To verify the effectiveness of acupuncture using Traditional Chinese Medicine tools (pulse and tongue), for several clinical conditions, in the public health service. This is a retrospective clinical study running in a single healthcare referral center in Brazil. Seventy-two patients participated (retrospective review of medical records). Acupuncture treatment was provided at the referral center.
Material and methodsThe main outcome measures included the patients' main complaints, sex, pain classification using the verbal rating scale (VRS), observation of the tongue (color change and presence of coating), and pulse palpation, which were used to assess the most affected San Jiao (SJ). The patients' energy status was classified by the acupuncturist as deficient or excessive in the first and last treatment sessions. Chi-squared test, Fisher's exact test, and binomial proportion test were used for comparisons of data.
ResultsPatients experienced significant analgesia at the end of treatment than that before treatment (p < 0.01). At the end of treatment, the tongue showed a greater amount of coating in patients with a deficient energy state (p = 0.02) than in those with excess energy (p = 0.70); however, there was no difference in the tongue color (p > 0.05) between both patient groups. Pulse analysis showed an initial difference according to energy status, with reduced pulse in a deficiency state (p < 0.05), and balanced pulse at the end of the treatment (p = 0.48).
ConclusionsAcupuncture is a therapeutic option for pain control and improved energy balance.
Verificar la eficacia de la acupuntura utilizando herramientas de la Medicina Tradicional China (pulso y lengua), para diversas condiciones clínicas, en el servicio público de salud. Se trata de un estudio clínico retrospectivo realizado en un único centro de referencia sanitaria de Brasil. Participaron 72 pacientes (revisión retrospectiva de las historias clínicas). El tratamiento de acupuntura se realizó en el centro de referencia.
Material y métodosLas principales medidas de resultado incluyeron las principales quejas de los pacientes, el sexo, la clasificación del dolor mediante la escala de calificación verbal (VRS), la observación de la lengua (cambio de color y presencia de recubrimiento) y la palpación del pulso, que se utilizaron para evaluar el San Jiao (SJ) más afectado. El estado energético de los pacientes fue clasificado por el acupuntor como deficiente o excesivo en la primera y la última sesión de tratamiento. Para comparar los datos se utilizaron la prueba de la chi-cuadrado, la prueba exacta de Fisher y la prueba de la proporción binomial.
ResultadosLos pacientes experimentaron una analgesia significativa al final del tratamiento que antes del mismo (p < 0,01). Al final del tratamiento, la lengua mostraba una mayor cantidad de recubrimiento en los pacientes con un estado energético deficiente (p = 0,02) que en los que tenían un exceso de energía (p = 0,70); sin embargo, no hubo diferencias en el color de la lengua (p > 0,05) entre ambos grupos de pacientes. El análisis del pulso mostró una diferencia inicial según el estado energético, con un pulso reducido en un estado deficitario (p < 0,05), y un pulso equilibrado al final del tratamiento (p = 0,48).
ConclusionesLa acupuntura es una opción terapéutica para el control del dolor y la mejora del equilibrio energético.
Pain is a warning symptom and has a negative impact on people's lives. Acupuncture is a useful relief option because of its analgesic effect.1
Numerous randomized clinical trials, systematic reviews, and meta-analyses have confirmed the therapeutic effectiveness of acupuncture for several diseases prevalent worldwide.2–5
In light of existing evidence and the increase in the demand for this therapy, the World Health Organization (WHO) recently published the WHO Traditional Medicine Strategy: 2014–2023,6 which evaluated the rates of worldwide use of integrative and complementary practices, research investment in the area, the characteristics of its consumption and institutionalization in health services in the last decade, as well as establishing the necessary goals for its expansion in Primary Health Care for the following decade.7
Synergistically, Traditional Chinese Medicine (TCM) treatment starts with patient observation, auscultation/olfaction assessment, investigation, and palpation.8–9 In TCM, the pulse and tongue are important for accurate diagnosis.
The evaluation of radial pulse involves palpation of both the wrists to check the state of the body, internal organ systems, and meridian systems.10 This pulse evaluation can also inform practitioners on the energy state of the organs, including the Upper Jiao, comprising the Heart and Lungs; the Middle Jiao, comprising the Spleen/Stomach and Liver/Gallbladder; and the Lower Jiao, comprising the Kidneys/Bladder.11
With the tongue observation, according to the principles of TCM, it is possible to analyze the physiological functions of and pathological changes in the human body. The coating of the tongue reflects the nature and location of the pathogenic factors and often indicates the condition of some organs. Therefore, meticulous observation of any alteration of the tongue coating is particularly necessary for the diagnosis and evaluation of disease progression.12
The energetic alterations of the Zang Fu can manifest as a lack or emptiness of Qi and/or Xue, leading to symptoms of fullness or emptiness in the energy channel, or by the entry of one or more negative energies, such as heat, cold, wind, humidity, and/or dryness; these energy imbalances inevitably cause deficiency- or excess-associated symptoms.13
TCM-based treatment plans are formulated according to the diagnosis, and thus tongue observation, pulse palpation, and the assessment of an individual's energy state (deficiency or excess) must be included.14
Owing to the increasing popularity of alternative practices, this study aims to verify the effectiveness of acupuncture using TCM tools (pulse and tongue) in the treatment of various clinical conditions in the public health service.
Materials and methodsStudy designThis retrospective clinical study analyzed data obtained from the medical records of patients who underwent acupuncture treatment from May 2018 to May 2019 at a primary healthcare referral center in Brazil. The acupuncture treatment was administered by a team of specialist acupuncture therapists with ≥3 years of experience. The study was conducted in accordance with the principles of the Declaration of Helsinki and under the approval of the Research Ethics Committee of FOP/UNICAMP# 60121116.1.0000.5418.
PatientsWe reviewed the medical records of 72 patients. The inclusion criteria were: age > 18 years, treated with acupuncture at the primary referral center, and availability of complete data in their clinical records. The exclusion criteria were: incomplete medical records and age < 18 years. All included patients had been treated with manual acupuncture, using a 0.25 × 30-mm Dong Bang® needle, with prior local sterilization using 70% alcohol.
Outcome measuresThe records included the following information: the main patient's complaint, sex, age, number of acupuncture sessions, verbal rating scale (VRS) assessment, pulse palpation and tongue observation, and the energy status assessed by the acupuncturist (deficient or excessive) at the first and last treatment sessions.
The main complaint of the patients was classified according to the reason for seeking acupuncture treatment.
Pain assessmentThe VRS, which rates pain intensity on a scale of 0 to 10, was used for the assessment of pain intensity in the first (before treatment; initial VRS) and last (after treatment; final VRS) acupuncture sessions, regardless of the number of sessions attended by the patients.15 The patients rated pain intensity—with the absence of pain being rated as zero and maximum pain intensity rated as ten—by answering the following question: “How much pain do you feel at this time? Rate it on a scale of 0 to 10, wherein 0 corresponds to no pain and 10 corresponds to maximum pain.”
Tongue observationThe tongue observation involved the patients showing their tongue to the acupuncturist, who assessed the tongue's color and classified it as follows: pink indicated a normal status, while a purple, reddish, or pale color indicated an alteration. The coating of the tongue was observed for its presence or absence. This information was observed at the beginning of the first and the last session of the complete treatment, regardless of the number of sessions attended by the patients.
Pulse examination and San JiaoPulse palpation was also performed, which was verified in the radial artery of both the right and left wrists, to assess its characteristics; in this study, priority was given to the position (anterior, middle, posterior), and strength of the pulse.15,16 Position was useful to evaluate the Cun, Guan, and Chi in the radial artery of the wrist—Cun corresponds to Upper Jiao (Heart/Lung organs), Guan corresponds to Middle Jiao (Spleen/Stomach, Liver/Gallbladder), and Chi corresponds to Lower Jiao (Kidneys/Bladder).11,16
In this study, to diagnose which San Jiao (SJ; Upper, Middle, or Lower) was more energetically affected, the weaker position on the wrist was noted. Therefore, the pulse was analyzed as follows: the participant was seated in front of the acupuncturist, and the palm of their hands rested on their knees, facing up. The pulse was always checked at rest. First, the Guan (Liver; the segment that covers the styloid apophysis, above the point P8) was checked with the middle finger of the acupuncturist; then, with the index and ring fingers, the Cun (Heart; the segment between the base of the thumb and the styloid apophysis, above the point P9) and Chi (rim; below the styloid apophysis, above the point P7) were assessed.16 The Cun, Guan, and Chi positions correspond to the positions of the Upper SJ (Heart and Lung), Middle SJ (Liver and Spleen), and Lower SJ (Bladder and Kidney), respectively.
When an abnormality was noticed in any region of the pulse, a uniform pressure was applied to the three regions; thereafter, each region was palpated separately to make a comparison and to obtain an accurate impression of the pulse as a whole. This process was verified because strength involves a subjective judgment about the pulse strength in the blood vessel, as detected by the acupuncturist's fingers.16
For the pulse analysis in this study, the pulse strength was rated from 1 to 3, for each of the nine positions, with a score of 1 indicating an absence of strength, and 3 indicating maximum strength in each position; thus, the total pulse (in both arms) was rated from 6 to 18. An increasing score indicated increasing energetic strength, considering both the right and left sides.
Assessment of emptiness and fullness statesThrough this pulse analysis, we were able to identify the most affected San Jiao (which in this study corresponds to the one with the lowest strength) at the beginning of the first and last sessions of the complete treatment, regardless of the number of sessions attended by the patients.
The states of emptiness and fullness were evaluated by the acupuncturist at the beginning of the first and last treatment sessions, considering the pulse variables, with values closer to 1 indicating emptiness and those closer to 18 indicating fullness. The emptiness and fullness states were also investigated based on anamnesis (which provided other data on the patient's general energy status), observation of the patient (face, hair, nails, etc.), auscultation and examination of olfaction, and tongue observation.17
Statistical analysisThe scores obtained were organized in tables and figures, and statistically analyzed with Graph Prism 7.0 software (GraphPad Software Inc., San Diego, CA, USA). An alpha level of 0.05 was considered significant. The chi-squared, Fisher's exact, and binomial proportion tests were used for comparisons of data.
ResultsThe majority of patients were women who were diagnosed with deficiency, with the most prevalent conditions being temporomandibular disorder (TMD) and sleep bruxism (SB). Before treatment, Upper Jiao was the most affected in the energy deficient group (p = 0.02), while at the end of the treatment, there was no difference between groups (p > 0.05) (Table 1).
Sex, the chief complaint, and SJ affected the correlation between deficiency and excess.⁎
| Deficiency(n=56) | Excess (n=16) | Overall (n=72) | Chi-squareOr exactFisher (p) | |||
|---|---|---|---|---|---|---|
| Gender | Female | 51 | 13 | 64 | 0.36 | |
| Male | 5 | 3 | 8 | |||
| Major Complaint | DTM /Bruxism | 25 | 6 | 31 | 0.76 | |
| Headache /Cervicalgia | 10 | 3 | 13 | |||
| Face Pain | 7 | 4 | 11 | |||
| Anxiety | 7 | 2 | 9 | |||
| Paralysis/Paresthesia /Salivation | 7 | 1 | 8 | |||
| SJ Affected initial | Upper Jiao | No | 23 | 12 | 35 | 0.02 |
| Yes | 33 | 4 | 37 | |||
| Middle Jiao | No | 49 | 14 | 63 | 1.00 | |
| Yes | 7 | 2 | 9 | |||
| Lower Jiao | No | 7 | 4 | 11 | 0.24 | |
| Yes | 49 | 12 | 61 | |||
| SJ Affected final | Upper Jiao | No | 33 | 10 | 43 | 1.00 |
| Yes | 23 | 6 | 29 | |||
| Middle Jiao | No | 47 | 15 | 62 | 0.44 | |
| Yes | 9 | 1 | 10 | |||
| Lower Jiao | No | 13 | 4 | 17 | 1.00 | |
| Yes | 43 | 12 | 55 |
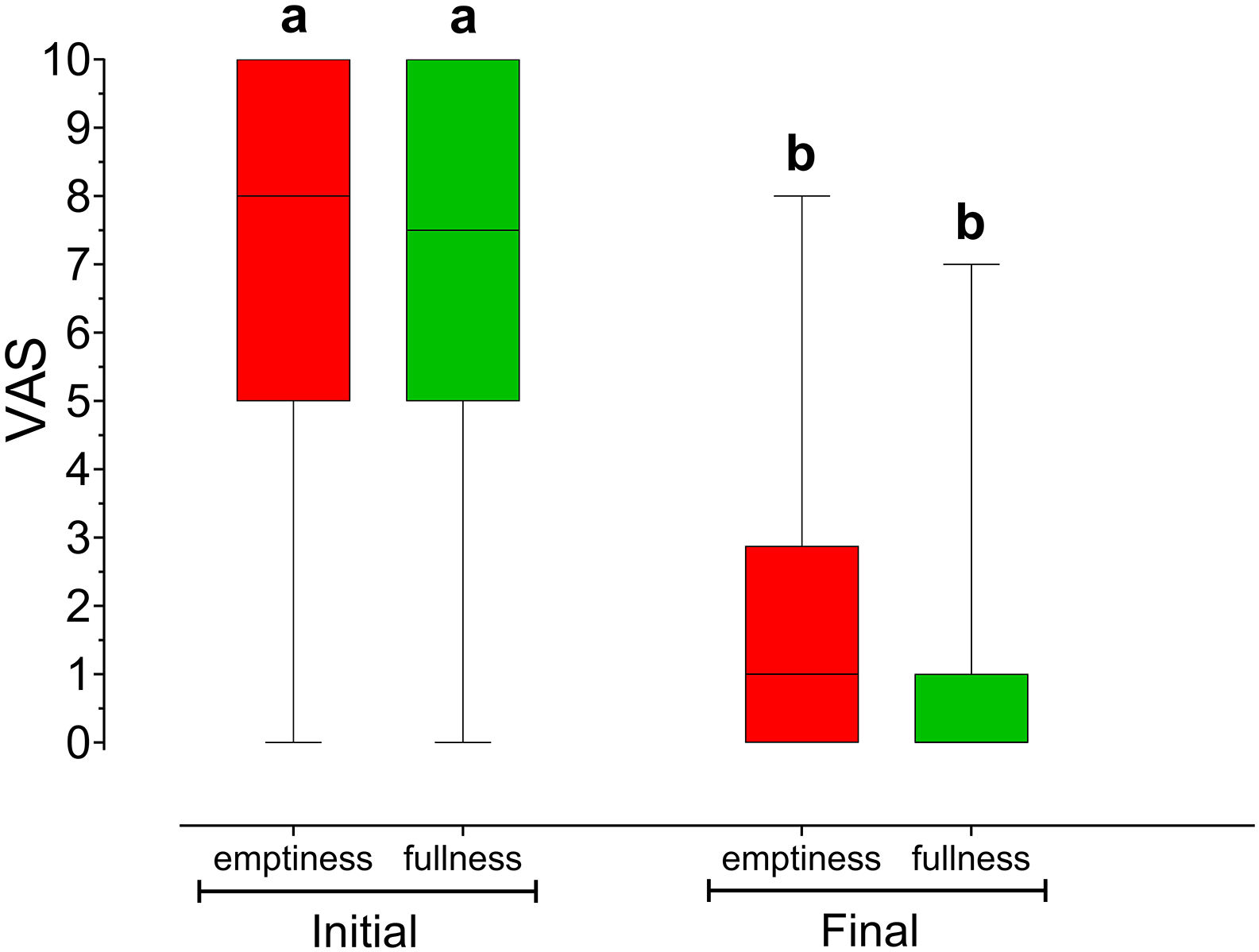
At the beginning of treatment, pain variable was equal between the groups (p > 0.99), when comparing between individuals diagnosed with deficiency and excess. At the end of treatment, there was a similar reduction in pain (p < 0.01) in both groups (p = 0.99). Fig. 1 presents the results of VRS analysis according to energy status.
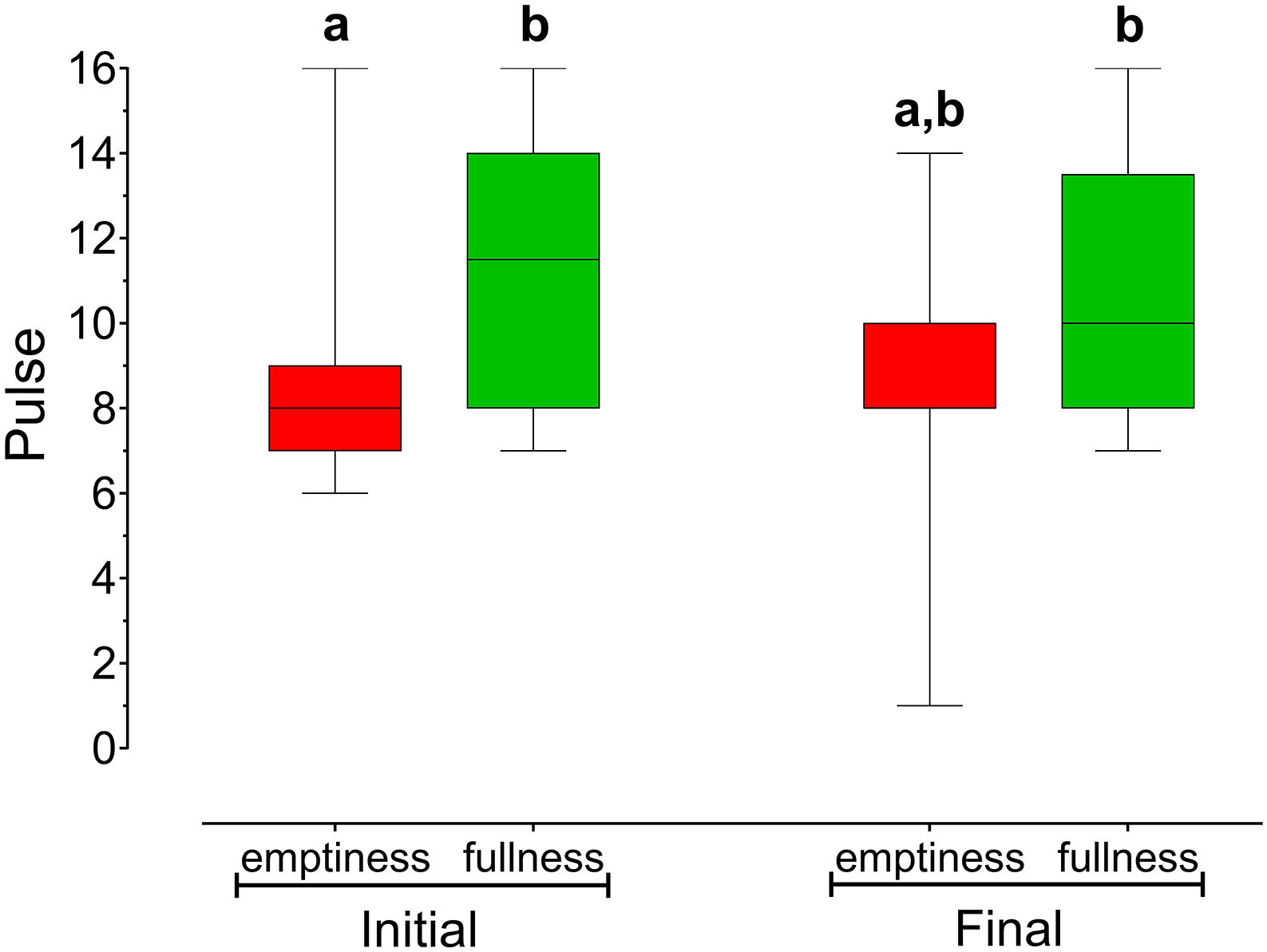
Initially, before treatment, the patient groups differed according to the energetic states of emptiness and fullness, as assessed by pulse palpation (p = 0.23)—the pulse intensity was stronger in patients with an energy excess state than in those with a diagnosis of energy deficiency. After treatment, the pulse intensity was balanced between the two groups (p = 0.48) (Fig. 2).
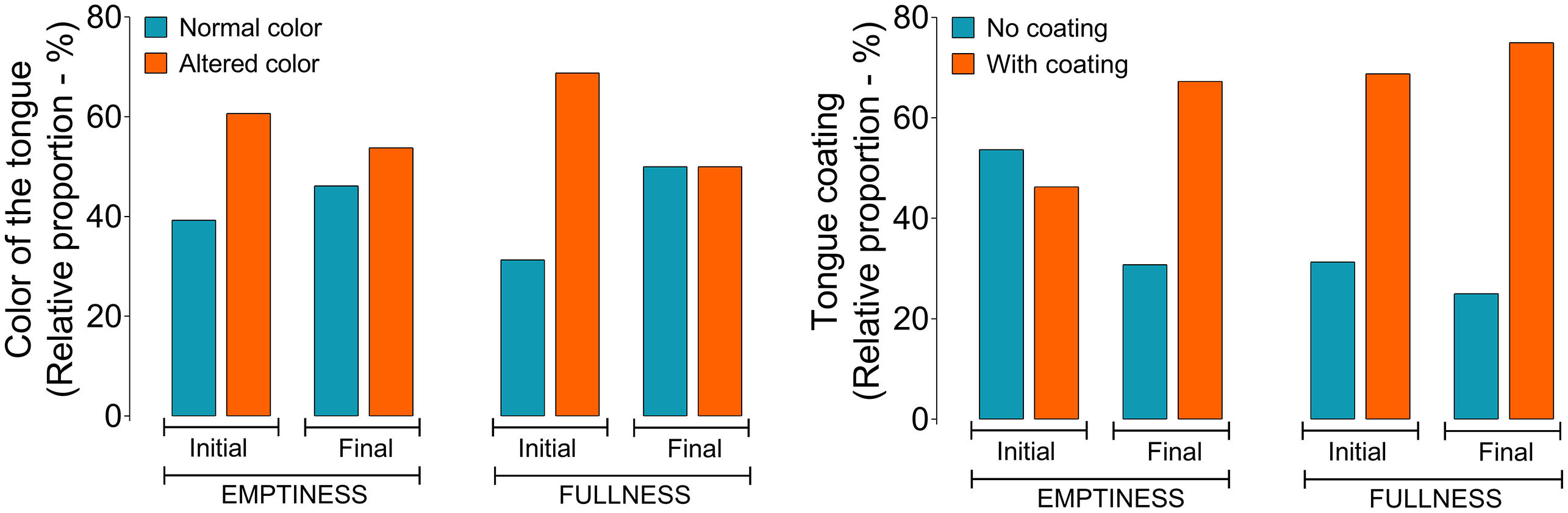
Fig. 3 shows that the majority of the patients in both groups had similarly altered coloration of the tongue (60.7% of patients were diagnosed with emptiness and 53.8% were diagnosed with fullness) (p = 0.55), and this finding persisted even after treatment (p = 0.79).
The presence of coating on the tongue at the beginning of treatment was verified in 46.3% of the patients in the empty state; at the end of treatment, this proportion increased to 68.8% (p = 0.02). In patients with fullness, the presence of a coating did not significantly change after treatment, comprising 67.3% of patients at the beginning and 75% at the end of treatment (p = 0.70).
DiscussionThe present study demonstrated the effectiveness of acupuncture treatment administered at a public service center for different complaints of the head and neck. Patients with both deficient and excess energy benefited from acupuncture treatment, which involved diagnostic methods such as pulse and tongue analyses. The study results show that patients reported significant analgesia at the end of the treatment (measured by the VRS). Thus, this study confirms the efficacy of acupuncture in reducing pain,2,5,18 but with an approach involving the public system.
In this study, the acupuncturist's diagnosis was based on energy deficiency or excess, since according to Yamamura (2001),19 any energy change in the Zang Fu—whether it is an increase (excess) or decrease (deficiency)—manifests as pathologic symptoms in the organs/viscera, or organic changes, which are the fundamental causes for the onset and development of diseases.
The acupuncturist's diagnosis included more information, such as anamnesis data on the patients' preference for flavors, habits, sleep, or stool and urine characteristics. On observing the face, skin, hair, nails, as well as the noises and smells emanating from the patients' body, in correspondence with pulse assessment and tongue observation data, a very close relationship was identified with the states of emptiness or fullness; this observation confirms the importance of this information for a good diagnosis and treatment follow-up.
This cohort included mostly women with energy deficiency, similar to those included in other studies.20,21,22 The observation of these patients, who exhibited more energy deficiency patterns than they did energy excess ones, has shown that Qi deficiency manifests as long-term internal pathologies, resulting in chronic diseases.23 According to Zotelli et al. (2018), participants who were diagnosed with TMD in their study had this pathology for an average of 9.2 years, along with an energy status indicative of Qi deficiency, confirming the relationship between chronicity and Qi deficiency.24
In both study groups (energy deficiency and excess), the VRS score was lower after acupuncture treatment than before treatment, demonstrating the effectiveness of acupuncture in reducing self-reported pain (p < 0.01). This analgesic effect can probably be explained by the micro-inflammation caused by the needle penetration, which promotes the natural production of serotonin, enkephalin, and endorphin. The release of these neurotransmitters blocks the propagation of pain stimuli, impairing their perception by the brain. Therefore, the body responds faster, decreasing the symptom intensity and inducing pain relief. Acupuncture stimulates the blood circulation dynamics due to microdilation and regional relaxation; promotes the release of hormones, such as cortisol and endorphins; increases host resistance through the stimulation of the hypothalamus, pituitary, and other glands important for systemic recovery; normalizes bodily functions; and stimulates metabolism in different organs.25,26
The presence of such an energetic state was also verified via pulse palpation, with greater intensity in patients diagnosed with fullness than in those diagnosed with emptiness (p = 0.23). After treatment, the pulse intensity was balanced in both groups (p = 0.48). This finding demonstrates the efficiency of acupuncture in normalizing patients' energy balance, which manifests as decreased pain and SJ balance. Although, the Upper Jiao was initially the most affected system in patients with a sense of emptiness, whereas after treatment, a balance was regained in both groups. This finding demonstrated that the treatment might have contributed to decreasing the Upper Jiao in the empty state. Considering that these patients sought the service with head and neck changes and probably experienced this false heat rising to the head, the basis would be the Yin emptiness of the Lower Jiao, which, despite these treatments, did not increase the energy in the groups, leading to a sufficient balance in lessening or ceasing the pain.
O'Brien et al. (2013) reported that changes in the radial pulse, evaluated by TCM professionals after a single visit, seem to coincide with changes in cardiovascular parameters.27 Pulse evaluation has been used in TCM for years, and it reflects a movement of vital energy—Qi—and blood. This means that pulses indicate the places where the blood is always concentrated, which circulates in a manner corresponding to an individual's vital energy. Therefore, pulse diagnosis involves the understanding of the transformation of vital energy and blood into the Meridians; it is also associated with the understanding of the physiology and pathology of the Zang Fu organs in the body. Based on this concept, the Yang and Yin in the body—a deficiency or excess of vital energy (Qi)—are evaluated to accurately diagnose syndromes; this evaluation is achieved by selecting the Meridians and acupuncture points and by applying the appropriate corresponding treatment.28 Thus, compiling pulse data by SJ was practical and sensitive for assessing these changes in energy states and to monitor the effects of acupuncture.
There was a greater amount of tongue coating in patients with a diagnosis of emptiness at the end of the treatment, which demonstrates the effectiveness of acupuncture and increased treatment response in the emptiness states. However, the tongue color was not sensitive to changes in any of the groups in the present study.
Tongue and pulse evaluation, commonly used in TCM, are described in the literature as the window for the diagnosis of pathologies because the tongue is rich in vascular, lymphatic, and neural supplies (the vagus and glossopharyngeal nerve; cranial nerves IX and X).29 This type of diagnosis is extremely important in clinical practice, with the tongue being an integral part of not only the digestive system, but also the respiratory system, and in direct contact with the external environment. Moreover, saliva, microorganisms, and food particles remain in the lining of the tongue, and reflect multiple factors, such as eating habits, lifestyles, and the microecological environment. Thus, Han et al. (2016) used tongue evaluation as a potential method for cancer screening; they used tongue images and analyzed the coating and the characteristics of the tongue, such as color, moisture, oiliness, fissures, and ecchymosis. The authors of this study reported early diagnoses after comparing the differences between healthy people and cancer patients, concluding that tongue diagnosis can provide a potential avenue for screening in TCM.30
In the present study, we focused on the tongue color and the presence or absence of a coating, demonstrating the possibility of evaluation and monitoring, as the presence of a coating demonstrated treatment effectiveness, increased energy for patients in states of emptiness, and balance for those in an energetic state of fullness.
This study could be conducted because of the initiative of volunteer acupuncturist therapists, between the State University of Campinas and the municipality of Piracicaba, São Paulo, Brazil. Because, even in Brazil, which has public policies of integrative and complementary practices, the municipalities are still in the initial stages. More investments must be made in public services, because as verified in the present study, acupuncture can provide the benefits of pain relief in various clinical conditions.
Although the effectiveness of pain reduction through acupuncture treatment has been demonstrated in this study, we consider the VRS-based assessment of pain a limitation because it was self-reported and, therefore, a subjective measure. The pulse palpation method used for the interpretation of SJ, which was used in the analysis of the results in this study, was innovative; however, the absence of previous reports that used SJ for the diagnosis and verification of treatment results made further comparisons impossible.
However, this study contributes to systematizing a classical and ancient knowledge, using the data of pulse and tongue diagnoses for the evaluation of treatment results. Thus, it is possible to demonstrate the effectiveness of acupuncture therapy in pain reduction and, in a certain way, energy balance in attended head and neck complaints.
The importance of continuing this work is clear, with acupuncture care being continued in the public health system. The effectiveness of acupuncture action on pain reduction, in relation to other analgesia methods, should be verified through a prospective study.
ConclusionAcupuncture is a therapeutic option for controlling pain caused by orofacial problems. This study contributes to the compiling and systematizing of public data to support acupuncture as a pertinent therapeutic modality.
Disclosure of interestThe authors declare no conflicts of interest.
Funding detailsThis study was not funded.
Data confidentialityThe authors declare that they followed the workplace protocols on the publication of patient data and that all participants received sufficient information and provided their written informed consent.
Right to privacy and informed consentAll patients and/or subjects in this study provided a written informed consent to the authors.
This document is in the possession of the correspondence author.
Contributed to conception, design, data acquisition and interpretation, performed all statistical analyses, drafted and critically revised the manuscript and final approval.
Contributed to drafted and critically revised the manuscript and final approval.
Contribution: performed all statistical analyses, drafted and critically revised the manuscript and final approval.
Contribution: effective scientific and intellectual participation in the study; study conception and design; manuscript writing; critical review and final approval.







 0.05. *VRS, verbal rating scale.' title='Initial and final VRS, and correlation between deficiency and excess. **Fisher's exact testa and Chi-squared testb, P > 0.05. *VRS, verbal rating scale.'/>
0.05. *VRS, verbal rating scale.' title='Initial and final VRS, and correlation between deficiency and excess. **Fisher's exact testa and Chi-squared testb, P > 0.05. *VRS, verbal rating scale.'/>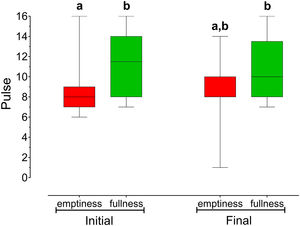 0,05. *VRS, verbal rating scale.' title='Initial and final pulse, correlation between deficiency and excess. * Fisher's exact testa and Chi-square testb, P > 0,05. *VRS, verbal rating scale.'/>
0,05. *VRS, verbal rating scale.' title='Initial and final pulse, correlation between deficiency and excess. * Fisher's exact testa and Chi-square testb, P > 0,05. *VRS, verbal rating scale.'/>