Article

Revista Española de Medicina Nuclear e Imagen Molecular (English Edition)
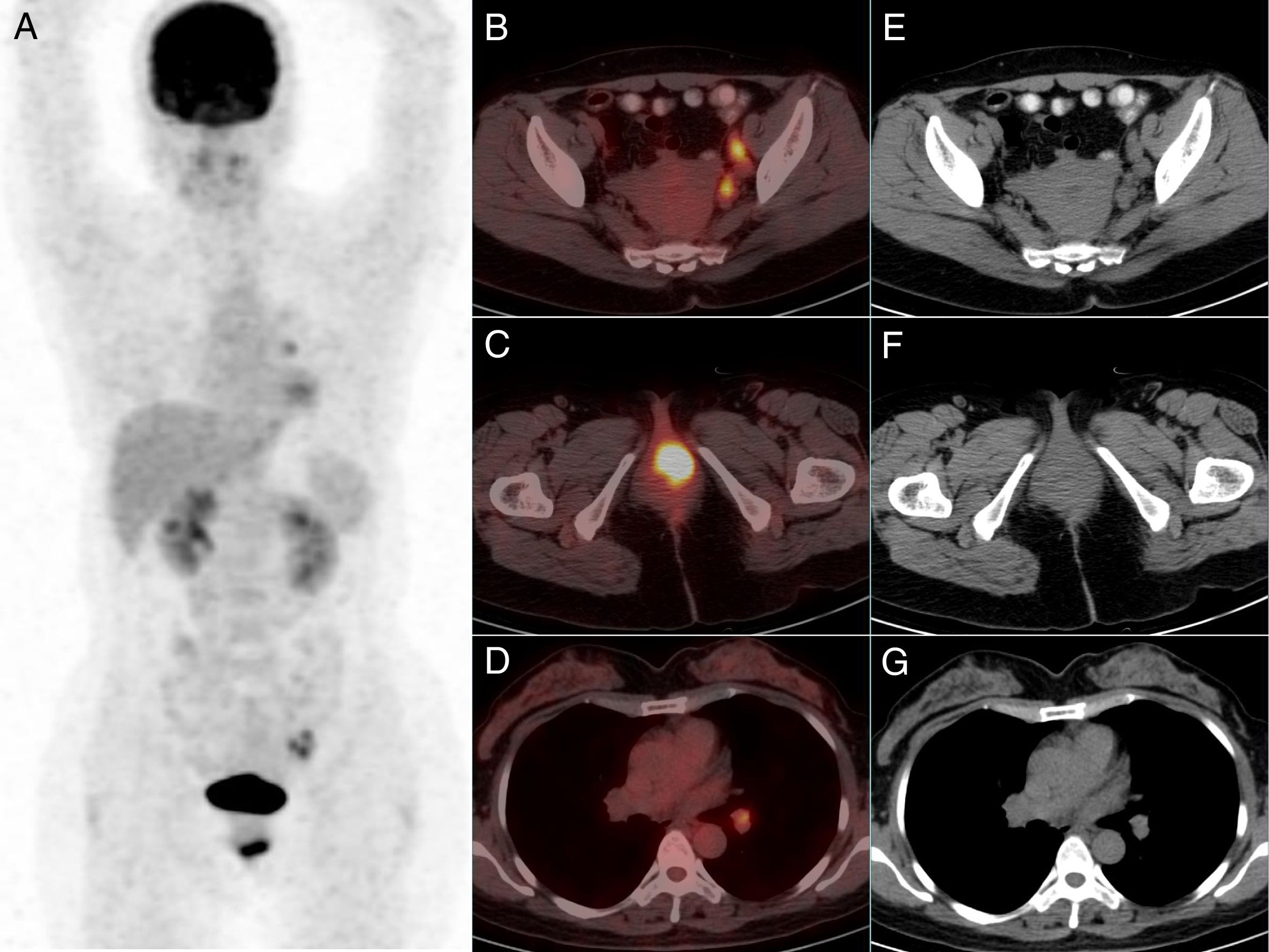
array:23 [ "pii" => "S225380891930045X" "issn" => "22538089" "doi" => "10.1016/j.remnie.2019.04.003" "estado" => "S300" "fechaPublicacion" => "2020-01-01" "aid" => "1071" "copyrightAnyo" => "2019" "documento" => "article" "crossmark" => 1 "subdocumento" => "sco" "cita" => "Rev Esp Med Nucl Imagen Mol. 2020;39:43-4" "abierto" => array:3 [ "ES" => false "ES2" => false "LATM" => false ] "gratuito" => false "lecturas" => array:1 [ "total" => 0 ] "Traduccion" => array:1 [ "es" => array:18 [ "pii" => "S2253654X19300617" "issn" => "2253654X" "doi" => "10.1016/j.remn.2019.04.001" "estado" => "S300" "fechaPublicacion" => "2020-01-01" "aid" => "1071" "documento" => "article" "crossmark" => 1 "subdocumento" => "sco" "cita" => "Rev Esp Med Nucl Imagen Mol. 2020;39:43-4" "abierto" => array:3 [ "ES" => false "ES2" => false "LATM" => false ] "gratuito" => false "lecturas" => array:2 [ "total" => 13 "formatos" => array:2 [ "HTML" => 7 "PDF" => 6 ] ] "es" => array:11 [ "idiomaDefecto" => true "cabecera" => "<span class="elsevierStyleTextfn">Imágenes de interés</span>" "titulo" => "Metástasis vaginal por cáncer de recto detectada por <span class="elsevierStyleSup">18</span>F-FDG PET/TC" "tienePdf" => "es" "tieneTextoCompleto" => "es" "paginas" => array:1 [ 0 => array:2 [ "paginaInicial" => "43" "paginaFinal" => "44" ] ] "titulosAlternativos" => array:1 [ "en" => array:1 [ "titulo" => "Vaginal metastasis from rectal cancer detected by <span class="elsevierStyleSup">18</span>F-FDG PET/CT" ] ] "contieneTextoCompleto" => array:1 [ "es" => true ] "contienePdf" => array:1 [ "es" => true ] "resumenGrafico" => array:2 [ "original" => 0 "multimedia" => array:7 [ "identificador" => "fig0005" "etiqueta" => "Figura 1" "tipo" => "MULTIMEDIAFIGURA" "mostrarFloat" => true "mostrarDisplay" => false "figura" => array:1 [ 0 => array:4 [ "imagen" => "gr1.jpeg" "Alto" => 1779 "Ancho" => 2371 "Tamanyo" => 325809 ] ] "descripcion" => array:1 [ "es" => "<p id="spar0005" class="elsevierStyleSimplePara elsevierViewall">Las imágenes de proyección de máxima intensidad de PET (A), de fusión axial (B-D) y de TC (E-G) revelaron que había múltiples adenopatías con avidez por la FDG a lo largo de las cadenas ilíacas internas y externas, con un eje corto y un SUVmáx de 15<span class="elsevierStyleHsp" style=""></span>mm y 6,4, respectivamente. Estas adenopatías deben considerarse metástasis tumorales. Además, había una masa hipermetabólica en la mitad izquierda de la vagina, con un SUVmáx de 10,8, pero sin alteraciones en el sitio correspondiente del componente TC de alta dosis de la PET/TC. Se pudo encontrar otro ganglio linfático anormal en el hilio pulmonar derecho, con un eje corto y un SUVmáx de 10<span class="elsevierStyleHsp" style=""></span>mm y 4,2, respectivamente. Según la vía de drenaje linfático del recto, la adenopatía hiliar era más probable que fuera una hiperplasia reactiva.</p>" ] ] ] "autores" => array:1 [ 0 => array:2 [ "autoresLista" => "Q. Fan, D. Huang, M. Su" "autores" => array:3 [ 0 => array:2 [ "nombre" => "Q." "apellidos" => "Fan" ] 1 => array:2 [ "nombre" => "D." "apellidos" => "Huang" ] 2 => array:2 [ "nombre" => "M." "apellidos" => "Su" ] ] ] ] ] "idiomaDefecto" => "es" "Traduccion" => array:1 [ "en" => array:9 [ "pii" => "S225380891930045X" "doi" => "10.1016/j.remnie.2019.04.003" "estado" => "S300" "subdocumento" => "" "abierto" => array:3 [ "ES" => false "ES2" => false "LATM" => false ] "gratuito" => false "lecturas" => array:1 [ "total" => 0 ] "idiomaDefecto" => "en" "EPUB" => "https://multimedia.elsevier.es/PublicationsMultimediaV1/item/epub/S225380891930045X?idApp=UINPBA00004N" ] ] "EPUB" => "https://multimedia.elsevier.es/PublicationsMultimediaV1/item/epub/S2253654X19300617?idApp=UINPBA00004N" "url" => "/2253654X/0000003900000001/v2_202011070654/S2253654X19300617/v2_202011070654/es/main.assets" ] ] "itemSiguiente" => array:19 [ "pii" => "S2253808919300448" "issn" => "22538089" "doi" => "10.1016/j.remnie.2019.04.002" "estado" => "S300" "fechaPublicacion" => "2020-01-01" "aid" => "1070" "copyright" => "Sociedad Española de Medicina Nuclear e Imagen Molecular" "documento" => "article" "crossmark" => 1 "subdocumento" => "sco" "cita" => "Rev Esp Med Nucl Imagen Mol. 2020;39:45-6" "abierto" => array:3 [ "ES" => false "ES2" => false "LATM" => false ] "gratuito" => false "lecturas" => array:1 [ "total" => 0 ] "en" => array:11 [ "idiomaDefecto" => true "cabecera" => "<span class="elsevierStyleTextfn">Interesting image</span>" "titulo" => "Incremental value of <span class="elsevierStyleSup">18</span>F-fluorocholine PET/CT in comparison with <span class="elsevierStyleSup">68</span>Ga-DOTA PET/CT in adrenal adenoma localization in a MEN1 patient" "tienePdf" => "en" "tieneTextoCompleto" => "en" "paginas" => array:1 [ 0 => array:2 [ "paginaInicial" => "45" "paginaFinal" => "46" ] ] "titulosAlternativos" => array:1 [ "es" => array:1 [ "titulo" => "Valor incremental de la PET/TC con <span class="elsevierStyleSup">18</span>F-Fluorocolina en comparación con la PET/TC con <span class="elsevierStyleSup">68</span>Ga-DOTA en la localización de adenoma suprarrenal en paciente con MEN1" ] ] "contieneTextoCompleto" => array:1 [ "en" => true ] "contienePdf" => array:1 [ "en" => true ] "resumenGrafico" => array:2 [ "original" => 0 "multimedia" => array:7 [ "identificador" => "fig0005" "etiqueta" => "Fig. 1" "tipo" => "MULTIMEDIAFIGURA" "mostrarFloat" => true "mostrarDisplay" => false "figura" => array:1 [ 0 => array:4 [ "imagen" => "gr1.jpeg" "Alto" => 1345 "Ancho" => 1500 "Tamanyo" => 246611 ] ] "descripcion" => array:1 [ "en" => "<p id="spar0005" class="elsevierStyleSimplePara elsevierViewall">The maximum intensity projection image (A) of <span class="elsevierStyleSup">68</span>Ga-DOTA-TATE, axial CT (B, D, F, H and J) and fused images (C, E, G, I and K) revealed nodular lesions in the left lobe of thyroid (B–C), in the pancreatic tail (D–E), horizontal segment of the duodenum (F–G) and in left adrenal gland (H–K).</p>" ] ] ] "autores" => array:1 [ 0 => array:2 [ "autoresLista" => "Yuxiao Xia, Zi Wang, Yanhong Zhao, Huipan Liu, Yue Chen" "autores" => array:5 [ 0 => array:2 [ "nombre" => "Yuxiao" "apellidos" => "Xia" ] 1 => array:2 [ "nombre" => "Zi" "apellidos" => "Wang" ] 2 => array:2 [ "nombre" => "Yanhong" "apellidos" => "Zhao" ] 3 => array:2 [ "nombre" => "Huipan" "apellidos" => "Liu" ] 4 => array:2 [ "nombre" => "Yue" "apellidos" => "Chen" ] ] ] ] ] "idiomaDefecto" => "en" "Traduccion" => array:1 [ "es" => array:9 [ "pii" => "S2253654X19300587" "doi" => "10.1016/j.remn.2019.03.004" "estado" => "S300" "subdocumento" => "" "abierto" => array:3 [ "ES" => false "ES2" => false "LATM" => false ] "gratuito" => false "lecturas" => array:1 [ "total" => 0 ] "idiomaDefecto" => "es" "EPUB" => "https://multimedia.elsevier.es/PublicationsMultimediaV1/item/epub/S2253654X19300587?idApp=UINPBA00004N" ] ] "EPUB" => "https://multimedia.elsevier.es/PublicationsMultimediaV1/item/epub/S2253808919300448?idApp=UINPBA00004N" "url" => "/22538089/0000003900000001/v1_202001150636/S2253808919300448/v1_202001150636/en/main.assets" ] "itemAnterior" => array:19 [ "pii" => "S2253808919300709" "issn" => "22538089" "doi" => "10.1016/j.remnie.2019.05.003" "estado" => "S300" "fechaPublicacion" => "2020-01-01" "aid" => "1076" "copyright" => "Sociedad Española de Medicina Nuclear e Imagen Molecular" "documento" => "article" "crossmark" => 1 "subdocumento" => "sco" "cita" => "Rev Esp Med Nucl Imagen Mol. 2020;39:41-2" "abierto" => array:3 [ "ES" => false "ES2" => false "LATM" => false ] "gratuito" => false "lecturas" => array:2 [ "total" => 5 "formatos" => array:2 [ "HTML" => 3 "PDF" => 2 ] ] "en" => array:11 [ "idiomaDefecto" => true "cabecera" => "<span class="elsevierStyleTextfn">Interesting image</span>" "titulo" => "Nonfunctioning paraganglioma incidentally detected by <span class="elsevierStyleSup">18</span>F-FDG PET/CT and confirmed by <span class="elsevierStyleSup">123</span>I-MIBG M scintigraphy" "tienePdf" => "en" "tieneTextoCompleto" => "en" "paginas" => array:1 [ 0 => array:2 [ "paginaInicial" => "41" "paginaFinal" => "42" ] ] "titulosAlternativos" => array:1 [ "es" => array:1 [ "titulo" => "Paraganglioma no funcional detectado incidentalmente en 18F-FDG PET/CT y confirmado mediante gammagrafia con 123I-MIBG" ] ] "contieneTextoCompleto" => array:1 [ "en" => true ] "contienePdf" => array:1 [ "en" => true ] "resumenGrafico" => array:2 [ "original" => 0 "multimedia" => array:7 [ "identificador" => "fig0015" "etiqueta" => "Fig. 3" "tipo" => "MULTIMEDIAFIGURA" "mostrarFloat" => true "mostrarDisplay" => false "figura" => array:1 [ 0 => array:4 [ "imagen" => "gr3.jpeg" "Alto" => 571 "Ancho" => 905 "Tamanyo" => 205410 ] ] "descripcion" => array:1 [ "en" => "<p id="spar0015" class="elsevierStyleSimplePara elsevierViewall">Hematoxylin and eosin stain showing cells with a well defined basophilic granular cytoplasm and nuclei with granular chromatic pattern (zellballen growth pattern) (A). Immunohistochemical technique showing a strong reactivity with chromogranin (B) and with synaptophysin (C).</p>" ] ] ] "autores" => array:1 [ 0 => array:2 [ "autoresLista" => "Rexhep Durmo, Domenico Albano, Valentina Crisafulli, Fabrizia Terraneo, Raffaele Giubbini, Francesco Bertagna" "autores" => array:6 [ 0 => array:2 [ "nombre" => "Rexhep" "apellidos" => "Durmo" ] 1 => array:2 [ "nombre" => "Domenico" "apellidos" => "Albano" ] 2 => array:2 [ "nombre" => "Valentina" "apellidos" => "Crisafulli" ] 3 => array:2 [ "nombre" => "Fabrizia" "apellidos" => "Terraneo" ] 4 => array:2 [ "nombre" => "Raffaele" "apellidos" => "Giubbini" ] 5 => array:2 [ "nombre" => "Francesco" "apellidos" => "Bertagna" ] ] ] ] ] "idiomaDefecto" => "en" "Traduccion" => array:1 [ "es" => array:9 [ "pii" => "S2253654X19300381" "doi" => "10.1016/j.remn.2019.05.001" "estado" => "S300" "subdocumento" => "" "abierto" => array:3 [ "ES" => false "ES2" => false "LATM" => false ] "gratuito" => false "lecturas" => array:1 [ "total" => 0 ] "idiomaDefecto" => "es" "EPUB" => "https://multimedia.elsevier.es/PublicationsMultimediaV1/item/epub/S2253654X19300381?idApp=UINPBA00004N" ] ] "EPUB" => "https://multimedia.elsevier.es/PublicationsMultimediaV1/item/epub/S2253808919300709?idApp=UINPBA00004N" "url" => "/22538089/0000003900000001/v1_202001150636/S2253808919300709/v1_202001150636/en/main.assets" ] "en" => array:15 [ "idiomaDefecto" => true "cabecera" => "<span class="elsevierStyleTextfn">Interesting images</span>" "titulo" => "Vaginal metastasis from rectal cancer detected by <span class="elsevierStyleSup">18</span>F-FDG PET/CT" "tieneTextoCompleto" => true "paginas" => array:1 [ 0 => array:2 [ "paginaInicial" => "43" "paginaFinal" => "44" ] ] "autores" => array:1 [ 0 => array:4 [ "autoresLista" => "Qiuping Fan, Dongqiong Huang, Minggang Su" "autores" => array:3 [ 0 => array:3 [ "nombre" => "Qiuping" "apellidos" => "Fan" "referencia" => array:1 [ 0 => array:2 [ "etiqueta" => "<span class="elsevierStyleSup">a</span>" "identificador" => "aff0005" ] ] ] 1 => array:3 [ "nombre" => "Dongqiong" "apellidos" => "Huang" "referencia" => array:1 [ 0 => array:2 [ "etiqueta" => "<span class="elsevierStyleSup">b</span>" "identificador" => "aff0010" ] ] ] 2 => array:4 [ "nombre" => "Minggang" "apellidos" => "Su" "email" => array:1 [ 0 => "suminggang@sina.com" ] "referencia" => array:2 [ 0 => array:2 [ "etiqueta" => "<span class="elsevierStyleSup">a</span>" "identificador" => "aff0005" ] 1 => array:2 [ "etiqueta" => "*" "identificador" => "cor0005" ] ] ] ] "afiliaciones" => array:2 [ 0 => array:3 [ "entidad" => "Department of Nuclear Medicine, West China Hospital, Sichuan University, No. 37 Guoxue Alley, Chengdu 610041, Sichuan, China" "etiqueta" => "a" "identificador" => "aff0005" ] 1 => array:3 [ "entidad" => "Department of Nuclear Medicine, Dazhou Central Hospital, No. 151 Dadong Street, Danzhou 635000, Sichuan, China" "etiqueta" => "b" "identificador" => "aff0010" ] ] "correspondencia" => array:1 [ 0 => array:3 [ "identificador" => "cor0005" "etiqueta" => "⁎" "correspondencia" => "Corresponding author." ] ] ] ] "titulosAlternativos" => array:1 [ "es" => array:1 [ "titulo" => "Metástasis vaginal por cáncer de recto detectada por <span class="elsevierStyleSup">18</span>F-FDG PET/TC" ] ] "resumenGrafico" => array:2 [ "original" => 0 "multimedia" => array:7 [ "identificador" => "fig0005" "etiqueta" => "Fig. 1" "tipo" => "MULTIMEDIAFIGURA" "mostrarFloat" => true "mostrarDisplay" => false "figura" => array:1 [ 0 => array:4 [ "imagen" => "gr1.jpeg" "Alto" => 1778 "Ancho" => 2370 "Tamanyo" => 326392 ] ] "descripcion" => array:1 [ "en" => "<p id="spar0005" class="elsevierStyleSimplePara elsevierViewall">The maximum intensity projection PET (A), axial fusion (B–D) and CT (E–G) images revealed there were multiple FDG avid lymphnodes along the internal and external iliac vessels, with short axis and SUVmax of 15<span class="elsevierStyleHsp" style=""></span>mm and 6.4 respectively. These lymphadenopathies should be cancer metastases. There was a hypermetabolic mass in the left part of the vagina in addition, with a SUVmax of 10.8, but no abnormality in the corresponding site on full dose CT component of PET/CT. Another abnormal lymph node could be found in the right lung hilum, with short axis and SUVmax of 10<span class="elsevierStyleHsp" style=""></span>mm and 4.2 respectively. According to the lymphatic drainage path of rectum, the hilar lymphadenopathy was more likely to be reactive hyperplasia.</p>" ] ] ] "textoCompleto" => "<span class="elsevierStyleSections"><p id="par0005" class="elsevierStylePara elsevierViewall">A 47-year-old woman complaining perineal discomfort for one month was admitted to our hospital. She had received a Miles radical resection for low rectal cancer 9 months earlier. The tumor was a moderately differentiated adenocarcinoma and qualified as T2N2aM0 (stage IIIB) disease by the 8th edition of the AJCC Cancer Staging Manual. Immunohistochemical results demonstrated the tumor cells were positive for CK20, Villin and CDX-2, but negative for CK7. Then, she received 6 cycles of oxaliplatin-based adjuvant chemotherapy with CapeOx regime. The last dose was administered 4 months ago. Because of perineal discomfort, she received unenhanced <span class="elsevierStyleSup">18</span>F-FDG PET/CT scanning for cancer surveillance. Her serum tumor makers (including CEA, CA-125, CA15-3 and CA19-9) test prior to PET/CT were negative. The PET/CT images revealed there were multiple lymphnode metastases along the left iliac vessels. There was a hypermetabolic mass in the left part of the vagina in addition, but no abnormality in the corresponding site on full dose CT component of PET/CT (<a class="elsevierStyleCrossRef" href="#fig0005">Fig. 1</a>). Subsequent physical examination found a mass in the lower part of the vagina. Histopathological study after biopsy confirmed the presence of moderately differentiated adenocarcinoma. Immunohistochemical results demonstrated the tumor cells were positive for CK20, Villin and CDX-2, P16 and EMA, but negative for CK7, Pax-8, ER and PR, which were compatible with the rectal origin. She got remission after receiving more 2 cycles of XELOX regime chemotherapy and concurrent radiotherapy. The patient was still in treatment at the time of report.</p><elsevierMultimedia ident="fig0005"></elsevierMultimedia><p id="par0010" class="elsevierStylePara elsevierViewall">Colorectal cancer is one of the most frequently diagnosed cancer and one of the leading cause of cancer death wordwide. The metastases are most frequently in the liver, pelvic and abdomen lymph nodes and lungs. The incidence of metastatic vaginal tumor was less than 0.03%. The most of them arose from uterus (65.9%), ovary (14.0%) and colorectum (8.5%).<a class="elsevierStyleCrossRef" href="#bib0020"><span class="elsevierStyleSup">1</span></a> Unlike the metastasis from gynecologic cancer, vaginal metastasis from colorectal cancer can present as possible primary lesion and be diagnosed before the colorectal primary lesion is diagnosed.<a class="elsevierStyleCrossRefs" href="#bib0020"><span class="elsevierStyleSup">1,2</span></a> It is difficult in clinical practice to discover a cancer metastasized to uncommon site on conventional imaging, especially for a patient with nonspecific complaint. <span class="elsevierStyleSup">18</span>F-FDG PET/CT can compensate for this limitation. It could detect 32% more extrahepatic metastasis than conventional imaging.<a class="elsevierStyleCrossRef" href="#bib0030"><span class="elsevierStyleSup">3</span></a> Information from PET/CT may result in a change in colorectal cancer management.<a class="elsevierStyleCrossRef" href="#bib0030"><span class="elsevierStyleSup">3</span></a> This whole body imaging method may be suitable for routine initial staging and post-treatment cancer surveillance, especially on a patient with clinical advanced stage or suspicion of recurrence. It is particularly hard to distinguish distant metastasis by an unusual source from a synchronous or metachronous primary cancer base on imaging only. But given to the primary vaginal carcinoma accounts for only 2% of all gynecologic malignancies and the detection of metastatic vaginal cancer may precede it is colorectal primary, when a vaginal tumor is shown to be hypermetabolic on PET/CT, metastasis should be in the scope of differential diagnosis.<a class="elsevierStyleCrossRef" href="#bib0025"><span class="elsevierStyleSup">2</span></a></p><span id="sec0005" class="elsevierStyleSection elsevierViewall"><span class="elsevierStyleSectionTitle" id="sect0005">Conflict of interest</span><p id="par0015" class="elsevierStylePara elsevierViewall">None declared.</p></span></span>" "textoCompletoSecciones" => array:1 [ "secciones" => array:2 [ 0 => array:2 [ "identificador" => "sec0005" "titulo" => "Conflict of interest" ] 1 => array:1 [ "titulo" => "References" ] ] ] "pdfFichero" => "main.pdf" "tienePdf" => true "NotaPie" => array:1 [ 0 => array:2 [ "etiqueta" => "☆" "nota" => "<p class="elsevierStyleNotepara" id="npar0005">Please cite this article as: Fan Q, Huang D, Su M. Metástasis vaginal por cáncer de recto detectada por <span class="elsevierStyleSup">18</span>F-FDG PET/TC. Rev Esp Med Nucl Imagen Mol. 2020;39:42–43.</p>" ] ] "multimedia" => array:1 [ 0 => array:7 [ "identificador" => "fig0005" "etiqueta" => "Fig. 1" "tipo" => "MULTIMEDIAFIGURA" "mostrarFloat" => true "mostrarDisplay" => false "figura" => array:1 [ 0 => array:4 [ "imagen" => "gr1.jpeg" "Alto" => 1778 "Ancho" => 2370 "Tamanyo" => 326392 ] ] "descripcion" => array:1 [ "en" => "<p id="spar0005" class="elsevierStyleSimplePara elsevierViewall">The maximum intensity projection PET (A), axial fusion (B–D) and CT (E–G) images revealed there were multiple FDG avid lymphnodes along the internal and external iliac vessels, with short axis and SUVmax of 15<span class="elsevierStyleHsp" style=""></span>mm and 6.4 respectively. These lymphadenopathies should be cancer metastases. There was a hypermetabolic mass in the left part of the vagina in addition, with a SUVmax of 10.8, but no abnormality in the corresponding site on full dose CT component of PET/CT. Another abnormal lymph node could be found in the right lung hilum, with short axis and SUVmax of 10<span class="elsevierStyleHsp" style=""></span>mm and 4.2 respectively. According to the lymphatic drainage path of rectum, the hilar lymphadenopathy was more likely to be reactive hyperplasia.</p>" ] ] ] "bibliografia" => array:2 [ "titulo" => "References" "seccion" => array:1 [ 0 => array:2 [ "identificador" => "bibs0015" "bibliografiaReferencia" => array:3 [ 0 => array:3 [ "identificador" => "bib0020" "etiqueta" => "1" "referencia" => array:1 [ 0 => array:2 [ "contribucion" => array:1 [ 0 => array:2 [ "titulo" => "Metastases to the female tract. Analysis of 325 cases" "autores" => array:1 [ 0 => array:2 [ "etal" => false "autores" => array:3 [ 0 => "M.T. Mazur" 1 => "S. Hsueh" 2 => "D.J. Gersell" ] ] ] ] ] "host" => array:1 [ 0 => array:2 [ "doi" => "10.1002/1097-0142(19840501)53:9<1978::aid-cncr2820530929>3.0.co;2-1" "Revista" => array:6 [ "tituloSerie" => "Cancer" "fecha" => "1984" "volumen" => "53" "paginaInicial" => "1978" "paginaFinal" => "1984" "link" => array:1 [ 0 => array:2 [ "url" => "https://www.ncbi.nlm.nih.gov/pubmed/6322966" "web" => "Medline" ] ] ] ] ] ] ] ] 1 => array:3 [ "identificador" => "bib0025" "etiqueta" => "2" "referencia" => array:1 [ 0 => array:2 [ "contribucion" => array:1 [ 0 => array:2 [ "titulo" => "Vaginal metastases from colorectal cancer" "autores" => array:1 [ 0 => array:2 [ "etal" => false "autores" => array:2 [ 0 => "H.J. Ng" 1 => "E.H. Aly" ] ] ] ] ] "host" => array:1 [ 0 => array:2 [ "doi" => "10.1016/j.ijsu.2013.09.004" "Revista" => array:6 [ "tituloSerie" => "Int J Surg" "fecha" => "2013" "volumen" => "11" "paginaInicial" => "1048" "paginaFinal" => "1055" "link" => array:1 [ 0 => array:2 [ "url" => "https://www.ncbi.nlm.nih.gov/pubmed/24076094" "web" => "Medline" ] ] ] ] ] ] ] ] 2 => array:3 [ "identificador" => "bib0030" "etiqueta" => "3" "referencia" => array:1 [ 0 => array:2 [ "contribucion" => array:1 [ 0 => array:2 [ "titulo" => "Diagnostic accuracy and impact on management of (18)F-FDG PET and PET/CT in colorectal liver metastasis: a meta-analysis and systematic review" "autores" => array:1 [ 0 => array:2 [ "etal" => false "autores" => array:6 [ 0 => "A.M. Maffione" 1 => "E. Lopci" 2 => "C. Bluemel" 3 => "F. Giammarile" 4 => "K. Herrmann" 5 => "D. Rubello" ] ] ] ] ] "host" => array:1 [ 0 => array:2 [ "doi" => "10.1007/s00259-014-2930-4" "Revista" => array:6 [ "tituloSerie" => "Eur J Nucl Med Mol Imaging" "fecha" => "2015" "volumen" => "42" "paginaInicial" => "152" "paginaFinal" => "163" "link" => array:1 [ 0 => array:2 [ "url" => "https://www.ncbi.nlm.nih.gov/pubmed/25319712" "web" => "Medline" ] ] ] ] ] ] ] ] ] ] ] ] ] "idiomaDefecto" => "en" "url" => "/22538089/0000003900000001/v1_202001150636/S225380891930045X/v1_202001150636/en/main.assets" "Apartado" => array:4 [ "identificador" => "7927" "tipo" => "SECCION" "en" => array:2 [ "titulo" => "Interesting images" "idiomaDefecto" => true ] "idiomaDefecto" => "en" ] "PDF" => "https://static.elsevier.es/multimedia/22538089/0000003900000001/v1_202001150636/S225380891930045X/v1_202001150636/en/main.pdf?idApp=UINPBA00004N&text.app=https://www.elsevier.es/" "EPUB" => "https://multimedia.elsevier.es/PublicationsMultimediaV1/item/epub/S225380891930045X?idApp=UINPBA00004N" ]
Consulte los artículos y contenidos publicados en éste medio, además de los e-sumarios de las revistas científicas en el mismo momento de publicación
Esté informado en todo momento gracias a las alertas y novedades
Acceda a promociones exclusivas en suscripciones, lanzamientos y cursos acreditados
The Revista Española de Medicina Nuclear e Imagen Molecular (Spanish Journal of Nuclear Medicine and Molecular Imaging), was founded in 1982, and is the official journal of the Spanish Society of Nuclear Medicine and Molecular Imaging, which has more than 700 members. The Journal, which publishes 6 regular issues per year, has the promotion of research and continuing education in all fields of Nuclear Medicine as its main aim. For this, its principal sections are Originals, Clinical Notes, Images of Interest, and Special Collaboration articles. The works may be submitted in Spanish or English and are subjected to a peer review process. In 2009, it became the leading Spanish journal in the field of Medical Imaging on having an Impact Factor , awarded by the Journal Citation Reports.
Science Citation Index Expander, Medline, IME, Bibliomed, EMBASE/Excerpta Medica, Healthstar, Cancerlit, Toxine, Inside Conferences, Scopus
See moreThe Impact Factor measures the average number of citations received in a particular year by papers published in the journal during the two preceding years.
© Clarivate Analytics, Journal Citation Reports 2022
SRJ is a prestige metric based on the idea that not all citations are the same. SJR uses a similar algorithm as the Google page rank; it provides a quantitative and qualitative measure of the journal's impact.
See moreSNIP measures contextual citation impact by wighting citations based on the total number of citations in a subject field.
See more
Revista Española de Medicina Nuclear e Imagen Molecular (English Edition)

¿Es usted profesional sanitario apto para prescribir o dispensar medicamentos?
Are you a health professional able to prescribe or dispense drugs?
Você é um profissional de saúde habilitado a prescrever ou dispensar medicamentos