Diagnosing a vertical root fracture may be a challenge because of the similarities with other pathologies. In the presented cases, endodontic treatments were performed as part of the overall treatment plan for full arch rehabilitation. The symptoms and signs were recorded and the extracted teeth analyzed. The fractured teeth were from bruxer patients. All teeth had deep located periodontal pockets, gingival swelling, tenderness to percussion and radiographic bone loss. Because the fracture line may not be visible in the crowned teeth with vertical root fracture, special attention has to be given to the clinical symptoms and signs. The clinical features of this pathology may vary from case to case. The purpose of this work is to contribute to a better knowledge of the signs and symptoms of this pathology.
Tendo em conta as semelhanças com outras patologias, o correto diagnóstico das fraturas radiculares verticais pode ser um desafio. Nos casos apresentados, os tratamentos endodônticos foram realizados devido a necessidades prostodônticas. Os sinais e sintomas foram registados e as peças extraídas analisadas. As fraturas registadas pertenciam a pacientes bruxómanos. Todos os dentes fraturados apresentavam bolsas periodontais localizadas, inflamação gengival, dor à percussão e perda óssea visível radiograficamente. Nestes casos clínicos deve ser dada uma especial atenção a todos os sinais e sintomas, uma vez que nem sempre é possível observar clinicamente a linha de fratura. Algumas características clínicas podem variar de caso para caso. O objetivo deste trabalho é contribuir para um melhor conhecimento das características desta patologia.
The symptoms and clinical signs of vertical root fracture (VRF) may be very easily confused with endodontic failure or periodontal disease.1,2 Just like with VRF, endodontic and periodontal pathology may have symptoms that include tenderness to percussion, palpation and pain upon chewing. Clinical signs can also be present as fistula, swelling, abscess and a deep probing depth.1,2 Radiographic features as vertical bone loss may be also compatible to several diagnoses.3 A correct treatment approach is dependent upon a correct diagnosis. The diagnosis of a VRF may be challenging because it is difficult to visualize, especially in teeth with crowns. This creates difficulties when a practitioner wants to formulate a treatment plan and there is some doubt of a VRF. It is of increased importance for one to understand that the most predictable treatment plan for the VRF is tooth extraction.4,5 The VRF has a prevalence of 13% of the extracted endodontically treated teeth.6
The purpose of this paper is to present two clinical cases of crowned premolars with root canal treatment that have vertical root fractures and to contribute to a better understanding of the signs and symptoms that may be present in this pathology so that a better diagnosis may be achieved.
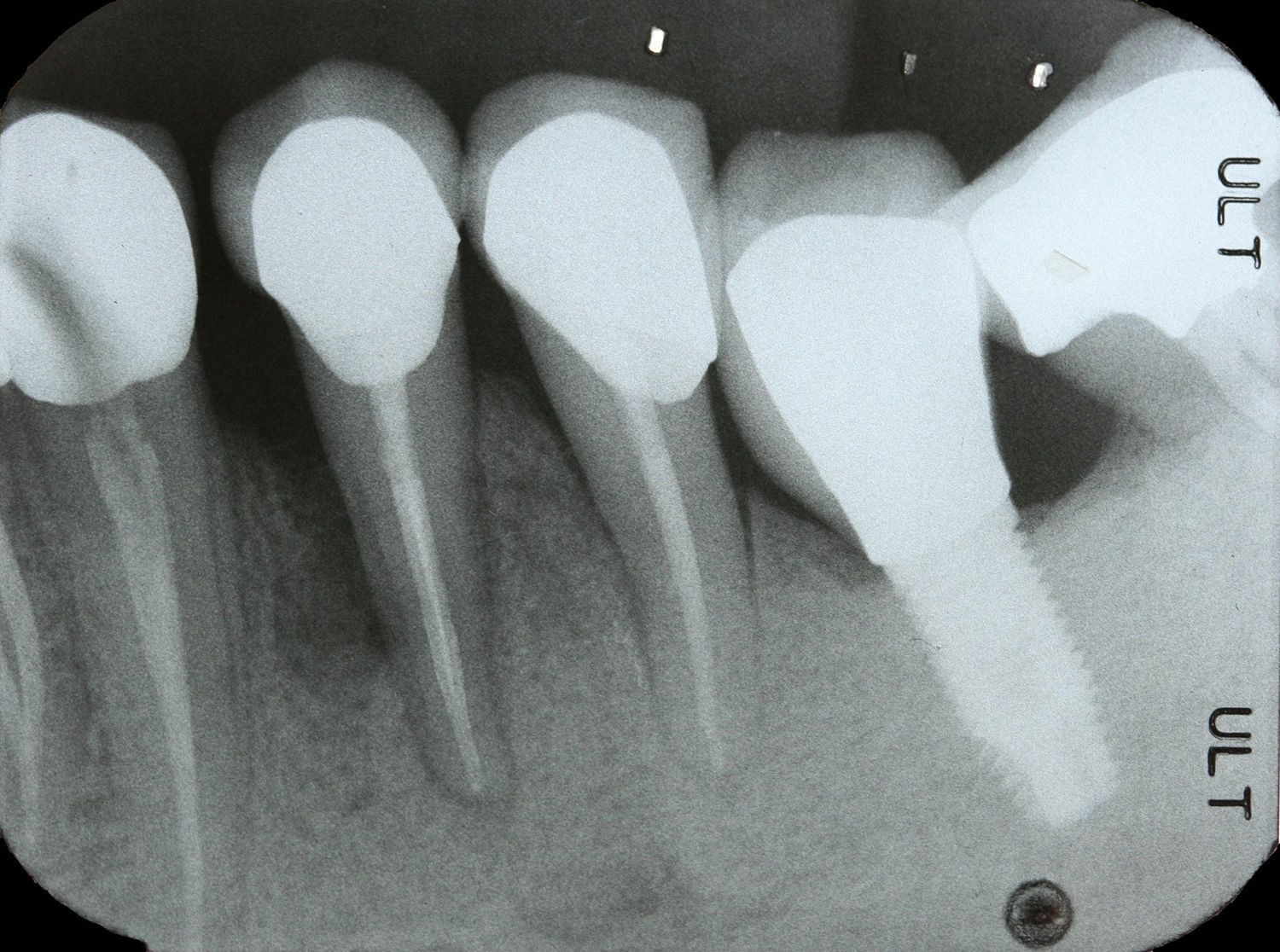
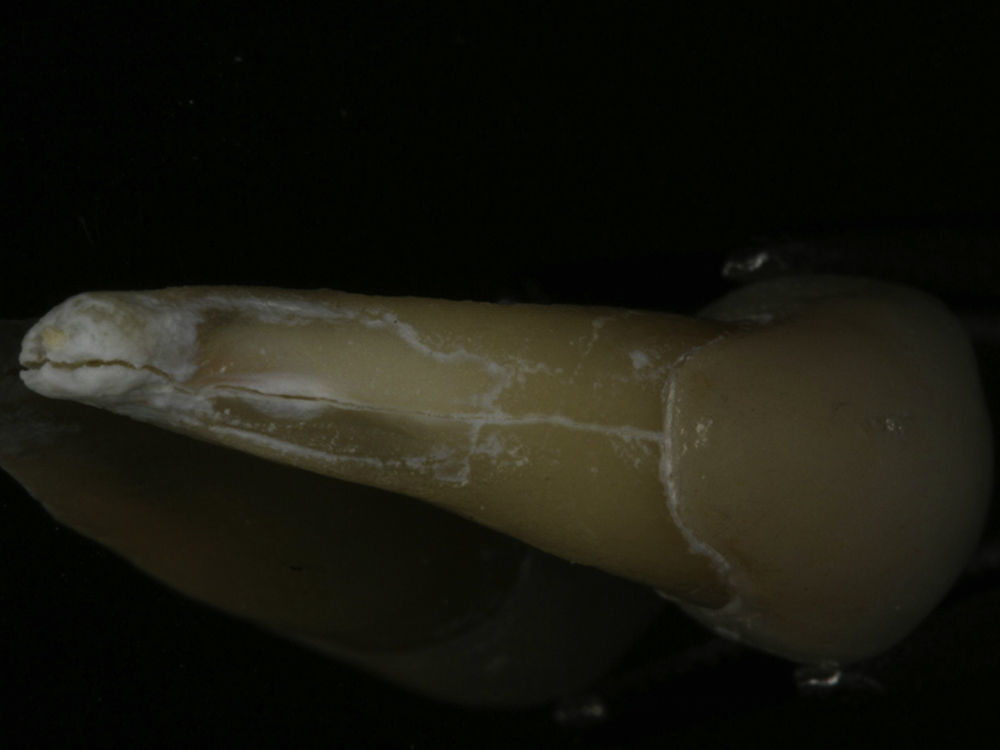
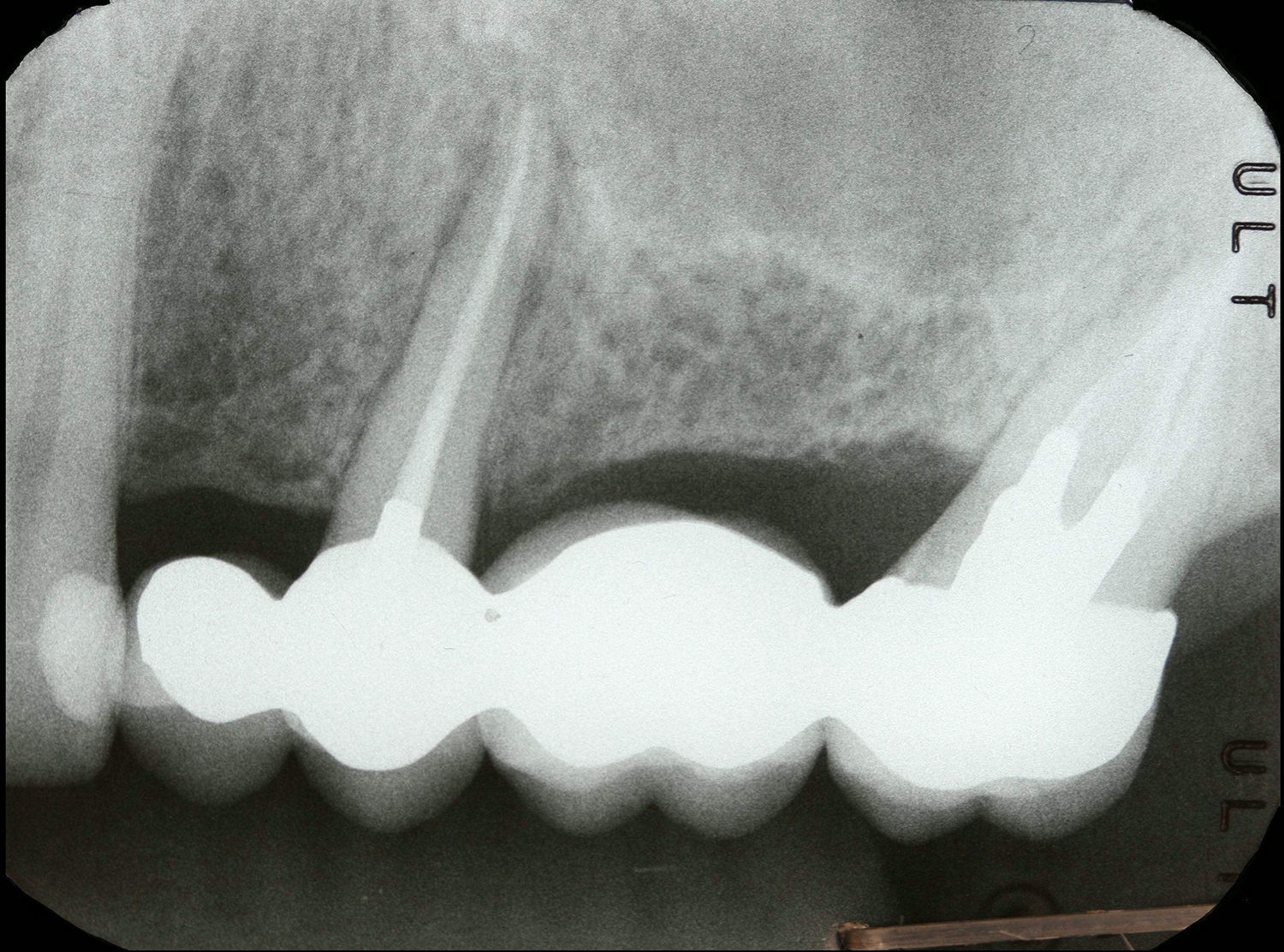
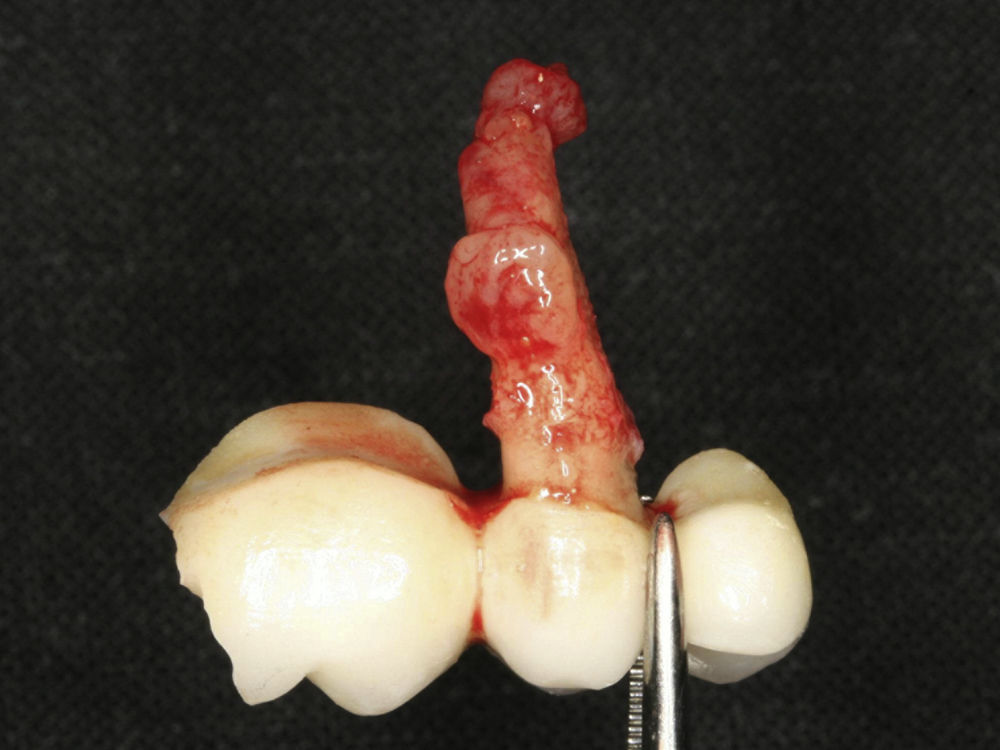
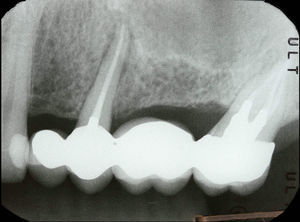
Case ReportCase report 1A 55-year-old male presented to an endodontic evaluation of tooth 34 (mandible first left premolar) and tooth 44 (mandible first right premolar). Heavy bruxism was diagnosed in the dental medical history. The patient confirms that he rarely uses his night mouthguard. The endodontic therapies were performed two years before as part of an oral rehabilitation plan following the quality guidelines of the European Society of Endodontology7. Tooth 34 had a cervical located fistula and gingival swelling. The tooth had tenderness to percussion and palpation and had a buccally located periodontal pocket of 7mm (Fig. 1) surrounded by normal periodontal depths of 3mm. A similar defect was present on the lingual periodontal region of the same tooth. A radiograph analysis was able to show a vertical bone loss of the mesial face to the root (Fig. 2). Based on the symptoms, clinical and radiographic signs a diagnosis of vertical root fracture was concluded. Extraction of tooth 34 was proposed and accepted. After the extraction it was possible to visualize the fracture lines (Fig. 3).
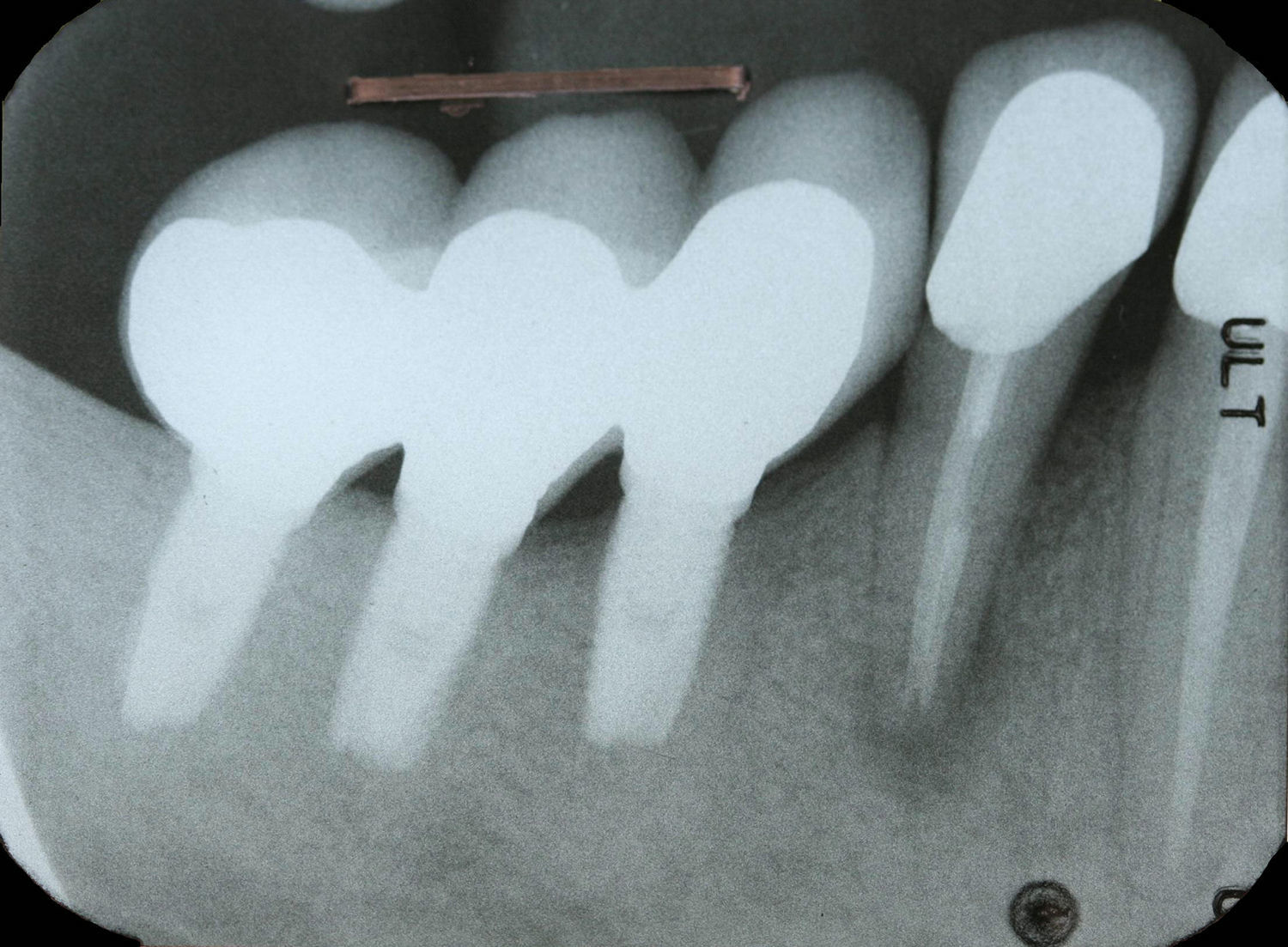
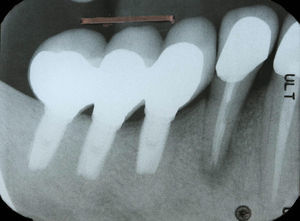
Tooth 44 was having symptoms and clinical signs similar to tooth 34 (Fig. 4), the radiographic analysis was able to show a halo lesion surrounding the root (Fig. 5). Similar diagnosis and treatment were presented to the patient, and it was possible to confirm the diagnosis after the extraction (Fig. 6).
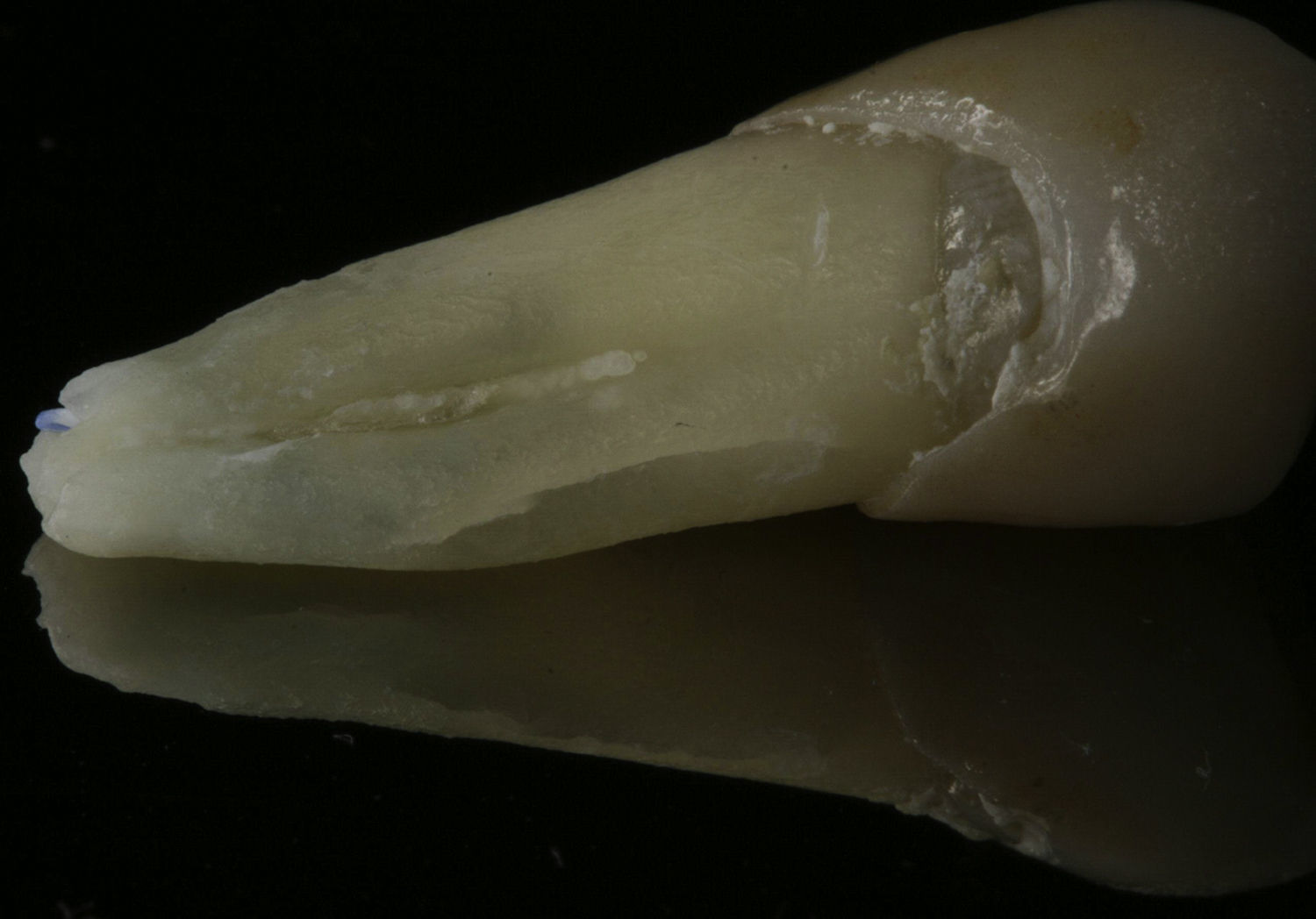
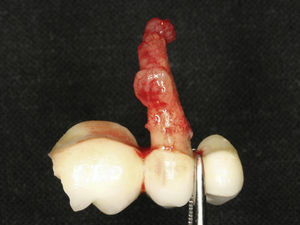
Case report 2A 45-year-old male presented to an endodontic evaluation of tooth 25 (maxillary second left premolar). Light bruxism was diagnosed in the dental medical history. The endodontic treatment was performed two years earlier. The tooth had tenderness to percussion, gingival swelling on the palatal region (Fig. 7) and a palatally located periodontal pocket of 8mm surrounded by normal probing depths. The radiographic analysis was able to show a halo lesion surrounding the root (Fig. 8). Based on the clinical and radiographic finding, a vertical root fracture was diagnosed and the extraction was proposed. After the bridge removal it was possible to observe granulation tissue attached to the root (Fig. 9) and the fracture lines (Fig. 10).
Causes for VRF may include excessive mechanical root canal preparation, excessive forces during the compaction of root-filling materials, excessive canal widening for post placement, lack of periodontal support, internal resorptions or occlusion stress.4,8–10
Four standard procedures have been described to allow a correct and definitive diagnosis: a visualization during an exploratory surgery,11 a visualization after tooth extraction,11 a radiographic visualization as long as there is a separation of fragments11 and a Cone Beam Computer Tomography visualization of the fracture.12,13
Since most of the times it is not possible to visualize the lines of fracture (Fig. 11), the diagnosis of VRF is based only on the symptoms and clinical signs. The most common sign of VRF is a deep probing pocket surrounded by normal pocket depths; this feature has a prevalence ranging from 64%14 to 93%15 of the cases. This characteristic appears because there is bone resorption surrounding the fracture line on the bone plate (Fig. 12). Lustig et al.,5 studying 110 VRF cases, were able to identify two types of bone resorption: a dehiscence defect and a fenestration defect. The dehiscence appears as a V-shaped bone loss with base in the coronal margin and was present in 91% of the cases. The fenestration defect appears as an oval shape bone loss preserving the coronal bone plate and was present in 9% of the cases. In all the cases the bone defects were surrounding the fracture line. Lustig et al.5 concluded, in their work, that the resorption is a consequence of a chronic inflammatory process where the granulation tissue replaces the bone following a bacterial infection that was able to gain an easy passage through the fracture line bypassing the defense line of the epithelial attachment. The same authors propose, after a correct VRF diagnosis, the extraction of the tooth without delay to prevent a more severe resorption of the bone plate.5 Despite some reported cases16,17 of successful treatment of VRF, the gold standard therapy for this pathology remains the fractured tooth extraction.4,5 The radiographic analysis may give some clues related to this bone loss. The most common radiographic feature of VRF is a halo radiolucency located on the lateral face of the root and extending to the periapical area,3 contrasting with the periapical radiolucency that remains surrounding only the periapex which is typical of the endodontic disease.3 Radiographic angular bone loss and periodontal radiolucency may also be present in the VRF.3 Llena-Puy et al.8 concluded in their study of 25 cases of VRF that periodontal pocket and a diffuse pain were the more common observation. These conclusions match the results of Tamse et al.18 where in 92 cases of VRF it was possible to identify a periodontal pocket in 67%, pain in 55%, tenderness to percussion in 56%, an abscess in 33% of them. These authors were also able to observe that the fistula, when present, frequently appeared closer to the gingival margin. Cohen et al.19 recorded pain to percussion in 69.74% of the cases, pain under mastication in 61.4%, while the presence of swelling and fistula were present only in 15.35% and 18.42% respectively.
Both cases presented in this report had VRF diagnosed just by analysis of the symptoms and signs since it was not possible to visualize any fracture. All cases had a localized periodontal pocket with gingival swelling and tenderness to percussion. Two of the teeth had a halo associated with the tooth in question on the radiographic image and one had a severe case of vertical bone loss. One of the cases had a fistula located near the gingival margin and both cases involved a patient who was a bruxer.
ConclusionsSince it may not be possible to visualize the vertical root fracture, clinical signs and symptoms are extremely important when attempting to make a diagnosis. Symptoms such as pain and tenderness to percussion or signs such as localized periodontal pockets, coronally located fistulas and radiographic halo radiolucencies may indicate a vertical root fracture. Not all the cases present the same features, and the diagnosis must be performed by analyzing a combination of features that may vary from patient to patient.
Ethical disclosuresProtection of human and animal subjectsThe authors declare that no experiments were performed on humans or animals for this investigation.
Confidentiality of dataThe authors declare that no patient data appear in this article.
Right to privacy and informed consentThe authors must have obtained the informed consent of the patients and/or subjects mentioned in the article. The author for correspondence must be in possession of this document.
Conflicts of interestThe authors have no conflicts of interest to declare.