The purpose of this clinical study is to demonstrate the effect of classical acupuncture on the Carpal Tunnel Syndrome (CTS) and the relationships that integrate the view of classical acupuncture treatment with current anatomical-physiological knowledge.
DesignA clinical study was carried out with patients with CTS.
SettingThe treatments were conducted in a private healthcare practice by a licensed acupuncturist.
ParticipantsThe five participants presented symptomatology for a period of no less than 6 months, had been diagnosed through electromyography, and additionally showed a positive test for Phalen's maneuver test. All the patients had surgical indications.
InterventionsClassical Chinese acupuncture was applied during a cycle of treatments.
Main measurementsThe Visual analog scale (VAS) was used to assess the level of discomfort regarding daytime paresthesia, nighttime paresthesia, pain, decrease in strength, and a proposed converted value of pressure pain threshold.
ResultsAll the parameters showed significant improvement. The mean difference was negative for pain (−7,4 points), daytime paresthesia (−5,2 points), nighttime paresthesia (−6,2 points), and loss of strength (−4,6 points), whereas the estimation for the pressure pain threshold was positive (+0,683 kgf/cm2).
ConclusionsIn the analysis of the results obtained through the classical acupuncture therapy, all parameters showed an improvement, which suggests and supports evidence of clinical efficacy on the CTS.
El propósito de este estudio clínico es demostrar el efecto de la acupuntura clásica en el síndrome del túnel carpiano (STC) y las relaciones que integran la visión del tratamiento de acupuntura clásica con el conocimiento anatómico-fisiológico actual.
DiseñoEstudio clínico con pacientes con STC.
EmplazamientoLos tratamientos fueron guiados en una clínica privada de salud por un acupunturista acreditado.
ParticipantesLos cinco participantes habían tenido síntomas durante un período no inferior a 6 meses, habían sido diagnosticados por electromiografía y, además, mostraron una prueba positiva para la maniobra de Phalen. Todos los pacientes fueron indicados para cirugía.
IntervencionesSe aplicó la acupuntura china clásica durante un ciclo de tratamientos.
MedicionesSe utilizó la Escala Visual Analógica (EVA) para evaluar el nivel de malestar en relación con la parestesia diurna, parestesia nocturna, dolor, disminución de la fuerza y un valor umbral de dolor por presión convertido propuesto.
ResultadosTodos los parámetros mostraron una mejora significativa. La diferencia de medias fue negativa para dolor (−7,4 puntos), parestesia diurna (−5,2 puntos), parestesia nocturna (−6,2 puntos) y pérdida de fuerza (−4,6 puntos), mientras que la estimación de la presión umbral del dolor fue positivo (+0,683 kgf/cm2).
ConclusionesEn el análisis de los resultados obtenidos mediante la terapia de acupuntura clásica, todos los parámetros mostraron una mejoría que sugiere y respalda la evidencia de la eficacia clínica en el STC.
The Carpal Tunnel Syndrome (CTS) is a peripheral neuropathy and the most common of the compressive neuropathies of the upper limb.1
The carpal tunnel is the space that extends along the palmar aspect of the wrist; it is surrounded and limited by the scaphoid tubercle and the trapezius in the radial aspect, by the hamate halo and by the pisiform bone in the ulnar aspect, and by the transverse ligament of the carpal on the palmar aspect. Through the tunnel passes the superficial and deep flexor tendons of the fingers and the median nerve.2
In this syndrome, the median nerve is compressed in the wrist region due to the reduced carpal tunnel space or the increase in the size of any of the nine structures that cross it.3
There is a relationship between this syndrome and repetitive manual work4 and so, it may be considered an occupational disease. However, CTS has also been associated with diabetes, obesity, pregnancy, and menopause,5 as well as with hypothyroidism.6 It predominantly affects the female gender; however, it seems that an equivalent risk between genders exists when the occupational exposure is identical.7,8
Symptomatology is diverse, including paresthesia, hypoesthesia, anesthesia, decreased strength and coordination in the first finger of the hand, eventually leading to thenar muscle atrophy, interfering with the patient's ability to deal with daily activities.9
In conventional medicine, its treatment consists of several conservative methods, which include drugs, physiotherapy, and the modification of daily and professional activities. In cases where there is no favorable response to these treatments, or when there is muscular atrophy or denervation, surgery may be used.10 However, available data suggest that there are long-term enduring abnormalities in a large percentage of patients after undergoing surgery,11 with the rate of re-occurrence of symptoms as high as 57%.12
In classical traditional Chinese medicine (CTCM), the carpal tunnel disorder may be understood according to two perspectives: 1) the symptomatic perspective, centered on paresthesia and atrophy; and 2) the traditional Chinese perspective of tendon pathology, which in ancient times included the nerves.
Paresthesia is defined in the classic Chinese medical literature, under the term: “insensitivity” (不仁 bù rén or 麻木 má mù), and its causes can be:
- •
Failure to transmit nerve impulses. Described in antiquity as: “The failure of the movement of defensive energy.”13
- •
Poor nutrition and failure in blood irrigation, described in the text “The Elementary Questions” as: “When the nutritive Qì is empty, there is numbness.”14
- •
Chronic injury of the nervous and circulatory system, described in antiquity as: “When there is no pain, but there is swelling, the disease has lingered and gone deep. The circulation of the nutritive and the defensive is rough and the channels and collateral occasionally relax. Therefore, they are obstructed. The skin lacks nutrition. Therefore, there is numbness.”15
- •
Neurasthenia, described in antiquity as: “When the body frequently is startled and fearful, and tendons and vessels are obstructed, it generates numbness disease.”16
- •
Diabetes, described in antiquity as: “When there is heat in the Spleen Qì, the Stomach dries and there is thirst. There is numbness in the muscles and the flesh, manifesting the atrophy of the flesh.”17
- •
Prolonged contraction of cold, described as: “When cold and bì (block) become diseases, and are retained without being eliminated, occasionally there is pain and numbness in the skin”.18
Concerning tendon atrophy, classical literature refers to many causes, however the most common is inflammation (heat) and malnutrition (dryness) in tendons: “When there is heat in the Liver Qì, the Gallbladder drains and the mouth is bitter and tendons and membranes dry. When the tendons and membranes dry, the tendons become tense and constrict, manifesting as tendons atrophy.”17
In the case of neuropathies, nerve damage is classified in traditional Chinese medicine as “tendon injury”. In the theory of traditional Chinese medicine, there is a particular histological categorization, known as: “the five bodies” (五 體 w¿ t¿). The five categories of tissues are: 1) Skin and hair; 2) Vessels; 3) “Flesh” or muscles and fat; 4) Tendons and membranes and 5) Bones and bone marrow.
In CTCM, the term “tendons” (筋 jīn) is comprehensive and includes various forms of connective, muscular, and nervous tissue. The “tendons” are organized in 12 strings or chains of muscular, nervous, tendinous and ligamentous tissues, which are called the “tendinous channels” (經筋 jīng jīn). In the theory of the channels and collateral vessels of traditional Chinese medicine, there are also 12 vessel systems, each associated with an internal organ. Of these channels, six are associated with the hands and the remaining six with the feet. The “tendinous channels” are associated with the 12 regular channels and collateral, according to the path of both structures. For example, the “Tài Yīn Lung channel” of the hand circulates from the abdomen and chest to the first finger of the hand. The “hand Tài Yīn tendon channel” circulates from the first finger to the thorax, and there is a coincidence in its path.
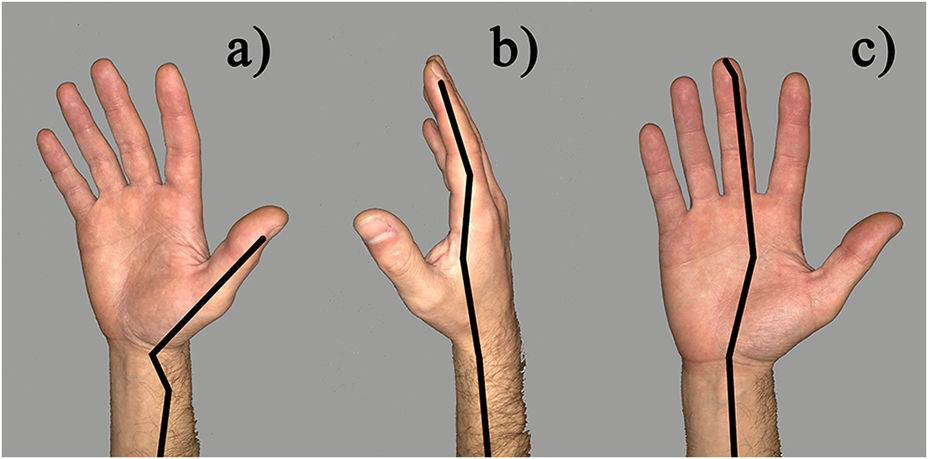
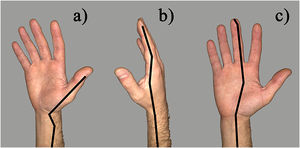
In CTS, the affected areas mainly concern the path of three “tendon channels”19 (see fig. 1):
- a)
The “hand Tai Yin tendon channel”, with its path starting at the first finger it reaches the thenar eminence and passes through the radial and palmar aspect of the wrist;
- b)
The “hand Yang Ming tendon channel”, with its path from the second finger to the first interosseous muscle and the radial and dorsal aspect of the wrist;
- c)
The “hand governor of the Heart tendon channel”, with its path from the third finger, passing through the center of the palm and the central region of the wrist in its palmar aspect.
Traditional Chinese medicine has several approaches:
- •
Acupuncture at the affected site itself or “Use [the site] of pain as [a cavity of] transport”;19
- •
Acupuncture at distal places;
- •
The application of “decoctions, poultices, fire, moxa, and puncture”.
The purpose of this clinical study is to demonstrate the effect of classical acupuncture in this syndrome, as well as the relationships that integrate the view of classical acupuncture treatment with current anatomical-physiological knowledge.
Material and methodsFive patients were studied in this clinical study. All patients had a medical diagnosis of CTS confirmed by electromyography. Additionally, patients showed positive for the Phalen's maneuver diagnostic test, and all patients had symptomatology for a period longer than 6 months.
The study followed the ethical guidelines mandated by the authors' respective licensing bodies regarding experimental techniques and procedures, which follows The Code of Ethics of the World Medical Association (Declaration of Helsinki) for experiments involving humans. Written informed consent was obtained from each patient.
Concerning the evaluation method, the patients were asked to describe the degree of discomfort on a scale of 0-10 (VAS), where 0 represents the absence of discomfort and 10 represents the maximum discomfort, for daytime paresthesia, nighttime paresthesia, pain, and decrease in strength. The status of the patient's complaints related to CTS in these four parameters was measured before and after a cycle of 5-6 acupuncture treatments.
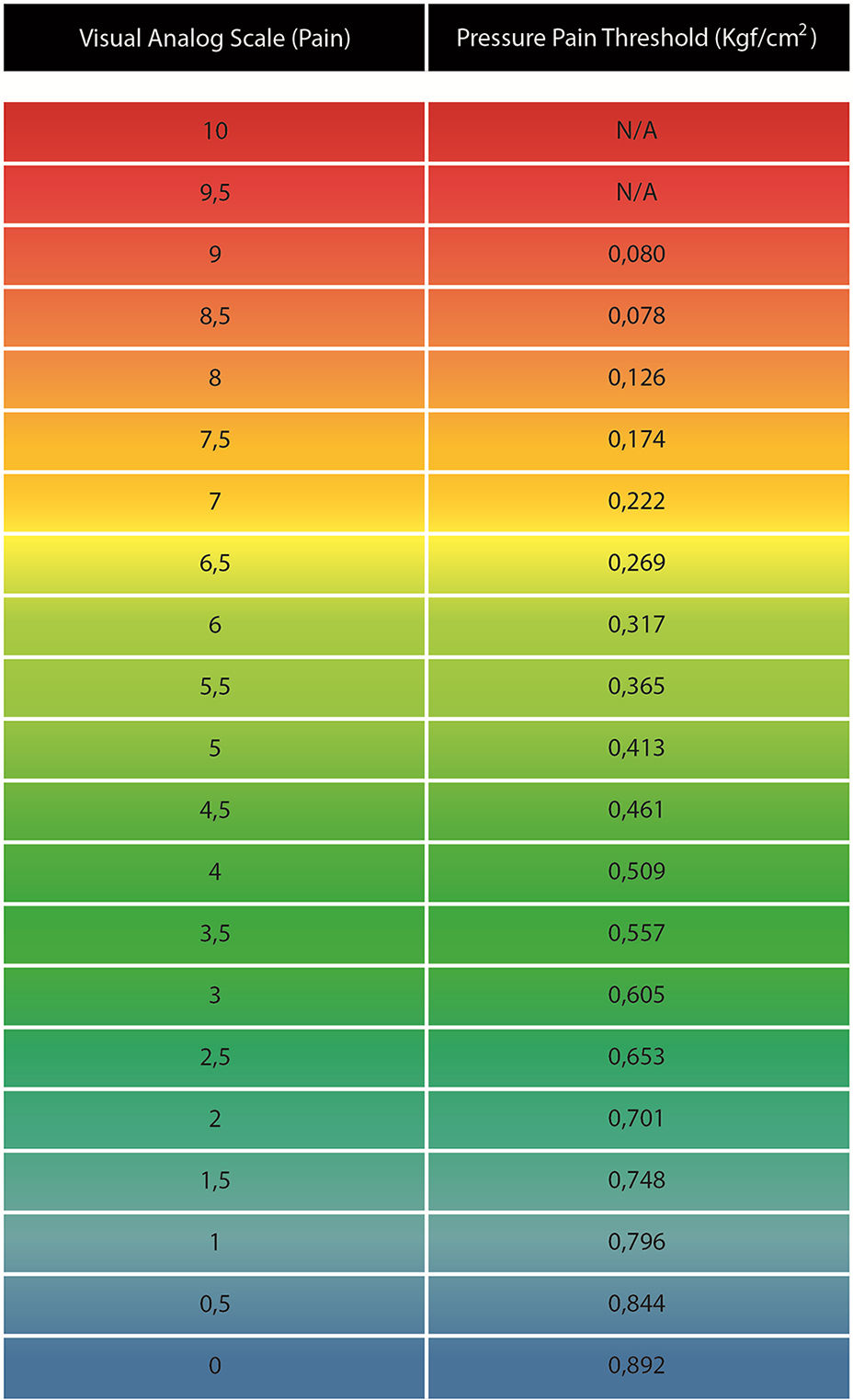
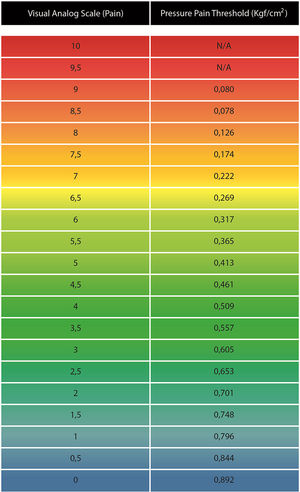
According to a study by Seca, Miranda20 using acupuncture, the decrease of pain levels assessed by the VAS is correlated to improvements in the pressure pain threshold in patients with rheumatoid arthritis of the hand. This allows us to propose that pain levels assessed by the VAS on CTS can be approximately quantified in kgf/cm2, and estimate the improvement of the pressure pain threshold for patients receiving the acupuncture treatment in this study. The scale is presented in fig. 2.
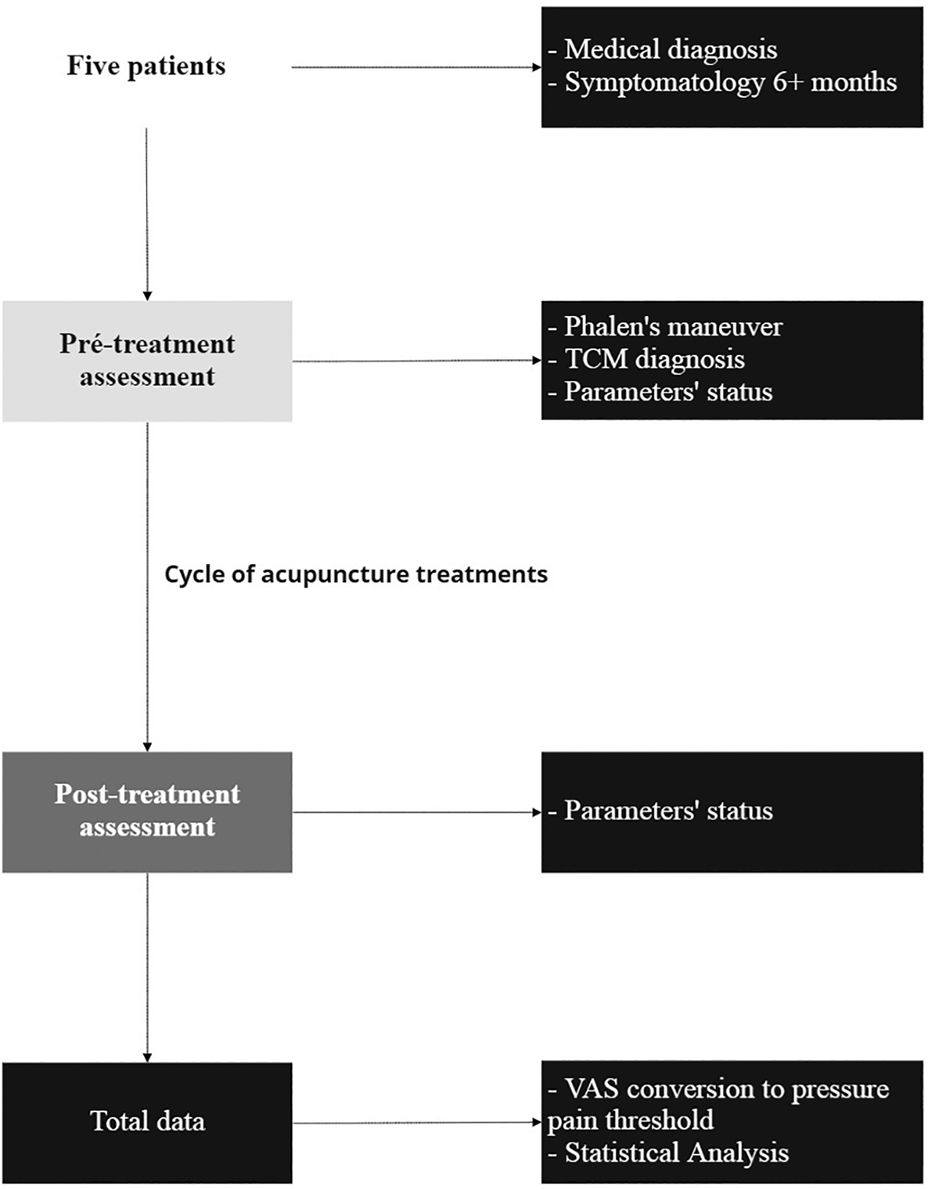
The overall study outline can be seen in fig. 3.
Filiform needles with a length of 25, 30, or 40 mm were used. A needle diameter of 0,25 mm or 0,30 mm was used according to the case.
The acupuncture cavities (or points) of the “hand Tai Yin channel”, the “hand Governor of the Heart channel” and the “hand Yang Ming channel” were selected as the main areas for treatment.
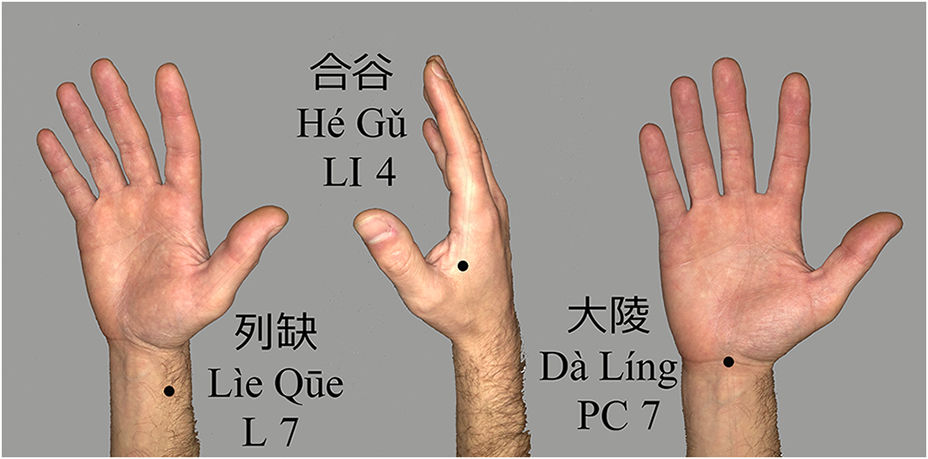
Some of the acupuncture cavities generally used as a base treatment were (fig. 4):
- -
“Rupture of the Sequence” (L 7 列缺 Lìe Qūe);
- -
“Union of Valleys” (LI 4 合谷 Hé G¿);
- -
“Great Hill” (PC 7 大陵 Dà Líng).
Other cavities were selected based on the constitutional balance in the perspective of CTCM.
Cases II, III, IV, and V continued their regular professional activities during the treatments.
The Wilcoxon sign test in IBM SPSS Statistics 26 software was used to compare overall pre- and post-treatment VAS results and the estimated pressure pain threshold levels. The significance level was fixed at 5%.
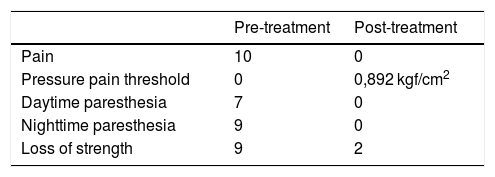
ResultsCase IFemale patient, 65 years. Retired teacher. Showed complaints of bilateral CTS for more than 1 year, with a severe degree of demyelination. Generalized pain in the palm and the first three fingers, with more aggravated pain at the base of the first finger and muscular atrophy of the thenar eminence of the right hand, with loss of strength, and both daytime and nighttime paresthesia. The patient was indicated for surgery.
There were concomitant pieces of evidence of “Liver Blood insufficiency and Liver Qì depression” pattern.
It was applied the base treatment at the cavities: “Rupture of the Sequence” (L 7 列缺 Lìe Qūe), “Union of Valleys” (LI 4 合谷 Hé G¿) and “Great Hill” (PC 7 大陵 Dà Líng). Additionally, some acupuncture cavities were used to treat the pattern evidence of “Liver Blood insufficiency and Liver Qì depression”, such as “Curved Spring” (Li 8 曲泉 Qū Quán), “Big and Solid” (Li 1 大敦 Dà Dūn), and “Crossing of the Three Yin” (Sp 6 三陰交 Sān Yīn Jiāo).
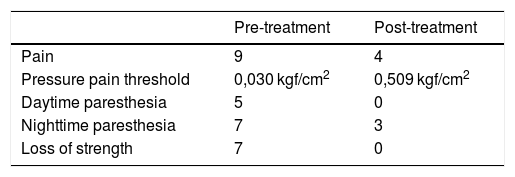
As we can observe on table 1, all parameters improved.
This patient had a very effective outcome in the eradication of pain and paresthesia as well as a good result in the treatment of loss of strength.
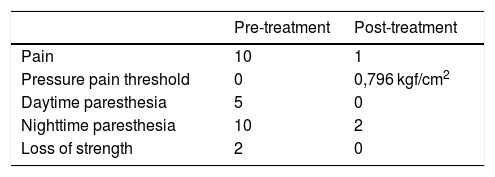
Case IIFemale, 60 years old, a nurse, presented severe symptoms of bilateral CTS for 1 and a half years. Severe pain in the first two fingers and wrist that worsens with regular work activities. Slight muscular atrophy of the right hand's thenar eminence, with loss of strength. Slight daytime paresthesia and severe nocturnal paresthesia. The patient was indicated for surgery.
Concomitant pieces of evidence of “Liver Blood insufficiency and Liver Qì depression, and Spleen and Kidney Qì deficiency with dampness retention” pattern were present. It was applied the base treatment at the cavities “Rupture of the Sequence” (L 7 列缺 Lìe Qūe), “Union of Valleys” (LI 4 合⾕ Hé G¿) and “Great Hill” (PC 7 大陵 Dà Líng). At the same time, some acupuncture cavities to treat the concomitant patterns were used, such as “Curved Spring” (Li8 曲泉 Qū Quán), “Big and Solid” (Li 1 ⼤ 大 敦 Dà Dūn), “Crossing of the Three Yin” (Sp 6 三陰交 Sān Yīn Jiāo), “Supreme White” (Sp 3 太 白 Tài Bái), “Spring of the Yin Hill” (Sp 9 陰陵泉 Yīn Líng Quán) and “Return of The Swift Flow” (K 7 復溜 Fù Liū).
As we can observe on table 2, all parameters showed improvements.
This patient had an effective result in the treatment of pain and night paresthesia and a very effective result in the complaints of loss of strength and day paresthesia.
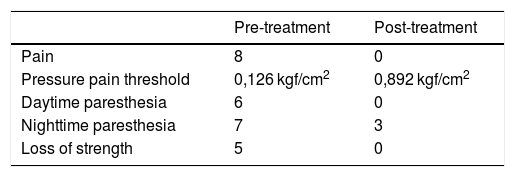
Case IIIWoman, 51 years old, teacher, with symptoms of right CTS for 10 months on a moderate to a severe degree. Pain, paresthesia, and loss of strength. The patient was indicated for surgery.
This patient presented accessory evidence of “Liver Qì depression” and “Spleen Qì deficiency”. It was applied the base treatment at the cavities “Rupture of the Sequence” (L 7 列缺 Lìe Qūe), “Union of Valleys” (LI 4 合谷 Hé G¿) and “Great Hill” (PC 7 大 陵 Dà Líng), as well as “Liver Transport” (B 18 肝俞 Gān Shū), “Supreme Path” (Li 3 太衝 Tài Chōng), “Supreme White” (Sp 3 太白 Tài Bái) and “Hidden White” (Sp 1 隱白 Y¿n Bái), were used as a complementary treatment to address the “Liver Qì depression” and the “Spleen Qì deficiency” patterns.
On table 3, we can observe improvements in all parameters. This patient had an outstanding result in the treatment of pain, daytime paresthesia, and loss of strength. The effect was less evident in the night paresthesia.
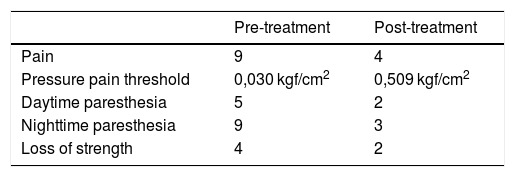
Case IVA woman, 42 years old, medical dentist, presented symptoms of bilateral CTS for 2 years, with aggravated symptoms in the right hand to a serious degree. Pain, paresthesia, with aggravation of paresthesia during nighttime. Loss of strength, difficulty in handling work tools. With surgical indication.
This patient had concomitant evidence of “Liver Blood insufficiency and Blood Stasis and Spleen Qì deficiency”. It was applied the base treatment at the cavities of: “Rupture of the Sequence” (L 7 列 缺 Lìe Qūe), “Union of Valleys” (LI 4 合谷 Hé G¿) and “Great Hill” (PC 7 大陵 Dà Líng). At the same time, to treat the above-stated patterns, it was used acupuncture cavities such as “Curved Spring” (Li 8 曲泉 Qū Quán), “Big and Solid” (Li 1 大敦 Dà Dūn), “Supreme White” (Sp 3 太白 Tài Bái), “Crossing of the Three Yin” (Sp 6 三 陰 交 Sān Yīn Jiāo), as well as bleeding and cupping at “Diaphragm Transport” (B 17 膈俞 Gé Shū).
Regarding this case, table 4 presents that all parameters improved.
This patient had a good result in the treatment of all the symptoms, but with an incomplete effect in all the parameters. The best response was in the symptoms of paresthesia.
Case VWoman, 49 years old, florist. Symptoms of bilateral CTS for 4 years were present, with aggravated symptoms in the right hand at a serious degree. Pain, paresthesia, with aggravation of pain at night. She also developed pain in both the elbow and arm during the previous year. Loss of strength with difficulty in handling work tools. The patient was indicated for surgery.
The patient also presented concomitant evidence of “Liver Blood insufficiency and Blood Stasis”. So, it was applied the base treatment at the cavities “Rupture of the Sequence” (L 7 列缺 Lìe Qūe), “Union of Valleys” (LI 4 合谷 Hé G¿) and “Great Hill” (PC 7 大陵 Dà Líng). At the same time were used some acupuncture cavities to treat the pattern “Liver Blood insufficiency and Blood Stasis”, such as “Curved Spring” (曲 泉 Qū Quán Li 8) with acupuncture and moxibustion, “Big and Solid” (Li 1 大敦 Dà Dūn) with moxibustion, “Crossing of the Three Yin” (Sp 6 三陰交 Sān Yīn Jiāo) with acupuncture and moxibustion, and with bleeding and cupping at “Diaphragm Transport” (B 17 膈俞 Gé Shū) and bleeding at “Curved Pond” (LI 11 曲池 Qū Chí).
Case V achieved improvements in all parameters, as we can observe on table 5.
The effect was most noticed in the treatment of loss of strength and daytime paresthesia. The result was not complete in the treatment of pain and night paresthesia, although there was a decrease in pain and daytime symptoms.
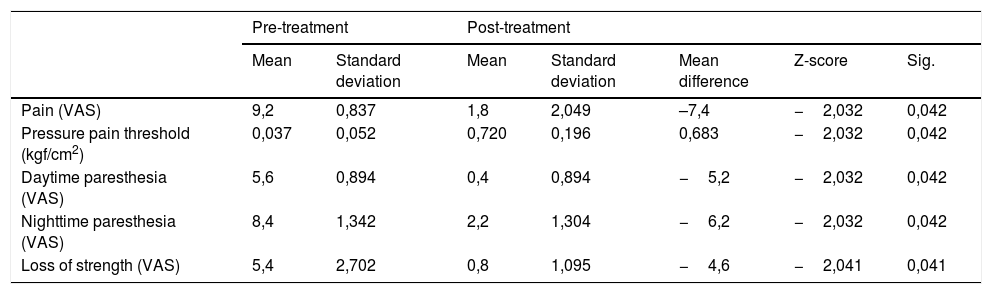
General resultsAs we can see in table 6, all parameters showed significant differences (p < 0,05) between pre- and post-treatment cycle values.
Pre- and Post-treatment overall differences for the evaluated parameters and approximate pressure pain threshold
| Pre-treatment | Post-treatment | ||||||
|---|---|---|---|---|---|---|---|
| Mean | Standard deviation | Mean | Standard deviation | Mean difference | Z-score | Sig. | |
| Pain (VAS) | 9,2 | 0,837 | 1,8 | 2,049 | –7,4 | −2,032 | 0,042 |
| Pressure pain threshold (kgf/cm2) | 0,037 | 0,052 | 0,720 | 0,196 | 0,683 | −2,032 | 0,042 |
| Daytime paresthesia (VAS) | 5,6 | 0,894 | 0,4 | 0,894 | −5,2 | −2,032 | 0,042 |
| Nighttime paresthesia (VAS) | 8,4 | 1,342 | 2,2 | 1,304 | −6,2 | −2,032 | 0,042 |
| Loss of strength (VAS) | 5,4 | 2,702 | 0,8 | 1,095 | −4,6 | −2,041 | 0,041 |
The mean difference was negative for pain (−7,4 points), daytime paresthesia (−5,2 points), nighttime paresthesia (−6,2 points), and loss of strength (−4,6 points), whereas the estimate for the pressure pain threshold was positive (+0,683 kgf/cm2).
DiscussionCTS is the most common of the incarceration neuropathies presenting the most varied and complex incidence and prevalence expressed by a diagnostic method based on physical exams for neurological deficits, which may involve assessments of impaired sensitivity, discrimination of two points in the distribution of the median nerve or thenar weakness.21–23
Surgical decompression is still a definitive treatment for CTS in an advanced situation, e.g., the release of the carpal tunnel in the USA is one of the most performed procedures, about 200,000 each year.24 In these cases, the surgical treatment seems to be more effective for CTS symptoms than immobilization, which has been the basis of conservative treatment.25 However, conservative treatment for CTS proves to be effective and the modification of activity is reasonable in patients with tolerable symptoms and absence of progressive neurological or functional deficits.23
Some people improve spontaneously and may frequently use nonsurgical interventions involving splinting, medications, exercises, modalities, and alternative therapies. Conservative treatment may include physical therapy (Hand/occupational therapy), bracing,26 iontophoresis and ultrasound,27 steroid injections,28 and mobilization exercises (e.g., tendon gliding and nerve gliding).29 However, surgical decompression (carpal tunnel release) is often elected. Alternative therapies are also frequently used, such as needles and low-level lasers acupuncture, static magnetic field (SMF), specific yoga, and Qi-Gong exercises.23
In the present research work, from the data analysis obtained through the acupuncture therapy of CTCM, we can observe that all parameters showed improvement. In agreement with recent research,30 we suggest that our results support the evidence of clinical efficacy.
In terms of the CTCM treatment method, different approaches were used:
- •
Local approach being, in the CTCM perspective a tendon problem, in some cases it was adopted the principle: “Use the pain [local] as the transport [cavity]” and the technic “restorative puncture” (恢刺刺 huī cì);30
- •
Distal approach: Being a tendon pathology, the best approach seems to be the local one. However, due to the patient's constitution, the pattern evidence, and the theoretical interrelationship between internal organs and body tissues, some distal points associated with the Liver channel and other related channels were used.
On both approaches, regarding the CTS, Napadow, Liu31 showed that acupuncture either at the affected hand, or distally at the ankle, improved nerve impulses in the wrist. Those who received local treatment also experienced brain remapping linked to long-term improvement in CTS.
Overall, after the treatment cycle patients showed significant improvements on the evaluated parameters, similarly to other studies using acupuncture.32–34 Specifically, our study showed that there was an average improvement rate of 80% regarding pain intensity and an improved average on the estimated pressure pain threshold of 0,682 kgf/cm2. Regarding daytime paresthesia, it was achieved an improvement average rate of 93%, while nocturnal paresthesia obtained an improvement average of 74%. In addition, the impairment related to the decrease in strength levels improved at an average of 85%.
Some studies already demonstrate that acupuncture improves clinical and neurophysiological findings of CTS alone31,34,35 or in complement to other methods.36–38 It seems to be associated with no serious adverse events39,40 and provides an alternative for patients who have oral steroid intolerance/contraindication or choose to avoid early surgery.41,42 Researchers often find it difficult to understand the mechanisms through which traditional Chinese medicine acts on the body. However, some have been demystifying these techniques, bridging Western understanding,43–47 allowing Chinese medicine to be considered a traditional model of vegetative system biology with a systemic therapeutic approach,48,49 employing vegetative reflex therapies such as acupuncture50 to regulate the nervous, circulatory, endocrine, and exocrine systems, achieving an improved state of well-being.51
This clinical study was performed to unveil the rationale behind the classic texts of Chinese medicine and the relationships that integrate the view of classical acupuncture treatment with current anatomical-physiological knowledge, applying it to specific cases of CTS and, of course, to understand its effectiveness.
Despite our positive results regarding the application of classical acupuncture in patients with CTS, there still is doubt as to what the outcome would be in terms of effectiveness with longer treatment periods and the complementary prescription of Chinese Phytotherapy. Larger samples and control groups would also improve the methodological quality of future studies.
FundingThis research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Declarations of interestNone.
We would like to thank all the patients involved in this study, Diana Queirós for designing fig. 2 “Proposed scale for the relation between VAS pain levels and pressure pain threshold”, Ricardo Moreira for revising the English text, and Mariana Ferreira for the title and abstract translation to Spanish.