, such as inadvertent drilling, excessive impaction or manipulation of the upper limb during glenoid exposure.21,31
TRSR is a very demanding technique, with a high rate of complications, many of them difficult to resolve. When analysing our series, we observed that the rate of complications was much higher when using this type of prosthesis to treat fracture sequelae in which there was a loss of bone stock of the proximal humerus, which in many cases caused prosthetic instability, and also after revision surgery. Complications were less frequent in cases where the implant was due to a diagnosis of arthropathy caused by massive rotator cuff tear. In addition, it appears that complications in these cases are easier to resolve.
In light of our results and supported on the literature, we consider that the reverse shoulder prosthesis achieves promising short-term results for the treatment of glenohumeral arthrosis and massive rotator cuff tears. The indications continue to evolve and the number of prostheses implanted throughout the world is rapidly increasing.
There should be strict indications for the use of reverse total shoulder prostheses, which should be reserved for patients aged over 60 years suffering shoulder arthropathy with clinical pseudoparalysis, who have sufficient bone stock to allow implantation of the glenoid component. We should be aware not only of the potential benefits, but also the complications and current concerns regarding the longevity of this type of prosthesis, in order to obtain optimal results with its implantation.
The objective of this article is to describe the clinical, radiographic and functional results, as well as the complications recorded after TRSR implantation in our centre over a period of 8 years. This was done through a retrospective, descriptive study, which was subject to the limitations of such kind of studies, in addition to the limitations entailed by the use of 2 prosthetic implants and the different preoperative diagnoses which lead to a possibly small sample size for each aetiology.
Ethical responsibilitiesProtection of human and animal subjectsThe authors declare that no experiments were performed on humans or animals for this investigation.
Confidentiality of dataThe authors declare that they have followed the protocols of their workplace on the publication of patient data.
Right to privacy and informed consentThe authors must have obtained the informed consent of the patients and /or subjects mentioned in the article. The author for correspondence must be in possession of this document.
Level of evidenceLevel of evidence IV.
Conflict of interestsThe authors have no conflict of interests to declare.
Please cite this article as: Cáceres-Sánchez L, Mesa-Mateo A, Barrionuevo-Sánchez FJ, García-Benítez B, Expósito-Triano S. Artroplastia total invertida de hombro. Evaluación de resultados clínicos y complicaciones tras una serie de 52 casos. Rev Esp Cir Ortop Traumatol. 2015;59:439–446.