Normal sexual functioning of both men and women, being a very complex process, is affected by numerous issues besides aging. Many factors affect the sexual function and lifestyle of the young population. In this article, we tried to review the literature to update the knowledge on benzodiazepine-related (BZD) sexual dysfunction (SD) and involved mechanisms of actions based on animal and human studies.
MethodsDifferent standard websites such as PubMed were used to review the literature and keywords including benzodiazepines, sexual dysfunction, gammaaminobutyric acid A (GABAA) receptor and erectile dysfunction were used.
ResultsSD is one of the most common disorders in males and females which has recently been demonstrated to be associated with psychotropic medications such as antihypertensive agents, tranquilizers, antihistamines, appetite suppressants, antidepressants and anxiolytics. BZDs are among the most common psychotropic agents worldwide. SD including decreased libido, erectile dysfunction (ED) and other undesired sexual urges were observed in the patients receiving BZDs.
DiscussionThe mechanisms of action of BZDs to induce SD mainly relate to enhanced GABAA receptor function which reduces penile erection.
El funcionamiento sexual normal de los varones y las mujeres, al ser un proceso muy complejo, se ve afectado por numerosos problemas, además del envejecimiento. Muchos factores afectan a la función sexual y al estilo de vida de la población joven. En este artículo intentamos revisar la literatura para actualizar el conocimiento sobre las disfunciones sexuales (SD, por sus siglas en inglés) relacionadas con benzodiacepinas (BZD) y los mecanismos de acción involucrados en estudios con animales y humanos.
MétodosSe utilizaron diferentes sitios web estándar, como PubMed, para revisar la literatura y las palabras clave que incluyen BZD, disfunciones sexuales, ácido gamma-aminobutírico A y disfunción eréctil.
ResultadosLas SD son uno de los trastornos más comunes en los varones y las mujeres, ya que recientemente se ha demostrado que están asociados a medicamentos psicotrópicos como agentes antihipertensivos, tranquilizantes, antihistamínicos, supresores del apetito, antidepresivos y ansiolíticos. Las BZD son uno de los agentes psicotrópicos más comunes en todo el mundo. Las SD que incluían disminución de la libido, la disfunción eréctil (DE) y otros impulsos sexuales no deseados, se observaron en los pacientes que recibieron BZD.
DiscusiónLos mecanismos de acción de las BZD para inducir SD se relacionan principalmente con la función mejorada del receptor de ácido gamma-aminobutírico A (GABAA) que reduce la erección del pene.
Sexual dysfunctions (SDs) are defined as disorders in sexual desire and in the psychophysiological alterations related to the sexual response cycle in men and women.1 Different factors such as drugs, chemicals, stress, smoking and psychological issues directly and indirectly have adverse effects on sexual performance and life quality of the young people.2 Although enhanced demand for clinical services and the potential effects of SDs on quality of life and interpersonal relationships,3 the relative epidemiologic data are limited. According to the few available investigations, it seems that SDs are highly frequent in males and females; male SDs (MSD: 10–52%) and female SD (FSD: 25–63%).4–7 Additionally, SD is widely recognized as a potential side effect and a common symptom in patients receiving psychotic drugs such as antipsychotics, anxiolytics medication, antidepressants and mood stabilizers as well as in the treatment of other psychiatric disorders.8 Recently, psychotropic-induced SD has been introduced as an increasingly especial clinical topic.9,10 Furthermore, SDs have become frequent side effect of treatment with wide range of antidepressants as a main reasons for premature drug discontinuation.11,12 Antipsychotic drugs have been relate to SDs, such as reduced sexual desire, delayed or retrograde ejaculation erectile dysfunction (ED), and anorgasmia.11,13 Psychotropic-induced SDs may have serious negative outcomes such as early discontinuation of pharmacotherapy or non-compliance with medication.14 Moreover, SDs may reduce the quality of life of patients, deteriorate self-esteem and cause different relationship problems.11 SDs have particularly been recorded with taking the anti-epileptic drugs,15 selective serotonin reuptake inhibitors (SSRIs),12,16 benzodiazepines (BZDs),17,18etc.
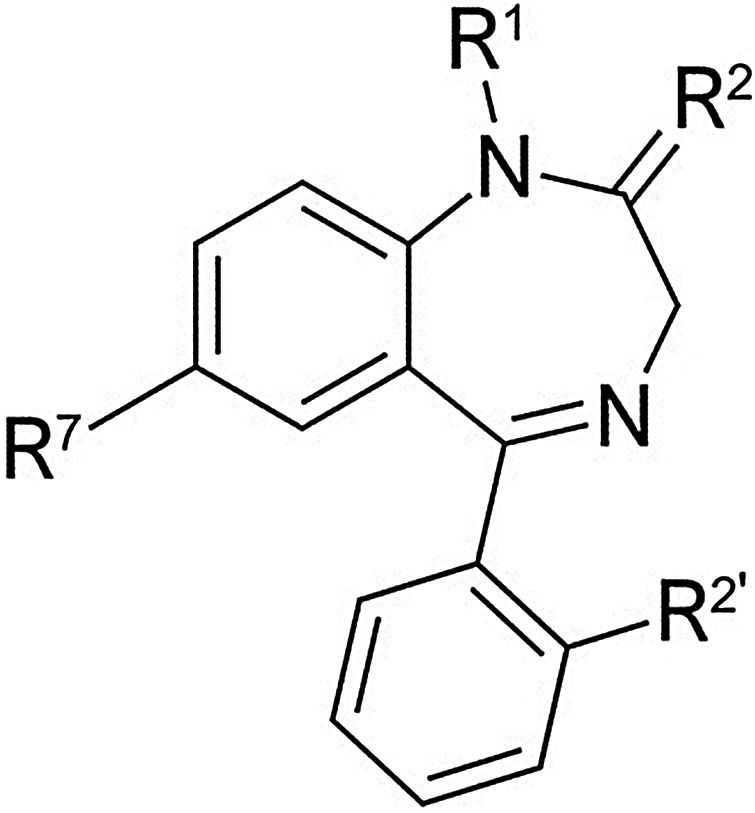
BZDs (Fig. 1) are known as one of the most prevalence psychotropic drugs in worldwide.19,20 BZDs are used for numerous to central nervous system (CNS) related disordered.21 Despite, these properties become undesired, wide range of adverse effects were recorded for BZDs.22 According to the literature, SDs were observed in the patients received BZDs. Decreased libido, erectile dysfunction (ED) and other sexual undesired urges were seen among BZDs users.18,23
In this review, the purpose was to provide an update on the adverse effects and various mechanism of actions of BZDs on sexual functions of patients receiving these agents due to different therapeutic plans of psychology other pharmacological therapies.
MethodsA different search engines such as PubMed were used to literature review using the keywords including benzodiazepines, sexual dysfunction, gammaaminobutyric acid A receptor and erectile dysfunction. Keyword searches were conducted for identifying different type of researches using electronic databases from their inception up to July 2018. We selected BDZs related SD reports which were recorded for different psychiatry disorders.
BenzodiazepinesBZDs, sometimes called “benzos”, are launched in the market as one of psychotropic drugs in the United States in 2007 with more than 112 million prescriptions or maybe in the worldwide.19,20 BZDs with anterograde amnesia, greater sedation and cognitive or psychomotor impairment effects,24 are used for wide range of indications such as insomnia, muscle relaxation, anxiety, relief from spasticity induced by CNS pathology and epilepsy. BZDs are administered for treatment of anxiety disorders because of proved safety and efficiency compared to older drugs.25 Nearly all clinical instances have been reported to have adverse effects intraoperatively. BZDs are known for their sedative and anxiolytic characteristics.26,27 BZDs act on the CNS through boosting the effects of the gammaaminobutyric acid A (GABAA) receptor (GABAAR) which results in producing sedation, relaxing muscles and decreasing the levels of anxiety. After only short-term use, tolerance and dependence can be developed in users.28 Instructions on BZDs administrations state that these drugs should be used for only a short time.29,30 Chronic use is an indication of drug dependency and related to undesired effects such as depression, mood swings, altered perception, violent and impulsive behavior, weight gain, cardiovascular disturbances, gastrointestinal symptoms, nausea, metabolic abnormalities, osteoporosis and the risk of fractures, etc.31–35 According to the literature, SDs were observed in the patients received BZDs.36
Benzodiazepines and sexual dysfunction: potential disorders and mechanisms of actionDrugs including antidepressants, tranquilizers, appetite suppressants, antihistamines, anxiolytics and antihypertensive agents have been known to be with increased rates of ED. However, different studies on drug-induced ED have shown the conflicting findings. Medication-induced SD can meaningfully affect with patients’ life quality and lead to unfortunate compliance.37 BZDs stimulate the inhibitory procedures of the CNS primarily through γ-aminobutyric acid, a main inhibitory neurotransmitter. Despite these agents have been commonly prescribed for more than three decades, limited clinical literature are available to investigate the correlations between BZDs and SD in both men or women.38 SD can result from a wide variety of psychological and physical causes. Among drugs, antihypertensive, diuretics, antihistamines, antidepressants, BZDs and antipsychotics are the common agents associated with SD.39 The available researches suggests that the impacts of BZDs on sexual function may be minimal.17,18 However, these adverse effects can affects the life style of these patients confirmed in the different investigations.
Nutt et al. presented that BZDs withdrawal enhanced sexual function.40 Segraves confirmed that several BZDs have been reported to ejaculatory impairment.41 Brock et al. hypothesized that the sedative effect of BZDs results in decreased libido among users, or that decreased libido stems from the anxiety states for which treatment is prescribed.18 The incidence of SD seemed to be more when BZDs were used in combination with other psychotropic agents. In a hospital-based cross-sectional study, Shetageri et al. evaluated the effects of psychotropic medication on female's sexual desire and showed that the prevalence of psychotropic-induced SD was more than 48%. Their results confirmed that SD was more common in patients who were on combination of antidepressants and BZDs.42 In a non-randomized study which involved 104 patients with bipolar disorder, Ghadirian et al. also showed that the incidence of psychotropic-induced SD more when the co-administration BZDs and lithium.43 Georgiadis and Holstege confirmed that patients received BZDs in combination with lithium showed to have significantly higher rates of SD (49%) than when lithium used alone (14%) or lithium in combination with other types of drugs (17%).44
Although BZDs have been shown to be related to medication with BZDs, Mazzilli et al. conducted a study on 1872 patients with ED and select patients receiving psychotropic drugs to evaluate the frequency of patients with ED. The prevalence of ED treated with psychotropic drugs more than three months was 9.5% (178/1872). Furthermore, the prevalence of ED based on the received drugs was reported as below: atypical antipsychotics in 16 (9.0%) patients; BZDs (alprazolam, clonazepam, lorazepam, bromazepam) in 55 (30.9%) patients; antidepressants in 33 (18.5%) patients; and multiple psychotropic drugs in 74 (41.6%) patients.45 In an investigation on 2040 patients, Corona et al. also reported on the relation between hormonal parameters and the use of SSRIs, non-SSRIs, antidepressants, BZDs. The higher levels of prolactin were only reported in patients using SSRIs compared to other BDZs and antidepressants.46
To defined the underlying mechanisms of action of BZDs to induce SD, Melis and Argiolas stated that BZD increased GABAAR function and GABAAR stimulation and reduced penile erection in rats by central procedures.47 As well, an alternative explanation for the observed trend may be that both ED and BZD are associated with ischemic vascular disease. The results of a population based study by Lapane et al. proved that BZD use may be related to enhanced incidence of ischemic heart disease,48 whereas other studies demonstrated an association between cardiovascular disease and ED.49,50 BZDs also cause drowsiness as a hypnotics agent and thus, reducing desire.51 In this study, the effect of different BDZs were investigated.
DiazepamDiazepam (Valium, 7-chloro-l, 3dihydro-l-methyl-5-phenyl-2H-1,4-benzodiazepin-2-one) as a BZD is administered for different indications such as sedation, anticonvulsant, anesthetic adjunct and behavioral disorders.52 Diazepam is known for its skeletal muscle relaxation properties; hence, there was thought that it would have utility in treating some forms of sexual pain. Recent research has highlighted the use of vaginal diazepam suppositories in the treatment of urogenital pain/pelvic floor dysfunction.53,54 In a retrospective study, Rogalski et al. studied the vaginal diazepam suppositories effects in 26 patients with high-tone pelvic floor dysfunction and sexual pain. Of the 26 women, 25 of them experienced subjective improvements in their pain levels. However, when assessing their pain improving through the female sexual function index (FSFI) scoring system, they did not demonstrated an improvement in sexual pain.54 Balon et al. showed that SD was associated with diazepam but not with Clonazepam.55 To define mechanisms of diazepam induced SD, there are many evidences indicating that Diazepam had antifertility effects on male rats through attenuating production of testosterone and steroidogenesis by inhibiting the hormones of pituitary gonadal axis and the StAR gene expression by its impacts on calcium ions.56 Riley and Riley investigated the effect of single dose diazepam on female sexual response induced by masturbation. They proved that diazepam related impairments induced by a dose-related manner.39 To define the mechanisms of diazepam induced SDs, there are many evidences stated that cell proliferation has been inhibited by diazepam according to both in vitro and in vivo. Clark and Ryan reported that diazepam exerted an anti-proliferative actions on 3T3 fibroblasts.57 As well, in an in vitro study, the anti-proliferative effects of diazepam on the proliferation of mouse spleen lymphocytes was recorded by Pawlikowski et al.58,59 Different factors may be involved in the inhibitory mechanisms of diazepam on cell proliferation. Maybe, the inhibitory actions of diazepam on cell proliferation are related to the induction of chromosomes malsegregation.60 Also, it was found that during the metaphase–anaphase transition, diazepam inhibit centrioles shifting, results in the monopolar spindle formation.61 Another possibility, which does not exclude the preceding mechanisms, is the effects of diazepam on calcium ions. BZDs receptors block the voltage-dependent calcium channels.62 Moreover, it is well known that calcium ions require for the initiation of DNA synthesis in the later G1-phase of the cell cycle.63 Additionally, it was reported that BZD inhibits the calmodulin-dependent protein kinase in the brain. Jones et al. found that formation of calcium–calmodulin complex plays critical role in the initiation of DNA synthesis by calcium.64 In the other wise, diazepam can act on the production of adrenocorticotropic hormone (ACTH, also corticotropin, adrenocorticotropin). Racagni et al. found that diazepam decreased ACTH production.65 El-Sokkary et al. showed that treatment with diazepam in rat caused the degeneration in the cells of the seminiferous tubules, vacuolation in their cytoplasm, reduction of seminiferous epithelial layers, hyalinization and edema of intertubular tissue. Also, their findings showed that serum testosterone level decreased in the diazepam treated rats which correlated with the pathologic changes in the testis tissue.66 Testosterone hormone is known as a main male hormone which Leydig cells synthesize these hormones from cholesterol.66 This decline of testosterone concentration may be due to the impact of diazepam on cholesterol levels of serum which is a precursor of testosterone synthesis by its effects on the Leydig cells.67
AlprazolamAlprazolam (Xanax, 8-chloro-1-methyl-6-phenyl-4H-s-triazolo [4,3-α] [1,4]) is a short-acting benzodiazepine used as an anti-anxiety medication prescribed to treat panic attacks and anxiety disorders.68 SD has been reported in the patients on alprazolam treatment. Lydiard and Howell reported that men and women who had received high doses of alprazolam (Xanax, 3–10mg/day) for panic disorder experienced ED, diminished sex drive and/or reduced ability to obtain orgasm in 50% of encounters.23 In particular, ED has been reported in subjects using serotonin selective re-uptake inhibitors (SSRI), lithium and BZDs.69 Specifically, BZDs and tricyclic antidepressants were associated with two- to threefold increase in odds of ED. In a survey study of Boston Area Community Health (BACH), Kupelian et al. showed a positive associations of tricyclic antidepressant and BZDs with ED.70 In another study by Holstege et al., it was demonstrated that patients with panic disorders received alprazolam caused significant rates of decreased libido and increased ED and orgasm dysfunction.71 Uhde et al. reported the relation between SD and alprazolam treatment in 47-year-old woman and a 32-year-old man with social phobia cases.72 Derby et al. evaluated the prevalence of ED in the patients with drug therapy in the MMAS cohort. Results of the MMAS on serotonin reuptake inhibitors (SSRIs), other antidepressants, and BZDs found a significant association of BZDs and ED (adjusted OR=1.98, 95% CI: 1.11, 3.53). The BZDs and ED association are consistent with results of the MMAS with a similar twofold increase in odds of ED.37 Conversely, in a multicenter comparative and double blind randomized study, Márquez et al., evaluated the 190 outpatients affected by panic disorder treated with alprazolam (sublingual and oral formulations) in Argentina. The Arizona sexual experience scale (ASEX) was carried out to assess SDs. They reported that there were no differences the in the ASEX scores before and after medication with alprazolam which defined that sexual sphere was not affected by alprazolam.73 Although, the overall risk of SD with the BZDs is relatively low, high-dose BZD therapy or BZDs in combination with anxiolytic antidepressants, have been associated with an enhanced incidence of SDs. Lydiard et al. demonstrated that men and women who were receiving high-dose alprazolam (3–10mg/d) for panic disorder reported ED, decrement sex drive, and/or reduced ability to achieve orgasm in 50% of cases,23 Also, Ghadirian et al. reported that the combination of BZDs with lithium was also associated with decreased sexual function in 49% of patients.43 However, the absence of documented baseline impairment and their combination with other psychotropics make it difficult to attribute the treatment-emergent dysfunction to BZDs in either of these studies.
LorazepamLorazepam (Ativan) with the chemical formula of 7-chloro-5-[o-chlorophenyl]-1,3-dihydro-3-hydroxy-2H-1,4-BZD-2-one is used to treatment of patients with active seizures, anxiety disorders and trouble sleeping, as well as to sedate those who are being mechanically ventilated.74 Some researchers have described increased sexual desire during treatment with lorazepam. Simões et al. introduced a case of 62-year-old woman with breast mucinous carcinoma, chronically medicated with ramipril and diazepam 5mg id. After, tumor resection and chemotherapy, lorazepam (1mg) was prescribed for her complication including difficulties on sleep onset. After administration of lorazepam, an overwhelming sexual desire was reported during the physical intercourse. Dopaminomimetic drugs can exacerbate sexual desire by raising the dopamine levels. In this way, BZDs, as GABA enhancers, would inhibit dopamine secretion leading to reduced libido. On the other hand, GABA inhibits serotoninergic-mediated vigilance and impulse control, leading to impulsivity and disinhibition.75
ClonazepamClonazepam (CLZ, Klonopin, 5-[2-chlorophenyl]-1,3-dihydro-7-nitro-2H-1,4-BZD-2-one) is an agent used to prevent and treatment of seizures and panic disorder. Although it was emphasized that using Clonazepam was not related to SD, some studies have described increased sexual disinhibition during treatment with clonazepam. Kubacki demonstrated the clonazepam related SD in a letter to the editor in 1987.76 As well, in as retrospective study, Fossey and Hamner examined the records of 100 male veterans with post-traumatic stress disorder (PTSD) for presence of SD. Their findings suggested that BZDs, especially clonazepam, could be a leading cause of SD in majority of male patients.77 As well, Yang et al. in a study on 100 male patients suffering from PTSD did not find any evidence that SD correlated with lorazepam, alprazolam, or diazepam use. However, they reported that approximately 43% of the patients with clonazepam treatment had SD, chiefly ED.78 Mutha et al. investigated the SD in patients using neuro-psychiatry medicines with SD and showed that patients on anxiolytic treatment such as clonazepam, alprazolam and diazepam associated with SD which using clonazepam was the most common drug among these patients.79
ConclusionIn conclusion, BZDs such as diazepam, alprazolam lorazepam, and clonazepam have been shown to induce wide range of sexual dysfunctions in both males and females e.g. decreased sexual desire, anorgasmia, ED, etc. Different mechanisms such as enhanced GABAAR function confirmed in different investigations to define the BZDs induced SD which mainly related with ED. Based on the results, we suggested to carefully select drugs for the treatment of neuropsychiatry diseases considering potential for SD.
Ethical disclosuresProtection of human and animal subjectsThe authors declare that no experiments were performed on humans or animals for this study.
Confidentiality of dataThe authors declare that no patient data appear in this article.
Right to privacy and informed consentThe authors declare that no patient data appear in this article.
FundingNo funding.
Conflict of interestAuthors declared no conflict of interest.