Re-implantation is a procedure whereby an accidentally or intentionally fully luxated tooth is placed in a socket. It is considered a form of tooth transplant. This treatment can adequately function, in certain cases, ankylosis might be present. This process can be defined as fusion of tooth and alveolar bone.
ObjectivePresentation of a re-implanted, ankylosed endodontically treated tooth with root resorption and replacement of this tooth with dental implant.
Case presentationA 32 year old female patient was referred to Periodontics and Implantology Department due to bone resorption of tooth number 12. Dental history reported by patient informed that tooth was extracted and intentionally re-implanted after endodontic treatment. After thirteen years the crown fractured, radiographic examination revealed external root resorption and ankylosis. Treatment consisted on guided bone regeneration after extraction and placement of 3i® implant (3.5 × 15mm) with immediate load, the gingival margin was modified by means of gingivoplasty procedure and increase of provisional's crown contour. In order to improve esthetics and morphology of keratinized gingiva, muco-gingival plastic surgery was conducted with rotary instruments.
ResultsOne year later, rehabilitation was completed with a screwed-in, fixed porcelain crown.
La reimplantación es la colocación en el alvéolo de un diente totalmente luxado (accidental o intencionalmente); es citada como una forma de trasplante dental; este tratamiento puede funcionar adecuadamente y en algunos casos se presenta anquilosis, definiendo este proceso como la fusión del diente y el hueso alveolar.
ObjetivoPresentar un diente reimplantado, con tratamiento endodóntico, anquilosado, con reabsorción radicular y su sustitución con un implante dental.
Presentación del casoPaciente femenino de 32 años, remitido al Departamento de Periodoncia e Implantología por resorción ósea del OD 12. Como antecedentes dentales referidos por el paciente, el diente fue extraído y reimplantado intencionalmente después del tratamiento endodóntico. Después de trece años, la corona se fracturó y en el examen radiográfico se apreció resorción radicular externa y anquilosis. El tratamiento consistió en regeneración ósea guiada post-extracción y a los seis meses la inserción de un implante 3i® de 3.25 × 15mm, con provisional inmediato, el margen gingival fue modificado por medio de gingivoplastia e incremento en el contorno del provisional. Para mejorar la estética y morfología de la encía queratinizada se realizó una cirugía plástica mucogingival con instrumentos rotatorios.
ResultadosDespués de un año se concluyó la rehabilitación que consistió en una corona atornillada de porcelana.
Tooth rehabilitation is an event with high demands of care in common circumstances, but, when linked to biological aspects, they can contribute to results’ success or failure, such is the case with patients afflicted with ankylosys problems.
When a tooth is re-implanted (placed in its sockets after accidental or intentional full luxation) repair process can sometimes be ankylosis1,which is defined as the fusion of tooth to alveolar bone.2
Ankylosis etiology might be diverse: it can be a lesion secondary to tooth resorption, hypercementosis, retained teeth, ancient root remnants and re-implants. Histopathological study of this condition shows existing continuity between affected tissues, with normal histological characteristics except for the absence of periodontal ligament.3
A normal periodontium, ankylosis and bone integration are physiologically related to bone dynamics. It has thus been observed that ankylosed teeth and bone-integrated implants can provide suitable occlusal function and become effective orthodontic anchors.4
In theory, ankylosis can be detected as a fortuitous event in periapical X-rays, due to loss of periodontal ligament space in small areas. Nevertheless, early diagnosis of ankylosis in X-rays is frequently difficult, due to the fact that ankylosed areas are very small or located in ill-visible sides of the root. Nevertheless, due to its asymptomatic nature, clinical diagnosis of ankylosis depends on the change of sound observed upon tooth percussion as well as a marked decrease of physiological lingual-facial excursion.5
Although etiology of ankylosis has not yet been clearly ascertained, some local conditions such as periapical infections, trauma and previous surgical procedures can be possible causes.6
By definition, if a tooth is ankylosed, it cannot move or erupt.6 It is for this reason that literature proposes that orthodontic forces (loads) used as treatment could not align the tooth, and would cause undesirable movement of adjacent teeth, moreover, the tooth could experience progressive root resorption.7–9
Areas of ankylosis are removed during surgical removal of the tooth. Moreover, there can be luxations of some residual portions, therefore, we must try to gain socket-like biological space for the bone, to become the future site in which to place the implant.11,12
CASE PRESENTATIONThe patient was a 32 year old female. An apparently healthy kindergarten teacher who was referred to the Periodontics and Implantology Department of the Graduate and Research School of the National School of Dentistry, National University of Mexico (UNAM) due to bone resorption of tooth number 12.
The patient reported that, at age 18, she was treated by a dentist for a carious lesion in tooth number 12. After the restoration was placed, she experienced persistent pain, therefore she was subjected to a root canal treatment at said tooth. The patient reported continuance of pain after this procedure which was probably due to an infection at the site. As part of treatment, the clinical operator decided to perform an extraction and re-implatation of toot number 11. The patient reported no discomfort in the area. When she was 28, esthetic reasons propted her to attend an orthodontist, who designed a treatment plan which included premolar extraction in the upper jaw. Treatment was discontinued after two years due to the fact thet tooth 12 did not show any movement; this caused the patient to suffer diastemas between upper teeth and in the esthetic zone lacated between teeth 13 and 12 (Figure 1).
When the patient was 31, the lateral tooth fractured during mastication; that prompted her to seek care at our institution.
The patient reported as first priority to restore tooth number 12 and achieve a natural-looking smile, without causing modifications to the remaining anterior area (Figure 2).
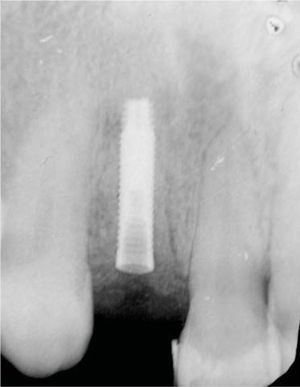
Radiographic findings revealed external root resorption in the tooth's neck area as well as ankylosis (Figure 3).
TREATMENTWith patient's previous informed consent, surgical procedure was executed in the three following procedures:
Periodontal phase 1 was conducted as a beginning, according to treatment plan.
First procedure- 1.
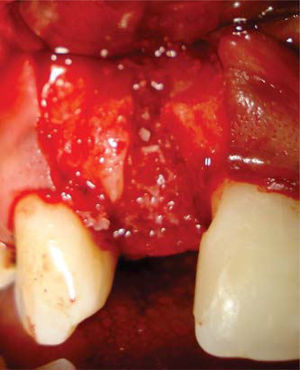
Extraction of crown of tooth 12 with the help or periostomes and extraction root remnants with rotary instruments (Spiral burr ACT30153i®) (Figure 4).
- 2.
Guided bone regeneration with 15 × 20mm resorbable collagen membrane (BIOMEND®) and bone xenograft 1g 500-1,000μ) (BIOCRISS®).
The aim of these steps was to preserve bone architecture for later implant placement (Figure 5).
Immediate provisional structure was achieved with an ovoid pontic with the crown of the extracted tooth, which was splinted with resin onto adjacent teeth (Figure 6).
Second procedure (six months later)- 1.
Use of burrs in order to place the implant without raising a flap.
- 2.
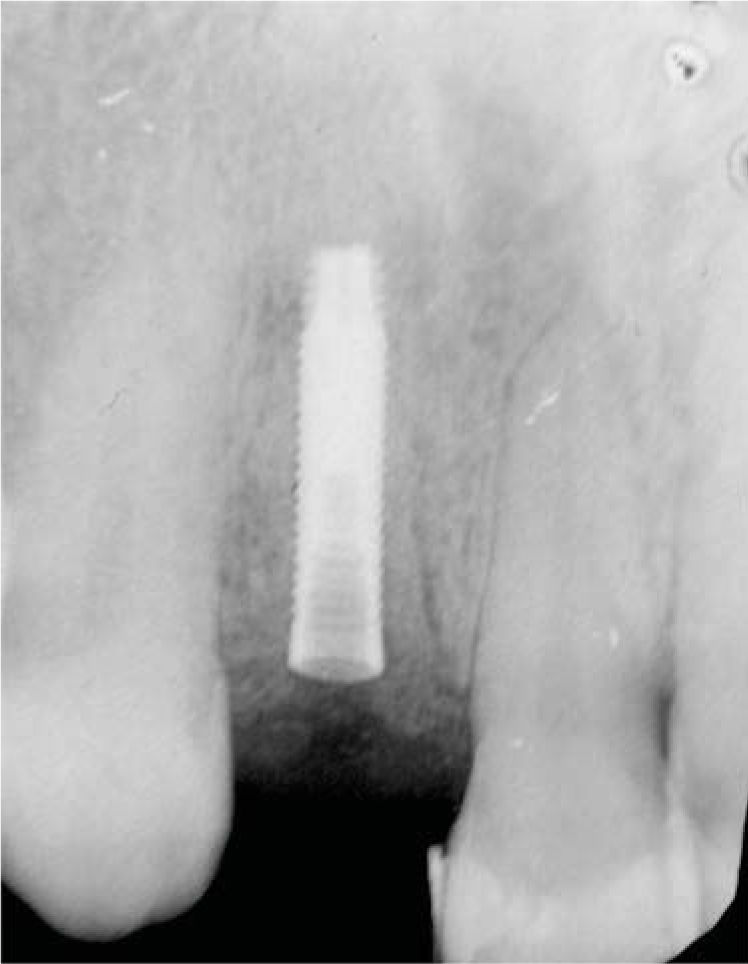
Placement of implant 3i® Osseolite Certain Micro Miniimplant. Implant measured 3.25mm in diameter and 15mm length (Figure 7).
Period of implant placement was classified as type 4, considering the fact that the ridge was clinically healed and soft tissue maturation allowed suitable manipulation.13
Prosthetic phase was conducted according to treatment plan at the Oral Prosthesis and Implantology Department of the Graduate and Research School, National School of Dentistry, National University of Mexico (UNAM): a pre-fabricated, 3.4 with acrylic crown immediate provisional device14 was placed (Certain 3i®) (Figure 8).
During these two procedures, pharmacological treatment included amoxicillin (750mg every 12hours for 8 days), ibuprofen (400mg every 6hours for 5 days) administered by mouth.
Third procedure ten months after extraction- 1.
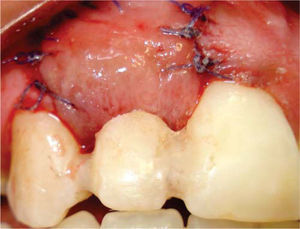
Internal chamfer (bezel) gingivoplasty.
- 2.
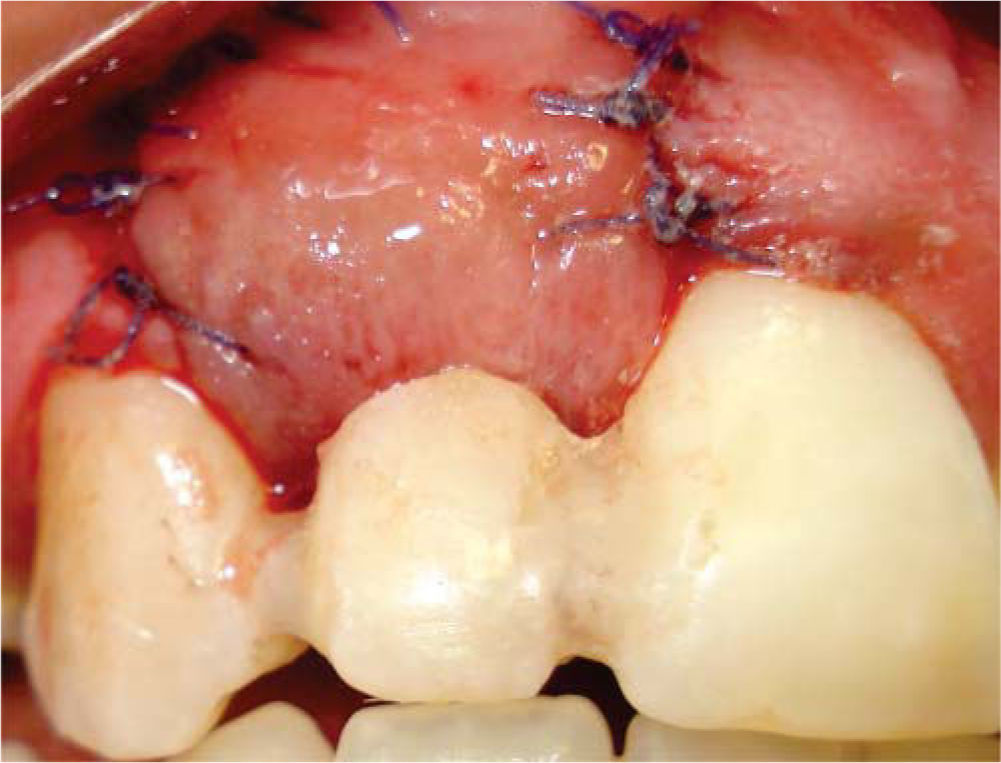
Muco-gingival plastic surgery with rotary instruments low speed diamond round burr (801.314035) (Edenta®, Switzerland) (Figure 9). The target of this procedure was to diffuse scars of previous surgeries in the keratinized gingiva.
Diagnosis of pathological processes such as ankylosis, cervical fracture and resorption commits the clinician to present treatment alternatives to replace teeth with poor diagnosis.15 The present case prompted the clinician to undertake non conventional procedures other than extraction, such as use of rotary instruments, in an attempt to preserve the greatest possible amount of alveolar bone, so as to be able to place an implant at a later date.
Use of a collagen membrane as a physical barrier, along with a bone graft in order to regenerate extraction site resulted in a suitably-sized flange to place an endo-osseous implant.16
Implant insertion surgery did not include flap raising, a trepan was used to remove gingival tissue and gain access to the bone, preserving gingival margin and papillae,17,18 thus avoiding recession in the presence of more stable tissues. After this, margin festoon was modified with an internal bevel which provided ideal length to the crown.
Low speed rotary instruments used to fade incision scars provided uniform color and aspect at the extraction site.
Prosthetic rehabilitation was completed 18 months later, it consisted on a screwed-in, implant-supported feldspathic porcelain crown (Noritake® Japan) with burnout device and gold ring (3i®) (Figure 10).
DISCUSSIONAnkylosis is a common phenomenon after a traumatic event such as dental luxation or avulsion; this can result in local destruction of the periodontal ligament.19
Replacement resorption is the result of an extended lesion of the periodontal ligament's most internal layer, and probably of cement as well.9
Treatment of an ankylosed permanent tooth might include surgical removal of the tooth and replacement with a fixed or removable prosthesis. A vertical or horizontal defect might appear after removal, which might hinder or preclude an esthetic prosthetic replacement.
In the upper jaw, tissue deficiencies might correspond to two categories: anatomical events such as congenital anodontia and pathological situations such as dental trauma, bone atrophy, acute and chronic infections as well as post-traumatic conditions such as ankylosed roots.10
In these cases, vertical and horizontal reconstruction of alveolar defects is required before implant placement.
In order to assess possible socket defects after extraction, integrity of existing soft and hard tissue must be considered, and number of remaining walls, circumstances of these walls, irrigation an clot-forming ability must be determined.
In order to achieve accurate assessment, before placing the implant, it is recommended to use a surgical guide with position of the future restoration's margin. It is also important to explore the socket using the tip of the probe in order to assess the level of the bone crest with respect to the gingival margin, palatal and buccal tables and inter-proximal crest.19
According to socket defect classification20 recommendation is made to preserve the socket and place the implant at a later two-phase stage. In the present clinical case it was considered that damage was moderate, since the absence of one socket wall severely compromised the soft tissue. Scientific literature informs of a 99.1% survival rate for immediate, non functional load implants.21
For this reason it is essential to control external dimensional changes in the socket which might occur six to twelve months after extraction, there can be horizontal reduction of 5-7mm = 50% thickness of the initial flange and a vertical 2-4.5mm reduction.22
Increase in horizontal dimension is a welldocumented procedure possessing maximum effectiveness and predictability, whereas increasing vertical defects caused by guided bone regeneration is a technically demanding treatment due to its unsatisfactory results.19
Iasella et al23 compared healing of an intact socket with and without bone graft and collagen membrane; they found that in control sites, thickness of the buccal aspect mucosa increased 0.4mm at four months, and in experimental sites thickness of mucosa decreased 0.1mm.
Socket full epithelialization was observed after 5 weeks, nevertheless, organization and maturation of collagen bundles adjacent to lamina propia took longer. Amount of histologically observed bone was greater in grafted sites, although they included vital and non-vital bone.23
The implant load was conventional. This concept is defined when the prosthesis is inserted in a second procedure, after healing period of three to six months.
Provisionalization was described in the present case as an immediate restoration, since it was placed in the 48hours following implant placement, but lacking occlusal function.24
Surgical considerations required to achieve immediate restorations are: implant selection, distribution and position guided by rehabilitation plan, diagnosis and surgical guides, minimization of biomechanical risks, implant clinical stability when there is suitable bone quantity and quality, on the contrary, it is advisable to select implants with rugged surfaces, adequate dimension and suitable clinical techniques in order to preserve contact between implant and bone.21
In order to achieve suitable esthetics in the rehabilitation of these compromised cases general assessment and esthetic analysis must be determined. After this, the 2 or 3 goals of the esthetic treatment must be established with the patient. All these details must be stated in simple language in the consent form. Before waxing-up procedure, it is necessary to establish a preview of length, filling and/or knowing whether gingival levels must be corrected. According to case difficulty, this preview can be directly or indirectly achieved, providing thus the patient with a general idea. Incisal position, length and anterior guide are of special importance at this stage. The patient wears the provisional restoration after which function, length, incisal profiles and finally details when smiling and occlusion are re-evaluated.25
CONCLUSIONSAnkylosis is an asymptomatic event which does not require treatment. Nevertheless, when patients exhibit a poor prognosis, and extraction is necessary, the surgical effort involved to remove the tooth might imply use of rotary instruments which might preserve the shape of the socket, as we have suggested. At a later point, affected bone tissue regeneration must be achieved avoiding thus bone defects which might compromise the quality of the flange.
In rehabilitation with implants, ankylosis is considered a high risk factor due to supporting tissue loss, therefore, being able to determine the implant's placing time plays an essential role to achieve soft and hard tissue stability, especially in areas where there are esthetic concerns.
Graduated, Implantology and Periodontics Clinic.
This article can be read in its full version in the following page: http://www.medigraphic.com/facultadodontologiaunam