Lunate traumatic fractures represent between 0.5% and 1% of carpal bone fractures. Transverse fracture through the body of the lunate (type V) are the least frequent and need surgical treatment if displaced, because it has a high risk of necrosis or pseudoarthrosis. The objective of this paper is to present our experience with arthroscopic treatment in patients with a delay in consolidation after a transverse fracture through the body of the lunate.
MethodsTwo clinical cases of delay in consolidation in transverse fracture through the body of the lunate are presented. Both cases have delay in consolidation
ResultsBoth fractures were misdiagnosed in initial simple radiographic exploration and were diagnosed with computerised tomography. Both patients were treated by debridement, bone grafting and osteosynthesis under arthroscopic control, obtaining a correct radiographic consolidation.
ConclusionArthroscopic treatment is a valid, effective and safe technique for the treatment of delay in consolidation of transverse fractures through the body of the lunate, and avoids complications and soft tissues injury of the open surgery techniques.
Las fracturas traumáticas del semilunar representan entre el 0,5% y el 1% de todas las fracturas del carpo. Las fracturas transversales del cuerpo del semilunar (tipo V) son las menos frecuentes y son quirúrgicas si están desplazadas, porque tiene alto riesgo de necrosis o pseudoartrosis. El objetivo de este trabajo es presentar nuestra experiencia con el tratamiento artroscópico en pacientes con un retraso en la consolidación tras una fractura transversal del cuerpo del semilunar.
Material y métodoPresentamos dos casos clínicos de retardos de consolidación tras fracturas transversales del cuerpo del semilunar.
ResultadosEn ambos casos no se diagnosticó la fractura con radiografía simple inicial y se diagnosticaron mediante tomografía computarizada. En ambos casos se produjo un retraso en la consolidación. Se trataron mediante cruentación, aporte de injerto y osteosíntesis bajo control artroscópico obteniendo una correcta consolidación radiográfica.
ConclusionesEl tratamiento artroscópico es una técnica válida, eficaz y segura para el tratamiento de los retardos de consolidación de las fracturas transversales del hueso semilunar, y evita las complicaciones y lesión de las partes blandas de las técnicas por cirugía abierta.
Fractures through the body of the lunate bone are rare fractures inside the carpal bone due to their location in the concavity of the lunate fossa of the distal radius, fixed by interosseous ligaments to the scaphoids and to the triquetral bone and distally protected by the head of the large bone. This location provides suitable protection from wrist trauma. Acute traumatic fractures of the lunate account for between .5% and 1% of all carpal fractures.1,2 It is the fourth carpal bone which fractures most often, after the scaphoid, triquetral and trapezoid bones. Controversy abounds regarding the relative frequency of fractures of the lunate bone since Kienböck’s disease (or pathological fractures secondary to Kienböck’s disease) or congenital bipartite lunate bones may confuse the diagnosis of acute traumatic fractures.1–3 Blood supply comes from the proximal, dorsal and volar carpal arcs which form three variable anastomoses inside the lunate bone.4,5 Blood supply is exclusively volar in 20% of lunate bones which are more vulnerable to pseudo-osteoarthritis and avascular necrosis. The mechanism of injury is typically a fall on the outstretched hand and the wrist in hyperextension, or through direct trauma with the wrist extended producing an axial compression of the large bone which impacts the lunate bone. The first step in fracture diagnosis of the lunate bone is to determine whether it was due to a pathological process such as Kienböck’s disease, a congenital anomaly such as bipartite lunate or an acute traumatic fracture.1,3 Lunate fractures are classified into five types according to the Teisen classification (based on a review of 17 cases over 31 years),1 with type I (fractures of the volar pole) being the most common and type IV (sagittal fractures of the body of the lunate) and V (transverse fractures through the body of the lunate) the rarest.1,6,7 In type V fractures the dorsal portion of the lunate is dorsally displaced because it is no longer attached by the volar ligaments and the large bone acts as a proximal wedge causing separation at fracture site level and a high rate of pseudo-osteoarthritis and delay in consolidation.1
Lunate fractures may go unnoticed in normal radiographies and therefore when they are suspected, computerized tomography (CT) may be of highly useful. Magnetic resonance (MR) is one of the best methods for diagnostic assessment of associated Kienböck’s disease. In type II lunate fractures (chip fracture not affecting the blood supply), type III (fracture of dorsal pole) and type IV, conservative treatment is recommended with immobilization from four to six weeks. In types I and V conservative treatment is recommended only in the case of no displacement and surgical treatment using reduction and fixation with Kischner wires or screws if there is displacement (some authors even recommend them in all cases) to reduce the risk of an unstable wrist or of osteonecrosis.6,7 Complications we may find after lunate fractures include pseudo-osteoarthritis or delay in consolidation, avascular bone necrosis, carpal instabilities and post-traumatic osteoarthritis.8 As far as we know no case of delay in consolidation or pseudo-osteoarthritis has been published of lunate fractures treated with arthroscopy.
The aim of this study was to present our experience with treatment using incision, bone grafting and osteosynthesis wholly performed by arthroscopy in patients with delayed consolidation following a transverse fracture through the body of the lunate (Teisen classification type V).1
Material and methodWe present two clinical cases of delayed consolidation of a transverse fracture through the body of the lunate (type V) which were wholly treated by arthroscopy. The patients signed an informed consent form for the procedures and the study was approved by the ethics committee.
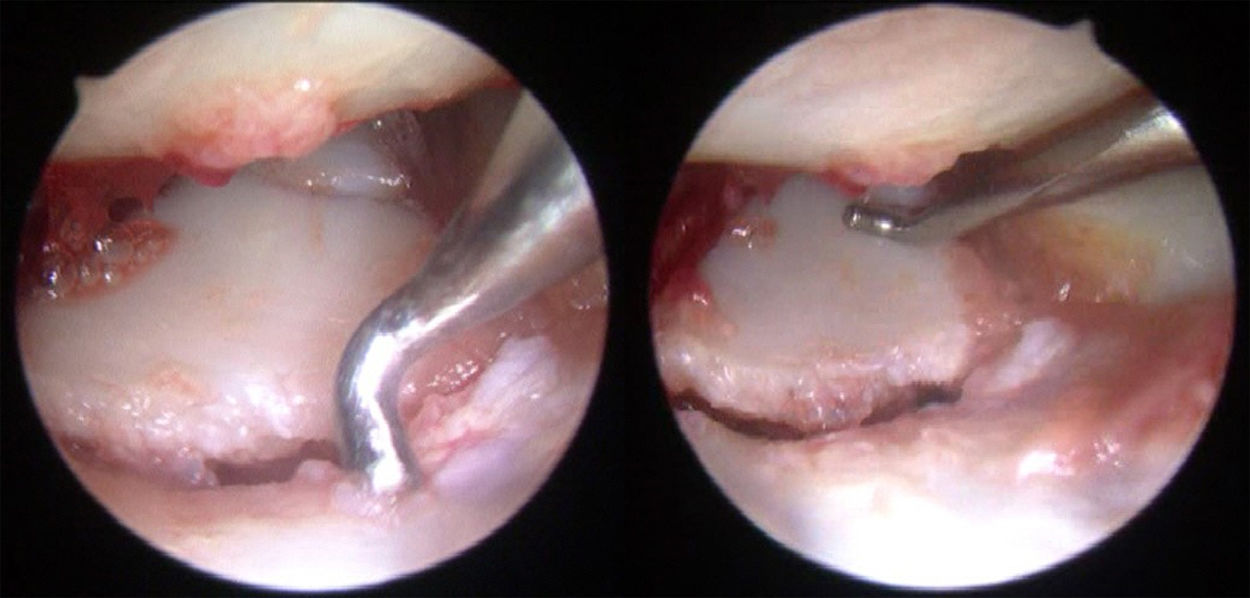
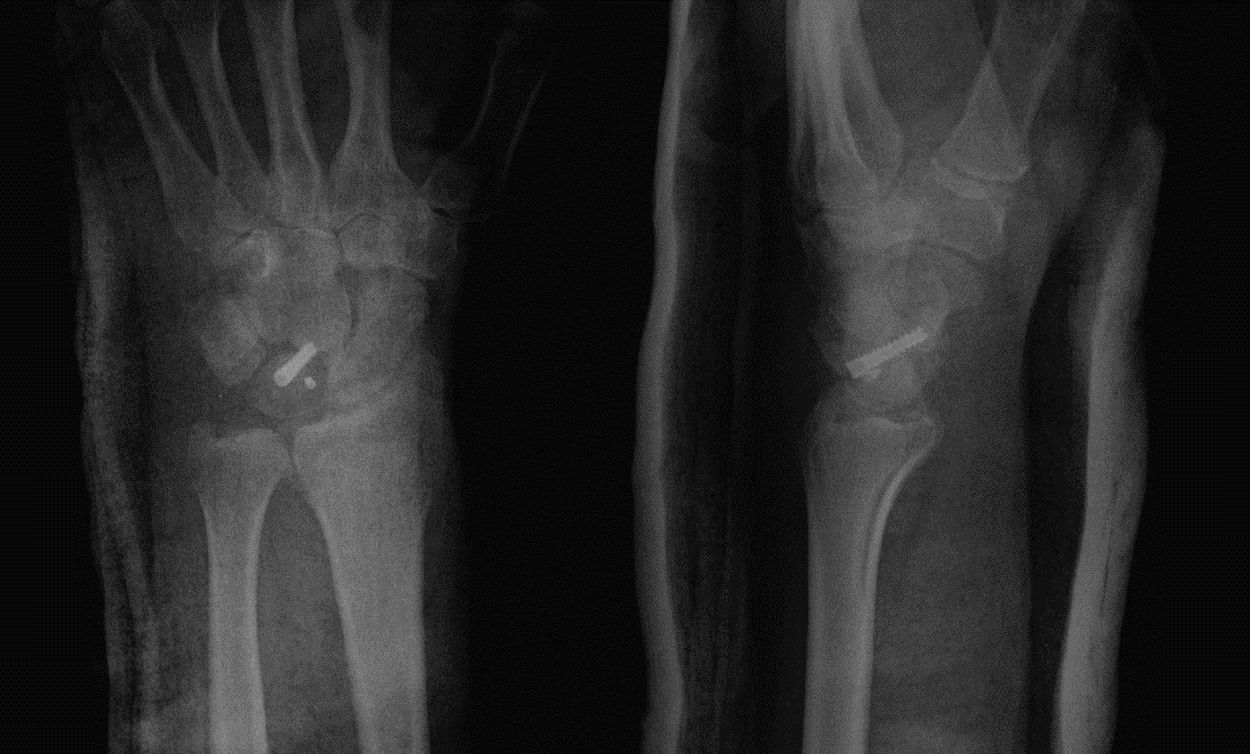
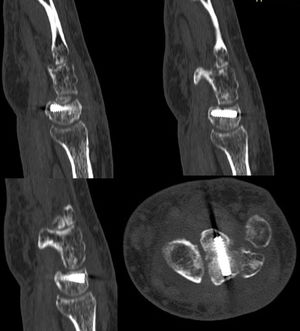
Clinical case 1A 51-year-old male manual worker who presented with sudden wrist pain after a fall. Following physical examination and imaging tests which included plain posteroanterior and lateral x-rays of the wrist, no bone injury was observed, and he was diagnosed with contusion of the wrist and fitted with a forearm cast for two weeks. After the two weeks the forearm cast was replaced with a wrist support and he was referred for physiotherapy. Due to the lack of improvement, CT and MR were performed after five months. The CT revealed a type V fracture through the body of the lunate which had not consolidated and the magnetic resonance ruled out the presence of osteonecrosis of the lunate. With these findings the patient was referred for consultation with the orthopaedic specialist for assessment regarding surgical treatment. A wholly arthroscopic intervention was performed: debridement and bleeding from the fracture site through the MC-R and MC-U portals, trabecular bone graft extracted from the homolateral olecranon and fixation with cannulated compression Acutrak type screw (Acumed Hillsboro, OR) under arthroscopic control of screw entry from the radius carpal portals 3–4 and 6R and fracture reduction using medial carpal vision. The patient was immobilized for one month with a forearm cast and the consolidation of the fracture was confirmed after three months, with clinical improvement in evolution and the return of the patient to their regular activity (Figs. 1 and 2).
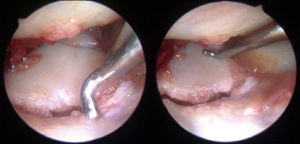
A 45-year-old male manual worker who after a fall from a height of 1.5 m presented with sudden wrist pain and dorsal swelling. Initially plain x-rays were requested of the wrist (posteroanterior and lateral projection) which showed no clear pathology. Due to suspected hidden injuries CT was requested which revealed a type V non displaced fracture through the body of the lunate and this was treated orthopaedically. Six weeks after treatment, the forearm cast was removed and a wrist support was fitted whilst the patient was referred for physiotherapy. Due to the absence of any clinical improvement, a further CT was requested after four months which showed delay in fracture consolidation (Fig. 3). It was decided that arthroscopic surgery be performed using the same technique as described in case 1. Arthroscopic examination confirmed the lack of consolidation (Fig. 4) and also detected a partial type 2 Gissler lesion of the scapholunate ligament which required capsuloligamentous repair suture, according to the technique described by Carratalá et al.9 and we performed (as described in case 1) debridement and bleeding from the fracture site, support of trabecular bone graft and fixation with cannulated compression Acutrak type screw (Acumed Hillsboro, OR) with satisfactory postoperative imaging controls (Figs. 5 and 6). The patient was immobilized with a brachial cast for one month and two weeks more with a forearm case followed by referral for physiotherapy with a wrist support. Three and a half months after surgery fracture consolidation was confirmed (Fig. 7) and the healing of the scapholunate ligament, with clinical improvement and a return of the patient to their regular activity.
We present two clinical cases of type V fracture, which is the least common type of lunate fracture, accounting for between .5% and 1% of carpal fractures.1,2,6 As occurred in the reported cases, it is commonplace for the fracture not to be observed plain X-rays, or for the severity or displacement to be minimized, and therefore when there is a suspicion of the condition or from the plain x-ray, CT must be performed for accurate diagnosis.2 Similarly to the case described by Hsu et al.,10 in our study, in case 1, the fracture was not suspected, and CT was therefore not requested, with consequent inaccurate diagnosis. The wrist was therefore not immobilised long enough and the fracture was determined in the delayed consolidation phase. In case 2, despite plain x-ray not being sufficient for diagnosis, clinical suspicion remained and CT was requested for accurate diagnosis. This resulted in the complete immobilization protocol being fulfilled.
The blood supply of the lunate bone has been widely studied.4,5 Both the volar and the dorsal blood supply are present in 74% to 100% of the bones. These studies have demonstrated that there is a single vascular blood supply in approximately 20% of the lunate bones. Of the lunate bones with a double blood supply, 33% have a single volar and dorsal vessel for anastomosis, 66% have three-vessel anastomosis and 10% have four-vessel anastomosis. In the lunate bones with a single blood vessel, the interruption of the supply may lead to necrosis of the bone. Similarly, a transverse fracture in these lunate bones may lead to vascular necrosis of the opposite pole. Although not all fractures which divide the lunate bone in their dorsal and volar halves lead to avascular necrosis of the bone, 20% of lunate bones only have one volar artery for blood supply. The displaced volar fragments unreached may increase the risk of avascular necrosis of the bone and therefore these fractures should be anatomically reduced and osteosynthesized. As a result type I and type V fractures lead to a higher risk of osteonecrosis and delay in consolidation, as occurred in our series.
In type V lunate fractures conservative treatment is recommended only if there is no displacement and if there is displacement surgical treatment is recommended with reduction and fixation with Kirschner wire, or screws if there is displacement (some authors even recommend they be used in all cases).6,7,10 Hsu et al.10 published the osseous union of an isolated transverse fracture of the lunate treated with open surgery with headless compression screws after seven weeks, with no evidence of osteonecrosis and recovery of the normal range of movement of the wrist. As a result, the recommended definitive treatment of displaced fractures is immediate anatomical reduction using open reduction and internal fixation to improve anatomical alignment and function status and to reduce the risk of future osteonecrosis.10 However, despite early and accurate treatment, several diverse complications may arise. Transverse fractures which depend on a single blood supply present with a high risk of avascular necrosis, particularly those of the volar pole. In the presence of this lesion particular care must be taken for perfect reduction of the fragments, to restore carpal congruency. Posterior complications to fracture of the lunate include psudo-osteoarthritis, avascular necrosis, instability of the carpal and post-traumatic arthritis.8 Osteonecrosis of the lunate bone may be a more devastating complication of lunate fractures, with advanced collapse and progression towards radius and carpal bone osteoarthritis. This would lead to further surgical interventions to alleviate pain, which includes radial shortening, radial wedge osteotomy, lengthening of the ulnar, the performing of rescue surgery such as proximal row carpectomy, denervation of the wrist or arthrodesis. In a systematic review on lunate fractures Shunmugam et al.11 found 34 acute fractures of the lunate published in 31 different articles. In eight of the 14 fractures -lunate dislocations led to a lack of union, avascular necrosis or the need for a rescue procedure with this type of lesion having the poorest prognosis.11
The use of arthroscopy leads to direct assessment of fractures, delay in consolidation or pseudo-osteoarthritis of the lunate bone and other lesions associated with soft tissue, if they are present. It also facilitates direct observation of both fracture reduction, bone grafting in the previously debrided region and the identification of the entry point of the guide wire and posterior positioning of the cannulated screw directly displaying screw entry. It also has the advantage of preserving the vascular structures of the body of the lunate on respecting the volar and dorsal insertions of soft tissue and blood vessels entry, in contrast to the traditional open approach. This in turn favours posterior consolidation in the delayed consolidation and pseudo-osteoarthritis of the lunate bone. Another major aspect provided by arthroscopy is the preservation of the posterior interosseous nerve, with its subsequent preservation of wrist propioception and the avoidance of injury to the dorsal ligaments, which means good mobility and functionality of the wrist after injury may be maintained. All these vascular, nerve and ligament structures may be damaged in open surgery approaches.
The arthroscopic treatment of the consolidation delays of an isolated fracture of the crescent without associated perilunate dislocation has not been previously described. Information does exist on the arthroscopic treatment of acute fractures of the crescent: Dana et al.12 published a case of an acute avulsion fracture of the dorsal pole of the crescent with a bone fragment separating the posterior part of the escafolunar ligament, which was successfully treated by arthroscopic percutaneous screw repair.
Arthroscopic treatment of delay in consolidation and pseudo-osteoarthritis of the scaphoid bones has been described and involves debridement of non union, bone grafting and rigid internal fixation in patients with minimally displaced pseudo-osteoarthritis. This treatment has been shown to have a series of advantages compared with conventional open surgery techniques.13 As occurs with the scaphoids, arthroscopic treatment of delay in consolidation of fractures of the lunate bone using debridement, grafting and osteosynthesis provide the same advantages (direct observation of reduction and osteosynthesis material implantation; lower soft tissue injury–blood supply structures, nerves and tendon, and the diagnosis and possible treatment of other coexisting intra-articular lesions which may be gone unnoticed).
To conclude, arthroscopic treatment using debridement, grafting and osteosynthesis is a valid, effective and safe technique for the treatment of delay in consolidation of transverse fractures through the body of the lunate and avoids complications and soft tissue injuries of the open surgery techniques.
Level of evidenceLevel of evidence IV.
FinancingThis study did not receive any type of financing.
Conflict of interestThe authors have no conflict of interests to declare.
Please cite this article as: Lucas FJ, Carratalá V, Miranda I, Carratalá R. Fracturas transversales del cuerpo del semilunar con retraso en la consolidación. Experiencia en el tratamiento artroscópico. Rev Esp Cir Ortop Traumatol. 2020;64:421–427.