The main objective of this study is to compare proportionally the incidence of total ankle arthroplasty (TAA) versus ankle arthrodesis and to determine the variables that may have influenced its indication. The secondary objective is to analyse the trend in the use of TAA using a population-based analysis and to compare our results with those reported by national registries in other countries.
Material and methodA retrospective review of the Minimum Basic Data Set from 1997−2017 was performed. Subjects were categorised according to surgical procedure. Their temporal evolution was analysed and hospital variables associated with the indication (age, sex, hospital complexity) were identified. In order to compare the trend in Spain with respect to other countries, the information was standardised as number of procedures per 100,000 inhabitants/year and a projection was made for the five-year period 2020–2025.
ResultsIn the period 1997−2017, 11,669 ankle arthrodesis and 1,049 TAAs were performed. The trend was increasing and significant for both procedures, however, in the last 10 years analysed the proportional trend of TAA decreased significantly. Being female (OR 1.32), being 65 years or older (OR 1.50) and being operated in a complex hospital (OR 1.31) were associated with the indication for a TAA. Compared to other countries, Spain has much lower rates of TAA utilisation, with minimal growth estimated for the year 2025.
ConclusionAlthough the use of TAA has increased, its growth has been lower than that of ankle arthrodesis and its current trend is proportionally decreasing, with female sex, age ≥ 65 years and the patient being operated in a medium/high complexity hospital being associated with the indication for TAA. Compared with other countries, Spain has much lower rates of use and its projection over the next five years, although increasing, is expected to be minimal.
El objetivo principal de este estudio es comparar proporcionalmente la incidencia de artroplastia total de tobillo (ATT) frente a artrodesis de tobillo y determinar las variables que han podido influir en su indicación. El objetivo secundario es analizar la tendencia en el uso de ATT utilizando un análisis de base poblacional y comparar nuestros resultados con los informados por los registros nacionales de otros países.
Material y métodoSe realizó una revisión retrospectiva del conjunto mínimo básico de datos de 1997−2017. Los sujetos fueron categorizados según el procedimiento quirúrgico. Se analizo su evolución temporal y se identificaron las variables hospitalarias asociadas con la indicación (edad, sexo, complejidad del hospital). Para poder comparar la tendencia en España con respecto a otros países se estandarizo la información como numero de procedimientos por cada 100.000 habitantes/año y se realizó la proyección para el quinquenio 2020–2025.
ResultadosEn el periodo 1997−2017 se realizaron 11.669 artrodesis de tobillo y 1.049 ATT. La tendencia fue creciente y significativa para ambos procedimientos, sin embargo, en los último 10 años analizados la tendencia proporcional de ATT decreció de manera significativa. El ser mujer (OR 1,32), tener 65 o más años (OR 1,50) y ser intervenido en un hospital complejo (OR 1,31) se asociaban con la indicación de una ATT. Comparativamente con el resto de los países, España presenta tasas de utilización de ATT mucho más bajas y para el año 2025 se estima un crecimiento mínimo.
ConclusiónA pesar de que ha aumentado el uso de ATT, su crecimiento ha sido menor que el de la AT y proporcionalmente su tendencia actual es decreciente, estando asociados con la indicación de ATT el sexo femenino, la edad ≥ 65 años y que el paciente sea intervenido en un hospital de media/alta complejidad. Comparativamente con otros países, España presenta tasas de utilización mucho más bajas y su proyección en el próximo quinquenio, aunque creciente, se prevé que será mínima.
Historically, ankle arthrodesis (AA) has been the treatment of choice for patients with advanced osteoarthritis of the ankle.1 This procedure is not free from complications such as pseudo osteoarthritis and the development of osteoarthritis in adjacent joints due to overload, with the possible presentation of pain and persistent changes to gait.
During the 1970’s, total ankle arthroplasty (TAA) was established as an alternative. The first designs were linked to early, common failures and were therefore not accepted for the treatment of ankle osteoarthritis.2–6 Current implant design more closely replicates the natural anatomy and biomechanics of the ankle, leading to lower wear and tear and lower rates of loosening.2–6 Advances in surgical instrumentation have thus improved the reproducibility of the technique.6
Compared with arthrodesis, TAA has had similar clinical outcomes,7,8 with several reports that describe a higher risk of revision surgery.8 However, no controlled clinical trials have been conducted to compare the 2 procedures.9 Furthermore, the tendency towards TAA use reflected in arthroplasty registers of other countries has been irregular, from a rising, sustained start in use to a sudden disuse or minimal use of implants.10,11
In Spain, ankle prosthesis has been the subject of very few publications and those existing are essentially descriptive with regards to prescription and surgical technique.12–15 Four publications deal with patient series with objective data16–19 and only one makes comparisons with AA,20 with better outcomes for TAA. As far as we are aware, no studies in Spain have analysed the use of TAA, nor are there any specific patient and hospitals factors which affect their indication compared with AA. The main objective of this study was to proportionately compare the rate of TAA with AA and determine whether variables such as age, sex or hospital characteristics could affect their indication. Our secondary objective was to analyse the trend in the use of TAA, using a populational base analysis and comparing our results with those of the national registers of other countries.
Material and methodUsing the basic minimum dataset (bMDS)21 a retrospective review was made from 1997 to 2017. The bMDS recorded all hospital admission from the National Health System using the ninth edition of the International Classification of Diseases (ICD-9) from 1997 until 2015 and the tenth edition (ICD-10) from 2016. Episodes of hospitalisation were identified where a TAA or AA procedure was undertaken. Those episodes were excluded where the procedure was “review of lower extremity joint replacement, unclassified elsewhere”.
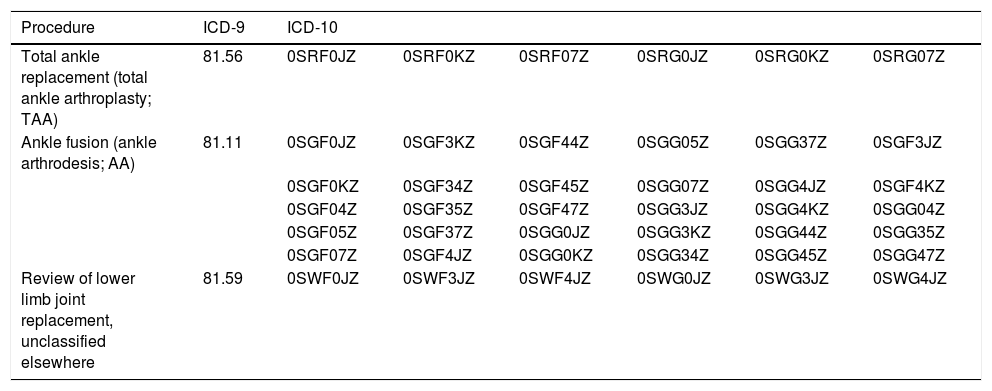
The ICD-9 codes have a length of 3–4 numerical characters, they are included in the tabular list of procedures: chapter 14 “Operations on the musculoskeletal system (codes 81.xx)”. ICD-10 codes have a length of 7 alphanumerical characters. Each one of the positions of the code represents one aspect of the procedure: First = Section (0 = Surgical); Second = Organic system (S= Lower joints); Third = Type of procedure (R = Replacement/G = Fusion/W = Revision); Fourth = Anatomical location (F/G = Ankle); Fifth = Approach; Sixth = Device; Seventh = Qualifier (Table 1).
ICD codes used.
| Procedure | ICD-9 | ICD-10 | |||||
|---|---|---|---|---|---|---|---|
| Total ankle replacement (total ankle arthroplasty; TAA) | 81.56 | 0SRF0JZ | 0SRF0KZ | 0SRF07Z | 0SRG0JZ | 0SRG0KZ | 0SRG07Z |
| Ankle fusion (ankle arthrodesis; AA) | 81.11 | 0SGF0JZ | 0SGF3KZ | 0SGF44Z | 0SGG05Z | 0SGG37Z | 0SGF3JZ |
| 0SGF0KZ | 0SGF34Z | 0SGF45Z | 0SGG07Z | 0SGG4JZ | 0SGF4KZ | ||
| 0SGF04Z | 0SGF35Z | 0SGF47Z | 0SGG3JZ | 0SGG4KZ | 0SGG04Z | ||
| 0SGF05Z | 0SGF37Z | 0SGG0JZ | 0SGG3KZ | 0SGG44Z | 0SGG35Z | ||
| 0SGF07Z | 0SGF4JZ | 0SGG0KZ | 0SGG34Z | 0SGG45Z | 0SGG47Z | ||
| Review of lower limb joint replacement, unclassified elsewhere | 81.59 | 0SWF0JZ | 0SWF3JZ | 0SWF4JZ | 0SWG0JZ | 0SWG3JZ | 0SWG4JZ |
ICD: International Disease Classification.
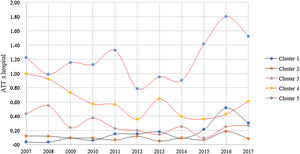
The subjects were classified according to the surgical procedures and the hospital variables associated with the indication were identified. For this the hospital cluster classification system was used.22 The type of hospital was dichotomised, with consideration of the centre complexity. Group 1 or low complexity (hospital belonging to clusters 1 and 2: with a mean of under 200 beds, fewer than 10 internal medicine resident physicians and an indication of activity, funding, and technology below the mean), and group 2 or medium/high complexity (clusters 3, 4 and 5: between 500 and 1,200 beds on average, between 60 and 300 internal medicine resident physicians and activity, funding, and technology above the mean). Gender and age variables were also assessed, divided into 2 groups with a cut-off age of 65 years.
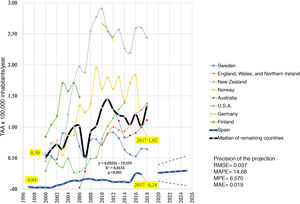
To gain an understanding of trends in Spain compared with other countries, information was used from the national arthroplasty registers of Sweden,23 New Zelanda,24 Norway,25 Australia,26 Germany,27 Finland28 and England, Wales and Northern Ireland.29 The United States (U.S.A.) had no ankle arthroplasty register, and information was therefore extracted from the Healthcare Cost and Utilization Project (HCUP).30 Information was standardised with regard to the total number of inhabitants per year studded provided by the World Bank31 and was presented as the number of arthroplasties per 100,000 inhabitants/year.
Statistical analysisStatistical analysis was preformed using SPSS v.22 and Excel software. The bilateral significance level of p in all tests was below .05.
The number of procedures made was compared. The association between the nominal variables was assessed using the exact Fischer test. The variables which presented with significant differences were included in a multivariate logistic regression model, with data expressed as odds ratio (OR) with their 95% confidence interval (95% CI). The Hosmer-Lemeshow test was used to study the model fit.
For Spain, temporal trend determination of different analyses was studied using the simple lineal regression model, its adjustment through the determination coefficient (R2) and its significance using Pearson statistics. For estimation of the 2020–2025 projection, the temporal Holt-Winters method was used and precision measurements were calculated.
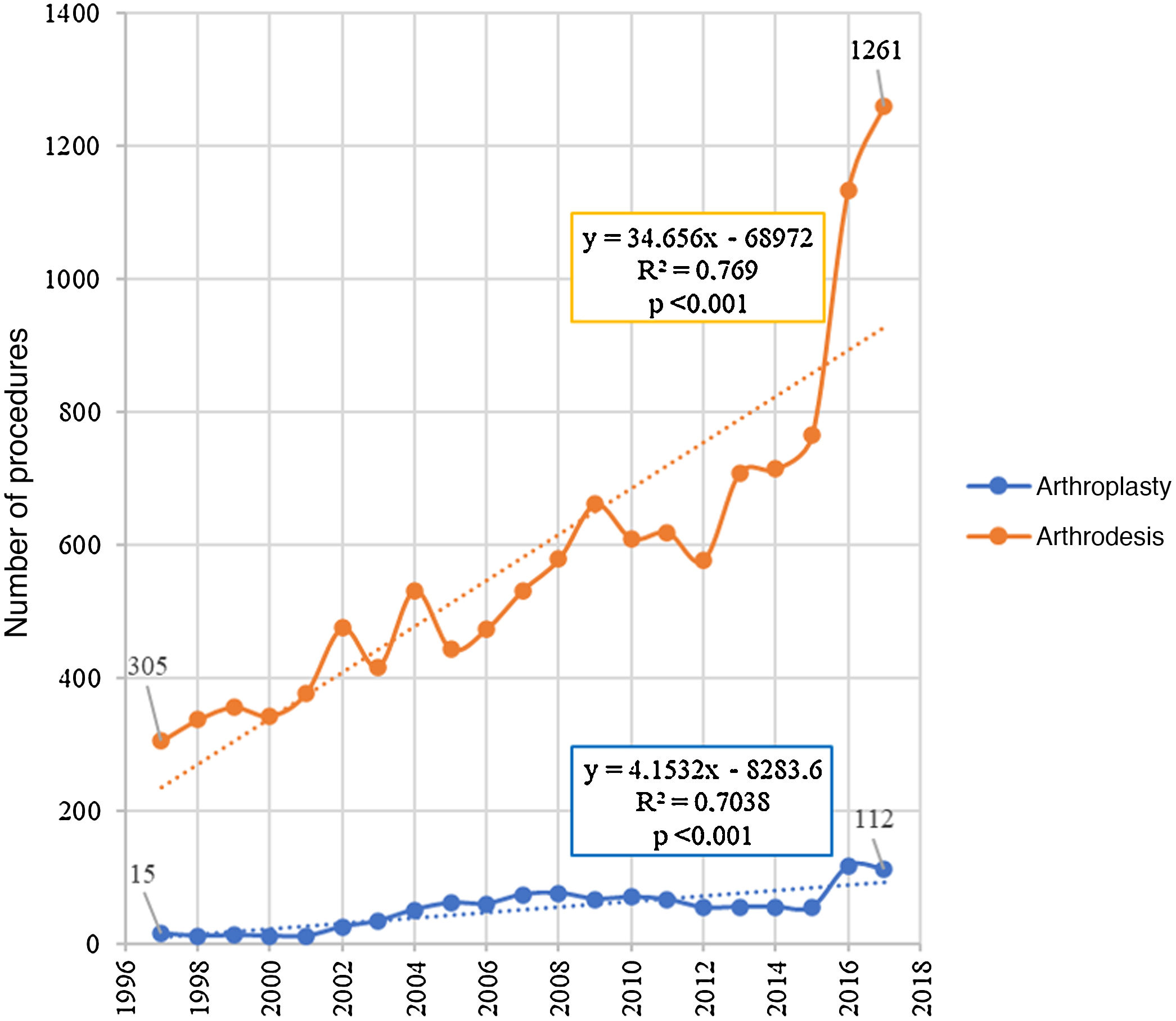
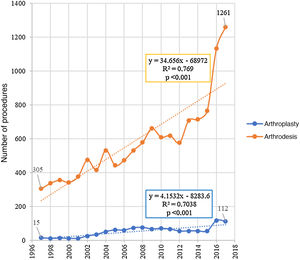
ResultsDuring the 1997−2017 period 11,669 AA and 1,049 TAA were performed. There was a rising, significant tendency for both procedures but in the case of arthroplasty growth was slow, with a rise of 4.1 TAA more per year, increasing from 15 in 1997 to 112 in 2017. In the case of arthrodesis, the increase in tendency was 8 times higher than that of TAA, rising from 305 to 1,261 during the same period (Fig. 1).
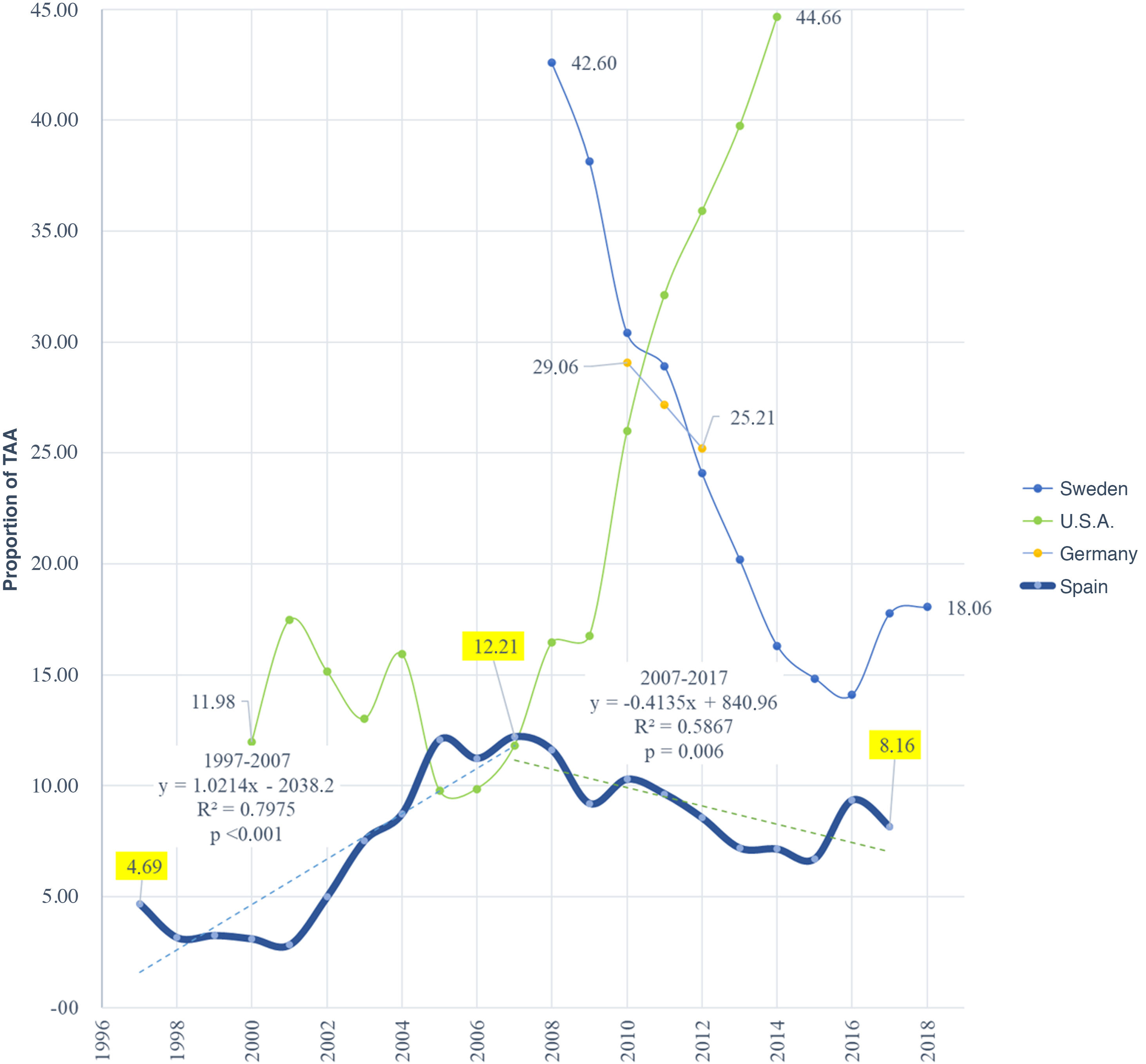
In Spain, compared with AA, the number of TAA increased from 4.69% of all procedures in 1997 to 12.21% in 2007, but during the following 10 years the proportional tendency fell significantly to 8.16% in 2017 (Fig. 2).
For the total period 1997−2017, 7.1% (497) of men and 9.7% (552) of women underwent a TAA (p < .001). Eight thousand seven hundred and thirty-one patients were aged 64 or under and 3,987 were 65 or over, with 10.7% (426) of the latter undergoing a TAA compared with 7.13% (623) of the patients being aged under 65 (p < .001). In the hospitals classified as group 1, 4,078 procedures were preformed with 7% (286) TAA, whilst in the group 2 hospitals 8,640 procedures were performed, with 8.83% (763) being TAA (p = .001).
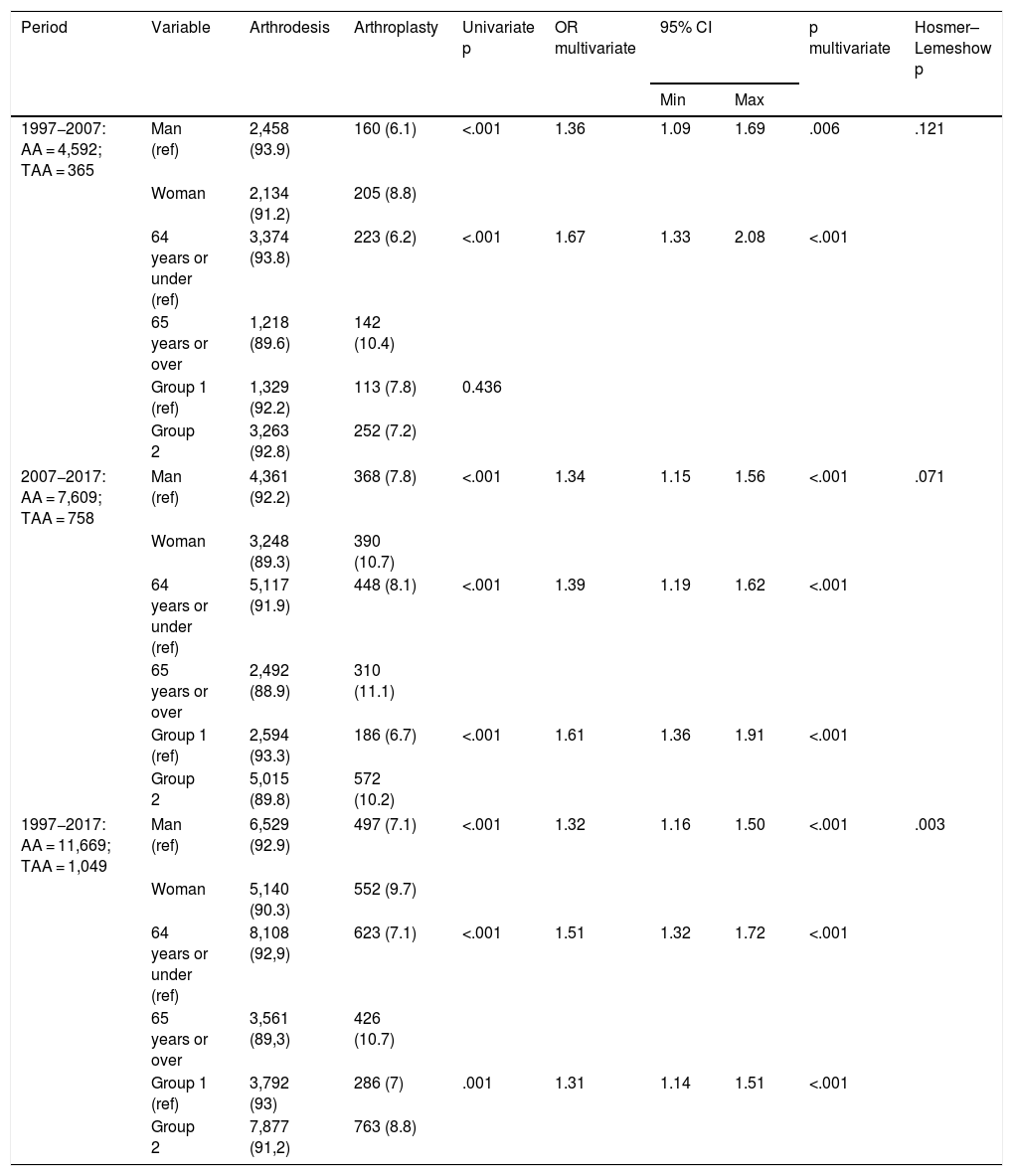
In the multivariate analysis, being a woman (OR 1.32; 95% CI 1.16–1.50; p < .001), being aged 65 or over (OR 1.50; 95%CI 1.32–1.72; p < .001) and undergoing surgery in a group 2 hospital (OR 1.31; 95%CI 1.13–1.51; p < .001) was associated with indication for a TAA (Table 2).
Predictor characteristics of procedure selection.
| Period | Variable | Arthrodesis | Arthroplasty | Univariate p | OR multivariate | 95% CI | p multivariate | Hosmer–Lemeshow p | |
|---|---|---|---|---|---|---|---|---|---|
| Min | Max | ||||||||
| 1997−2007: AA = 4,592; TAA = 365 | Man (ref) | 2,458 (93.9) | 160 (6.1) | <.001 | 1.36 | 1.09 | 1.69 | .006 | .121 |
| Woman | 2,134 (91.2) | 205 (8.8) | |||||||
| 64 years or under (ref) | 3,374 (93.8) | 223 (6.2) | <.001 | 1.67 | 1.33 | 2.08 | <.001 | ||
| 65 years or over | 1,218 (89.6) | 142 (10.4) | |||||||
| Group 1 (ref) | 1,329 (92.2) | 113 (7.8) | 0.436 | ||||||
| Group 2 | 3,263 (92.8) | 252 (7.2) | |||||||
| 2007−2017: AA = 7,609; TAA = 758 | Man (ref) | 4,361 (92.2) | 368 (7.8) | <.001 | 1.34 | 1.15 | 1.56 | <.001 | .071 |
| Woman | 3,248 (89.3) | 390 (10.7) | |||||||
| 64 years or under (ref) | 5,117 (91.9) | 448 (8.1) | <.001 | 1.39 | 1.19 | 1.62 | <.001 | ||
| 65 years or over | 2,492 (88.9) | 310 (11.1) | |||||||
| Group 1 (ref) | 2,594 (93.3) | 186 (6.7) | <.001 | 1.61 | 1.36 | 1.91 | <.001 | ||
| Group 2 | 5,015 (89.8) | 572 (10.2) | |||||||
| 1997−2017: AA = 11,669; TAA = 1,049 | Man (ref) | 6,529 (92.9) | 497 (7.1) | <.001 | 1.32 | 1.16 | 1.50 | <.001 | .003 |
| Woman | 5,140 (90.3) | 552 (9.7) | |||||||
| 64 years or under (ref) | 8,108 (92,9) | 623 (7.1) | <.001 | 1.51 | 1.32 | 1.72 | <.001 | ||
| 65 years or over | 3,561 (89,3) | 426 (10.7) | |||||||
| Group 1 (ref) | 3,792 (93) | 286 (7) | .001 | 1.31 | 1.14 | 1.51 | <.001 | ||
| Group 2 | 7,877 (91,2) | 763 (8.8) | |||||||
When we analysed whether the variables which were associated with the TAA indication were the same for the periods 1997−2007 and 2007−2017, we found that, for the first period, the hospital complexity was not the same. For the second period the same variables as those in the total period analysis associated with the TAA indication were maintained and the model was adjusted (Hosmer–Lemeshow p = .071).
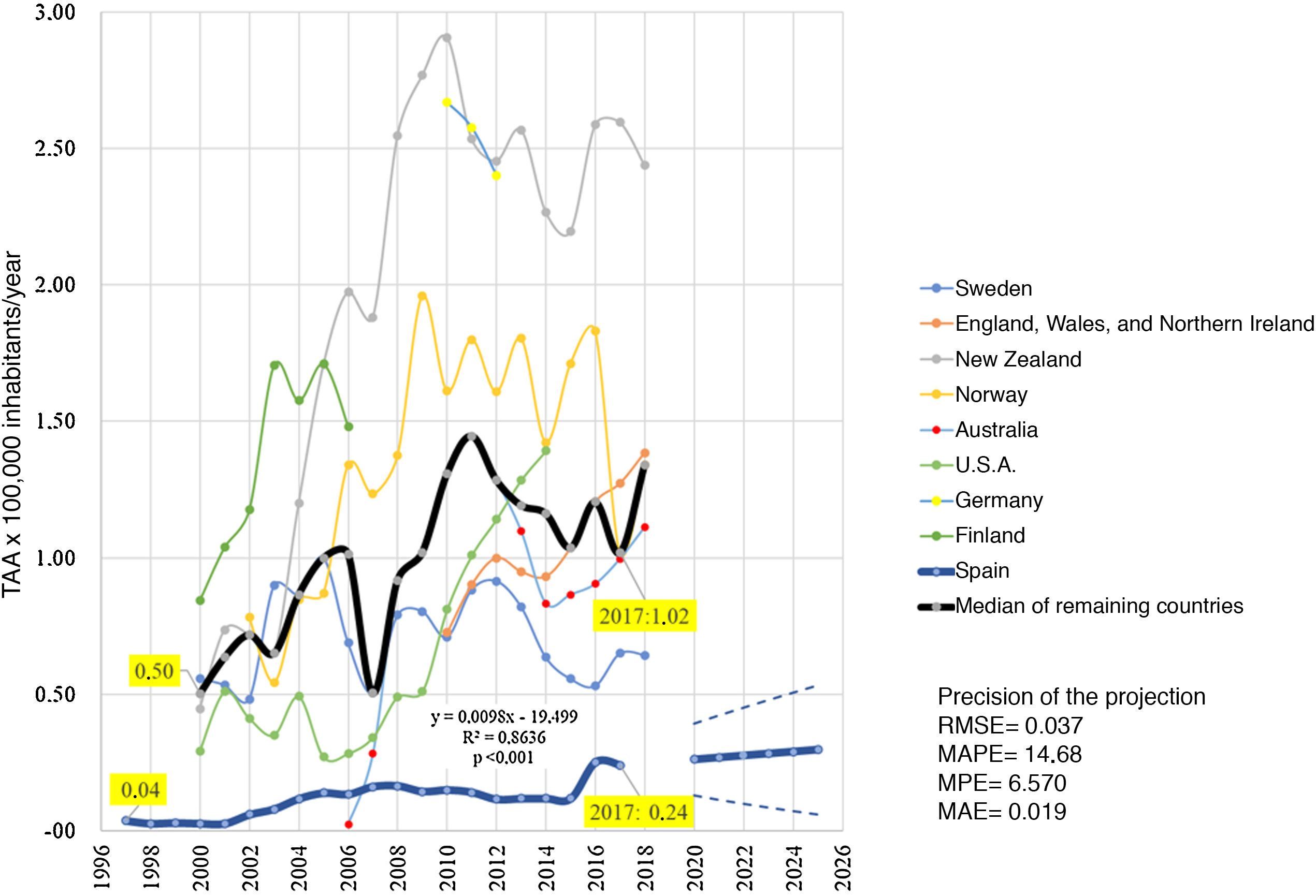
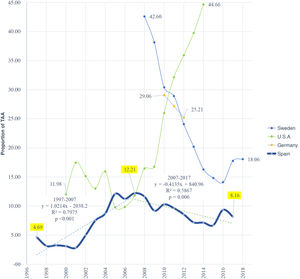
With regards to the population, a significant growth in the use of TAA for each 100,000 inhabitants/year in the total period was observed, increasing from .04 procedures in 2007 to .24 in 2017. However, compared with the other countries analysed, Spain presented much lower usage rates. In 2017, the median of use for every 100,000 inhabitants/year in the other countries was up to 4 times higher than in Spain, with the closest difference being with Sweden where .65 TAA for every 100,000 inhabitants were performed (Fig. 3). The most extreme difference was New Zealand which performed 2.60 ATT for every 100,000 inhabitants (Fig. 3).
For the year 2025 a minimum growth was estimated in the use of TAA up to .30 (95%CI .06–.53) for every 100,000 inhabitants (Fig. 3).
DiscussionComparatively we observed an increase in the proportion of TAA regarding the total number of procedures for the whole period studied but we cannot ignore that the said period consisted of 2 stages. In the most recent stage (2007−2017) there was a negative tendency in the proportion of TAA. These results concur with those observed in European countries such as Sweden or Germany and differ from those observed in U.S.A. where it is believed that the enthusiasm for the use of TAA from 2006 onwards is related to the approval by the FDA (Food and Drug Administration) of the INBONE (Wright Medical Technology, Arlington, TN); Salto-Talaris (Tornier, Stafford, TX), Eclipse (Integra Life Sciences, Plainsboro, NJ) and S.T.A.R. (Small Bone Innovations, Morrisville, PA) systems, which were offered as alternatives to the Agility (DePuy, Warsaw, IN) system which up until then had been the only one approved.32
Throughout the period studied (1997−2017), when the TAA was the prescribed therapy, the factors associated with this choice were: being female; 65 years of age or above. We also observed that the most complex hospitals tended to carry out a high proportion of TAA. However, this predictive model was not adjusted (Hosmer-Lemeshow p = .003). On analysis of the second half of the study period (2007−2017), we observe that the same variables were associated with TAA as the prescribed therapy, in an adjusted model (Hosmer-Lemeshow p = .071).
Countries such as New Zeland24 or the conglomerate of England, Wales and Northern Ireland29 performed more TAA in men, 60.65% and 59.6%, respectively. In U.S.A. the same amount of TAA was performed on both sexes.32 In Sweden, as with Spain, more TAA were performed on women.23 These differences are difficult to explain. As far as we know, the possible influence of gender in patient satisfaction or prosthesis maintenance has not been explicitly studied. In the analysis of the majority of records no gender influence was found in TAA survival.24,26,28,33,34 In the Swedish record an association between the female sex and the need for revision was found.35 In one clinical study the female sex was a factor associated with problems of wound healing after TAA, but after correcting the confusion variables, this was no longer an associated factor.36 On the contrary, in another study the male sex was associated with the appearance of one or more complications within 30 days following surgery.37 Therefore, bearing in mind all the evidence, we believe that gender should play no role when considering a patient as a candidate for TAA.
Despite the fact that being 65 years of age or above is a factor associated with TAA selection, in Spain 59% of arthroplasties have been implanted in patients who are younger. TAA in young patients has long been considered to be surgically contraindicated with the cause allegedly being that due to the excessive load components are subjected to, this could, to some extent, promote loosening,12 and therefore this procedure was to be considered an exceptional, not as a primary procedure and only as an alternative to arthrodesis. Notwithstanding, clinical evidence is contradictory. When the topic is specifically approached, age is not associated with a higher risk for revision or wound healing problems.38 Also, age cut-offs are varied. For several authors, patients under 55 years of age are at greater risk of TAA failure,39 whilst for others this threshold is at 70 years of age.40 In analyses of registers in Sweden,35 patients under 60 were at greater risk of revision surgery and by contrast, age was not found to be associated with survival in the TAA records of Norway, Finland or New Zealand.28,33,41 Despite the risk of prosthetic loosening being present, unlike other load joints, such as the hip or knee, the aetiology of tibiotalar osteoarthritis is related to a background of trauma or chronic instability. This implies a younger mean age, patients of working age, with higher functional requirements and demanding of improved quality of life. However, as has already been commented upon, after an AT it has been demonstrated how in the long term, osteoarthritis develops in the neighbouring joints.1 This is because the loss of joint mobility at ankle level leads to an increase in the mobility of these joints, particularly at the Chopart joint level but also at subtalar level. Jones et al.,42 found that being young in age was a progressive risk factor of osteoarthritis in neighbouring joints after an AA, and that patients with an increase of one radiographic degree in the subtalar joint or in the talonavicular joint (according to the osteoarthritis scale of Van Dijk and the osteoarthritis scale of Kellgren–Lawrence), were more likely to obtain a standard or poor score in the FAOS S (Foot and Ankle Outcome Score) and the AOS (Ankle Osteoarthritis Scale). Because TAA maintains movement the appearance of osteoarthritis in neighbouring joints is prevented and subtalar arthrodesis may also even be avoided in the case that this joint is found to be impaired during surgery, and this could be an advantage in younger patients. However, it should be noted that prescribing TAA in a young patient should be strict and limited to those with good general status, who are not obese, have no major diseases, are physically active, play moderate sport, who have permanent strong pain, difficulty walking and limited mobility, but whose joint continues to have suitable biomechanical conditions, with functioning passive structures, good bone quality, without desaxations of the lower limb and good skin cover.12 This could also be an option in young patients with arthrodesis of the contralateral ankle.12
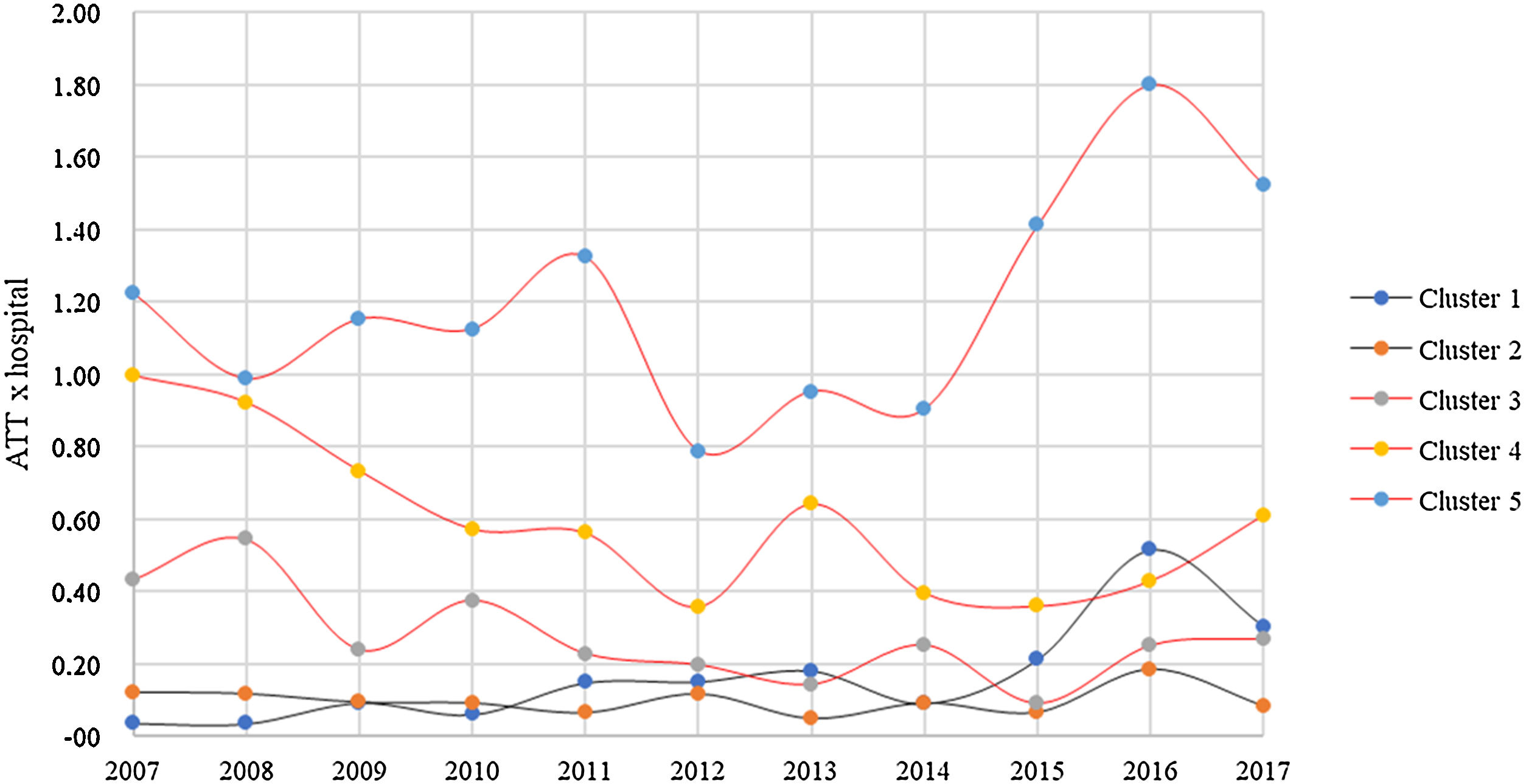
In Spain, the most complex hospital centres have increased the proportion of TAA they perform, from 69% (1997−2007) to 75% (2007−2017) and undergoing surgery in these centres is a factor which is associated with choosing arthroplasty as treatment when they are compared with group 1 centres. This could be linked to the creation of specific foot and ankle units in hospitals of greater complexity and with a growing sub-specialisation of the orthopaedic surgeon. The Spanish National Health System consists of 13% of hospitals belonging to cluster 1, 47% to cluster 2, 22% to cluster 3, 11% to cluster 4 and the remaining 7% to cluster 5.22 Extrapolating these numbers to those of the national catalogue of hospitals,43 it is in the last cluster where a greater accumulation of procedures per hospital were found (Fig. 4). Our results are in keeping with the register analyses, where it has been recommended that the TAA be performed in specialised centres and by specialised surgeons to avoid limiting the experience and to be able to overcome the necessary learning curve to undertake the procedure with sufficient guarantee.43,44 This is of particular importance, bearing in mind that many studies indicate that a prolonged learning curve is associated with poorer clinical outcomes for patients and a reduction in implant survival.34,44–46 It is true that the Spanish average of 1.2 (1.5 in 2017) TAA per high complexity centre is low. The English register reports of 4.2 TAA per unit/year.29 In New Zealand in 2018, 18 surgeons performed 117 TAA (6.5/surgeon), and of these, 3 carried out over 15 procedures and 9 carried out fewer than 5.27 Although our data do not indicate the number of TAA per surgeon, such a low overall number of TAA observed suggests that it is difficult to achieve the 21 procedures per year necessary to reduce the number of adverse events and prevent long hospital stays,46 with it being recommendable to assess the creation of specialised reference units. For example, in Sweden fewer units and surgeons preform TAA, which results in higher numbers per surgeon. This and the supposedly increasing experience of these surgeons may have helped to improve the reported outcomes in this register.47
Regarding population, growth observed has been very slow and projection in the best of cases is to reach .53 TAA per 100,000 inhabitants in the year 2025, in a model with acceptable precision, albeit far from the current median of the other countries. This leads us to believe that in Spain there is a tendency to prefer AA as first treatment option, including for the near future. It is to be expected that expansion of TAA will undoubtedly take off when a higher number of accessible review systems become available. At present, few TAA review systems exist. For review of the tibial component intramedullary stems may be used which are designed not to impair the anterior cortical of the tibia and which lead to stable fixation despite metaphysary defect.48,49 For the talar component, options are more unreliable, due to the characteristics of the bone itself. Systems with attachment to the heel bone exist, as do extra thick polyethylene (Salto Talaris XT, Integra LifeSciences, Plainsboro, Nueva Jersey, U.S.A.) or tailor-made prostheses. Furthermore, the outcomes of revision TAA are lower than those of primary TAA, with poor outcomes in functional scales and patient satisfaction, and a poor survival of the implant of only 55% at 10 years.50 This all means that the secondary arthrodesis continues being the procedure of choice when a TAA fails. This is a complex procedure which requires the use of structural allografts or tantalum spacers, with fusion rates of approximately 90% where clinical outcomes are lower than those of primary arthrodesis (under 50% of satisfied patients) and functional outcomes are low.51
The main limitation of this study is that, as with any large administrative database, data entry into the bMDS may be subject to errors or imprecise coding. Equally, the effect of changes in ICD coding which occurred during the study period is difficult to determine. As a result of all of this, our results should be cautiously interpreted. Despite these limitations, we believe that the large patient sample in our analysis has led to us drawing up plausible conclusions regarding TAA usage tendencies in Spain.
ConclusionThis study shows that despite the increased use of TAA, its growth has been lower than that of AA and proportionally its current tendency is dropping. The associated factors with TAA are being female, aged 65 years or above and the patient having undergone surgery in a hospital of medium/high complexity. Furthermore, compared with other countries, Spain presents much lower usage rates and in the next five-year-term its projection may increase, but will be minimal.
Level of evidenceLevel of evidence: IV.
Conflict of interestsThe authors have no conflict of interest to declare.
Please cite this article as: Novoa-Parra CD, Gil-Monzó E, Díaz-Fernández R, Lizaur-Utrilla A. Tendencia en España en el uso de artroplastia total de tobillo frente a artrodesis en el periodo 1997−2017. Rev Esp Cir Ortop Traumatol. 2021;65:450–459.