The objective demonstration of minor spinal and spinal-cord lesions following accidents is a classic discussion issue in both Clinical and Forensic Medicine. Particular problems are the patients with symptomatic spinal cord damage and normal neuroimaging. These situations are usually named with acronyms: SCIWORA (“spinal cord injury without radiographic abnormality”), SCIWNA (“apinal cord injury without neuroimaging abnormality”), and SCIWORET (“spinal cord injury without radiological evidence of trauma”).
Our purpose is to review the main clinical, radiological, and medico-legal features of these conditions, often unknown by those who are not used to treating spinal cord lesions. The main objective is focused on the medico-legal problems of these conditions. The results of our review places under question some aspects of the recent 35/2015 Spanish Law on accidents compensation, in particular when dealing with minor spinal injuries. Therefore, a review of the recent Spanish law's statements about spinal minor injuries compensation is required.
La objetivación de las lesiones espinales o medulares en accidentes es un tema clásico de discusión tanto en Medicina Asistencial como en Medicina Forense. Un problema particular son los pacientes con daño medular sintomático y neuroimagen normal. Estos casos se denominan con los acrónimos SCIWORA («spinal cord injury without radiographic abnormality»), SCIWNA («spinal cord injury without neuroimaging abnormality») y SCIWORET («spinal cord injury without radiologic evidence of trauma»).
Nuestro propósito es revisar los aspectos clínicos, radiológicos y médico-legales de estos cuadros, desconocidos muchas veces para quien no trata habitualmente lesionados medulares. El objetivo principal está centrado en los aspectos médico-legales de estos cuadros. Nuestros resultados cuestionan algunos aspectos del reciente sistema para la valoración de los daños y perjuicios causados a las personas en accidentes de circulación (Ley 35/2015), en los llamados traumatismos cervicales menores. En consecuencia, el tratamiento que la reciente legislación española da a dichos traumatismos podría necesitar ser revisada.
The absence of lesions on a plain radiograph and computed tomography in the presence of a patient with a neurological deficit of spinal cord origin is known as SCIWORA (spinal cord injury without radiographic abnormality).1–3
The concept was introduced by Pang and Wilberger in 19822; initially, it was conceived for paediatric cases, and, within these, for the cervical region. In children, the greater elasticity and mobility of the cervical rachis, along with the size and weight of the head, may cause cervical spinal cord damage without fractures or dislocations.
The identification of symptoms of this type in the adult population has given rise to the acronym SCIWORET (spinal cord injury without radiologic evidence of trauma) for adults, since many adults have spondylotic changes, thus they would exhibit radiological abnormalities and would not be included in SCIWORA.4
The advent of magnetic resonance imaging (MRI) has made it possible to demonstrate spinal cord lesions in patients with plain radiographs and normal CT scans. The vast majority (90%) of SCIWORA cases are spinal cord injury patients in which both tests (X-ray and CT) are negative, but the MRI scan is pathological. In the remaining cases of SCIWORA, approximately 10%,5 there are symptomatic spinal cord lesions with normal MRI6; i.e., they would be normal spinal-cord injury patients with normal X-ray, CT and MRI.
Accordingly, there is a strong case for restructuring the terminology, and speaking of SCIWORA in cases where neural damage is revealed in MRI, but the other tests are normal.7 If, in a case with clinical spinal cord damage, all imaging tests, including MRI, are normal, we would speak of SCIWNA, or “spinal cord injury without neuroimaging abnormality”8 (Table 1).
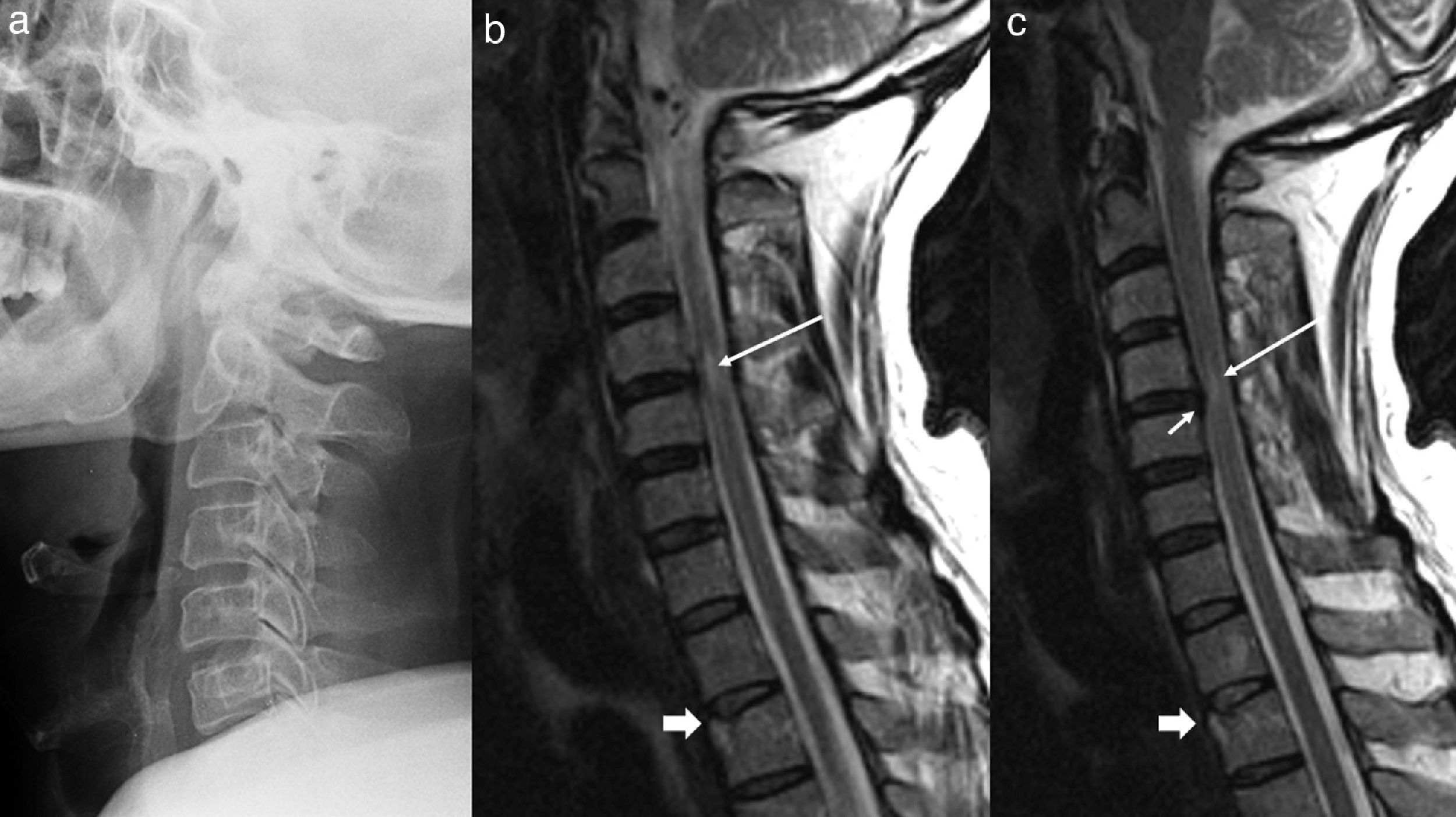
Presentations with symptomatology and normal neuroimaging.
| Acronym | Text | Meaning |
|---|---|---|
| SCIWORA | Spinal cord injury without radiographic abnormality | Admits MRI showing spinal cord damage, with normal X-ray and CT scans. |
| SCIWNA | Spinal cord injury without neuroimaging abnormality | Plain X-ray, CT and MRI scans normal, but there is clinical spinal cord damage |
| SCIWORET | Spinal cord injury without radiologic evidence of trauma | Admits pathological data in plain X-ray, CT and MRI scans, but not related to injury |
The basis of all these presentations is the disassociation between the clinical symptoms (symptoms or signs of neurological affectation) and radiology (Normal X-ray, CT, MRI). Apart from the clinical interest that this may hold, from the medico-legal perspective, the implications may be significant. Thus, Spanish Law 35/20159 establishes that a spinal injury in which the symptoms are based on pain, and the complementary tests are normal, must be considered a minor spinal injury. Injuries of this type only exceptionally give rise to sequelae; moreover, these are minor. In addition, they must only be compensated as temporary injuries. Consequently, there is a risk that certain SCIWORA or SCIWNA may be erroneously considered as minor spinal injuries, particularly if the symptoms or clinical examination data (which the law omits) are not carefully analysed.
This study attempts to review the matter, and to provide guidance for the proper diagnosis and assessment of such cases.
The literature has been reviewed, along with our Centre's experience in such cases.
We undertake a critical review of the published works to identify the current concepts on injuries of this type. The main medico-legal issues are reviewed, in particular those arising subsequent to the coming into force of Law 35/2015.
DiscussionAetiopathogenesisPang's original description mentions 4 causal mechanisms for these symptoms: flexion, hyperextension, longitudinal distraction and ischaemia.2 It is thought that the response is mainly to a hyperextension of the rachis, and, accordingly, it is normally seen in road accidents or in direct craniofacial trauma.7
In adults, one common characteristic is the existence of cervical spondylosis. In such cases, the presence of posterior discoarthritic bars, as well as the redundancy of ligaments owing to telescoping, may give rise to intramedullary damage, even after a slight hyperextension.10
Schneider et al.11 described a central cord syndrome in patients with a narrow canal who had suffered trauma owing to hyperextension. The typical presentation is that of a greater neurological deficit in the upper limbs compared to the lower ones.
A number of authors indicate another aetiological possibility, the traction of the spinal cord from the most distal roots or nerves, such as the sciatic or thoracic nerves, in flexion-extension mechanisms of the rachis.12,13 This cause is interesting, since one marker of the radicular stretching when the root is detached from its point of insertion (which is called avulsion) is arachnoid cysts in the radicular origin. These cysts are easily identifiable in MRI. Clinically, the avulsion sometimes produces small subarachnoid haemorrhages which result in spinal or radicular pain and meningeal syndrome (headache, neck pain and stiff neck).
Other possible causes are vascular, such as arterial dissection which would compromise the irrigation of the spinal cord. We have evaluated one case in which a post-traumatic lumbar-gluteal arteriovenous fistula conditioned a venous engorgement of the epidural venous system, with Foix-Alajouanine ischaemic myelopathies at D8 level owing to venous congestion.
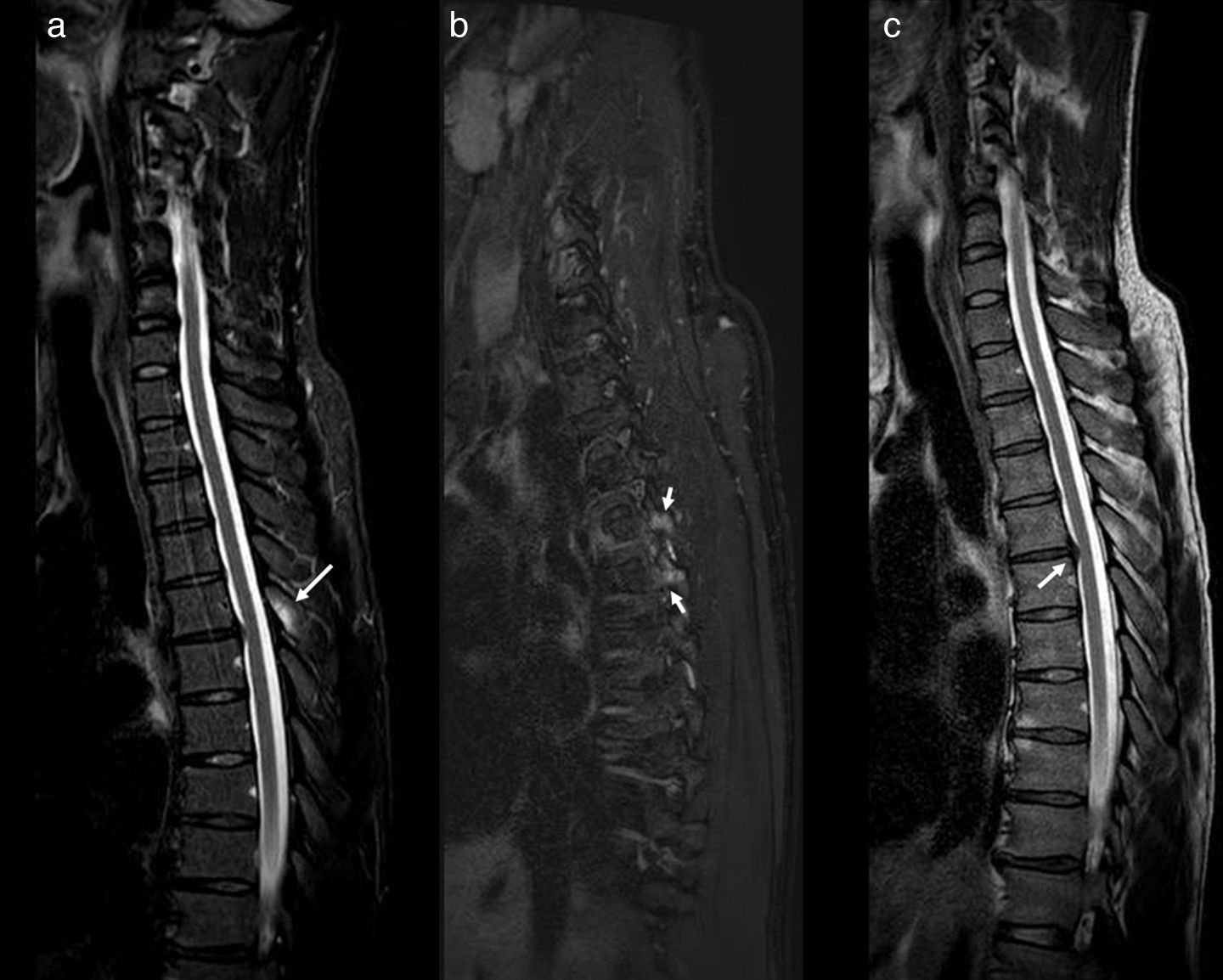
Clinical symptomsPatients with SCIWORA have a wide range of clinical manifestations, from mild, transitory symptoms or deficits (e.g. paraesthesia), to tetraparesis or tetraplegia. Some patients only experience symptoms at the time of trauma, while in others, the neurological deficits only become apparent some days later.1 One element of paramount importance is that large-scale traumas are not specified, since, particularly in adults, there may be cofactors (co-causes) which justify the spinal cord damage. For example, cervical arthrosis or canal stenosis (Fig. 1). This often violates the medico-legal criterion of proportionality. Another characteristic is that these patients do not always exhibit neurological symptoms, or these may be subtle or not expertly assessed. Consequently, they may erroneously be considered as minor cervical injuries (according to Law 35/2015).
MRI of cervical column with STIR sequences (a) and T2 (b and c) in sagittal planes. An inversion of the cervical lordosis with advanced degenerative disco-vertebral changes in C3 to C7 can be discerned (thick arrows in b) and a significant stenosis of the central canal at C4 and C5 level (arrows in b). In the STIR sequence, no bone marrow oedema is noted even in the soft tissue which may suggest an acute lesion (a). Nonetheless, in the T2 sequence, a hypersignal can be made out in the spinal cord at C4–C5 level (arrow in c), consistent with a spinal cord oedema (Kulkarni pattern II). Clinically: previous normality. Occipital pain and paraesthesia in all 4 limbs subsequent to abrupt hyperextension mechanisms. Upon examination: spastic tetraparesis and gait ataxia.
The most suitable diagnostic tool for these cases is MRI. It must include sequences such as: Spin-echo T1 (T1 SE), gradient-echo T2 (T2-weighted GRE) and STIR (short-term T1 inversion recovery).1
One important issue is that often the appropriate sequences are not carried out. In this regard, it has been reported that the STIR sequence is the most suitable for screening traumatic lesions in the rachis, since it saturates fat and boosts the signal in tissues with long relaxation times in T2, increasing sensitivity in the detection of bone marrow and soft tissue oedema. So much so that it has been singled out owing to its luminosity, in which lesions show up like light bulbs, being qualified as a “forensic sentinel sign”14 (Fig. 2). Numerous studies refer to the usefulness of this sequence as a way of screening in minor injuries,15–17 emphasising the value thereof for detecting lesions in ligaments which would otherwise go unnoticed.18 Consequently, one could say that an early MRI scan that does not include this sequence would be nothing short of invalid for forensic purposes, as acute lesions in soft tissue and ligaments may go unnoticed.
MRI of dorsal column with STIR sagittal sequences (a), Dixon T2FS (b) and T2 (c). Bone marrow oedema can be observed in the spinous process of D5 (arrow in a) and in the pedicles of D5 and D6 (arrows in b), without defining fracture lines. A central protrusion of the disc D5-D6 is shown (arrow in c).
Another MRI technique which may be useful–in this case for detecting spinal cord lesions–is spectroscopy. This has been proposed in patients with spondylotic myelopathies19 and chronic cervical strain.20 Despite the small number of cases, it has proved to be capable of revealing spinal cord lesions which go unnoticed in conventional MRI.
Other methods also demonstrate possibilities for relating incapacity in spondylotic myelopathies and MRI findings.21 The usefulness of sequences such as diffusion (diffusion weighted imaging [DWI]) has been described, highlighting the fact that in patients with normal MRI, the DWI may reveal traumatic lesions in soft tissue.22
Magnetic resonance transfer (MRT) would seem to characterise the integrity of white matter, which may help to establish a prognosis.23 It has been indicated that this may be of use in cervical strain to identify spinal cord lesions which would otherwise go unnoticed.24 Nonetheless, these systems (DWI and MRT) have yet to be completely validated and may give rise to false positives.25
The most extensive classification for spinal cord injuries in MRI is that of Kulkarni et al.26: Pattern I (haemorrhage), extensive central area of hypointensity surrounded by a fine border of hyperintensity in T2 sequences. Pattern II (oedema): area of hyperintensity in T2. Pattern III (spinal cord contusion), thin central area of hypointensity surrounded by a thick border of hyperintensity in T2 sequences. In cases of cervical injury, the use of this terminology is recommended, since it allows the clarification of issues of medico-legal and healthcare interest, such as the data or extent of the injury. Reports on these cases do not always include this classification.
It is also possible for the initial MRI to be normal or unspecific and, if a check-up is performed some time later, for signs of spinal cord damage to be found.27 This correlates directly with the chronological medico-legal criterion, owing to which caution must be exercised in terms of the limit set by Law 35/2015 with regard to cervical injuries (72h).
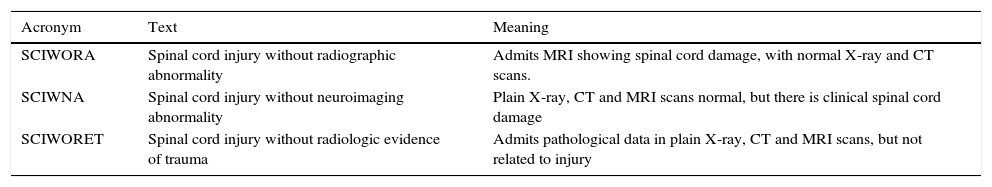
On occasion, the MRI of the affected region may be normal, but there may be remote lesions in the rachis, which act as markers of the mechanism of injury (Fig. 3). If these regions are not included in the MRI, this may be normal. Thus, it is advisable for the study to include an extensive area of the rachis believed to be affected, or at times more than one region, as there is also the problem of non-contiguous lesions.28
Lateral radiograph of the cervical column (a) and MRI of the cervical column with weighted sagittal sequences in T1 (b) and T2 (c). In the lateral radiograph, only a straightening of the lordosis can be observed. The MRI images show an irregularity and alteration in the signal for the upper D2 disc, consistent with a compression fracture (thick arrows in b and c). A small central protrusion can be observed at C4–C5 level (arrow in c), which associates a slight reduction in the canal and an area of spinal cord oedema (long arrows in b and c).
On occasion, information on the diagnosis is provided by the joint analysis of a number of tests. For example, CT may be useful for providing information on the previous state, and MRI on the latter and the acute repercussions thereof (Fig. 4).
Sagittal reconstruction of cervical CT (a) and STIR sequence of MRI (b) on sagittal planes. The patient exhibited an initial tetraparesis from which he recovered within a few hours. The image shows a posterior osteophyte C6–C7 (a), as well as an image of hypertrophy of the posterior longitudinal ligament at the same level. This previous state could probably have caused a spinal cord shock.
When the imaging tests are normal, physical examination and evoked potentials are the best way of focusing on the spinal cord injury.29 Nonetheless, as we shall go on to see, they may have false positives and negatives.
Medico-legal issuesWe shall now focus on the issue of damage assessment in light of the current Spanish legislation.
Article 135 of Law 35/2015 establishes that minor cervical injuries (MCI) “are diagnosed on the basis of the expression of the existence of pain in the injured party. They are not susceptible to verification by means of complementary medical tests”.
This wording may cause problems in relation to the symptoms analysed herein. On one hand, many of these patients feel no pain, since the manifestations are neurological and they may be scantly expressive (paraesthesia, weakness of limbs, alterations in sensitivity, in gait, dizziness, etc.). The wording seems to make it clear that if the individual has symptoms other than pain, we are no longer dealing with a minor injury, owing to which in such cases, the absence of pain may not be interpreted as an exclusion criterion for cervical injury in general, but instead only for minor cervical injury. In other words, all cases with non-painful symptoms (or signs) will go on to swell the ranks of the group of spinal cord injuries other than MCI. This opens the way for these cases not to be compensated only as temporary injuries, and also for a broader spectrum of sequelae (those for MCI are severely restricted in the Law and, in addition, require a detailed report if they are to be taken into account).
Another issue is the condition established by the Law in the sense that an MCI is not susceptible to be demonstrated by means of complementary tests. More specifically, SCIWORA and SCIWNA, have normal radiological tests, and may thus fall into the category of MCI, despite the presence of neurological damage. Especially if the patient asserts that he/she only feels pain and no neurological abnormalities are discovered in the examination.
A specific problem could derive from standard symptoms. In these cases, the neuroimaging may be markedly pathological, but there may be no evidence of a traumatic origin for this abnormality. This is extremely common. We only need to think of cases with arthrosis, rigid vertebral masses or canal stenosis. Since Law 35/2015 requires normality in the complementary tests, these cases will make it necessary, on one hand, to give an opinion on the meaning of these findings in the injury. Some of these, even if they are degenerative, may have played a key role in the spinal cord damage. Rigid masses are known to have severe mechanical effects in the adjacent mobile discs, tending towards those conducive to myelopathy at these levels. Neurological deficits have been described after minimal injuries.30,31
That is to say that the classification of a case as SCIWORET does not prejudge the non-existence of traumatic effects on the spinal cord owing to, for example, a previous state. In these cases, a highly detailed analysis of causality and co-causality is required, along with a precise understanding of the meaning of the radiological terms which may appear in the neuroimaging reports.
Thus, we need to be aware of the existence of these presentations and to fine tune the neurological clinical examination. This requires training for those treating or assessing these patients. The neurological examination is difficult and requires experience. At times, the appearance of “soft signs” in the examination (e.g. concealed pyramidal syndrome, a hypopallesthesia, a nystagmus, spine-related gait disorder, suspended anaesthesia, etc.) requires experience in the examination and treatment of neurological patients. This does not always occur in emergency department bays or in physical injury assessment units.
On the other hand, the MRI needs to be assessed appropriately, since, as we have already seen, spinal cord damage is only evident in certain sequences. It must be ensured that the MRI study includes sequences with fat saturation, such as STIR, before ruling out any possible neurological damage.
Article 155 itself establishes that minor cervical injuries are compensated as temporary injuries, provided that the nature of the injurious act may give rise to the damage in accordance with the following generic causality criteria:
- -
Chronological, which consists of the symptomatology appearing within a medically explicable period. In particular, it is especially relevant for the purposes of this criterion that the symptoms appear within 72h after the accident, or that the injured party receive medical care within this period.
- -
Of intensity, which consists of matching the injury suffered and the mechanism through which it came about, taking into account the intensity of the accident and all other variables which may affect the probability of its existence.
This wording implies two additional problems. On one hand, it is known that in cases of SCIWORA the onset of symptoms may be delayed, from a few minutes up to 48h in around 50% of patients. But symptom-free intervals of up to 7 days have been reported.32
This symptom-free period has been related to repeated spinal cord injuries against unstable vertebrae,1 although it may also have other origins, such as vascular (dissections, secondary ischaemic changes, etc.).
Consequently, this temporal criterion must be treated with extreme caution. Even the limit of 72h, which Law 35/2015 establishes for considering a cause–effect relationship, may be questionable.
The possibility of detecting neurological damage in a SCIWORA by means of evoked potentials has been proposed as the best option. Nonetheless, this technique is not free of false negatives. In an extensive series of intra-operative spinal surgery monitoring, rates of 0.36% (45 cases) were reported for patients in whom the neurological damage was not shown by the evoked potentials.33 False negatives with transcranial magnetic stimulation have also been published.34 In continuous monitoring during surgical interventions, sensitivity was 89%,35 but the sensitivity for an isolated (non-continuous) test could be even lower.
It should also be pointed out that the modality of the potential may give rise to false negatives. Thus, if only the motor potential is examined, we are testing the motor pathways which are situated in the anterolateral part of the spinal cord. On the other hand, the somatosensory evoked potentials examine the spinal cord pathways, which are mainly posterior. In this way, one of these modalities may be negative, and if the other is not performed, it will not be possible to ensure the indemnity of the spinal cord as a whole.
ConclusionsIn healthcare, but above all, medico-legal settings, extreme care must be taken when assessing cervical injuries, particularly in symptomatic patients, presenting either with pain or any other symptom.
The points of Law 35/2015 in relation to cervical injuries must be interpreted flexibly, since, otherwise, serious errors can be made in the assessment of the damage in these cases. Specifically, the existence of presentations such as SCIWORA, SCIWORET and SCIWNA implies that the normality of neuroimaging tests does not exclude the possibility of spinal cord damage.
Likewise, these presentations call into question the criteria of proportionality and chronology that Law 35/2015 demands as a prerequisite in order to assess a spinal cord injury, with both causality criteria having to be interpreted flexibly and adapted to the case in question.
In these cases, neurophysiological tests, and more specifically evoked potentials, can give rise to false negatives, owing to which they must be performed comprehensively and interpreted with caution. The normality of the tests does not exclude the presence of spinal cord damage after a spinal cord injury, even one of low energy.
In these cases, a suitable and detailed anamnesis–including the investigation of symptoms or signs of a previous state, as well as an expert and detailed neurological examination–appears to be the best way of detecting spinal cord damage, of guiding the examinations and, in short, of correctly assessing a patient with a cervical injury.
Once again, and in spite of the fact that Law 35/2015 seems to have overlooked it, by placing the entire burden of proof on complementary tests, the axiom that “in Medicine, clinical symptoms are first and foremost” emerges as the element of greatest value in these cases.
Conflicts of interestThe authors declare that they have no conflicts of interest.
Please cite this article as: Aso Escario J, Sebastián Sebastián C, Aso Vizán A, Martínez Quiñones JV, Consolini F, Arregui Calvo R. Lesión medular con normalidad radiológica. Etiología, diagnóstico y problemática médico-legal. Rev Esp Med Legal. 2017;43:155–161.