Solitary bone cyst of the mandible is an intra-osseous cavity lacking epithelial lining considered a pseudocyst. Due to its uncertain etiology and pathogenesis, it has received several names such as traumatic bone cyst or idiopathic bone cyst. From a clinical perspective, it is oftentimes an asymptomatic lesion, with festooned borders when located between dental roots. It is an empty cavity but might contain blood, serous or serous-hematic fluid and can be perceived in routine X-ray examinations. The present article describes the case of a solitary bone cyst located in the body of the mandible of a 17-year old female patient. Afflicted with Fallot's tetralogy. Clinical, diagnostic and radiologic aspects as well as treatment are described.
El quiste óseo solitario de la mandíbula, es una cavidad intraósea sin recubrimiento epitelial, considerado un pseudoquiste, ha recibido diversas denominaciones debido a su etiología y patogenia inciertas como quiste óseo traumático, quiste óseo solitario y quiste óseo idiopático. Clínicamente suele ser una lesión asintomática, muestra bordes festoneados cuando está localizado entre las raíces dentales, es una cavidad vacía pero puede contener sangre, fluido seroso o serohemático y es descubierta en exámenes radiológicos de rutina. En este artículo se presenta un caso de quiste óseo solitario localizado en el cuerpo mandibular que acomete a un paciente femenino de 17 años de edad con tetralogía de Fallot, revelando aspectos clínicos, diagnósticos e imagenológicos y tratamiento.
Lucas and Blum first described solitary bone cysts of the mandible in 1929. Nevertheless, it was not until 1949 that Rushton established the diagnostic criterion of this condition. It was defined as a simple cyst lacking epithelial lining with intact bone wall, filled with fluid and lacking evidence of chronic or acute inflammation.1,2
Donkor and Punnia-Moorthy suggested a possible sub-classification of solitary bone cyst based upon its content: empty cysts could be named idiopathic cysts, cysts with solid filling could be named according to the histological aspect of its content (fibrous or with granulation tissue), cysts with liquid content with a biochemical profile similar to blood plasma could be called extravasation cysts.3
These cysts have been described with different terms such as: solitary bone disease, solitary bone cyst, haemorrhagic cyst, extravasation cyst, single chamber cyst, simple and idiopathic cysts. This diversity in terms only reflects the uncertain origins of this lesion.3–5
The World Health Organization's (WHO) International Tumor Histological Classification accepted the term «simple bone cyst» in 1971, and the «term solitary bone cyst» in 1992 so as to differentiate this lesion from other cystic lesions of the jaws.6,7 In the 1997 WHO classification, solitary bone cyst is included in the group of bone-related non-neoplastic diseases along with aneurismatic cysts, ossifying fibroma, fibrous dysplasia, bone dysplasia, giant cell central granuloma and cherubism.1,4,8
LITERATURE REVIEWEpidemiologySolitary bone cysts are also found in other parts of the skeleton, more commonly in long bones (90-95%) with predominance in the metaphysis region of the humerus proximal ends (65%) as well as femoral shaft (diaphysis) (25%).6,9
According to scientific literature, solitary cysts occur frequently in young subjects, especially males. This could be due to the fact that males are more exposed to traumatic lesions than females. This is particularly the case of extra-facial solitary cyst variants9,10. Nevertheless, it has also been reported that solitary bone cysts have their onset in equal proportion in males and females in their second decade of life.4,11
In contrast, authors such as Cortell-Ballester and Peñarrocha referred having observed that solitary bone cysts were more frequently present when subjects were under 20 years of age; they exhibited mild predilection for females.1,12
Saito et al concluded that solitary bone cysts in young subjects were characterized as being asymptomatic, radio-lucid lesions with minimal expansion in the mandible, whereas solitary bone cysts in older groups were radio-opaque with cement hyperplasia or dysplasia and with loss of tooth-related lamina dura.3,8
Horner and Forman describe a different sub-group of solitary bone cysts characterized for appearing with fibrous-bone lesions seemingly developing in older patients.8
Incidence of these cysts in the upper jaws is not common, it represents 1% of all maxillary cysts. Most solitary bone cysts have been located in the body of the mandible, in the premolar and molar region (75%), with possible and sometimes severe extension towards the back. The second most common site is the mandibular symphisis.12,13 Few cases are reported in the mandibular ramus, condyle and upper jaw.11 It has been proposed that the maxillary sinus might impede visualization of maxillary lesions.2 This condition can appear as multilobular,13 multiple2,3,14 and bilateral14,15 lesions.
SymptomatologyIn most cases, solitary cysts of the mandible are asymptomatic, lacking inflammation or other functional signs; teeth adjacent to the lesion respond to vitality tests. These lesions are frequently accidentally discovered in x-ray studies.12,16,17
Some patients report pain, inflammation and/ or tooth sensitivity.3 These cysts can uncommonly present fistula, root resorption, paresthesia and/or pathological fractures.7
These lesions rarely cause complications, nevertheless, the possibility of a pathological fracture in extended lesions cannot be overlooked.4
When solitary bone cysts of the mandible are associated to bone cement dysplasia (florid bone dysplasia),3,6,18 cementoma, odontoma5,18 and mesodermal tumor,10 patients have reported pain and inflammation.
Radiographic findingsIn most cases, solitary bone cysts appear as a radiolucid lesion with irregular but well defined borders, of normal appearance and mixed with cancellous bone, they might be partially sclerotic.3,8,12,17,19,20 The main characteristic of solitary bone cysts is their «festooned effect» when they extend towards dental roots, nevertheless, this festooned line has equally been present even in edentulous zones.8,11,19,21 Matsumura et al describe a «double line» circumscribing the lesions in 19 cases.3
Greater recurrence has been reported in long bones where solitary cysts appear with a festooned border when compared to solitary cysts with smooth borders; the aforementioned has not been reported in the lower jaw. Therefore, a festooned margin is a sign of possible recurrence, nevertheless it must not be confused with inter-dental festoon associated to intact lamina dura.4
Loss of lamina dura is mainly observed in patients over 30 years of age. In younger subjects it is minimal.22
Another radiographic characteristic is the widespread extension of the lesion along the mandibular body without bone expansion, cortical bone becomes thinned down due to endosteal erosion. In most cases, there is no displacement of adjacent teeth, dental root divergence or loss of lamina dura.3,20,23 Root resorption is rare (0-8.7%) and can cause lamina dura disappearance in 16-62% of all cases.8 In some studied cases, the mandibular canal partially disappears without any displacement, and in others displacement of said canal can be suspected.3,22,23
Mathew et al concluded that canal displacement could be the result of local increase of osmotic pressure resulting from the decomposition of hemolytic products, or the fact that the canal could be pushed in a lingual direction by the formation of an intrabone hematoma as result of a given traumatic event. Both aforementioned mechanisms could support the etiology of solitary bone cyst due to trauma.24
Matsumara et al mentioned that within the scope of their experience, solitary cysts become radioopaque with time, since no radio-opaque lesions were observed in the panoramic x-rays of young patients.3,23 Furukawa et al established that solitary bone cysts can be radiographically divided into three types, they proposed that each type possessed different etiology. Type I represented typical radiographic characteristics and originated from an intra-medullar hemorrhage; Type II exhibited lateral bone expansion, calcified bodies and an empty cavity caused by cystic degeneration of fibrous-bone lesions; Type III showed ill-defined radio-lucid lesions in a fibrous dysplasia caused by focal degeneration in the bone formation process.3
Cortical expansion has been observed in cases of solitary bone cyst of the mandible concomitant with florid bone dysplasia,3,6 cementoma, odontoma,23 hypercementosis, periapical cement dysplasia7 and mesodermal tumor.10
HistopathologyMicroscopic studies revealed a cancellous bone cavity lined with a cystic wall composed of a thin fibrous connective membrane with numerous collagen fibers. The cavity lacked epithelial7 lining and could be empty and without lining or with scarce liquid content.1,13,17 Scant,recent bone deposits could be observed.5,6
The following could equally be observed fibroblasts, osteoclast-like giant cells, congested capillaries and cholesterol crystals, granulation tissue, erythrocytes, hemosiderin, as well as aseptic bone necrosis. It must be nevertheless noted that these factors are not always constant.17,19
Analysis of fluid contained in solitary bone cysts seems to support the conclusion that it is a transudate lacking micro-organisms showing significant concentrations of enzymatic factors which indicate osteoclastic activity. The presence of metalloproteinases is of the utmost importance since these substances are involved in osteolitic and osteogenic phenomena. Absence of cystic content could indicate end of evolution and seems to be dependent on location. Solitary bone cysts of the mandible are frequently empty.4,9,11,22,24
EtiologySeveral causative agents have been proposed: tumor-elicited bone degeneration, calcium metabolism alterations, local alterations in the bone growth, venous obstruction,14 osteolysis increase, intramedullary bleeding, local ischemia, mild infectious processes, bone marrow infection, bone marrow ischemic necrosis, loss of blood supply due to hemangioma or lymphoma,1,19 lymphatic drainage obstruction from sinusoidal veins which will lead to trabecular bone resorption,2 developmental anomalies in which synovial fluid incorporates into the bone,2,5 blockage of interstitial fluid's normal drainage,2 failure in osteogenic cell differentiation25 or any combination of the aforementioned factors. Any type of trauma could cause a cyst of this type, including dental extractions1 or excessive force applied during orthodontic treatments.15
When taking into consideration many of the presented theories, and regardless of location, three theories prevail: 1) bone growth anomaly, 2) process of tumor degeneration and 3) a particular triggering factor for hemorrhagic trauma.2,4,9
Bone growth anomalyPredominant locations of solitary bone cyst close to cartilaginous growth plates could explain certain local anomalies during bone growth and development periods. Certain authors suspect that solitary bone cysts could represent an «out of control» bone remodeling area. In the lower jaw, the primary ossification point is located close to the mental foramen, this is a favorite area for solitary bone cyst onset, it is therefore possible to consider the hypothesis of a cellular differentiation anomaly during ossification and growth periods, related to local environmental factors, which would induce mechanical restrictions during osteogenesis and angiogenesis processes.4,9
Process of tumor degenerationSolitary bone cysts have been associated to osteodystrophic pathological conditions such as fibrous dysplasia and giant cell granuloma. The first could be caused by fibrous and micro-cystic degeneration, in the case of giant cell granuloma, liquefaction found in the central section induces solitary cyst formation as part of a healing process.4,9
TraumaThis hypothesis, proposed by Howe, is the most accepted and discussed. It is based on trauma occurrence followed by intra-medullar hemorrhage and hematoma.1,9,11
Trauma can also cause thrombosis or persistent spasm of an artery with ischemia and aseptic necrosis, causing thus cyst formation. Vascular alterations are supposedly associated to the resorption phenomenon, due to multiple micro-trauma events in teeth and alveolar process. Scientific literature reports a range of one week to 20 years as the time interval from trauma occurrence to solitary bone cyst detection.4,9,11
DIAGNOSISSolitary bone cyst diagnosis is determined by the association of clinical examination, radiographic findings, physical exploration and whenever possible, histopathological examination.16
Solitary bone cysts are fortuitously found in routine X-ray analyses.1,26 Definite diagnosis of solitary bone cysts is inevitably reached during surgery, when a cavity lacking epithelial lining, either empty or with content (blood) and/or friable, hemorrhagic, hard-to remove, grayish-yellow tissue is observed.11,12,26
Differential diagnosisDifferential diagnoses reported in literature include: odontogenic keratocyst, epithelial calcifying odontogenic tumor, adenomatoid odontogenic tumor, dentigerous cyst, residual cyst, ameloblastoma, aneurysmal cyst, mixoma, lateral periodontal cyst, radicular cyst, adenomatoid odontogenic tumor, apical periodontitis, giant cell central granuloma, and ameloblastic fibroma. These two latter lesions are especially noteworthy, since they tend to appear in the same age group and location of solitary bone cysts.2,7,16,18,26,27
Cystic degeneration has been reported in patients with fibrous dysplasia, which resulted in a cavity lacking epithelial lining. Nevertheless, in jaws and extra-cranial bones, fibrous dysplasia accompanies more aneurysmal cysts than solitary bone cysts.4
Radio-lucid areas observed in upper or lower jaws or around tooth apexes, due to pulp involvement, could lead to a misdiagnosis of apical periodontitis.16
TREATMENTRecommended treatment for mandibular solitary bone cyst is surgical exploration followed by curettage of bone walls. Hemorrhage within the cavity produces a clot which is eventually replaced by bone. It is believed that in some cases, spontaneous resolution will take place.4,12–14
Selected surgical procedures for treatment of this lesion include cavity exploration, fenestration, aspiration and condyle osteotomy (whenever the condyle is affected). Results obtained in Suei et al‘s study indicated that prognosis is more favorable when lesions are treated with fenestration and cavity filling, although no statistically significant differences were recorded.18,22
It has been proposed to use bovine freeze-dried bone, cancellous bone of the iliac crest, as well as introduction of autologous blood with patient's bone or hydroxyapatite.4,12,22 Other materials used are absorbable gel sponge and soluble haemostatic gauze.18
The aforementioned techniques could be particularly useful whenever rehabilitation with bonesupported implants in the affected area is required. Nevertheless, introduction of radio-opaque materials in the cavity could hinder the diagnosis of a possible lesion recurrence.1
Many authors concur in the theory that teeth with apexes involved within the lesion must not be subjected to endodontic treatment, since they present favorable prognosis and normal healing takes place without any further complications.12,19 Some authors recommend not undertaking curettage on the cavity's ceiling in an attempt to preserve vitality of adjacent teeth,12 while others suggest that de-vitalization of teeth within the lesion site is a factor that prevents solitary bone cyst healing.18
It is suggested that solitary bone cysts, concurrent or not with other lesions, must continue under radiographic control after surgical intervention, focusing on those solitary bone cysts which appear with concurrent lesions, since it has been reported they exhibit greater rate of recurrence.3,5,18
Suei et al. assume that suitable or adequate bone formation cannot be considered full lesion healing due to the fact that there might be recurrence even after substantial bone formation or regeneration.18
Sapone and Hansen suggested that periodic observation should be observed until radiographicallydetermined full healing of the solitary bone cyst takes place. Patients must be recalled every four months during the first year after surgery, every six months on the second year and once a year after that, until full healing is observed.3,18
Suei, Tagucho and Tanimoto mention that the aforementioned intervals are too short, since neither healing nor recurrence can be confirmed at early stages of the post-operative period. Excepting those cases with post-operative complications such as pain and infection, it is more sensible to conduct the first radiographic control in a period of 12 to 17 months after surgery, since this is the time in which most observed solved cases are confirmed.1,18
After the first post-operative control, it is sufficient to follow-up the case at 1 to 2 year intervals, since early detection of recurrence is not particularly useful. In most cases, resolution or recurrence will be confirmed at the first or second radiographic control within the first three years after surgery.5,13,18
Life-long follow-up might be necessary (even after healing) in cases of solitary bone cyst with concurring cement-bone dysplasia, since, in those cases, there is high probability of new lesion development. This also applies to cases with multiple solitary bone cyst lesions.18
PrognosisIn 90% of all cases, prognosis is generally favorable since surgical exploration elicits bone growth stimulation effected through new bleeding. It has been reported that graft placement does not favor prognosis.5
Recurrence is infrequent. In Kuroi's review, only 4 out of 255 patients experienced recurrence after treatment.14 Some reports point out that solitary bone cyst recurrence was above 20%; this proportion was even higher in cases of atypical solitary bone cysts.3,13,14
Horner et al suggested that recurrence could be possible in cases when the original causes of the lesions were still present after surgery. Lindsay et al suggested that lack of resolution could be the result of an infection perpetuated by non vital roots and teeth previously subjected to root canal treatments.14
Suei et al concluded that there was a relationship between radiographic characteristics of the lesions and their prognosis. Most lesions in studied cases with radiographic findings showing intact lamina dura and smooth margin resolved after surgery, or experienced spontaneous resolution, whereas over 60% recurrence was reported in cases of lamina dura absence, root resorption, expansion of cortical bone, festooned borders, radio-opaque mass or multiple cavities.25
CLINICAL CASEA 17 year old female patient with base diagnosis of Fallot's tetralogy and denied history of mandibular trauma was remitted to the Maxillofacial Surgery service of the Specialties Regional Hospital «Bicentenario de la Independencia » ISSSTE (Institute of Social Security services for Government Employees) presenting a radio-lucid lesion in the left premolar region.
The patient reported painful symptoms and paresthesia in the left area of the chin. Intraoral physical examination did not reveal volume increase, tooth mobility, periodontal pockets, alterations in adjacent mucosa, data of fistula or any type of secretions. In involved teeth, dental vitality test was positive (Figure 1).
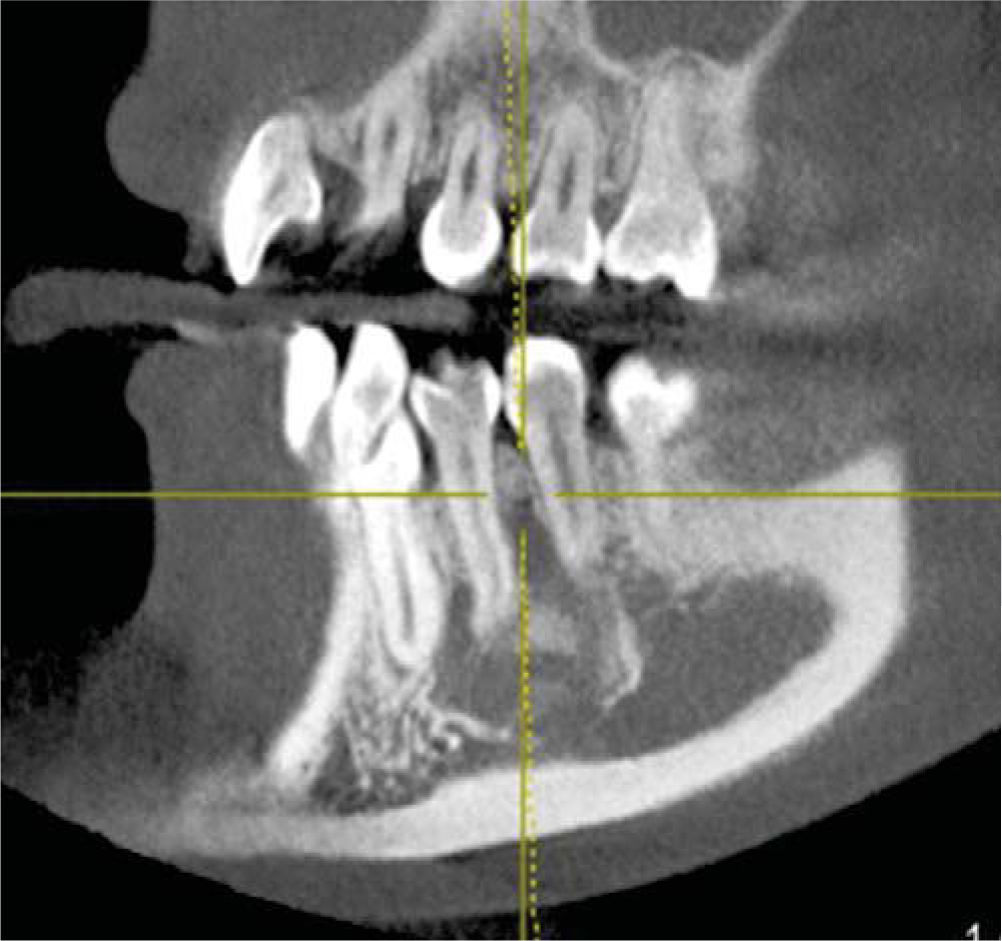
Orthopantomography revealed a radio-lucid lesion, with an irregular border and radio-opaque halo. The lesion involved first premolar, second premolar, and lower left canine, no root resorption or displacement was observed. The lesion exhibited a festooned border in the area of involved dental roots (Figures 2 and 3) and did not present expansion of cortical bone, nevertheless it exhibited thinning in lingual and vestibular cortical bone (Figure 4).
A .3 × .3cm incision biopsy of the lesion at the external cortical bone was undertaken. An empty bone cavity lacking epithelial lining was observed (Figure 5). The sample was sent for pathological examination; results of said study revealed trabecular bone without significant histopathological changes, therefore, a diagnosis of solitary bone cyst of the mandible was emitted. One year later, radiographic control revealed formation of significant trabecular bone (Figure 6).
The case of mandibular solitary bone cyst studied in the present article has the peculiarity of occurring in a patient afflicted with Fallot's tetralogy: a congenital heart disease characterized by exhibiting pulmonary artery stenosis, aortic override, intra-ventricular communication and right ventricle hypertrophy. The mechanism whereby growth is affected is probably multi-factorial, including tissue hypoxia, increase of energy expenditure, decreased food intake as well as frequent respiratory infections.28,29
Solitary bone cysts could be related to Fallot's tetralogy due to the alterations in calcium metabolism found in patients afflicted with this condition. This can determine the development of an osteolysis zone. Children afflicted with Fallot's tetralogy are more prone to suffer chromosomal disorders such as Down's syndrome and Di George's syndrome (condition causing heart defects, low calcium levels and immunodeficiency).29 This latter could be important in cases where Fallot's tetralogy were to be present, due to hypocalcemia produced by hypoparathyroidism, along with other calciummetabolism related factors. All the aforementioned would lead us to consider the etiopathogenesis of solitary bone cyst as the product of an hormonal alteration.
One among the multiple theories about the origins of solitary bone cysts is related to alteration in bone growth,9 as well as flaws in mesenchymal tissue during the process of cartilage and bone formation.19 Due to its location, the solitary bone cyst afflicting our patient could be related to this theory since in the mandible, the primary ossification point is located close to the mental foramen, therefore, it is an ideal area for the onset of a solitary bone cyst due to its predominantly close location to cartilage growth plates. In Blum's and Toma's studies, mentioned in Xanthinaki case11 it is concluded that there must be a predisposition of idiosyncratic factors in the pathogenesis of solitary bone cysts, such as peculiarities in the vessel walls or an abnormal blood clotting, related to chronic hypoxemia present in patients with Fallot's tetralogy, which might include altered calcium functions in blood clotting.28
Even though in most cases solitary bone cysts of the mandible are asymptomatic,10,11,18 reported pain and paresthesia were the reasons why the patient sought treatment. In this case, X-rays studies did not reveal presence of radio-opaque lesions concomitant with solitary bone cyst, therefore it was concluded that painful symptoms experienced by the patient were due to cyst location.
The lesion extended along the mandibular body without causing bone expansion; lower buccal and lingual cortical bone became thinner (Figure 4). There was no displacement of adjacent teeth towards the lesion; teeth responded positively to vitality tests. These data concur with those reported by Chrcanovic's30 and Xanthinaki's11 clinical case studies. Microscopic study revealed trabecular bone lacking significant histological data, such as mentioned by Harnet et al.9
In spite of multiple treatments suggested in scientific literature to treat solitary bone cysts,12,13,18 in our case, when the lesion was approached to harvest the biopsy and no epithelium was found, it was decided to perform bone curettage of cavity walls and bone regeneration induction.
Control X-ray examination was conducted one year after surgery, bearing in mind results reported by Suei et al18 where it was stated that lower frequency of control examinations will result in lesser patient exposition to radiation. In most cases resolution or recurrence are confirmed at the first or second radiographic controls in a 3 year span after surgery since diagnosis of early recurrence is not significant when we consider that this is a progressively growing lesion.
CONCLUSIONSIn solitary bone cysts cases, undoubtedly, the determinant factor is surgical exploration of the lesion, although its clinical characteristics and scientific literature descriptions must be borne in mind as well as the fact that histological and radiographic characteristics are important to sustain accurate diagnosis.
Since etiology of these cysts is unknown to the present date, it can only be intuited according to personal characteristics of each patient. The most accepted theory suggested a traumatic origin for these lesions. Nevertheless, when trauma is discarded as etiologic factor, the most accepted theory would be related to calcium metabolism alterations associated to the overall condition of our patient.
Some authors suggest to preserve the lesion in observation hoping for a possible spontaneous resolution. Nevertheless, we decided to undertake surgical approach due to the painful symptoms reported by the patient and to discard as well the possibility of other lesions. We suggest to undertake surgical approach of any lesion with presumptive diagnosis of solitary bone cyst.
Although it is reported in scientific literature that solitary bone cysts are asymptomatic, we concluded that paresthesia and painful symptoms experienced by our patient were related to the anatomical location of the lesion. Oftentimes it is not possible to establish a diagnosis through histopathological study due to insufficient amounts of sample, which would be the case in empty solitary bone cysts, or cysts with scarce fibrous connective tissue adhered to the cavity walls. Moreover, results can provide non-significant characteristics for differentiation of other pathological lesions, or even in proper diagnosis of solitary bone cysts.
Other treatments could be applied, such as bovine freeze-dried bone graft, iliac crest cancellous bone, introduction of autologous blood with patient's bone or hydroxyapatite, to be achieved in cases of recurrence, in cases of extensive solitary bone cysts, or when cysts are concomitant with other lesions.
Maxillofacial surgeon at the Specialty Regional Hospital Bicentenario de la Independencia, ISSSTE (National Institute of Social Services for Government Employees), State of Mexico.
This article can be read in its full version in the following page: http://www.medigraphic.com/facultadodontologiaunam
Graduate, School of Dentistry, Faculty of Graduate Studies, Iztacala National University of Mexico (UNAM).