Epulis fissuratum is a pseudotumor growth located over the soft tissues of the vestibular sulcus caused by chronic irritation from poorly adapted prostheses. The definitive treatment is excision with appropriate prosthetic reconstruction. The use of laser carbon dioxide (CO2) in the treatment of these lesions presents many advantages over conventional surgery including surgical technique without direct contact with tissue, without bleeding or need for sutures, minimal postoperative pain and edema. The haemostatic capacity of CO2 laser is describe widespread being a usefull instrument for oral surgery in patients that suffered from clotting disorders.
ObjectiveThe aim of this article is to present a case of epulis fissuratum in a patient with antithrombotic medication demonstrating the usefulness of the CO2 laser for treatment of this lesion.
Case reportWe present a case of a 72 years-old female, referred to Hospital Nossa Senhora da Conceição de Valongo, Porto, with growth of vestibular oral mucosa in the mandible and maxilla associated with ill-fitting prostheses, suggestive of epulis fissuratum. She was taking antithrombotic medication. These lesions were excised with CO2 laser. Three weeks after surgery, both areas were completely reepithelizaded. No significant complications were recorded as hemorrhage, pain, swelling or infection. Prosthetic rehabilitation and function were achieved with the fabrication of new upper and lower dentures. The patient was seen a month and 1 year after treatment lying free of recurrence.
ConclusionThe use of CO2 lasers are nowadays the Gold Standard in the excision of this type of pathology especially in patients with hemorrhagic diathesis or antithrombotic therapy.
Uma epulis fissuratum é um crescimento pseudotumoral localizado nos tecidos moles do sulco vestibular causado pela irritação crónica de uma prótese dentária mal adaptada. O tratamento definitivo é a sua excisão com reconstrução protética adequada. A utilização de laser de dióxido de carbono (CO2) no tratamento destas lesões apresenta muitas vantagens sobre a excisão convencional não apresentando contacto directo com os tecidos, sem sangramento ou necessidade de suturas, e com dor e edema mínimos. A capacidade hemostática do laser de CO2 está bem descrita sendo um instrumento útil em cirurgia oral em doentes com alterações da coagulação.
ObjectivosO objectivo deste artigo é apresentar um caso de uma doente com epulis fissuratum que realizava medicação anti-agregante plaquetária, demonstrando a utilidade do laser de CO2 no tratamento destas lesões.
Caso clínicoApresentamos um caso de uma mulher de 72 anos, enviada ao Hospital Nossa Senhora da Conceição de Valongo, Porto, com crescimento da mucosa oral vestibular na maxila e mandíbula associadas a próteses dentárias desadaptadas, compatíveis com epulis fissuratum. A doente realizava anti-agregantes plaquetários. Ambas as lesões foram excisadas com laser de CO2. Três semanas após a cirurgia, ambas as feridas operatórias encontravam-se completamente cicatrizadas. Não se verificaram complicações significativas como hemorragia, dor, edema ou infecção. A reabilitação protética foi realizada com novas próteses totais superior e inferior. A doente foi observada após um mês e um ano encontrando-se livre de recidiva.
ConclusãoA utilização do laser de CO2 é hoje em dia fulcral na excisão deste tipo de patologia especialmente em doentes com diáteses hemorrágicas ou com terapias anti-trombóticas.
Epulis fissuratum is a pseudotumor growth located over the soft tissues of the vestibular sulcus caused by chronic irritation from badly adapted prostheses with variable degrees of hypertrophy and hyperplasia.1 Clinically, this adaptive lesion presents a raised sessile lesion in a form of folds, with a smooth surface and normal mucosa coloration.2 Depending on the intensity of the trauma, the surface may become ulcerated. The definitive treatment is excision with appropriate prosthetic reconstruction. Recurrences are rare as long as the sources of trauma and/or the patient's habits are eliminated and the appropriate prosthetic rehabilitation is provided.1,2
In modern societies, there is an increasing number of older patients with common systemic diseases such as cardiovascular diseases, especially those treated with anticoagulation therapy because of cardiologic indications. In last years, some guidelines of dental management of patients using anti-thrombotic drugs recommended to not routinely discontinue anti-platelet and anti-coagulation medication before dental surgery. As result the risk of a severe bleeding during or after oral surgical procedures is elevated.3
Lasers have been in use in the medical community since the 1970s. In the 1980s, oral surgeons began using carbon dioxide lasers for soft tissue procedures, and in 1989 the first laser specifically designed for use in dentistry was introduced.4 Nowadays, the most used lasers in oral surgery are CO2 laser, Er:YAG laser, Nd:YAG laser, diode laser, argon laser and KTP laser. The CO2 laser emits energy with a 10.6μm wavelength in the infrared zone that is absorbed by water. The high water content of the oral soft tissues makes this laser a useful tool in oral soft surgery with many advantages over conventional surgery including convenient mucosa removal, excellent haemostasis with a bloodless field, high precision in tissue destruction, no need for sutures, non contact surgery, bactericidal properties that minimize the possibility of infection and minimal postoperative pain and edema.2,5-7 The haemostatic capacity of CO2 laser is describe widespread being a useful instrument for oral surgery in patients that suffered from clotting disturbances.8,9 The aim of this article is to present the treatment of a maxillary and mandibular epulis fissuratum in a patient with antithrombotic therapy with CO2 laser surgery and prosthetics rehabilitation.
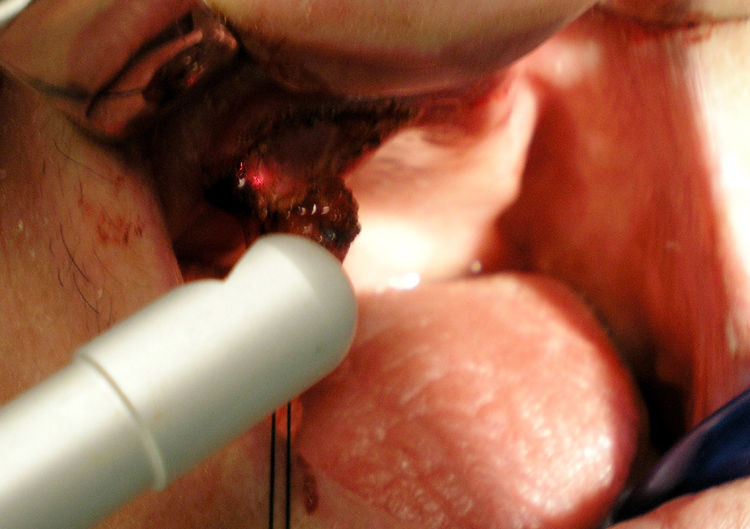
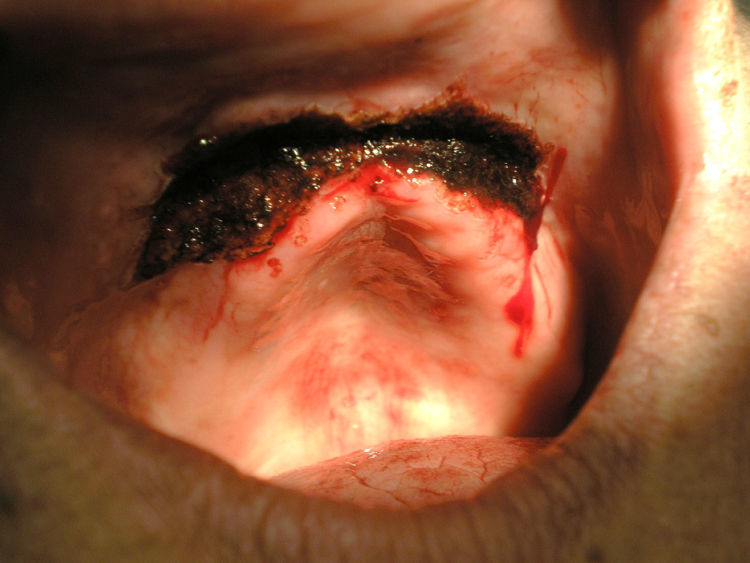
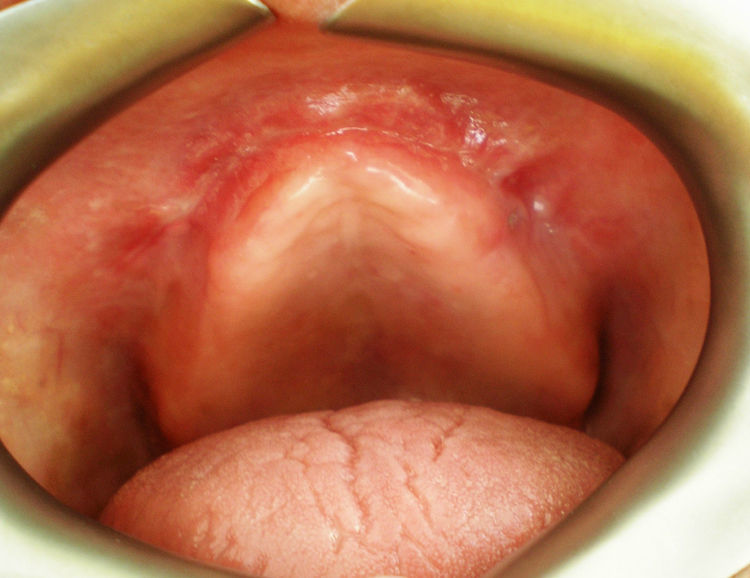
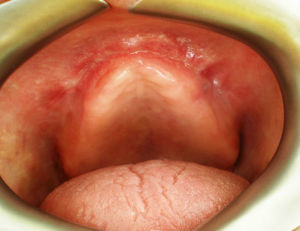
Case reportA 72 years-old women was referred to Hospital Nossa Senhora da Conceição de Valongo (ISCSN/CESPU, Porto, Portugal) for evaluation of a maxillary and mandible gingival mass. She reported a gingival enlargement with 12 months of evolution with oral discomfort using booth prostheses. She had arterial hypertension, congestive heart failure, osteoporosis, diabetes mellitus (type II). Habitual medication included ticlopidina 250mg, glibenclamida 20mg, and captopril 25mg. On oral examination a fibrous mass of 6×2cm, with multiple folds, and normal mucosa coloration was located on mandibular vestibular sulcus and two other similar fibrous masses, with 2×1cm each, were in maxillary vestibular sulcus (Figs. 1–3). She was using upper and lower complete prostheses both badly adapted. There were no cervical or submandibular adenopathy. Epulis fissuratum presumptive diagnoses were made. Complete blood count, coagulation tests and general biochemistry were within normal values with an INR of 2.1. She had not stopped her habitual medication for surgery. These lesions were treated under local anesthesia with carbon dioxide laser (DEKA™ Smart US 20D), pulse mode, 0.9mm focus, 5-6W power (Figs. 4–7), focalizing the beam for mucosal cut and defocalizing when tissue vaporization was required.10 Usual safety precautions of protecting the operator, patient, and assistant were followed. Only the site of surgery was exposed; all other areas were protected with wet gauze. Aditionaly to epulis removal we perform a partial vestibuloplasty. No suturing was used and the wound was allowed to repair by second intention. Excised tissues were submitted for routine histological examination on 10% formalin solution with indication of a CO2 laser excision. Appropriate new prosthetic rehabilitation was provided. After 3 weeks, wound healing was completed uneventfully (Figs. 8 and 9). In maxillary sulcus a 3-mm depth extension was gained, increasing the prosthesis retention. She didn’t report postoperatory pain or oedema. On histopathology report both lesions revealed “fibrous tissue with some lymphocytic infiltration, limited by a stratified epithelium with acantosis. There were no signs of malignancy”. It was concluded that these lesions were both epulis fissuratum. The patient was seen in 1 month and one year after and was free of recurrence.
DiscussionEpulis fissuratum is not a true tumor but an adaptive fibroepithelial response due a chronic low-grade irritation from poorly adapted prostheses with variable degrees of hypertrophy and hyperplasia. The term epulis, first used by Virchoff, that means over the gums, it′s not appropriate to these lesions as the affected mucosa is oral mucosa of vestibular sulcus and not gingival mucosa.1,11 On the other hand, the term epulis refers only to the site. In this view some authors prefer to call these lesions denture-induced fibrous hyperplasia.12,13
Most of epulis fissuratum occur in the anterior region of the upper or lower jaws.1,5,13 Simultaneous upper and lower presentation, as in present case, is less frequent. More than 60% have a multifold presentation.5 They present more in females and in a advanced age.1,13 The most frequent complaints are a fibrous mass in the mouth, as happened in our case, disuse of dentures, pain or the need for renewal of dentures.13
Surgical excision is the definitive treatment of epulis fissuratum, always with appropriate prosthetic reconstruction. The treatment is usually performed with conventional surgery excision with scalpel. However this technique is related with significant loss of sulcus depth.5 In this view, CO2 laser excision is a useful tool in this type of surgery with its cutting precision and the uniqueness of its noncontact technique reducing the risk of infection and sterilization of the surgical wound. One of the main advantages over convencional surgeries is an excellent haemostasis. For these reasons there is no need for suture and the wound is allowed to repair by second intention. This allows the maintenance of an adequate sulcus depth important for achieving a correct peripheral seal for dental prosthesis retention and stability, preventing further recurrences.14
The patient presented in this article is one of many patients with cardiovascular disease medicated with antithrombotic drug. As recent guidelines suggests the patient cardiologist preferred not to suspend this medication during oral surgery.3 Over the past years, laser hemostasis has been established as an alternative to convencional techniques.7–9,15,16 Gáspár & Szabó, 1989, found no significant differences between the group of patients with hemorrhagic diathesis and control patients in the respect of the duration of operation, degree of bleeding and healing of the wound and complication.8 The authors conclude that CO2 laser high energy was found to be well applicable in the field of oral surgery owing to its excellent hemostatic effect. In our case we observed a good bleeding control in mandibular epulis and maxillary epulis. We think that CO2 laser is a precious help in the treatment of these patients. Blood vessels smaller than 0.5-mm diameter are spontaneously sealed, allowing excellent visibility (bloodless operating field) and precision when dissecting through the tissue planes.1 Comparative to scapel surgery a coagulum of denatured collagen on the surface is formed and with laser sterilization of wound, the acute inflammation reaction is delayed and minimal, with few myofibroblasts and hence little wound contraction.7 All these advantages minimizes possible postoperative hemorrhage.
Additional and important advantages of CO2 lasers, as we observed in our case, are minimal postoperative complains as pain, infeccion and edema.2 Attending to the size of the lesions here presented it is remarkable that during operative and postoperative period pain was absent. This is an important advantage of CO2 laser treatment report by many authors. Pogrel et al, 1990, attributed this reduction in pain to the fact that the inflammatory reaction associated with CO2 laser application is reduced, since blood and lymphatic vessel sealing occurs, with prevention of the extravasation of fluids responsible for inflammation and pain.17 Moreover, laser irradiation cause sealing of the nerve endings in the surgical contact area and the denaturalized collagen layer formed on the surface of the surgical wound serves to isolate from the oral fluids.17,18 However, with secondary cicatrization epithelial regeneration is delayed and the wounds take a longer time to re-epitheliase.4,6,7
The healing process was finish at three weeks without scaring and with anatomic sulcus integrity. Fisher & Frame, 1984 suggest treatment of epulis fissuratum with CO2 laser without first intention, since second intention healing was seen to cause scant tissue alteration and little loss of vestibular depth.18 In the present case, in maxillary sulcus, a 3-mm depth extension was even gained, increasing the prosthesis retention. Dentures must be readjusted and placed as soon as possible.2,17,19 Recurrences are rare as long as the sources of trauma and/or the patient's habits are eliminated and the appropriate prosthetic reconstruction is provided. Tamarit-Borrás et al, 2005, observed that the relapse cases of patients that had epulis fissuratum CO2 laser excision, had failed to replace or re-fit their dentures.1
In this view, we considered that CO2 laser excision with readjust of dentures is the best treatment for these patients. The CO2 laser effectively removed both lesion and kept bleeding under control during the surgical procedure e postoperative period. This is in accordance with other works. Keng & Loh, 1992, in 20 patients submitted to epulis fissuratum CO2 laser excision observed bleeding control in most patients, with no hemorrhage in the postoperative period, as well notable absence of pain and infection.5 Tuncer et al, 2010, observed that CO2 laser was an effective instrument for soft tissue excisional biopsies with minimal intraoperative and postoperative complications and good pain control compared to scalpel surgery.6
In conclusion, given the intrinsic qualities of CO2 laser when used for oral tissue surgery, it is reasonable to assume that this treatment option should become the Gold Standard in denture related hyperplasias, especially in patients with hemorrhagic diathesis or antithrombotic therapy.
Conflicts of interestThe authors have no conflicts of interest to declare.