In accordance with parental legal duties, parents and guardians should be informed about health issues relevant to child health. Current Spanish legislation acknowledges autonomy from 16 years or emancipated minors. This study analyses the information given to the parents or legal guardians of minors over 14 years of age attending a tertiary-level general hospital emergency department on psychoactive substance intoxication (alcohol, cannabis, benzodiazepines).
Material and methodsThe medical records of minors treated in the emergency department of a tertiary-level hospital, between 2016 and 2017, were reviewed. A survey of medical and nursing professionals from the emergency services was also conducted.
ResultsOf the medical records that mentioned that the minor attended the emergency department with friends (11.5%), 5 (9.6%) did not specify if the parents or guardians were called. Of the 26 medical records (50%) in which there was no mention of whether if the minor attended alone or accompanied, 22 (42.3%) made no mention of informing parents. The study data show that 28 of the 35 respondents (80%) always notified if the minor had not been accompanied to the emergency department by a parent or guardian.
ConclusionsThere is lack of information relating to informing parents/guardians, as well as a discrepancy between the data provided by health professionals and the medical reports analysed.
El cumplimiento de los deberes de la patria potestad exige a los padres y/otutores estar informados de aquellos aspectos relevantes relacionados con la salud del menor. La legislación actual reconoce la autonomía a partir de los 16 años o menores emancipados. Eneste trabajo se analiza la información que reciben los padres o tutores legales de los menoresmayores de 14 años que acuden a un servicio de urgencias hospitalario general de tercer nivelpor intoxicación aguda por alcohol y otras drogas de abuso incluidos medicamentos como lasbenzodiacepinas si se consumen con fines recreativos.
Material y métodosSe revisaron las historias clínicas de los menores atendidos en el servicio deurgencias de un hospital de tercer nivel durante los años 2016 y 2017 para conocer la informaciónreferida a los padres y se entrevistó a los médicos y enfermeros de dicho servicio para conocerla información que daban a los padres/tutores.
ResultadosEn las historias clínicas en las que se citaba que el menor iba acompañado poramigos (11,5%), 5 de ellas (9,6%) no especificaban si se había realizado el aviso a padres/tutores.De las 26 historias clínicas (50%) en las que no había especificación del acompañamiento, en 22(42,3%) tampoco existía especificación del aviso. Mientras que 28 de los 35 encuestados (80%)afirma avisar siempre que el menor no hubiera ido acompañado por sus padres o tutores.
ConclusionesSe pone de manifiesto la existencia de una falta de información de tipo asistencialrelativa al aviso a padres/tutores, así como una discrepancia entre los datos proporcionadospor los médicos y enfermeros y los obtenidos en las historias clínicas.
Guardianship demands that the parents and/or tutors responsible for a minor are obliged to comply with the duty of care. For this they have to be informed about relevant circumstances for the health of the minor.1
The first version of Law 41/2002 stated that information was restricted to tutors or legal representatives for minors aged 12 years, while active listening by a professional is required for those older than 12 years, and if a minor is considered to be mature, their opinion may be taken into consideration.2,3 Nevertheless, the change to the laws protecting children and adolescents introduced by Organic Law 8/2015 of 22 July and Law 26/2015 of 28 July establishes the right of a minor to be heard, and sets 16 years as the “coming of age” when minors come into full legal authority without the need to grant consent by representation. This is also applied to emancipated minors under 16, and this therefore expresses the position of mature minors more clearly.4,5 I.e., a 16 year-old minor (or younger if emancipated) is able to understand the situation as explained to them and knows how to express their opinion in a way that may determine an action that they consider to be beneficial for their own well-being.6
Nevertheless, this decree contains exceptions to the above consideration, in which the said representation will be necessary:
- a)
An action with severe consequences for the health or life of the patient.
- b)
When the professional believes that the minor will not be able to make a decision or when their psychological or physical state does not allow them to, or because a judicial judgement confirms the said incapacity.
- c)
When the patient lacks the emotional or intellectual capacity for comprehension, as established by the definition of a mature minor.
Clinical symptoms of intoxication by alcohol or other drugs of abuse that requires treatment in an emergency department is in itself a situation involving objective risk for the health of a minor. It may be considered to be potentially serious depending on their age, the type of substance consumed, the amount consumed and the form of administration, so that the parents or tutors must be informed of this so that they can establish measures to help the minor in a possible situation of risk due to the consumption of such substances.
The basic characteristics of care in emergency departments are defined by a context in which the urgent need for treatment takes precedence over compliance with formal matters and clinical history (CH) content, where the priority is urgent care for the patient. Nevertheless, it must not be forgotten that it is vitally important to fill out the CH, not only from a medical point of view, but also in legal terms. This is because in conflictive situations, its content is an effective tool for resolving possible legal disputes.
The aim of this study is to how the parents/legal tutors of minors are informed by medical personnel in situations involving intoxication by psychoactive substances in a tertiary referral hospital emergency department.
Material and methodsA retrospective, observational and descriptive transversal study was performed, in which the histories of patients seen in the emergency department of a general tertiary hospital due to acute intoxication by psychoactive substances were reviewed. This study included all of the patients aged from 14 to 17 years inclusive who received medical care due to the said cause from January 2016 to December 2017. The SELENE hospital computer system was used to review and search for CH. The following variables were analysed: year, age, sex, specification of whether or not a minor was mature, accompanying individuals, information supplied to parents or tutors, and when this took place. All of these data were anonymised according to health data protection criteria.
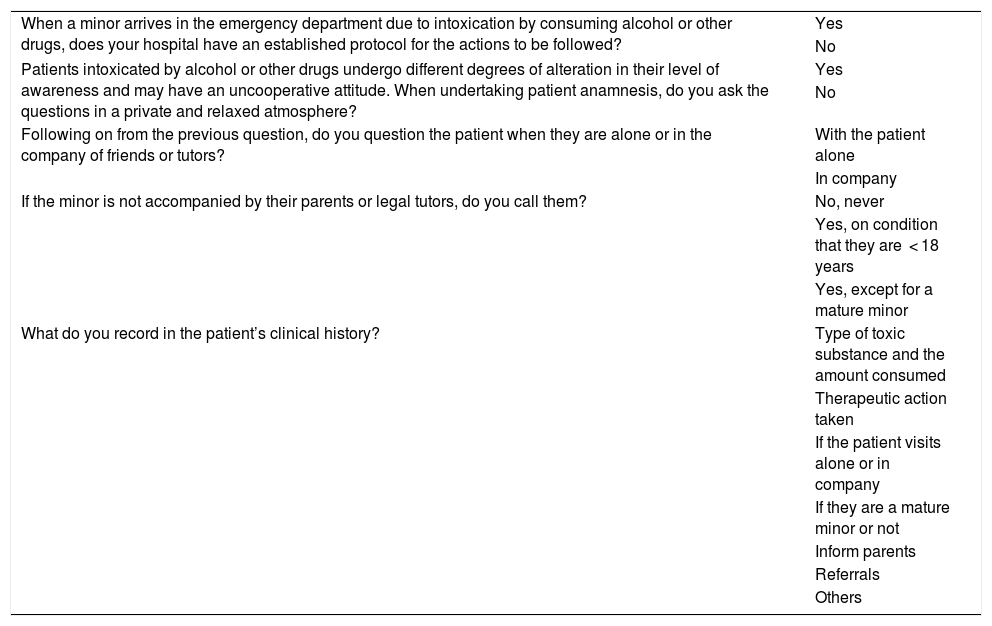
On the other hand, a prospective study was carried out using a questionnaire with closed questions. This was aimed at medical and nursing professionals in the said emergency department (Table 1), and a total number of 35 participants agreed to take part voluntarily.
Study questionnaire.
| When a minor arrives in the emergency department due to intoxication by consuming alcohol or other drugs, does your hospital have an established protocol for the actions to be followed? | Yes |
| No | |
| Patients intoxicated by alcohol or other drugs undergo different degrees of alteration in their level of awareness and may have an uncooperative attitude. When undertaking patient anamnesis, do you ask the questions in a private and relaxed atmosphere? | Yes |
| No | |
| Following on from the previous question, do you question the patient when they are alone or in the company of friends or tutors? | With the patient alone |
| In company | |
| If the minor is not accompanied by their parents or legal tutors, do you call them? | No, never |
| Yes, on condition that they are < 18 years | |
| Yes, except for a mature minor | |
| What do you record in the patient’s clinical history? | Type of toxic substance and the amount consumed |
| Therapeutic action taken | |
| If the patient visits alone or in company | |
| If they are a mature minor or not | |
| Inform parents | |
| Referrals | |
| Others |
Version 21.0 of the SPSS statistical package for Windows was used for statistical analysis of the data. This took the form of calculating averages, standard deviation and the Student T-test for the quantitative age variable, as well as the calculation of different correspondences, such as Pearson’s Chi-squared coefficient for the other qualitative variables.
ResultsOf a total of 4,173 minors aged from 14 to 17 years treated in the emergency department during the period studied, 52 were treated due to acute intoxication by psychoactive substances. 17 (32.7%) of these cases corresponded to the year 2016 and 35 (67.3%) corresponded to 2017. 90% of them were seen due to alcohol consumption, 8% for cannabis and 2% for benzodiazepines.
The average age was 15.58 years, with a standard deviation of 1.091. 21.2% (n = 11) of the patients were 14 years old; 25% (n = 13) were 15; 28.8% (n = 15) were 16 and the remaining 25% (n = 13) were aged 17 years old.
53.8% (n = 28) of the patients were male, and 46.2% (n = 24) were female. To check whether there were age differences according to sex (the average age of the males was 15.50 years, and for the females it was 15.67 years) the Student T-test for independent samples was applied. No statistically significant differences emerged in this respect (P > .05).
None of the data in the CH specified whether minors were mature or not.
50% of the CH did not state whether minors had visited the emergency department alone or accompanied. 11.5% specified that the minor had visited with a friend or friends, while in 36.5% of cases they were accompanied by family members. There was only one case which specified that the patient visited alone.
In 51.9% of the CH in which there was no reference to whether minors were accompanied or not by a family member, it was observed that nor was there any mention of contact with their parents or legal tutors. Only two CH specified this in connection with when they were informed.
No significant differences were found in the different variables (in company, informing parents or tutors) depending on the sex or age of the minors (P > .05).
The questionnaire applied to medical and nursing personnel in the emergency department was completed by 35 professionals, 74.3% of whom were medical staff and 25.7% were nurses. 51.4% (n = 18) were men and 48.6% (n = 17) were women. Regarding the number of years they had worked in the department, 34.3% (n = 12) had worked there for less than 2 years, 28.6% (n = 10) had worked there for from 2 to 10 years, and 37.1% (n = 13) had been working there for more than 10 years.
When they were asked whether there is a protocol governing action, 77.1% of those surveyed answered no, while 22.9% said that there is.
When they were asked whether the clinical interview with the patient took place in a private and relaxed atmosphere, 54.3% responded that it did. On the other hand, when they were asked if this interview took place with the patient alone or with company, 51.4% said that the patient was alone, while 48.6% said that they were in company.
In the cases in which minors visited in the company of their parents or legal tutors, 8.6% stated that they never called, 80% said that they always did so when they were under the age of 18 years, and 11.4% always called unless the minor were mature.
When they were asked what they included in the patient history, 97.12% of the respondents stated that they recorded the type of substance and the amount consumed. 94.2% recorded the therapeutic action taken, and informing the parents was marked by 74.28%.
No significant differences were found according to the profession, sex or years worked of the emergency department medical staff (P > .05) except for the question on whether they interviewed the patient in the presence of those accompanying them, or whether, on the contrary, they interviewed minors alone. 76.9% of the interviewees with more than 10 years experience interviewed and examined minors when alone with them. On the other hand, 75% of those who had been working in the department for a shorter time (less than 2 years) interviewed and examined minors in the presence of those accompanying them (Pearson’s chi-squared test 6.746; P = .034).
DiscussionNo previous studies were found in the literature with which to compare our data. In the questionnaire applied to emergency department doctors and nurses, 80% always called when a minor was not accompanied in their visit to the same by their parents or tutors. The others never called to report that the minor was in the emergency department, or they considered that if a minor were mature then this was sufficient reason not to call. This shows that the majority do inform parents or tutors of the assistance received by a minor and the reason for the same.
Some studies state that emergency department and primary care doctors say they lack sufficient knowledge about how to create a good doctor-patient relationship with minors, or how to act in areas connected with drug consumption, as they are unclear about the situations in which the principle of confidentiality and independence of the minor takes precedent.7,8 However, for the minors themselves confidentiality is one of the most important aspects of their medical care.7
The consumption of substances of abuse is a true public health problem, and it is necessary that those working in this field publicise the resulting risks and problems for the health of minors.9 It is more complex for emergency departments to evaluate minors in terms of acute or chronic psychoactive substance consumption. This is because relatively little is known about the patient, and they spend relatively little time in the department. Nevertheless, in cases of acute intoxication the principle of beneficence takes priority over independence, and therefore informing parents or tutors must be treated as a part of medical action. This action is protected by the law, which states that they are the representatives of the minor and may therefore establish the measures which are necessary to benefit them in a situation of risk due to exposure to and consumption of intoxicating substances.10
74.28% of the respondents stated that they record informing parents or legal tutors in the CH. Notwithstanding this, in the review of 52 clinical histories, 42.3% of the CH did not specify at all whether or not they were present, and nor do they specify if the parents were informed.
These data show that, although professionals state that they inform the parents or legal tutors and record this in the clinical history, a substantial percentage do not record whether the parents have been informed of the situation. Only one clinical history states that a minor visited alone and that their parents were informed of this, together with when this was done.
Medical professionals have the duty to prepare CH clearly and in an ordered way, showing all of the points in connection with the process of treating their patients. This is why the preparation of a good clinical history may vary depending on the department in question and the situation regarding emergency hospital admissions. The increasing demand by users and the resulting saturation of emergency departments may lead professionals to become overworked. This in turn may result in insufficient capacity for decision-making and a fall in the quality of medical actions, including the preparation of a correct clinical history.11,12
The discrepancy between the data obtained by medical professionals and the CH is notable, and moreover 77.1% of the respondents stated that there is no protocol which lists the aspects that must be considered when treating these cases and how to specify the same in clinical histories. This is also the case for the most relevant data, from who accompanies the patient when they visit and who must be informed according to current law. The differences found would not depend on the occupation of the professionals in question or their sex or number of years worked in the department, as no significant differences were found respecting these aspects. In one study the professionals did not consider the lack of a standardised protocol to be an obstacle against offering good quality care, although this was not the case for lack of time or an overload of work in medical attention.13 Nevertheless, clinical practice guides may be necessary for the medical professionals who deal with situations involving exposure to and the consumption of drugs of abuse by young people, so that they can approach them correctly.9
Attention in the emergency department requires care and organised attention that as well as being effective, also complies with the established legal framework. Compliance with the legal framework leads to higher levels of efficiency. However, compliance with legal obligations is often considered from a reductionist viewpoint, in which non-compliance is penalised and compliance does not give rise to the resolution of any conflict in care. On the contrary, it is fundamental that professionals understand compliance with legal obligations to be a tool that facilitates the clinical relationship and helps to improve medical attention.
We believe that positive education regarding compliance with ethical and legal aspects is important, thereby guaranteeing the attainment of the long-term objectives for improving care to which the majority of medical professionals are committed.
ConclusionsThe majority of the CH analysed contained few data about the process of informing the parents or legal tutors of minors treated for intoxication by psychoactive substances.
Although the majority of the professionals surveyed stated that they had informed the parents and/tutors, this was not recorded in the CH.
Correct action as defined by professional codes of ethics and current legal regulations is necessary, as doctors are obliged to know the said laws and to apply them.
Conflict of interestsThe authors have no conflict of interests to declare.
Please cite this article as: Esquiva AL, Romero MF, Rodríguez RG, Luna Maldonado A. Problemas de información a los padres y tutores en la asistencia a urgencias en menores de 14 a 17 años por consumo de sustancias psicoactivas. Rev Esp Med Legal. 2020. https://doi.org/10.1016/j.remle.2019.10.001