The objective of this study is to describe a case of nasolabial cyst, treated successfully by surgical enucleation, and provide a brief review of the current state of knowledge on this lesion. A 47-year-old white woman presented with a painless, well-circumscribed left-sided mass near the ala nasi with marked facial deformity. Computed tomography showed a cystic lesion in the lateral nasal region. The lesion was excised through a sublabial incision and histopathological examination confirmed the diagnosis of nasolabial cyst. Nasolabial cysts originate from nonodontogenic tissues, their growth is limited to soft tissue, and their occurrence is considered infrequent. These cysts are usually asymptomatic and produce characteristic signs, such as elevation of the ala nasi and effacement of the nasolabial sulcus on the affected side. Imaging tests and microscopic examination will confirm the diagnosis. The treatment of choice is surgical excision.
O objetivo deste estudo é apresentar um caso de cisto nasolabial tratado mediante enucleação cirúrgica e rever a literatura existente a respeito desta lesão. Paciente do sexo feminino, leucoderma, 47 anos de idade, com queixa de tumefação indolor em região de asa do nariz do lado esquerdo. Foi submetida à TC, a qual demonstrou lesão de aspecto cístico em região nasal lateral. A lesão foi exposta e removida por meio de incisão Wassmund e submetida à análise histopatológica, que confirmou o diagnóstico de cisto nasolabial. O cisto nasolabial tem origem em tecidos nãoodontogênicos, é restrito aos tecidos moles e sua ocorrência é considerada infrequente. Em geral é assintomático e produz sinais característicos como elevação da asa do nariz e desaparecimento do sulco nasolabial do lado afetado. Os exames por imagem, complementados pela análise microscópica, são os definidores do diagnóstico. Seu tratamento é a remoção cirúrgica.
Nasolabial cysts are uncommon lesions located near the alar cartilage and extending into the inferior nasal meatus, superior alveolabial groove and floor of the nasal vestibule.1
Nasolabial cysts were first described by Zuckerkandl.2 The term nasolabial cyst itself was coined by Rao,3 and remains the most common name for this lesion, which has also been reported as nasoalveolar cyst, nasal vestibular cyst, mucoid cyst of the nose, and Klestadt's cyst, among a variety of other names.
It is classified as a developmental, nonodontogenic, extraosseous cyst, is usually located in the area of the nasolabial sulcus, just below the ala nasi, accounts for approximately 7% of maxillary cysts, and is unilateral in 90% of cases.4–6
The pathogenesis of nasolabial cysts is still uncertain. They were initially believed to originate from fusion of the globular, lateral nasal and maxillary processes, due to proliferation of entrapped epithelium along the fusion line.4 Currently, the most widely accepted theory is that it originates from the inferior and anterior portion of the nasolacrimal duct.1,6–8 This theory is supported by the fact that the nasolacrimal duct is lined with pseudostratified columnar epithelium, which is found in the cavities of nasolabial cysts.5
Nasolabial cysts predominantly affect women (75% of cases) and arise most commonly in the fourth and fifth decades of life.4,5,8,9
Due to the peculiar presentation and location of these lesions, their diagnosis is almost exclusively clinical.9 The most common sign is enlargement causing facial asymmetry due to displacement of the upper lip, with elevation of the ala nasi and effacement of the nasolabial sulcus.5 Local pain, nasal obstruction, and concomitant infection—which can lead to abrupt enlargement of the lesion—may also be present.9
On periapical radiographs, nasolabial cysts may present as a radiolucent area in the apical region of the maxillary incisors.5,10 Standard occlusal views show posterior displacement of the radiopaque line corresponding to the bony margins of the anterior nasal aperture.6 When a more precise analysis of the borders of the lesion is required, computed tomography is the imaging modality of choice.11
The differential diagnosis includes periapical inflammatory lesions, nasal abscess, nasopalatine duct cyst, dermoid or epidermoid cyst, and salivary gland neoplasm. Pulp vitality testing of the adjacent teeth is useful, as a positive result will rule out periapical inflammatory lesions.1
The present report aims to describe the clinical presentation, diagnosis, and surgical treatment of nasolabial cyst by means of an illustrative case report.
Case reportThe patient described in this work has given informed consent.
A 47-year-old white woman presented to the outpatient Oral and Maxillofacial Surgery clinic of Universidade Federal de Pelotas (Pelotas, Brazil) for assessment of a left-sided mass in the region of the ala nasi (Fig. 1). The patient was unable to describe precisely how long the lesion had been present. The lesion was painless and there was no history of epistaxis or nasal discharge, although the patient reported partial obstruction of the left nasal cavity. Extraoral examination revealed facial asymmetry with slight elevation of the ala nasi and deformation of the left nasolabial sulcus. On palpation, the lesion was nodular, soft, fluctuant, circumscribed and did not extend beyond the soft tissues.
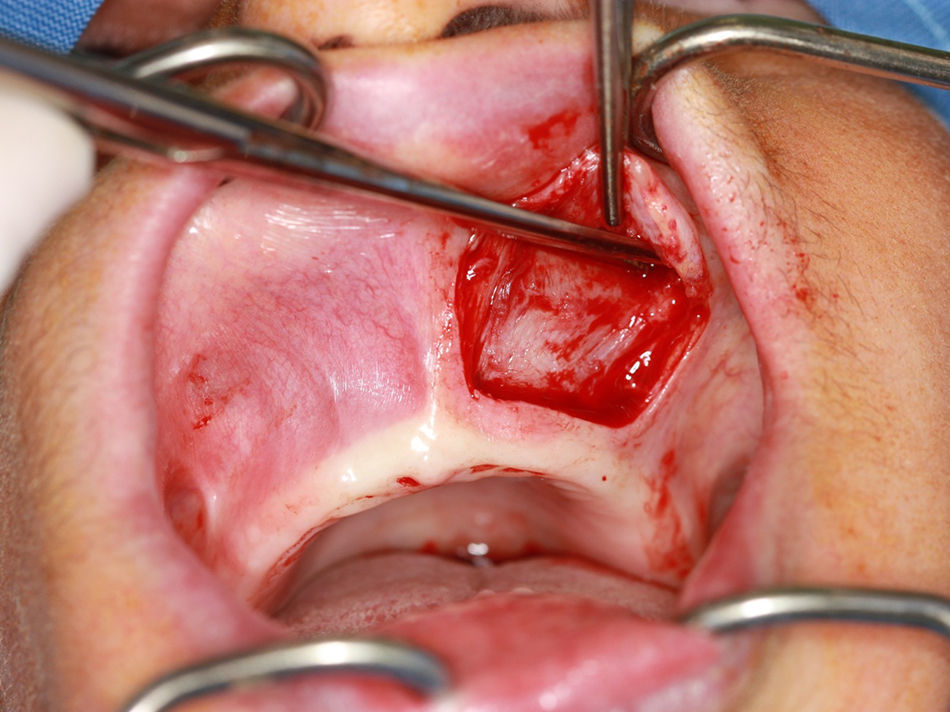
Intraoral examination revealed a fully edentulous maxillary arch and presence of a nodular lesion consistent with the extraoral findings, extending anteriorly toward the alveololabial groove (Fig. 2). The mass was rounded, swollen, and clearly circumscribed. The patient had no systemic comorbidities.
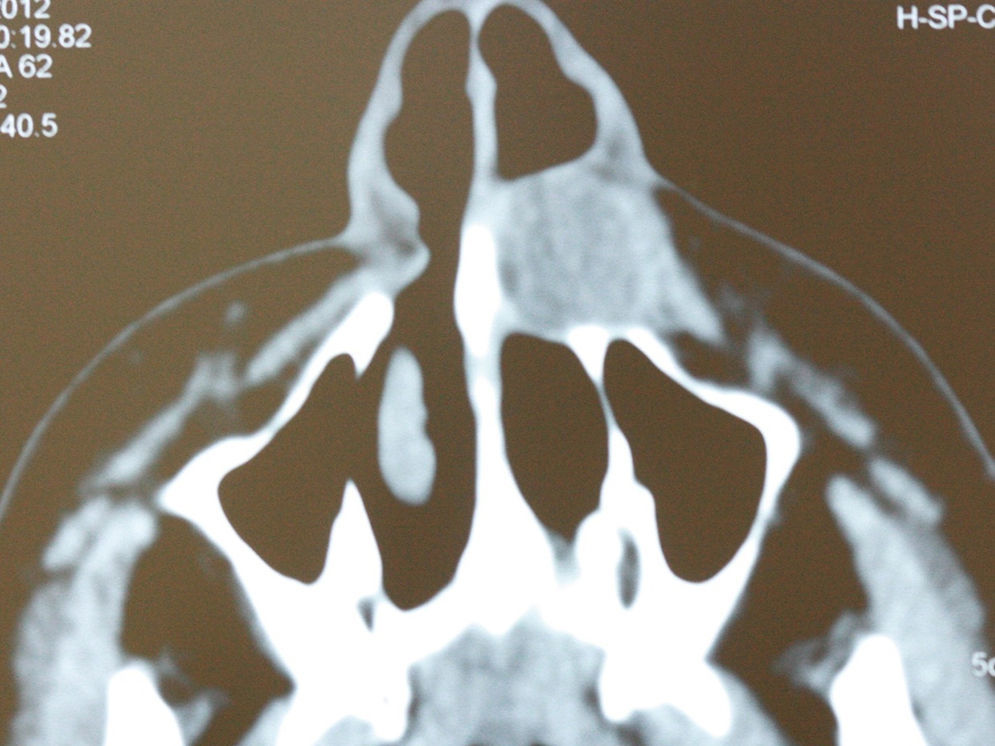
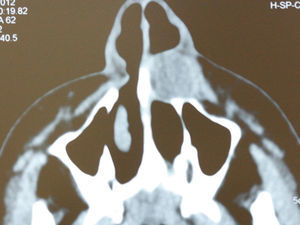
Computed tomography (CT) showed a cystic lesion in the lateral nasal region with a mean diameter of 20mm (Fig. 3).
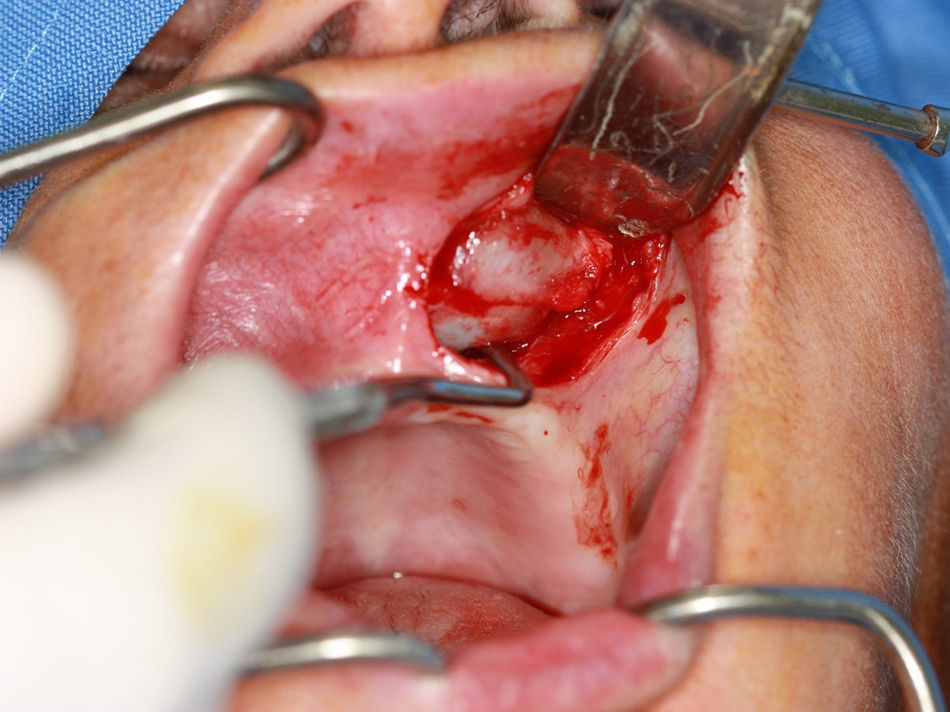
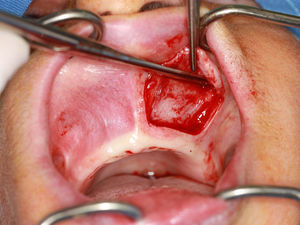
For the surgical approach, left-sided infraorbital and nasopalatine nerve blocks were performed, a flap was raised using Wassmund incision, the cyst capsule was dissected with the aid of Metzenbaum scissors (5mm Curved Slim Line Version, Quinelato, Brazil) and curettes (Lucas n.85, Quinelato, Brazil) (Figs. 4 and 5) and the lesion was excised.
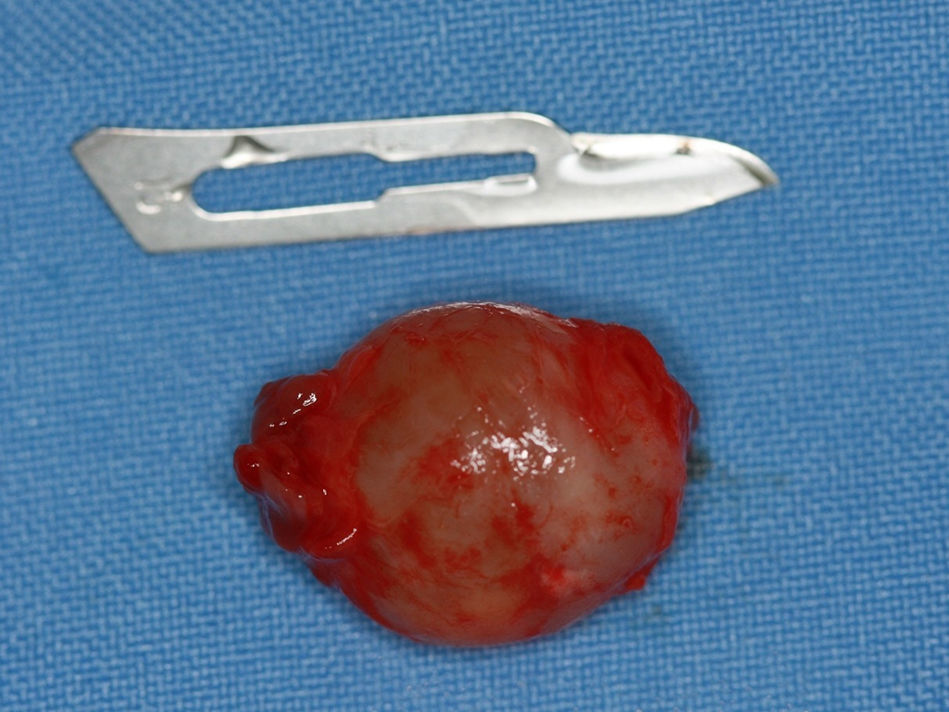
On gross examination, the lesion was covered by a reddish fibrous capsule and was approximately 20mm in diameter (Fig. 6).
The surgical wound was closed with simple interrupted sutures (4-0 nylon monofilament Ethicon, Somerville, NJ), which were removed on the 7th postoperative day (Fig. 7).
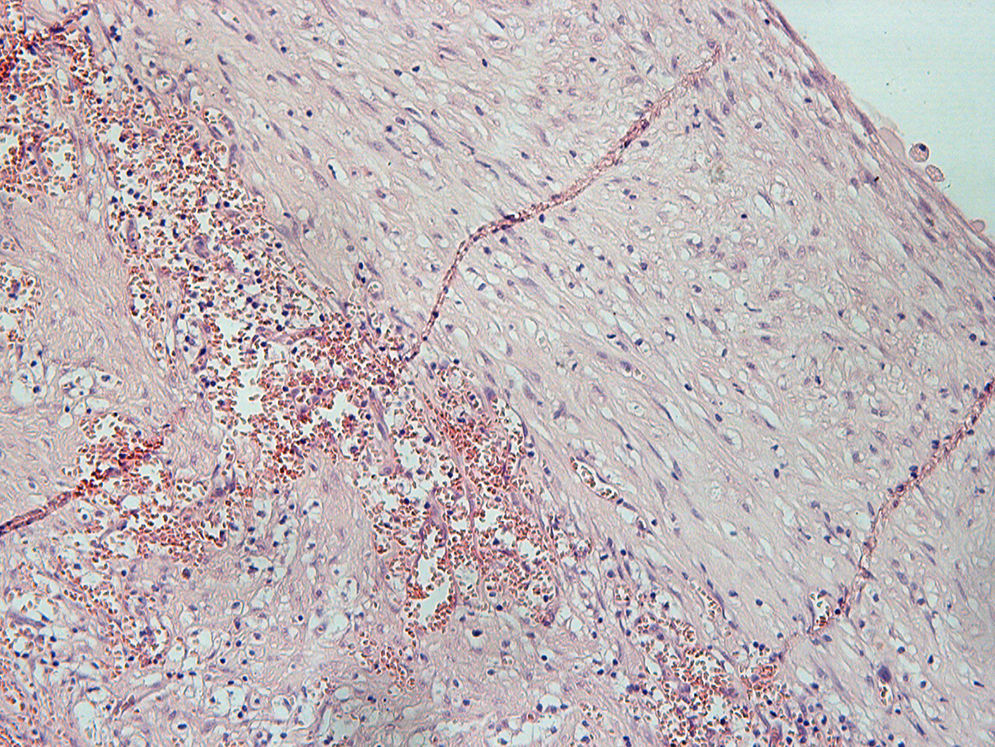
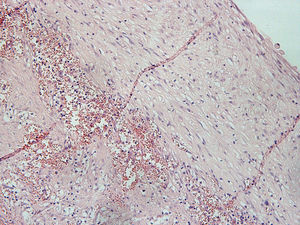
Histopathological analysis revealed a cystic lesion, mostly lined with a thin layer of stratified squamous epithelium, with a fibrous capsule and chronic inflammatory changes of varying intensity, consistent with a nasolabial cyst (Fig. 8).
The patient was prescribed paracetamol 1000mg for analgesia and had an uneventful postoperative course. There was no evidence of systemic infection then was not prescribed antibiotics. She remains well at 9-month follow-up (Fig. 9).
DiscussionThis case illustrates the most common features found in patients with nasolabial cysts, and corroborates the reports 4, 5. The clinical features described 9, 12 were observed in this case, particularly the most marked signs, such as effacement of the nasolabial sulcus and elevation of the ala nasi. Some patients with a nasolabial cyst may be asymptomatic, but most have at least one of the three cardinal symptoms: partial or complete nasal obstruction, well-circumscribed swelling (both seen in this patient) or localized pain.12,13
Except in the event of maxillary erosion, nasolabial cysts are undetectable on plain radiography, as they only contain soft tissue.9,10 Conversely, Seward11 described two possible radiographic aspects: increased radiolucency adjacent to the apical region of the incisors and deformity of the radiopaque line corresponding to the inferior border of the piriform aperture. According to Nixdorf et al.,1 occlusal views can aid the diagnosis by confirming the signs described by Seward,11 an assertion that runs counter to the opinions of authors who claim there are no radiographic signs of the nasolabial cyst.
The differential diagnosis of nasolabial cysts may include other lesions affecting the anterior maxillary region, such as odontogenic cysts and periapical abscesses and granulomas. Pulp vitality testing of the adjacent teeth is essential for proper diagnosis, as a coincidental lesion being absent, they will be vital in cases of nasolabial cyst. Dermoid and epidermoid cysts should also be considered in the differential, although they are associated with yellow discoloration of the overlying mucosa, whereas in nasolabial cysts, the mucosa conserves its normal pink hue or appears blue-tinged.1 Furthermore, dermoid and epidermoid cysts are usually diagnosed in childhood, while nasolabial cysts are more common in adult patients.14
CT scans usually reveal a homogeneous, cystic lesion, with no contrast uptake, anterior to the piriform aperture. Larger lesions may be associated with bone remodeling of the underlying maxilla.15 In the case reported herein, CT was performed due to the absence of radiographic findings and showed a well-delimited cystic lesion in the lateral nasal region.
Most studies have reported enucleation as the treatment of choice for nasolabial cysts.1,13 As they are entirely composed of soft tissues, nasolabial cysts are unresponsive to marsupialization.14 Alternative treatment modalities have been suggested, including aspiration, cauterization, injection of sclerosing agents, and incision and drainage; however, these methods are associated with high recurrence rates.16,17 Therefore, in view of the ease of surgical resection and its curative potential, we believe alternative methods should not be employed unless mandated by circumstance.
The aspiration of cyst content (to test for cholesterol crystals and rule out odontogenic lesions) and injection of radiopaque medium are unnecessary and increase the risk of infection substantially,9 although both procedures can distend the lesion and make it more easily detectable on clinical examination. As nasolabial cysts are usually in close proximity with the floor of the nasal cavity, perforation of the nasal mucosa during surgical excision is not unusual.13 Should this complication occur, the perforation should be closed with absorbable sutures so as to prevent development of oronasal fistula.4,9
Histopathological examination reveals ciliated pseudostratified columnar epithelium and, occasionally, stratified squamous epithelium.12 In a scanning electron microscopy study of the inner surface of nasolabial cysts, non-ciliated columnar epithelium with basal cells and goblet cells is found.12 In our patient, histopathology revealed a cystic lesion with signs of chronic inflammation, a fibrous capsule, a glossy and smooth inner surface, and yellow-tinged seromucous contents, confirming the diagnosis of nasolabial cyst.
ConclusionBased on the literature and the present case report, we conclude that, despite the low frequency of nasolabial cysts, it is essential that dental practitioners be able to recognize the key features of these lesions so as to be able to distinguish them from lesions of odontogenic origin and thus enable safe and proper treatment planning. Such key features may be difficult to detect because patients may be asymptomatic, but most exhibit well-circumscribed swelling, localized pain, and partial or complete nasal obstruction on the affected side. Therefore, a diagnostic hypothesis of nasolabial cyst should be backed up by clinical examination and imaging; computed tomography (CT) scanning may be required; and histopathology is necessary to confirm the diagnosis. After the diagnosis of nasolabial cyst is established, the optimal treatment modality consists of complete excision of the lesion, showing good prognosis and rare cases of recurrence.
Ethical disclosuresProtection of human and animal subjectsThe authors declare that the procedures followed were in accordance with the regulations of the responsible Clinical Research Ethics Committee and in accordance with those of the World Medical Association and the Helsinki Declaration.
Confidentiality of dataThe authors declare that they have followed the protocols of their work center on the publication of patient data and that all the patients included in the study have received sufficient information and have given their informed consent in writing to participate in that study.
Right to privacy and informed consentThe authors must have obtained the informed consent of the patients and/or subjects mentioned in the article. The author for correspondence must be in possession of this document.
This study was supported by the Universidade Federal de Pelotas, RS, Brazil.