Malingering, defined as a deliberate attempt to lie or deceive in connection with an illness or disability, exaggerating the symptomatology, with the aim of obtaining a personal benefit, is a complex phenomenon, seldom studied in our professional context. The objective of this study was to analyse the way in which this phenomenon manifests itself in the forensic field.
Material and methodsAn incidental sample of 190 subjects attended in the Psychology Unit (IMLCFC) over 16 months was selected. The Structured Inventory of Malingered Symptomatology (SIMS) was administered to them, while assessing certain clinical indicators of malingering and other psychometric results. A descriptive statistical analysis of the sample was performed, focusing on the correlations between clinical and psychometric suspicion, and on specific vs. generic test sensitivity.
ResultsThe structured clinical criterion to detect malingering correlates moderately with the result obtained in the SIMS; the total score in this test presents a positive, albeit attenuated, correlation with the exaggeration indicators from the main psychopathology test; malingering is a highly prevalent response style in subjects seeking work-related sickness compensation, with a pattern of significantly increased responses compared to that observed in criminal samples.
DiscussionThe assessment of malingered psychological symptoms in the forensic context requires a multi-method strategy that includes structured clinical diagnosis, specific detection instruments, and other complementary psychometric tests, in order to generate convergent validity that contributes to the detection of this phenomenon.
La simulación, definida como intento deliberado de mentir o engañar en relación con una enfermedad o discapacidad, exagerando la sintomatología, con el objetivo de obtener un beneficio personal, es un fenómeno complejo, poco estudiado en nuestro contexto profesional. El objetivo de este estudio fue analizar el modo en que se manifiesta dicho fenómeno en el ámbito forense.
Material y métodosSe seleccionó una muestra incidental de 190 sujetos atendidos en la Unidad de Psicología (IMLCFC) durante 16 meses. Se les administró el Inventario Estructurado de Simulación de Síntomas (SIMS), a la vez que se valoraban ciertos indicadores clínicos de simulación y otros resultados psicométricos. Se realizó un análisis estadístico descriptivo de la muestra, así como de las correlaciones entre sospecha clínica y psicométrica, y entre sensibilidad del instrumento específico y de los instrumentos genéricos.
ResultadosEl criterio clínico estructurado para detectar la simulación correlaciona moderadamente con el resultado obtenido en el SIMS; la puntuación total en esta prueba presenta una correlación positiva, aunque atenuada, con los indicadores de exageración del principal test de psicopatología; la simulación es un estilo de respuesta altamente prevalente en sujetos de la jurisdicción social, con un patrón de respuestas significativamente incrementado respecto al observado en muestras penales.
ConclusiónLa valoración de la simulación de síntomas psicológicos en el contexto forense requiere de una estrategia multimétodo que incluya el juicio clínico estructurado, instrumentos específicos de detección, y otras pruebas psicométricas complementarias, al efecto de generar validez convergente que contribuya a la detección de dicho fenómeno.
Etymologically, the word “simulation” stems from the Latin simulare: representing something, pretending or imitating something that it is not.1 It is described in the fifth edition of the Diagnostic and Statistical Manual of Mental Disorders (DSM-5)2 as the “representation of false or highly exaggerated physical or psychological symptoms, motivated by external incentives, such as avoiding military conscription or work, obtaining an economic reward, avoiding criminal responsibilities or to obtain drugs”. This is a complex phenomenon that was studied relatively little in our national context until a few years ago, and it has forensic, judicial, medical, administrative, socioeconomic and even ethical and moral implications.
The conceptualisation of simulation included in the DSM-5 has been criticised (González Ordi et al.3) based on certain limitations: it is a one-dimensional category definition of the phenomenon; the manifestation of simulation is not restricted to medical-legal contexts; it involves a certain degree of inference and subjectivity in the evaluation process, and no operational criteria are supplied for how to obtain evidence; there is insufficient empirical support for the correlation between an antisocial personality disorder and the suspicion of simulation, and the combination of criteria proposed lacks sufficient predictive validity.
The International Classification of Diseases (ICD-10)4 does not consider simulation to be a mental disorder, and it includes it in the chapter entitled Factors that influence the state of health and contact with health services, defining it as “a person who pretends to be ill (with clear motivation)”. In our case we have opted to underline the following definition5: “deliberately trying to lie or deceive in connection with a disease or disability, exaggerating its symptoms, with the aim of obtaining a personal benefit, which is generally economic in nature, or which leads to being freed from duties and obligations”.
There is a certain degree of heterogeneity in connection with the statistical prevalence of this phenomenon in the figures that are supplied. A classical reference is that by Mittenberg et al.,6 whose study indicated a rate of incidence of from 8% to 30% in neuropsychological evaluation contexts in the U.S.A., where its upper limit corresponded to evaluations for professional disability. In forensic samples Rogers et al.7 give an average estimated rate of 17.4%. Respecting the diseases which are simulated the most often, the said authors give figures of from 30% to 40% for mild cranioencephalic trauma, fibromyalgia and chronic fatigue syndrome, somatomorphic disorders and pathological processes associated with pain. In a recent national study, Capilla et al.8 recorded that the most simulated diseases in medical-legal contexts were associated with chronic pain (45%-60%) and affective disorders (anxiety and depression, 50%).
Regarding the explanatory variables, Widows and Smith9 mentioned certain socioecological factors as “favouring” simulating behaviour, together with certain personal and circumstantial variables in connection with the individual. The adaptive model proposed by Rogers10 would be the one that best enables comprehension of the phenomenon: it considers simulation to be the result of rational cost-benefit analysis and an individual coping strategy when faced with adverse external circumstances.
Our study aims to analyse how the simulation of psychological symptoms manifests in the forensic context. Its specific objectives are, on the one hand, to study which differential descriptive characteristics characterise the population of subjects of simulators vs non-simulators in our forensic environment, and on the other hand, to evaluate the utility of clinical criteria as well as the available psychometric instruments in detecting and quantifying simulation.
Material and methodsA random sample was selected of 190 subjects seen in the Psychology Unit of the Medical-Forensic Clinic of the IMLCFC over a period of 16 months. These cases had been referred by forensic doctors and judicial authorities within the district of Catalonia (penal authorities, 57.37%; social authorities, 37.37%; civil authorities, 2.63%; cases against the state, 2.63%), for clinical and psychometric assessments.
Exclusion criteria were defined prior to selecting the definitive sample: age under 18 years or above 75 years, illiteracy, relevant difficulties in the written and verbal comprehension of the Spanish language, intellectual disability, disabling psychological symptoms or moderate to severe cognitive deterioration.
To select certain subgroups of interest, the following sequential protocol was applied to all of the subjects: 1) analysis of the available medical and psychological documentation; 2) anamnesis; 3) psychopathological examination of the subject; 4) initial classification as a malingerer or non-malingerer according to the structured clinical judgement of the professional, depending on the concurrence of 2 or more of the following criteria, adapted from Slick, Sherman and Iverson11: the presence of an external incentive which the subject himself could identify; the role of the person to be evaluated as a plaintiff or litigant; discrepancy between the severity of the accredited disease and the alleged degree of discomfort or dysfunction; discrepancy between the type of disease and the symptoms described; alleged symptoms, involvement or dysfunction in the absence of known psychopathological antecedents; 5) the detection of limited intellectual capacity and/or slight or slight to moderate cognitive deterioration; 6) administration of the Structured Inventory of Malingered Symptoms (SIMS)9; and 7) administration of complementary psychometric personality and psychopathological tests: the Millon Clinical Multiaxial Inventory (MCMI-III)12 and the Symptom 90 checklist (SCL-90-R).13
The SIMS is a self-reporting test with 75 items with a dichotomic response (T/F), designed as screening to detect the simulation of psychopathological and neurocognitive symptoms. This gives a total score and 5 partial scores on the scales of Psychosis, neurological deterioration (Dn), amnesiac disorders (Am), low intelligence and affective disorders. The MCMI-III and SCL-90-R were used as generic instruments for comparison; the first is a test designed for the clinical population and is composed of 175 items with a dichotomic response (T/F). This gives a profile with scores on 4 control scales (including, Sincerity [X] and Devaluation [Z]), 14 for personality dimensions and 10 for clinical syndromes. The second one is a list of 90 self-reported items on a Likert-type scale (0-4) which gives scores for 3 general discomfort indicators (these include the positive symptoms total [PST]) and 9 psychopathological symptomatic dimensions. The psychometric properties of these instruments may be consulted in their reference manuals.9,12,13
Given that the sample was random and not controlled a priori, as well as the needs and limitations intrinsic to expert intervention in the context of public forensic medicine, not all of the subjects could be subjected to the same protocol of complementary psychometric tests; the effective administration of the SIMS was the minimum indispensible criterion for inclusion in the study sample. The sizes of the different subgroups were: SIMS (n = 190), SIMS and MCMI-III (n = 119), SIMS and SCL-90-R (n = 49).
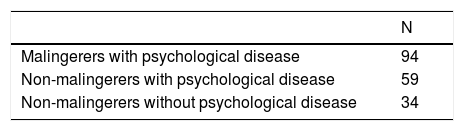
Due to the interest in studying the said variables in connection with the presence or absence of psychopathology in the subjects, the general sample was subdivided into 3 groups post hoc, distributed as shown in Table 1; malingering individuals with no disease were not included, given the low level of representativeness of the sample obtained (n = 3).
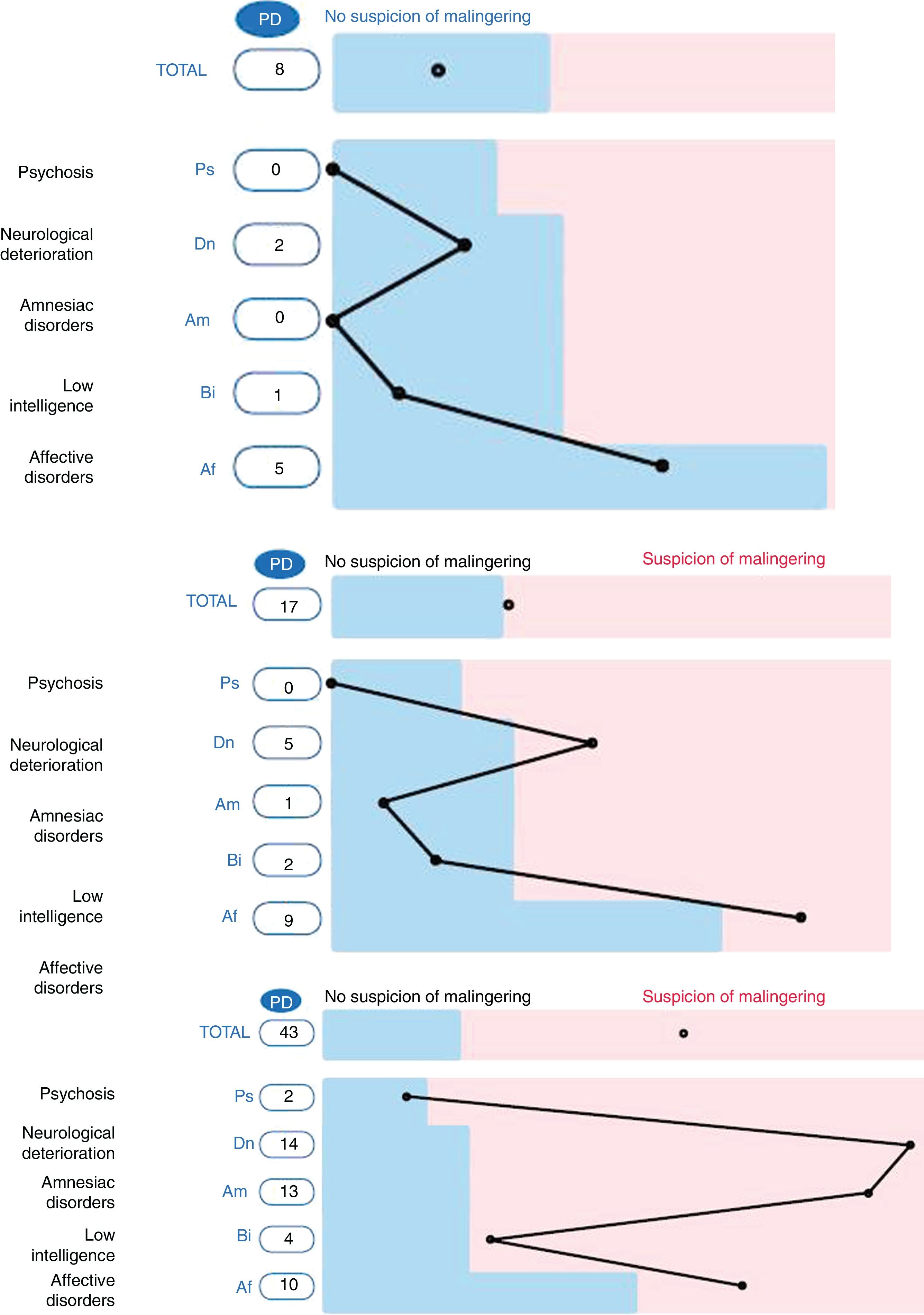
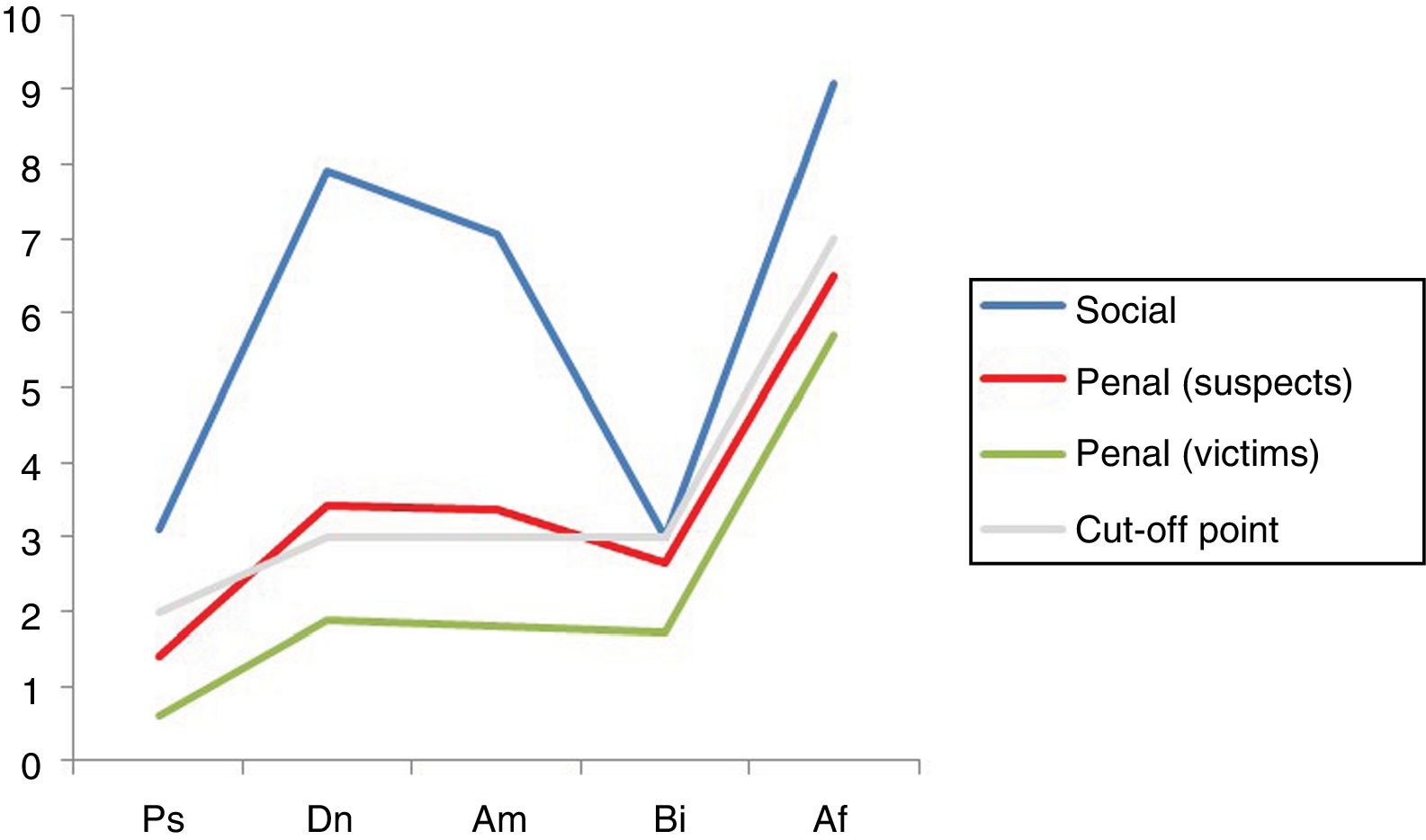
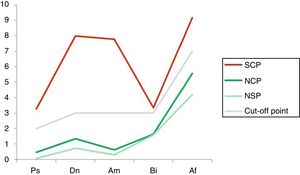
The criterion “malingerer/non-malingerer” was determined according to the total score obtained in the SIMS, in connection with the cut-off point suggested by the Spanish adapters of the instrument (PT > 16). Fig. 1 shows 3 examples of SIMS profiles, all extracted from the sample of social-professional jurisdiction subjects: without the suspicion of malingering (total score and scores on the scales below the cut-off point), possible malingering (total score slightly above the cut-off point and slightly raised on 2 scales) and very probable malingering (total score clearly above the cut-off point, and positive scores on 4 scales).
The criterion “with/without disease” was established on the basis of the documented accreditation of a personal history of psychopathological disorder/s, as well as according to the result of the clinical examination, following the protocol described above.
Statistical analysisData were processed in Excel spreadsheets. Descriptive statistical analysis was undertaken of the sample characteristics (age, sex, jurisdiction and psychopathology, etc.) together with the correlation (Spearman’sρ) between clinical and psychometric suspicion, between the sensitivity of the specific instrument and the generic instruments used. The Student t-test was used to compare quantitative variables between both study groups, and in the case of qualitative variables groups were compared using the Chi-squared test (χ2). A variance analysis was performed for the comparison of quantitative variables among more than 2 study groups. Statistical processing was carried out using version 14.0 of the Statistical Package for the Social Sciences (SPSS) program for Windows. The level of significance proposed was P < .05.
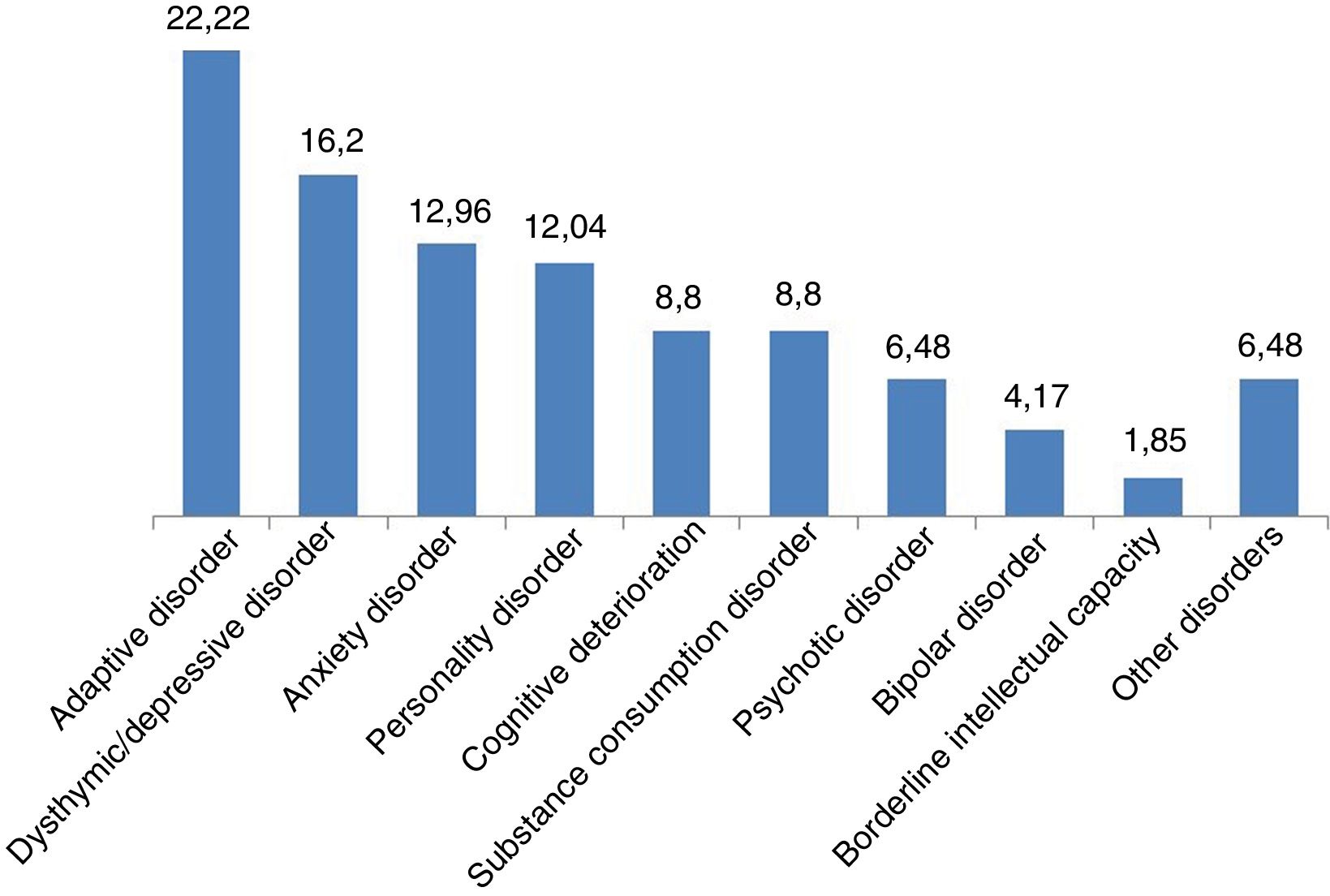
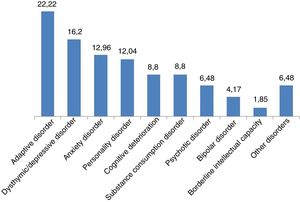
Results1) General description of the sample. 52.11% of the subjects were of the female sex. The age range was from 19 to 72 years, with an average of 40.87 (SD: 12.06) years, and the main age bands were those from 36 to 45 years (29.47%) and from 46 to 55 years (24.74%). More than half of the sample had terminated their primary education (55.26%), while the others had secondary education (22.11%), higher education (12.63%) or unfinished primary schooling (10%). Based on their judicial status they were mainly professional disability claimants (37.37%), victims (29.47%) and under investigation by penal law authorities (27.9%). 80.53% of the subjects had some type of psychopathological disorder (Fig. 2).
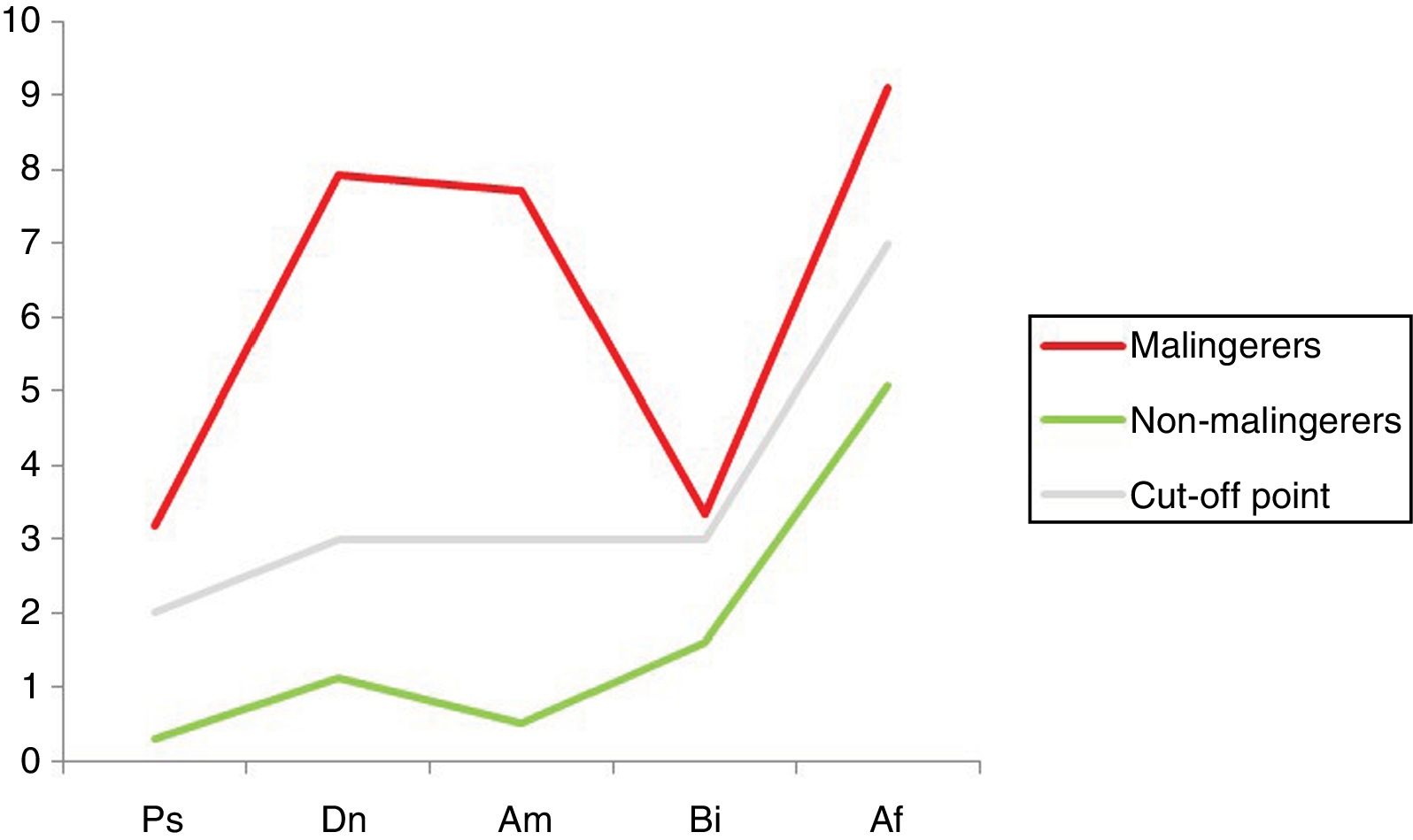
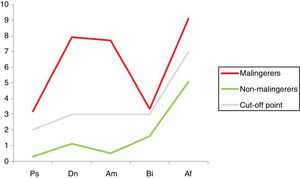
2) Results of the malingering test. Somewhat more than half of the total sample (51%) scored higher than the cut-off point in the SIMS (PT > 16), so that they were classified as malingerers. The majority of these subjects were men (54.95%). The total average SIMS score in this group was 31.28 (SD: 9.16), as opposed to 8.62 (SD: 4.14) in the non-malingering group (P < .001). Both groups are compared based on their scores in the five scales of the test in Fig. 3 (P < .001).
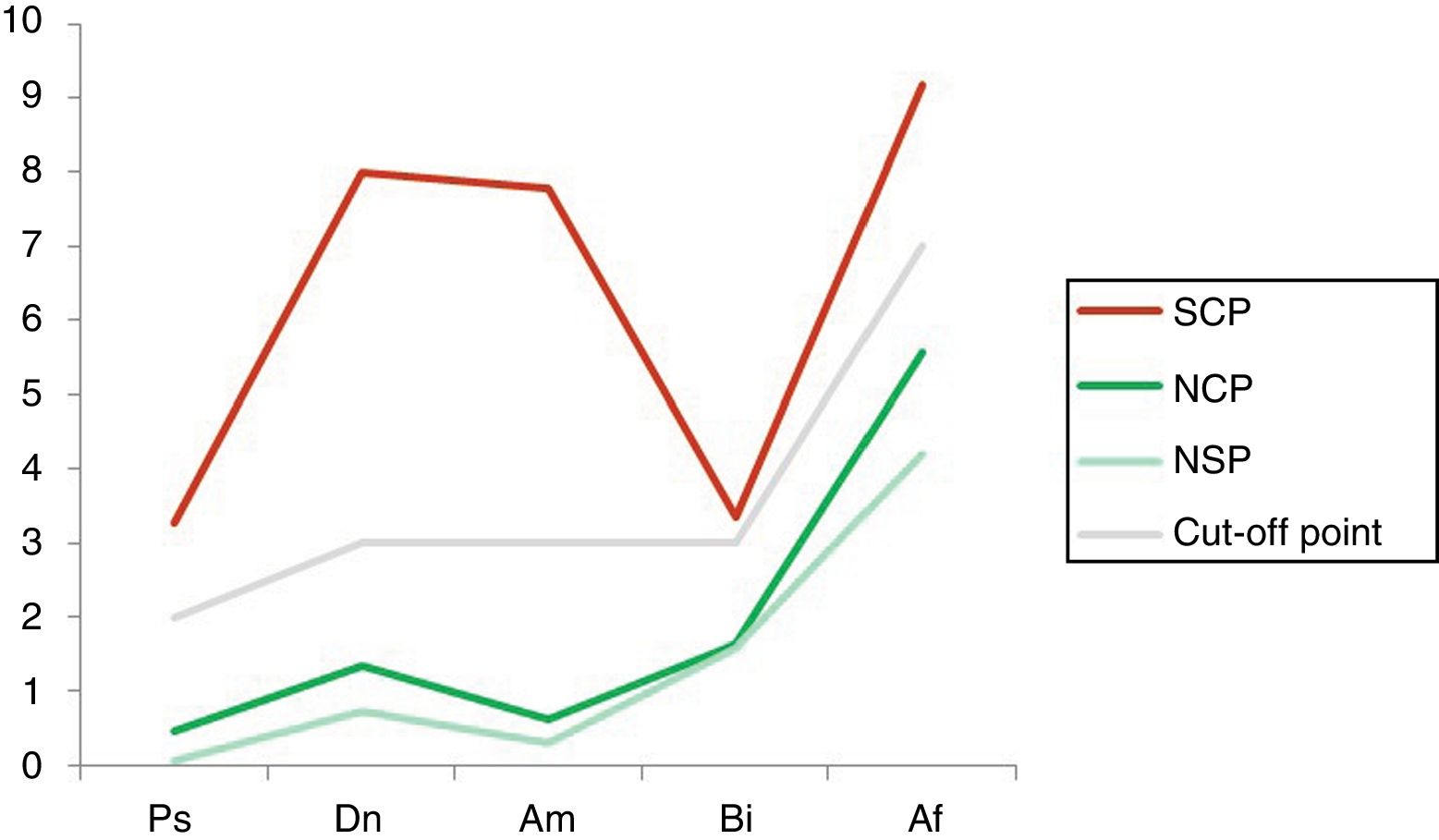
It can be seen that the Dn and Am scales are the ones that show the greatest divergence and therefore discriminatory power between the conditions of being a malingerer or non-malingerer. When the 3 subgroups obtained from crossing the “malingering” and “disease” criteria are compared, it is found that the subjects with psychological disorder/s obtained higher total SIMS scores than the disease-free group, regardless of whether or not they malingered. Fig. 4 shows the distribution of the scores of the 3 groups studied on the test scales (P < .001).
Average scores obtained in the SIMS scales in the 3 subgroups. Af: affective disorders; Am: amnesiac disorders; Bi: low intelligence; Dn: neurological deterioration; NCP: non-malingerers with disease; NSP: non-malingerers without disease; Ps: psychosis, SCP: malingerers with disease.
In connection with the clinical criterion, a correlation coefficient of 0.69 was obtained between suspicion of malingering in the clinical examination and a positive result in the SIMS; i.e., the detection of possible malingering by using subjective criteria in the interview was ratified by a complementary objective test in 69% of cases.
3) Comparison with generic psychometric tests. Comparing the sensitivity of a specific instrument for malingering with the MCMI-III control indicators, it was found that the Z scale Devaluation of the latter, which assesses the degree of symptom exaggeration (Z ≥ 75), had a correlation of 0.60 with the total SIMS score. The X scale for Sincerity would be less sensitive in detecting malingering. This is associated with a style of response indicative of openness or transparency (X ≥ 75), and this only correlated with half of the cases (0.50) with a positive SIMS score. Regarding the SCL-90-R, it was found that the indicator it includes to detect the exaggeration of symptoms (PST ≥ 50 in men and ≥ 60 in women) had a correlation index of 0.58 with a total positive score in the SIMS.
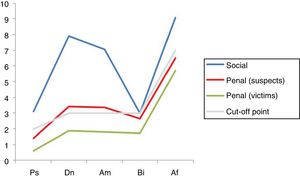
4) Results according to jurisdiction. An outstandingly higher presence of malingering was found in the subjects who claimed due to professional disability (86% of malingerers) than was the case for those involved in penal proceedings (42% in those under investigation —P < .001—, 21% in victims —P < .001—). The difference between those involved as suspects and the victims was also significant (P < .020). The average total scores in the SIMS were significantly higher in the professional jurisdiction group (30.15 points) respecting suspects and victims (17.32 and 11.73 points, respectively; P < .001). Fig. 5 shows the average distribution of scores in the 5 scales of the test for the 3 jurisdictional groups (P < .001).
DiscussionIn this study the SIMS scales that displayed the greatest discriminatory power between malingerers and non-malingerers were Dn and Am; the scale with the smallest discrepancy in average score between both conditions was Bi, in which, on the other hand, there was practically no difference between the groups with and without disease. Additionally, this scale is the only one that broke with the analogue pattern of scores in the malingering and non-malingering groups; once again the Bi scale showed almost zero discriminatory power between the subgroups with and without disease. The lesser discriminatory power of this scale is confirmed by other studies.14,15 On the other hand, Dn and Am are the scales which most broadly surpass the cut-off point for malingering.
It can be seen that the structured clinical criterion for detecting malingering correlates moderately with the SIMS result. The total score in the latter has a positive and significant correlation with the exaggeration indicators of the main generic test (MCMI-III), and more specifically with the Z scale. The correlation was also positive and significant in comparison of the SIMS with the PST indicator of the SCL-90-R. Malingering is a style of response that is highly prevalent in the sample of social jurisdiction subjects, with a pattern of replies in the SIMS that is significantly higher than is observed in the penal samples.
It is hard to supply data on the prevalence of malingering which could be used to compare with our study; we are not aware of any study in this respect in the Spanish judicial context based on samples extracted from different jurisdictions. Comparison with other countries may be distorted by the highly heterogeneous nature of judicial systems. In any case, we consider the data on basic rates of malingering supplied by Mittenberg et al.6 to be of interest: 30% in cases of professional disability or compensation, 29% in cases of injury assessment and 19% in criminal cases. Some authors have hypothesised that, in general, the possibility of obtaining an economic compensation would be more likely to lead to exaggeration of the symptoms, while cases in connection with criminal responsibility would be associated with a higher rate of symptom malingering.16
When our results are compared with those of previous studies, the work of adapting the SIMS to the Spanish population9 is an essential reference. The total average scores obtained in the said study were similar: 7.6 (SD: 3.6) in the control group (non-malingering) and 33.8 (SD: 12.0) in the experimental (malingering) group. These scores show a suitable degree of discriminatory capacity between the group with disease and the group of malingerers. As was the case in our study, the malingerers obtained notably higher scores in comparison with the group of non-malingerers, including those with disease, and this reinforces the hypothesis that the SIMS makes it possible to discriminate between cases with some type of genuine disorder and individuals who are malingering a disease. The total average scores in the malingering and non-malingering groups in our study are comparable to those obtained in other previous studies.15,17
Although the figures showing the average scores for the different SIMS scales have similar distributions, certain differences can be found. For example, the groups of non-malingerers (with and without disease) obtain closer scores in our study, while there is more difference between the scores for adapting the SIMS. This is basically because of the slightly higher pattern of scores in the clinical group (non-malingerers with disease). There is relative equidistance between the different average scores in the work for adapting the SIMS; on the other hand, in our study a notable divergence was found between the Dn and Am scales. An analogous pattern in the distribution of average scores in the SIMS scales is found in other studies on the detection of malingering in medical-legal contexts.18
With the alternative cut-off points proposed by the Spanish adapters, sensitivity/specificity indexes for Dn and Am are obtained (0.88/0.97 and 1.00/0.95, respectively), that would not differ significantly from the other scales. Nevertheless, in another interesting study which used a sample composed of patients diagnosed with mixed anxiety-depressive disorder and adaptive disorder18 (the most common diseases in our sample), the indicator scales were those which offered the greatest discriminatory power, only less than the total score.
In connection with the comparison between the SIMS and the MCMI-III, in the above-mentioned adaptation work,9 as was the case in our study, moderate levels of correlation were obtained (0.55) between the total SIMS score and the Z scale; when the profile is analysed according to subscales, Dn and Af had the best indexes (0.44 and 0.42, respectively). According to the said authors, these results would be along the same lines as those of other previous studies.16,19 These studies indicated that the MCMI-III was less effective in detecting symptom exaggeration, making it a less recommendable instrument than others (such as the MMPI-220) for use in forensic assessment contexts.
The utility of the SCL-90-R in detecting malingering has hardly been studied, perhaps because this scale is used less in the forensic field than other instruments. The classic work by Edens et al.21 found low to moderate positive correlations between the different SIMS scales and the Global Severity Index of the SCL-90-R, a different indicator from the PST analysed in our study. More specifically, the best correlation indexes are obtained in connection with the total score of the SIMS (0.52) and the Af subscale (0.49). While the Global severity index is informative respecting the degree of symptom severity reflected in the test, the PST would be an indicator that is specifically aimed at recording the degree of distortion (minimising or maximising symptoms) in the style of response.
Respecting the classificatory precision of the SIMS, unlike the clinical criterion here we are able to make use of the study by González Ordi et al.,14 which was based on a random sample and used expert judges to classify the subjects as probable malingerers or non-malingerers. They did so based on protocol-governed empirical criteria, in a similar way to the methodology used in our study. The sensitivity indicators showed that the SIMS was able to suitably detect 82% of the malingerers, while the specificity indicators made it possible to correctly exclude the 93% of participants who did not malinger, according to the clinical criterion; the said predictive validity values differ from the levels of agreement between clinical and psychometric efficacy far more moderately in our work, although it should be pointed out that their study had a small sample size (n = 14).
Regarding the limitations of our study, we have to say that the fact of using a random sample, and therefore one that was not controlled, does not make it possible to learn the real rate of prevalence of malingering within the forensic context, and that this datum would be of great interest; for this, it would be necessary to select a representative sample of the said population and subject it to systematic screening for this condition. On the other hand, it would be essential to have a broad sample of malingerers together with the corresponding control group. Additionally, an optimum approach would have to be based on a prospective empirical design, and our study was undertaken by applying a retrospective analysis to accumulated data.
We believe it to be appropriate to propose future lines of research: 1) to analyse the degree of sensitivity and specificity of the SIMS in a population with real psychopathology; 2) to study the marginal suppositions in which using the SIMS gives rise to false positives and false negatives; and 3) to methodologically refine the differentiation between overlapping response styles that involve symptom exaggeration rather than malingering, based on its conscious and deliberate nature and its links with a possible psychopathological basis.
The detection of psychological symptom malingering in the forensic field requires a multiple method strategy which includes structured clinical judgement, specifically designed psychometric instruments and other habitually-used instruments such as the Personality Evaluation Inventory22 or the Minnesota Multiphasic Personality Inventory-Restructured.23 The aim would be to obtain the maximum amount of converging validity to guide the differential diagnosis of a condition with highly important implications for expert assessment as well as in terms of its judicial consequences, such as the potentially injurious “labelling” of the subject so classified.
To conclude, this study shows that the SIMS is a useful instrument for detecting the malingering of psychological symptoms at a forensic level, especially its scales for neurological deterioration and amnesiac disorders.
Conflict of interestsThe authors have no conflict of interests to declare.
We would like to thank Dr. Alexandre Xifró Collsamata for his invaluable contribution to the statistical analysis of data using the SPSS program.
Please cite this article as: López-Miquel J, Pujol-Robinat A. Análisis descriptivo de la simulación de síntomas psicológicos en una muestra forense. Rev Esp Med Legal. 2020. https://doi.org/10.1016/j.reml.2020.01.001
The original research on which this paper is based received a grant from the Centre d’Estudis Jurídics i Formació Especialitzada (Departament de Justícia, Generalitat de Catalunya) (see DOGC n.° 6033, 28.12.2011).