Article

Revista Española de Medicina Nuclear e Imagen Molecular (English Edition)
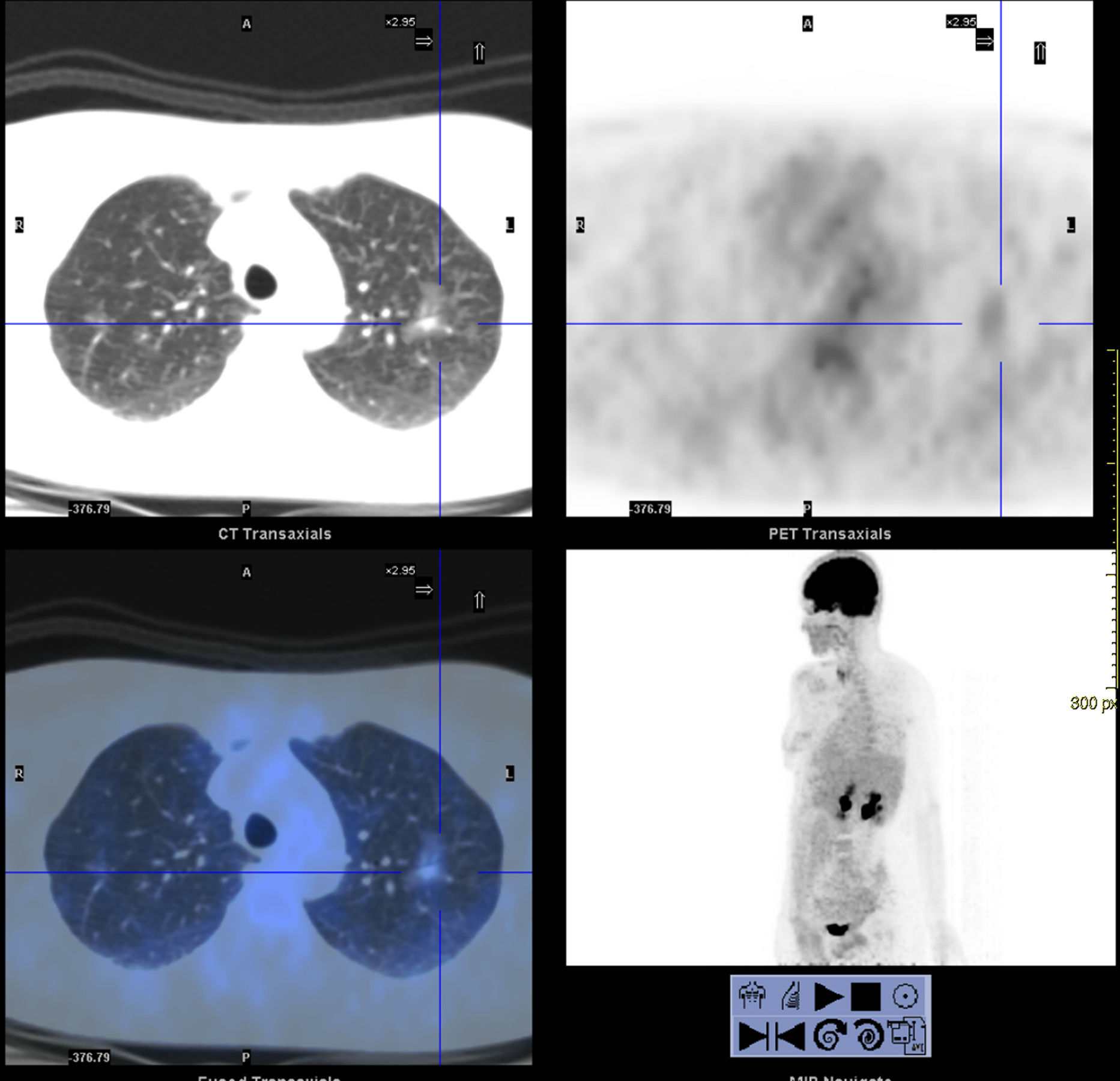
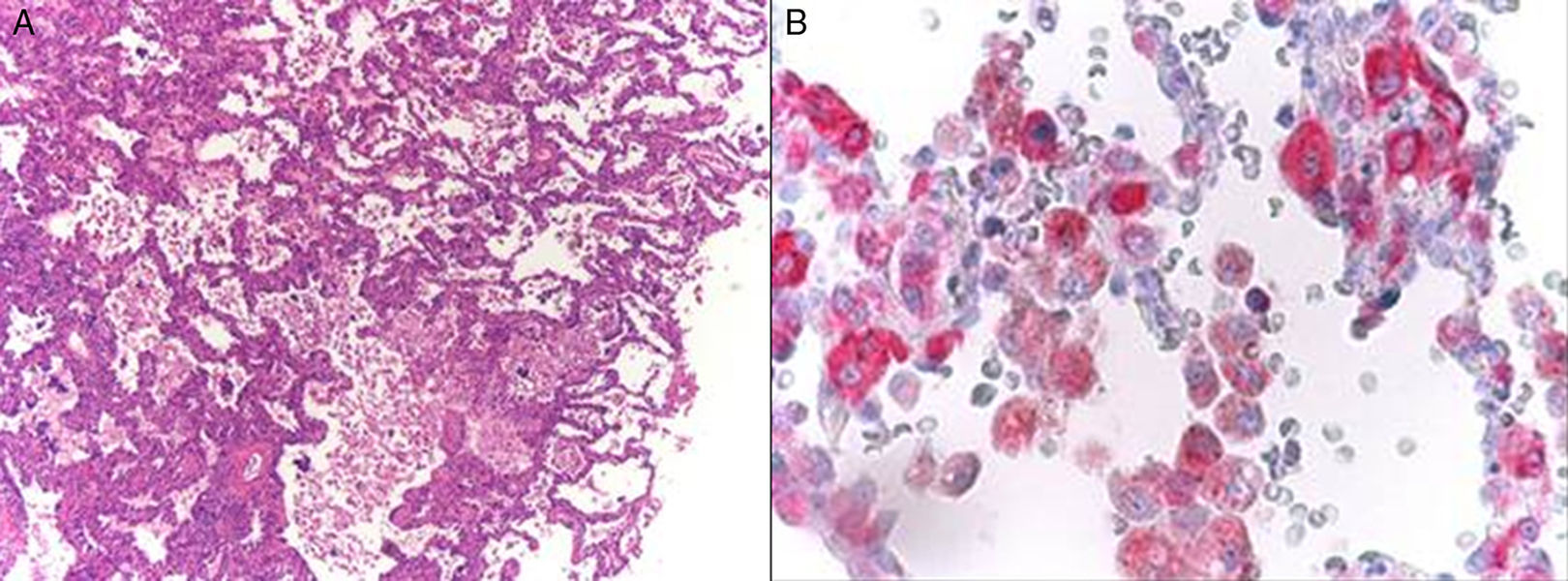
array:23 [ "pii" => "S2253808915001007" "issn" => "22538089" "doi" => "10.1016/j.remnie.2015.10.004" "estado" => "S300" "fechaPublicacion" => "2015-11-01" "aid" => "700" "copyright" => "Elsevier España, S.L.U. and SEMNIM" "copyrightAnyo" => "2015" "documento" => "article" "crossmark" => 1 "subdocumento" => "sco" "cita" => "Rev Esp Med Nucl Imagen Mol. 2015;34:390-2" "abierto" => array:3 [ "ES" => false "ES2" => false "LATM" => false ] "gratuito" => false "lecturas" => array:2 [ "total" => 61 "formatos" => array:2 [ "HTML" => 15 "PDF" => 46 ] ] "itemSiguiente" => array:18 [ "pii" => "S2253808915000968" "issn" => "22538089" "doi" => "10.1016/j.remnie.2015.10.001" "estado" => "S300" "fechaPublicacion" => "2015-11-01" "aid" => "681" "copyright" => "Elsevier España, S.L.U. and SEMNIM" "documento" => "article" "crossmark" => 1 "subdocumento" => "sco" "cita" => "Rev Esp Med Nucl Imagen Mol. 2015;34:393-5" "abierto" => array:3 [ "ES" => false "ES2" => false "LATM" => false ] "gratuito" => false "lecturas" => array:2 [ "total" => 95 "formatos" => array:2 [ "HTML" => 72 "PDF" => 23 ] ] "en" => array:11 [ "idiomaDefecto" => true "cabecera" => "<span class="elsevierStyleTextfn">Interesting image</span>" "titulo" => "Pulmonary epithelioid hemangioendothelioma: Nuclear medicine and <span class="elsevierStyleSup">18</span>F-FDG PET/CT findings" "tienePdf" => "en" "tieneTextoCompleto" => "en" "paginas" => array:1 [ 0 => array:2 [ "paginaInicial" => "393" "paginaFinal" => "395" ] ] "titulosAlternativos" => array:1 [ "es" => array:1 [ "titulo" => "Hemangioendotelioma epitelioide pulmonar: Medicina Nuclear y hallazgos de <span class="elsevierStyleSup">18</span>F-FDG PET/TC" ] ] "contieneTextoCompleto" => array:1 [ "en" => true ] "contienePdf" => array:1 [ "en" => true ] "resumenGrafico" => array:2 [ "original" => 0 "multimedia" => array:7 [ "identificador" => "fig0005" "etiqueta" => "Fig. 1" "tipo" => "MULTIMEDIAFIGURA" "mostrarFloat" => true "mostrarDisplay" => false "figura" => array:1 [ 0 => array:4 [ "imagen" => "gr1.jpeg" "Alto" => 662 "Ancho" => 959 "Tamanyo" => 85905 ] ] "descripcion" => array:1 [ "en" => "<p id="spar0005" class="elsevierStyleSimplePara elsevierViewall">Image showing clubbed fingers.</p>" ] ] ] "autores" => array:1 [ 0 => array:2 [ "autoresLista" => "M. Yang, B.D. Nguyen, M.C. Roarke" "autores" => array:3 [ 0 => array:2 [ "nombre" => "M." "apellidos" => "Yang" ] 1 => array:2 [ "nombre" => "B.D." "apellidos" => "Nguyen" ] 2 => array:2 [ "nombre" => "M.C." "apellidos" => "Roarke" ] ] ] ] ] "idiomaDefecto" => "en" "EPUB" => "https://multimedia.elsevier.es/PublicationsMultimediaV1/item/epub/S2253808915000968?idApp=UINPBA00004N" "url" => "/22538089/0000003400000006/v1_201510310036/S2253808915000968/v1_201510310036/en/main.assets" ] "itemAnterior" => array:18 [ "pii" => "S2253808915001019" "issn" => "22538089" "doi" => "10.1016/j.remnie.2015.10.005" "estado" => "S300" "fechaPublicacion" => "2015-11-01" "aid" => "703" "copyright" => "Elsevier España, S.L.U. and SEMNIM" "documento" => "simple-article" "crossmark" => 1 "subdocumento" => "crp" "cita" => "Rev Esp Med Nucl Imagen Mol. 2015;34:387-9" "abierto" => array:3 [ "ES" => false "ES2" => false "LATM" => false ] "gratuito" => false "lecturas" => array:2 [ "total" => 93 "formatos" => array:2 [ "HTML" => 15 "PDF" => 78 ] ] "en" => array:13 [ "idiomaDefecto" => true "cabecera" => "<span class="elsevierStyleTextfn">Clinical note</span>" "titulo" => "Follow-up <span class="elsevierStyleSup">99m</span>Tc EC renal dynamic scintigraphy and DMSA-<span class="elsevierStyleSmallCaps">III</span> SPECT/CT in unmasking a masqueraded case of Horseshoe kidney" "tienePdf" => "en" "tieneTextoCompleto" => "en" "tieneResumen" => array:2 [ 0 => "en" 1 => "es" ] "paginas" => array:1 [ 0 => array:2 [ "paginaInicial" => "387" "paginaFinal" => "389" ] ] "titulosAlternativos" => array:1 [ "es" => array:1 [ "titulo" => "Seguimiento mediante gammagrafía renal dinámica con <span class="elsevierStyleSup">99m</span>Tc-EC y SPECT/TC con DMSA <span class="elsevierStyleSmallCaps">III</span> para desenmascarar un riñón en herradura" ] ] "contieneResumen" => array:2 [ "en" => true "es" => true ] "contieneTextoCompleto" => array:1 [ "en" => true ] "contienePdf" => array:1 [ "en" => true ] "resumenGrafico" => array:2 [ "original" => 0 "multimedia" => array:7 [ "identificador" => "fig0005" "etiqueta" => "Fig. 1" "tipo" => "MULTIMEDIAFIGURA" "mostrarFloat" => true "mostrarDisplay" => false "figura" => array:1 [ 0 => array:4 [ "imagen" => "gr1.jpeg" "Alto" => 962 "Ancho" => 1950 "Tamanyo" => 226408 ] ] "descripcion" => array:1 [ "en" => "<p id="spar0015" class="elsevierStyleSimplePara elsevierViewall">Intravenous urography (IVU) images. (a) Plain film of KUB region shows no radio-opaque calculus. After intravenous bolus injection of water soluble contrast, sequential plain films were acquired at 7, 15, 60 and 120<span class="elsevierStyleHsp" style=""></span>min. Plain images (b–e) revealed normally located both kidneys with prompt extraction of contrast in adequate concentration. Right PCS is compact with sharp fornicial angles and maintained papillary impression. Right ureter is normal in course, caliber and outline. Left PCS is dilated with blunting of fornicial angles and ballooning of calices. Left ureter is not visualized. Plain image (f) acquired 5<span class="elsevierStyleHsp" style=""></span>min after intravenous injection of lasix which revealed complete excretion of contrast from right PCS while persistence of contrast in left PCS (s/o left sided grade <span class="elsevierStyleSmallCaps">IV</span> hydronephrosis with pelviureteric junction obstruction). Intraop micturating cysto-urethrogram (MCU) image (g) No e/o evidence of vesicoureteric reflux (VUR).</p>" ] ] ] "autores" => array:1 [ 0 => array:2 [ "autoresLista" => "T.K. Jain, R.K. Basher, B.R. Mittal, A. Bhatia, K.L.N. Rao" "autores" => array:5 [ 0 => array:2 [ "nombre" => "T.K." "apellidos" => "Jain" ] 1 => array:2 [ "nombre" => "R.K." "apellidos" => "Basher" ] 2 => array:2 [ "nombre" => "B.R." "apellidos" => "Mittal" ] 3 => array:2 [ "nombre" => "A." "apellidos" => "Bhatia" ] 4 => array:2 [ "nombre" => "K.L.N." "apellidos" => "Rao" ] ] ] ] ] "idiomaDefecto" => "en" "EPUB" => "https://multimedia.elsevier.es/PublicationsMultimediaV1/item/epub/S2253808915001019?idApp=UINPBA00004N" "url" => "/22538089/0000003400000006/v1_201510310036/S2253808915001019/v1_201510310036/en/main.assets" ] "en" => array:14 [ "idiomaDefecto" => true "cabecera" => "<span class="elsevierStyleTextfn">Interesting images</span>" "titulo" => "Ground-glass opacity of the lung in a patient with melanoma: “The radiological seed of doubt”" "tieneTextoCompleto" => true "paginas" => array:1 [ 0 => array:2 [ "paginaInicial" => "390" "paginaFinal" => "392" ] ] "autores" => array:1 [ 0 => array:4 [ "autoresLista" => "G. Dalpiaz, K. Kawamukai, A.M. Parisi, L. La Torre, D. Forcella, G. Leuzzi" "autores" => array:6 [ 0 => array:3 [ "nombre" => "G." "apellidos" => "Dalpiaz" "referencia" => array:1 [ 0 => array:2 [ "etiqueta" => "<span class="elsevierStyleSup">a</span>" "identificador" => "aff0005" ] ] ] 1 => array:3 [ "nombre" => "K." "apellidos" => "Kawamukai" "referencia" => array:1 [ 0 => array:2 [ "etiqueta" => "<span class="elsevierStyleSup">b</span>" "identificador" => "aff0010" ] ] ] 2 => array:3 [ "nombre" => "A.M." "apellidos" => "Parisi" "referencia" => array:1 [ 0 => array:2 [ "etiqueta" => "<span class="elsevierStyleSup">b</span>" "identificador" => "aff0010" ] ] ] 3 => array:3 [ "nombre" => "L." "apellidos" => "La Torre" "referencia" => array:1 [ 0 => array:2 [ "etiqueta" => "<span class="elsevierStyleSup">c</span>" "identificador" => "aff0015" ] ] ] 4 => array:3 [ "nombre" => "D." "apellidos" => "Forcella" "referencia" => array:1 [ 0 => array:2 [ "etiqueta" => "<span class="elsevierStyleSup">d</span>" "identificador" => "aff0020" ] ] ] 5 => array:4 [ "nombre" => "G." "apellidos" => "Leuzzi" "email" => array:1 [ 0 => "gio.leuzzi@yahoo.it" ] "referencia" => array:2 [ 0 => array:2 [ "etiqueta" => "<span class="elsevierStyleSup">d</span>" "identificador" => "aff0020" ] 1 => array:2 [ "etiqueta" => "<span class="elsevierStyleSup">*</span>" "identificador" => "cor0005" ] ] ] ] "afiliaciones" => array:4 [ 0 => array:3 [ "entidad" => "Department of Radiology, Bellaria Hospital, Bologna, Italy" "etiqueta" => "a" "identificador" => "aff0005" ] 1 => array:3 [ "entidad" => "Department of Thoracic Surgery, Maggiore and Bellaria Hospitals, Bologna, Italy" "etiqueta" => "b" "identificador" => "aff0010" ] 2 => array:3 [ "entidad" => "Department of Oncology, Imola, Italy" "etiqueta" => "c" "identificador" => "aff0015" ] 3 => array:3 [ "entidad" => "Department of Surgical Oncology, Thoracic Surgery Unit, Regina Elena National Cancer Institute – IFO, Rome, Italy" "etiqueta" => "d" "identificador" => "aff0020" ] ] "correspondencia" => array:1 [ 0 => array:3 [ "identificador" => "cor0005" "etiqueta" => "⁎" "correspondencia" => "Corresponding author." ] ] ] ] "titulosAlternativos" => array:1 [ "es" => array:1 [ "titulo" => "Opacidad pulmonar en vidrio esmerilado en un paciente con antecedente de melanoma: “la semilla radiológica de la duda”" ] ] "resumenGrafico" => array:2 [ "original" => 0 "multimedia" => array:7 [ "identificador" => "fig0015" "etiqueta" => "Fig. 3" "tipo" => "MULTIMEDIAFIGURA" "mostrarFloat" => true "mostrarDisplay" => false "figura" => array:1 [ 0 => array:4 [ "imagen" => "gr3.jpeg" "Alto" => 600 "Ancho" => 1620 "Tamanyo" => 238442 ] ] "descripcion" => array:1 [ "en" => "<p id="spar0015" class="elsevierStyleSimplePara elsevierViewall">(A) Microscopic findings (Haematoxylin and Eosin, original magnification ×5): tumor cells spreading along the alveolar walls and organized in lepidic pattern. No necrotic foci were evidenced. (B) The tumor cells were diffusely stained for antibody anti-S100. Based on these findings, the final pathology was consistent with lung metastasis from melanoma.</p>" ] ] ] "textoCompleto" => "<span class="elsevierStyleSections"><p id="par0005" class="elsevierStylePara elsevierViewall">A 51-year-old Caucasian woman referred to our Department for radiological evidence of ground-glass opacity (GGO) of the left lung. She was an active smoker; her medical history was unremarkable with the exception of the surgical excision 2 years before of a malignant melanoma localized in the left hand and with metastases of axillary nodes (staged as pT3bN0M1b). A contrast-enhanced computed tomography scan (CT) revealed a non-solid nodule (measuring 2<span class="elsevierStyleHsp" style=""></span>cm) of the left upper lobe (LUL) along with some subcentimetric GGOs bilaterally (<a class="elsevierStyleCrossRef" href="#fig0005">Fig. 1</a>). After the admission, an <span class="elsevierStyleSup">18</span>FDG PET-CT (PET-CT) highlighted an increase of its solid component associated to a slight uptake (SUVmax 2.1) of the LUL lesion (<a class="elsevierStyleCrossRef" href="#fig0010">Fig. 2</a>). No signs of pathologic mediastinal nodes or extra-thoracic disease were disclosed. Given the subsolid nature of the nodule, bronchoscopy or CT-guided biopsy were not performed, thus, after a multidisciplinary meeting, the patient underwent a thoracoscopic LUL wedge resection. Frozen section disclosed atypical cells with lepidic growth only, making a proper pathological diagnosis unfeasible: hence, an uneventful left upper lobectomy plus systematic lymphadectomy was performed. Interestingly, final pathology evidenced intra-pulmonary metastasis from melanoma expressing c-kit mutation (B-Raf wild-type) without nodal involvement (<a class="elsevierStyleCrossRef" href="#fig0015">Fig. 3</a>), so the patient started chemo and immuno-therapy. One year after surgery, oncological follow-up evidenced a stable disease.</p><elsevierMultimedia ident="fig0005"></elsevierMultimedia><elsevierMultimedia ident="fig0010"></elsevierMultimedia><elsevierMultimedia ident="fig0015"></elsevierMultimedia><p id="par0010" class="elsevierStylePara elsevierViewall">So far, the management of nonsolid/subsolid pulmonary nodules is an extremely challenging issue. As advocated by the Fleischner Society, persistent nonsolid/subsolid nodules usually represent part of the pathologic spectrum of lung adenocarcinoma.<a class="elsevierStyleCrossRef" href="#bib0020"><span class="elsevierStyleSup">1</span></a> Moreover, lung metastasis from adenocarcinoma of thoracic or extra-thoracic origin (gastrointestinal tract, pancreas, kidney) and atypical adenomatous hyperplasia may present with such radiological features and lepidic growth. On the other hand, benign lesions arising from lymphoproliferative disorders, organizing pneumonia and focal interstitial fibrosis may mimic sometimes lung neoplasms given the high rate of GGOs related to these diseases.</p><p id="par0015" class="elsevierStylePara elsevierViewall">Pulmonary metastases from melanoma commonly present as one or multiple solid nodules at standard imaging while GGOs are very rarely reported in literature.<a class="elsevierStyleCrossRef" href="#bib0025"><span class="elsevierStyleSup">2</span></a> In this setting, PET-CT may play a role in the case of subsolid metastasis.<a class="elsevierStyleCrossRef" href="#bib0030"><span class="elsevierStyleSup">3</span></a> In fact, in our patient nuclear images (along with CT) were useful: (i) to evaluate the increase of nodule density; (ii) to assess the <span class="elsevierStyleSup">18</span>FDG uptake of the solid component (as reported for nodules exhibiting a solid part measuring more than 10<span class="elsevierStyleHsp" style=""></span>mm); (iii) to exclude nodal or extra-thoracic disease. Unfortunately, this uncommon radiological behavior reflects the pathological one related to lepidic growth (resulting from cancer spreading along alveolar walls), thus leading in difficult pathological diagnosis and, sometimes, overtreatment. In fact, due to the adenocarcinoma-like pathologic pattern, the patient underwent lobectomy rather than lung-sparing surgery.</p><p id="par0020" class="elsevierStylePara elsevierViewall">In conclusion, in case of radiological evidence of GGOs after surgery for melanoma, follow-up through CT scan and growth rate evaluation are well-recognized options to further analyze such nodules.<a class="elsevierStyleCrossRef" href="#bib0020"><span class="elsevierStyleSup">1</span></a> When non-solid nodules acquire partially solid pattern, PET-CT may be useful to better characterize the solid component and to accurately stage the disease. Furthermore, in the suspect of primary or secondary lesions, surgery is usually indicated in order to obtain final diagnosis and oncological treatment simultaneously.</p><span id="sec0005" class="elsevierStyleSection elsevierViewall"><span class="elsevierStyleSectionTitle" id="sect0005">Conflicts of interest</span><p id="par0025" class="elsevierStylePara elsevierViewall">None declared.</p></span></span>" "textoCompletoSecciones" => array:1 [ "secciones" => array:2 [ 0 => array:2 [ "identificador" => "sec0005" "titulo" => "Conflicts of interest" ] 1 => array:1 [ "titulo" => "References" ] ] ] "pdfFichero" => "main.pdf" "tienePdf" => true "multimedia" => array:3 [ 0 => array:7 [ "identificador" => "fig0005" "etiqueta" => "Fig. 1" "tipo" => "MULTIMEDIAFIGURA" "mostrarFloat" => true "mostrarDisplay" => false "figura" => array:1 [ 0 => array:4 [ "imagen" => "gr1.jpeg" "Alto" => 740 "Ancho" => 975 "Tamanyo" => 142239 ] ] "descripcion" => array:1 [ "en" => "<p id="spar0005" class="elsevierStyleSimplePara elsevierViewall">CT scan performed before admission (axial slice): CT images demonstrate a non-solid nodule (measuring 2<span class="elsevierStyleHsp" style=""></span>cm in the major axis) of the left upper lobe along with some subcentimetric ground-glass opacities bilaterally.</p>" ] ] 1 => array:7 [ "identificador" => "fig0010" "etiqueta" => "Fig. 2" "tipo" => "MULTIMEDIAFIGURA" "mostrarFloat" => true "mostrarDisplay" => false "figura" => array:1 [ 0 => array:4 [ "imagen" => "gr2.jpeg" "Alto" => 1800 "Ancho" => 1865 "Tamanyo" => 220244 ] ] "descripcion" => array:1 [ "en" => "<p id="spar0010" class="elsevierStyleSimplePara elsevierViewall">Whole body PET/CT performed 1<span class="elsevierStyleHsp" style=""></span>h after the administration of 296 MBq of 1<span class="elsevierStyleSup">18</span>FDG (axial and oblique slices): the images evidenced an increase of the solid component of the lung nodule associated with a slight <span class="elsevierStyleSup">18</span>FDG uptake (SUVmax 2.1). No signs of pathologic mediastinal nodes or extra-thoracic disease were disclosed.</p>" ] ] 2 => array:7 [ "identificador" => "fig0015" "etiqueta" => "Fig. 3" "tipo" => "MULTIMEDIAFIGURA" "mostrarFloat" => true "mostrarDisplay" => false "figura" => array:1 [ 0 => array:4 [ "imagen" => "gr3.jpeg" "Alto" => 600 "Ancho" => 1620 "Tamanyo" => 238442 ] ] "descripcion" => array:1 [ "en" => "<p id="spar0015" class="elsevierStyleSimplePara elsevierViewall">(A) Microscopic findings (Haematoxylin and Eosin, original magnification ×5): tumor cells spreading along the alveolar walls and organized in lepidic pattern. No necrotic foci were evidenced. (B) The tumor cells were diffusely stained for antibody anti-S100. Based on these findings, the final pathology was consistent with lung metastasis from melanoma.</p>" ] ] ] "bibliografia" => array:2 [ "titulo" => "References" "seccion" => array:1 [ 0 => array:2 [ "identificador" => "bibs0005" "bibliografiaReferencia" => array:3 [ 0 => array:3 [ "identificador" => "bib0020" "etiqueta" => "1" "referencia" => array:1 [ 0 => array:2 [ "contribucion" => array:1 [ 0 => array:2 [ "titulo" => "Recommendations for the management of subsolid pulmonary nodules detected at CT: a statement from the Fleischner Society" "autores" => array:1 [ 0 => array:2 [ "etal" => true "autores" => array:6 [ 0 => "D.P. Naidich" 1 => "A.A. Bankier" 2 => "H. MacMahon" 3 => "C.M. Schaefer-Prokop" 4 => "M. Pistolesi" 5 => "J.M. Goo" ] ] ] ] ] "host" => array:1 [ 0 => array:2 [ "doi" => "10.1148/radiol.12120628" "Revista" => array:6 [ "tituloSerie" => "Radiology" "fecha" => "2013" "volumen" => "266" "paginaInicial" => "304" "paginaFinal" => "317" "link" => array:1 [ 0 => array:2 [ "url" => "https://www.ncbi.nlm.nih.gov/pubmed/23070270" "web" => "Medline" ] ] ] ] ] ] ] ] 1 => array:3 [ "identificador" => "bib0025" "etiqueta" => "2" "referencia" => array:1 [ 0 => array:2 [ "contribucion" => array:1 [ 0 => array:2 [ "titulo" => "Ground-glass nodules found in two patients with malignant melanomas: different growth rate and different histology" "autores" => array:1 [ 0 => array:2 [ "etal" => false "autores" => array:6 [ 0 => "M.J. Kang" 1 => "M.A. Kim" 2 => "C.M. Park" 3 => "C.H. Lee" 4 => "J.M. Goo" 5 => "H.J. Lee" ] ] ] ] ] "host" => array:1 [ 0 => array:2 [ "doi" => "10.1016/j.clinimag.2009.10.036" "Revista" => array:6 [ "tituloSerie" => "Clin Imaging" "fecha" => "2010" "volumen" => "34" "paginaInicial" => "396" "paginaFinal" => "399" "link" => array:1 [ 0 => array:2 [ "url" => "https://www.ncbi.nlm.nih.gov/pubmed/20813308" "web" => "Medline" ] ] ] ] ] ] ] ] 2 => array:3 [ "identificador" => "bib0030" "etiqueta" => "3" "referencia" => array:1 [ 0 => array:2 [ "contribucion" => array:1 [ 0 => array:2 [ "titulo" => "High-risk melanoma: accuracy of FDG PET/CT with added CT morphologic information for detection of metastases" "autores" => array:1 [ 0 => array:2 [ "etal" => false "autores" => array:6 [ 0 => "K. Strobel" 1 => "R. Dummer" 2 => "D.B. Husarik" 3 => "M. Pérez Lago" 4 => "T.F. Hany" 5 => "H.C. Steinert" ] ] ] ] ] "host" => array:1 [ 0 => array:2 [ "doi" => "10.1148/radiol.2442061099" "Revista" => array:6 [ "tituloSerie" => "Radiology" "fecha" => "2007" "volumen" => "244" "paginaInicial" => "566" "paginaFinal" => "574" "link" => array:1 [ 0 => array:2 [ "url" => "https://www.ncbi.nlm.nih.gov/pubmed/17641374" "web" => "Medline" ] ] ] ] ] ] ] ] ] ] ] ] ] "idiomaDefecto" => "en" "url" => "/22538089/0000003400000006/v1_201510310036/S2253808915001007/v1_201510310036/en/main.assets" "Apartado" => array:4 [ "identificador" => "7927" "tipo" => "SECCION" "en" => array:2 [ "titulo" => "Interesting images" "idiomaDefecto" => true ] "idiomaDefecto" => "en" ] "PDF" => "https://static.elsevier.es/multimedia/22538089/0000003400000006/v1_201510310036/S2253808915001007/v1_201510310036/en/main.pdf?idApp=UINPBA00004N&text.app=https://www.elsevier.es/" "EPUB" => "https://multimedia.elsevier.es/PublicationsMultimediaV1/item/epub/S2253808915001007?idApp=UINPBA00004N" ]
Consulte los artículos y contenidos publicados en éste medio, además de los e-sumarios de las revistas científicas en el mismo momento de publicación
Esté informado en todo momento gracias a las alertas y novedades
Acceda a promociones exclusivas en suscripciones, lanzamientos y cursos acreditados
The Revista Española de Medicina Nuclear e Imagen Molecular (Spanish Journal of Nuclear Medicine and Molecular Imaging), was founded in 1982, and is the official journal of the Spanish Society of Nuclear Medicine and Molecular Imaging, which has more than 700 members. The Journal, which publishes 6 regular issues per year, has the promotion of research and continuing education in all fields of Nuclear Medicine as its main aim. For this, its principal sections are Originals, Clinical Notes, Images of Interest, and Special Collaboration articles. The works may be submitted in Spanish or English and are subjected to a peer review process. In 2009, it became the leading Spanish journal in the field of Medical Imaging on having an Impact Factor , awarded by the Journal Citation Reports.
Science Citation Index Expander, Medline, IME, Bibliomed, EMBASE/Excerpta Medica, Healthstar, Cancerlit, Toxine, Inside Conferences, Scopus
See moreThe Impact Factor measures the average number of citations received in a particular year by papers published in the journal during the two preceding years.
© Clarivate Analytics, Journal Citation Reports 2022
SRJ is a prestige metric based on the idea that not all citations are the same. SJR uses a similar algorithm as the Google page rank; it provides a quantitative and qualitative measure of the journal's impact.
See moreSNIP measures contextual citation impact by wighting citations based on the total number of citations in a subject field.
See more
Revista Española de Medicina Nuclear e Imagen Molecular (English Edition)

¿Es usted profesional sanitario apto para prescribir o dispensar medicamentos?
Are you a health professional able to prescribe or dispense drugs?
Você é um profissional de saúde habilitado a prescrever ou dispensar medicamentos