Paracoccidioidomycosis is a systemic mycosis caused by Paracoccidioides brasiliensis, and it's endemic in many countries of South America.10 It has been uncommonly reported in AIDS patients until last few years, when it has been more frequently described.3,8,9,11 Recently, Morejón et al. showed that paracoccidioidomycosis and HIV-infected patients (n=53) presented CD4+ count <200cells/μL in 83.7%, lymphadenomegaly in 80%, cutaneous lesions in 66.7% and hepatomegaly in 64.2% of studied cases. Moreover, 80% of patients presented a HIV viral load of >30,000copies/mL of plasma.5 These data suggest that, severe paracoccidioidomycosis in HIV/aids patients is an related to pronounced immunosuppression. However, coinfected patient can present severe and disseminated disease even with CD4+ cell count in the normal range, as observed in this case report.
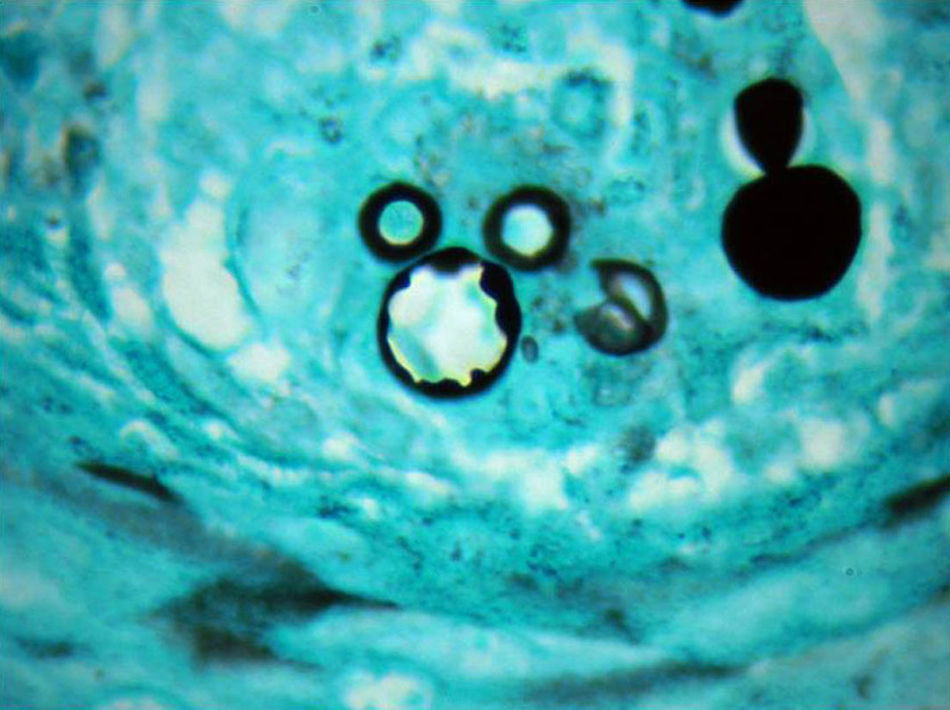
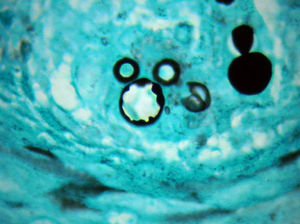
We report the case of a 21-year-old male patient from an urban area of São Paulo state, Brazil, who was referred with a four-month history of fever, weight loss, lymphadenomegaly and cutaneous lesions. He had been an inmate in a state prison, and had inhaled illicit drugs but denied previous medical problems. His clinical presentation was remarkable due to multiple erythematous, infiltrated and ulcerated skin lesions on his face, trunk and limbs (Figs. 1 and 2). He also presented cervical, axillar and inguinal lymphadenomegaly plus hepato-splenomegaly. Biopsy samples from skin lesions and cervical lymph nodes showed diagnostic structures of P. brasiliensis (Fig. 3). Nested-PCR and culture in Mycosel® agar from skin tissue sample were also positive for P. brasiliensis. Chest X-ray and computerized tomography (CT) showed normal to discrete interstitial pulmonary infiltration. Abdominal CT revealed diffuse augmentation of liver and spleen and retroperitoneal lymphadenomegaly. A suspected HIV infection was confirmed by positive serology (ELISA and Western-blot tests). Additional laboratory studies showed CD4+=875cells/μL; viral load >30,000copies and double immunodiffusion test for anti-P. brasiliensis antigen with positive results (IDD=1/16). Hematological study was normal with an erythrocyte sedimentation rate of 42mm/h. Testing of HBV, HCV and HTLV-I was negative.
Treatment was performed with amphotericin B, total dose=1960mg with clinical cure, followed by trimethoprim-sulfamethoxazole 320+1600mg/daily. HAART therapy was not prescribed at that moment and patient did not return for the follow-up.
This reported case is very useful to demonstrate some aspects related to paracoccidioidomycosis and HIV coinfection: although the expected clinical profile of paracoccidioidomycosis in patients bearing the age of this particular case is to present lymphadenomegaly and skin lesion, the exuberance of this clinical presentation, particularly the magnitude of lymphonodes augmentation and number & aspect of skin lesions draw our attention to possible subjacent immunosuppression, in this case an unnoted HIV-infection. It has also been suggested that urban and young patients with severe paracoccidioidomycosis might be routinely screened for HIV infection. Also important is the fact that patients with paracoccidioidomycosis and HIV despite clinical severity can present discrete pulmonary involvement or no detectable involvement at all and, that amphotericin B deoxycholate is still the first choice in severe paracoccidioidomycosis despite its side effects.1,2,4,7
As the HIV infection is spreading to the interior of many countries in South and Central America, the possibility of HIV associated to endemic diseases prevalent in such countries must be considered in our clinical reasoning.6