Central odontogenic fibroma is a benign odontogenic tumor derived from the dental ectomesenchymal tissues. It is a rare lesion that could be seen in all age‐groups and that it is found both in the mandible and in the maxilla.
A 24‐year‐old caucasian male patient was referred, reporting a pressure on the left side of the upper jaw. There were no other symptoms and no recent history of pain. The clinical examination did not reveal buccal or palatal expansion. The left maxillary second premolar was mobile. Radiographic evaluation showed the presence of a unilocular radiolucent well‐defined area around the roots of the maxillary left canine, first and second premolars. Root canal treatment was carried out in teeth 23, 24 and 25. The lesion was surgically removed under general anesthesia. The histopathological diagnosis confirmed central odontogenic fibroma. The patient showed no clinical or radiographic signs of recurrence one year after surgical excision.
O fibroma odontogénico central é um tumor odontogénico benigno que deriva do ectomesênquima dentário. É uma patologia rara que atinge várias faixas etárias e que tanto pode afetar a mandíbula como a maxila.
Um indivíduo de 24 anos, raça caucasina, veio à consulta de medicina dentária apresentando uma sensação de pressão no lado esquerdo da maxila. Para além deste aspeto o paciente não referia mais sintomatologia. Ao exame clínico foi possível verificar a ausência de abaulamento das corticais ósseas. O dente 25 apresentava mobilidade. Após realização de exame radiográfico verificou‐se a presença de uma lesão unilocular radiotranslúcida, com contornos bem definidos, na proximidade das raízes dos dentes 23, 24 e 25. Efetuou‐se a exérese cirúrgica da lesão, sob o efeito de anestesia geral. O exame anatomo‐patológico confirmou o diagnóstico de fibroma odontogénico central. O paciente não apresenta sinais clínicos ou radiográficos de recidiva após um ano da remoção da lesão.
Central odontogenic fibroma (COF) is an extremely rare benign tumor accounting for only 0.1% of all odontogenic tumors.1 This lesion is considered to be derived from ectomesenchymal tissue of dental origin such as periodontal ligament, dental papilla, or dental follicle.2 Histologically, this lesion is characterized by the presence of colagenous fibrous connective tissue containing varying amounts of odontogenic epithelium. Clinically, it presents as a slow growth asymptomatic mass which, in most cases, can remain unknown until the appearance of a swelling. In more severe cases root resorption and displacement of adjacent teeth have been reported.3 COF appears in both the mandible and maxilla (55% and 45% respectively). In the maxilla it has a tendency to involve the anterior area whereas in the mandible the molar and premolar areas are the most prevalent sites.2,4 It is reported to occur in a wide age group with a female predilection.5,6 Most COFs present as a radiolucent unilocular lesion with well‐defined contours that can simulate lesions of endodontic origin. However they may also appear as multilocular lesions and in rare instances may exhibit a mixed radiolucent/radiopaque appearance with poorly defined or diffused borders.2 Enucleation or surgical curettage is the appropriate therapy and recurrence is low.7
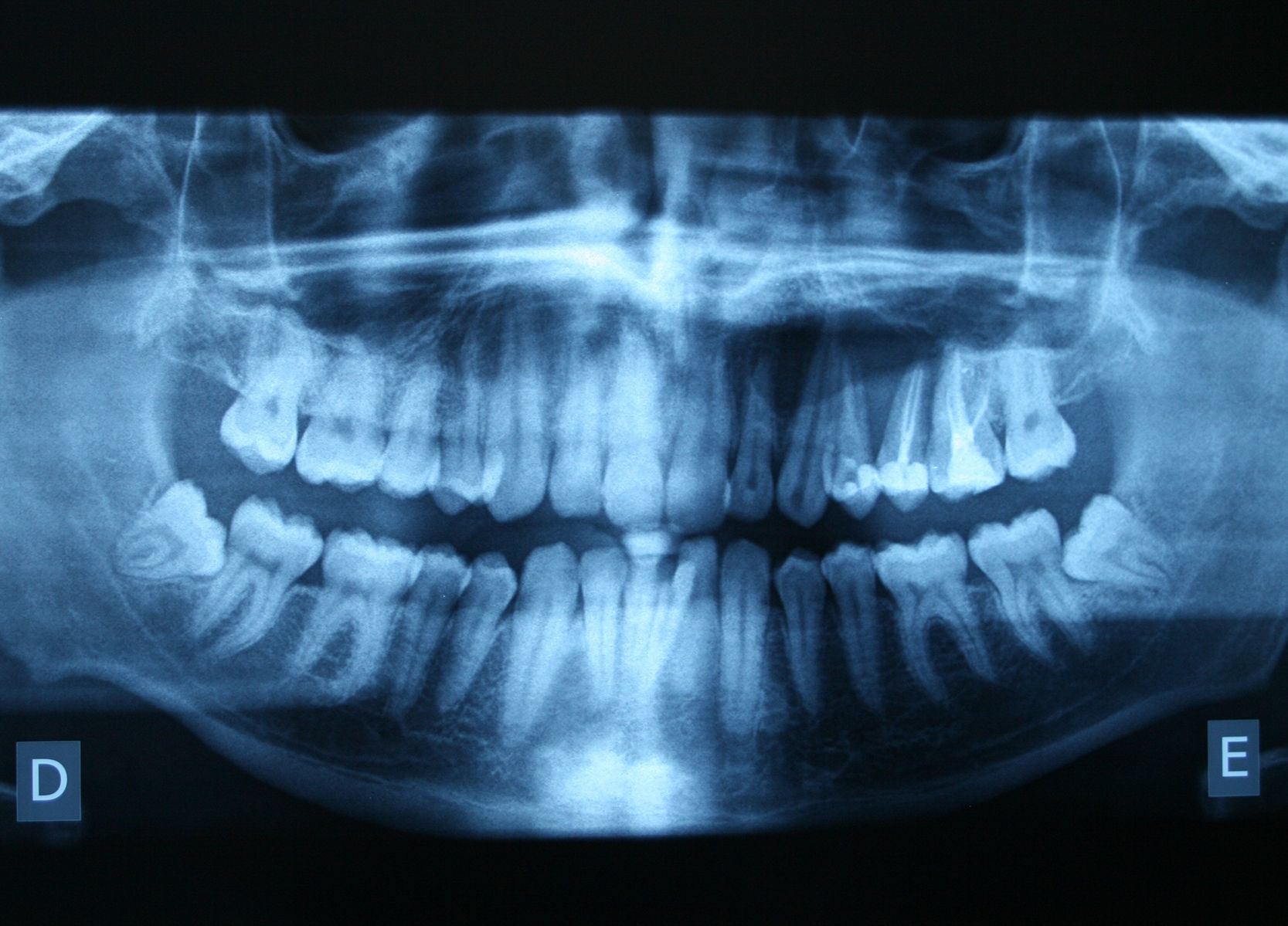
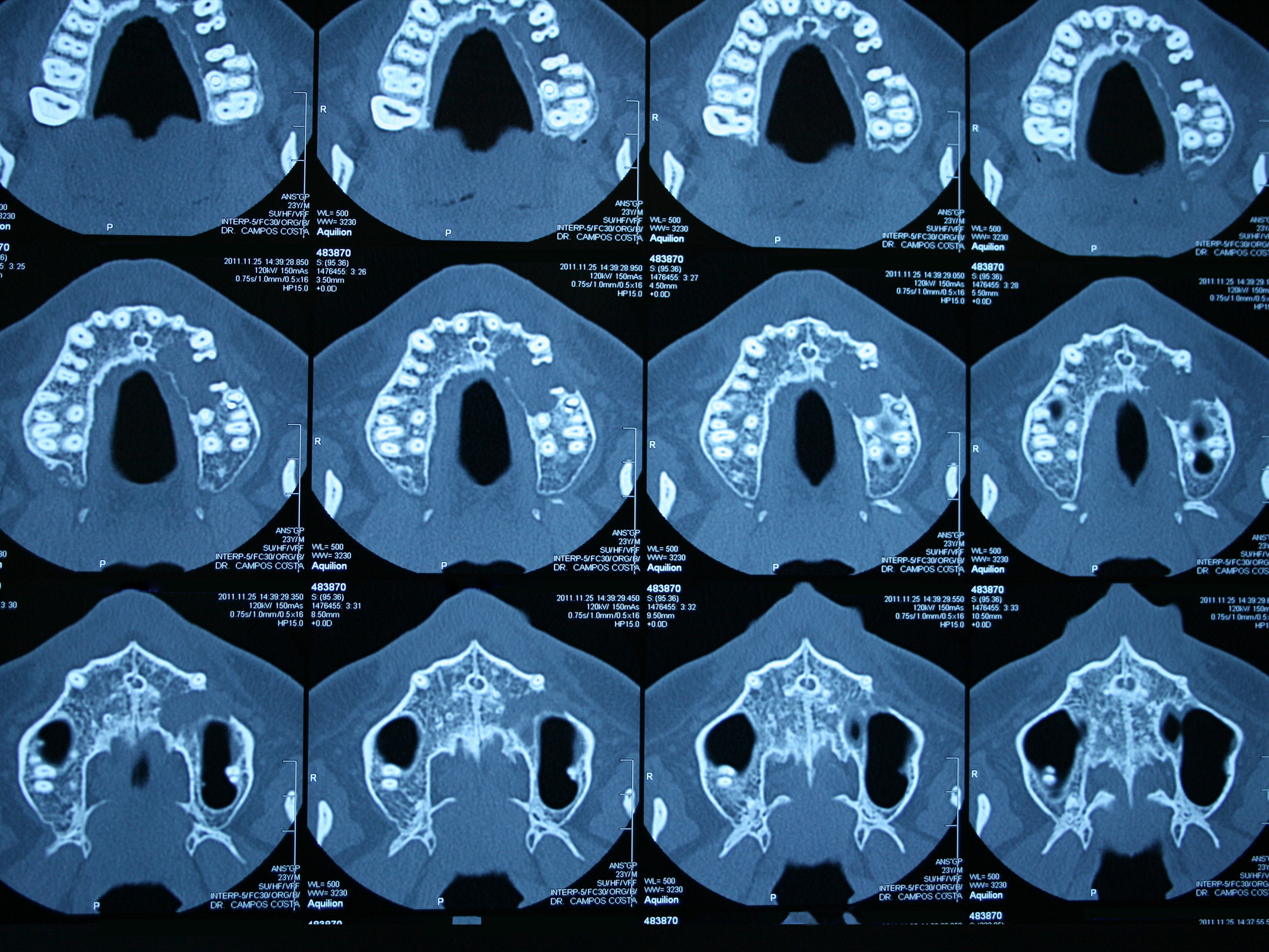
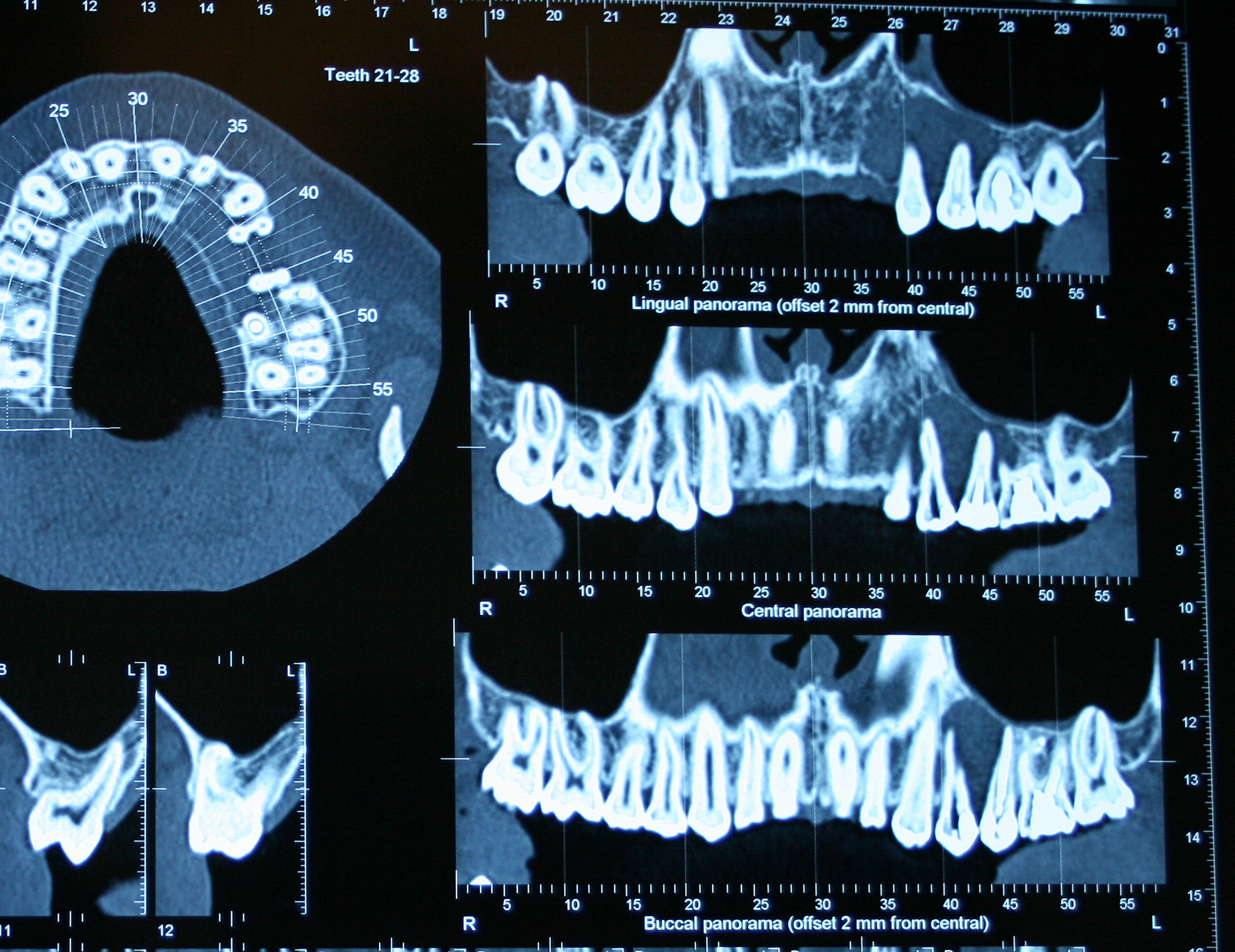
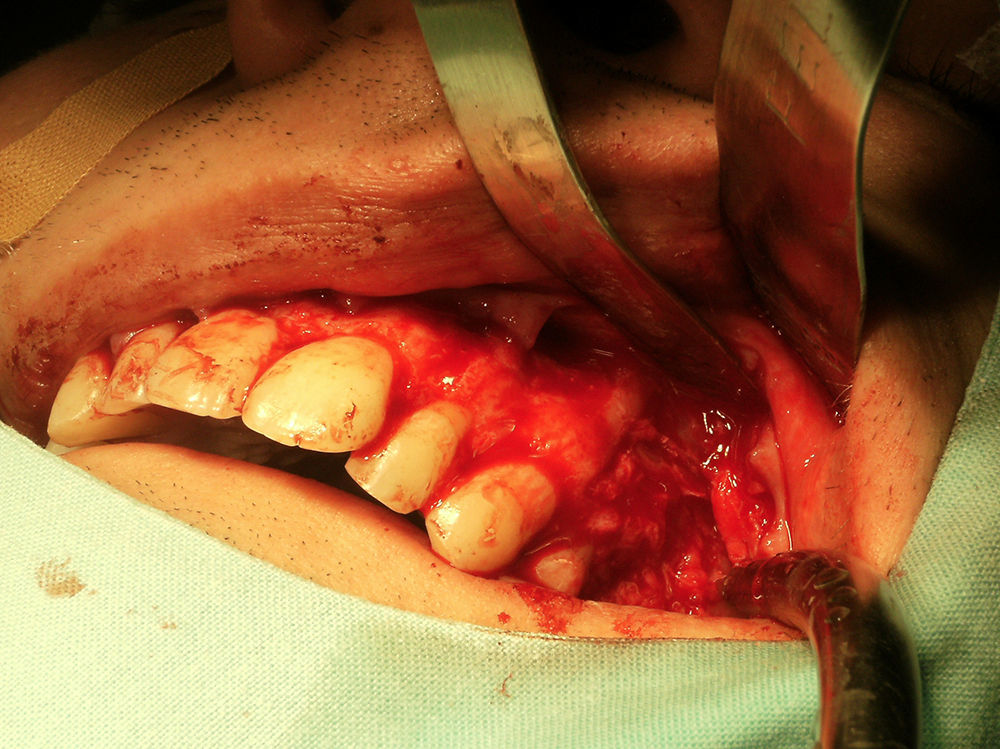
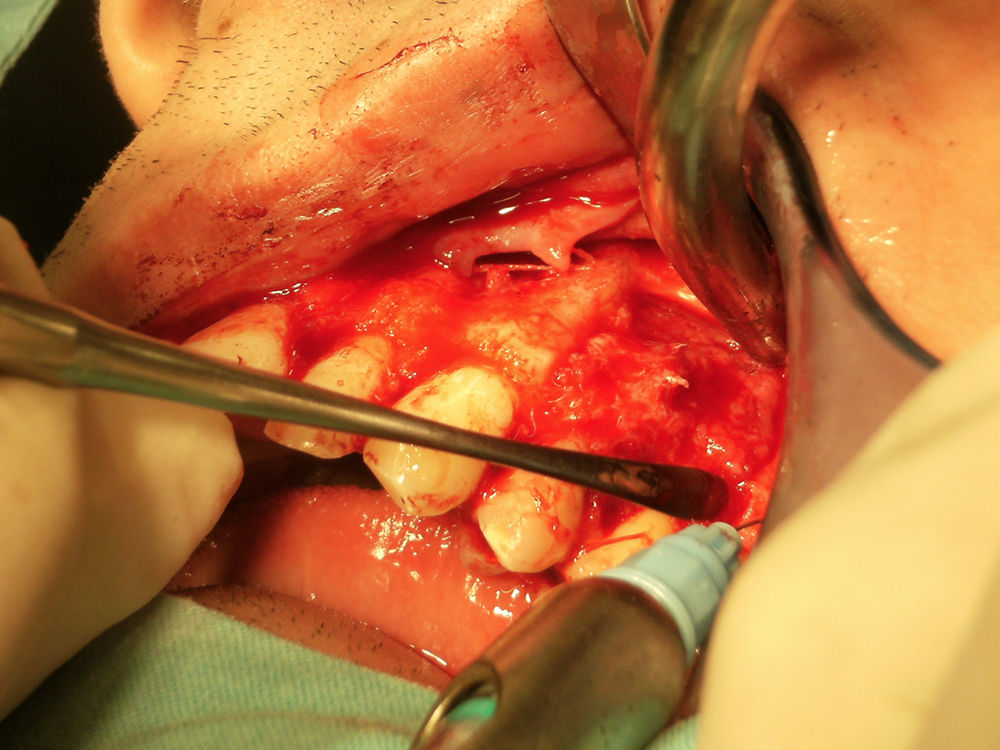
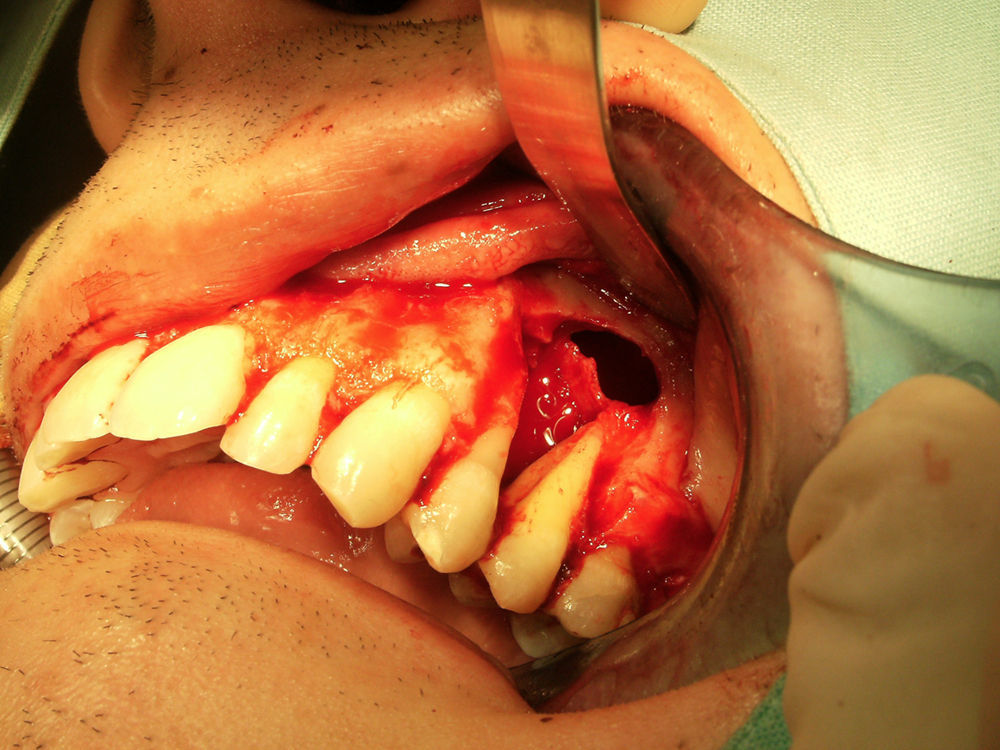
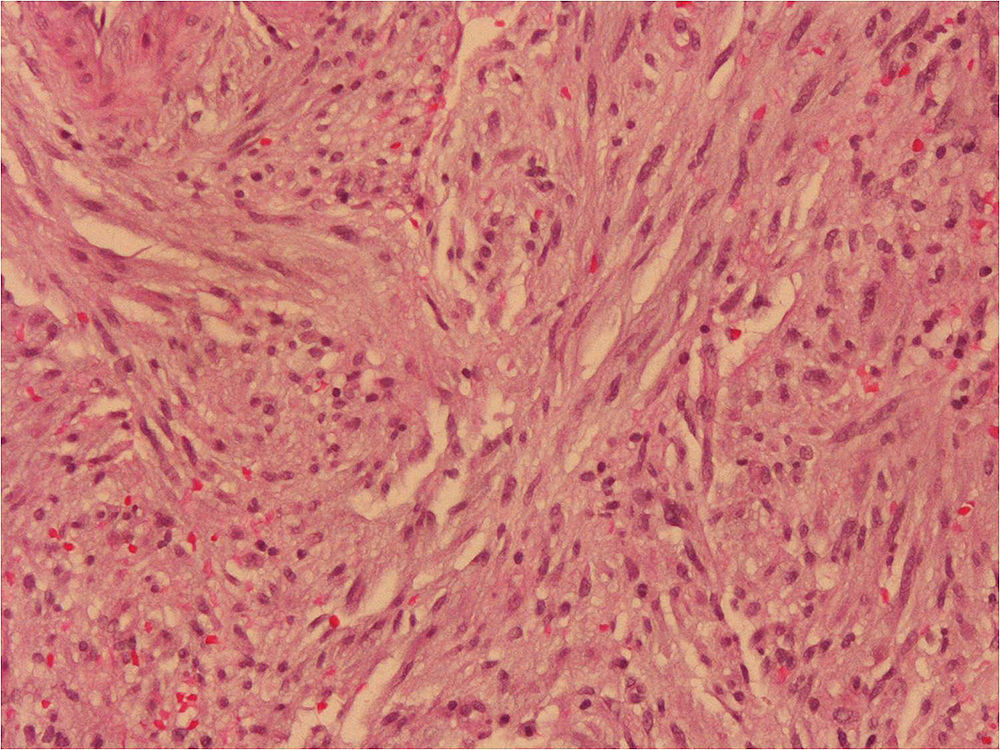
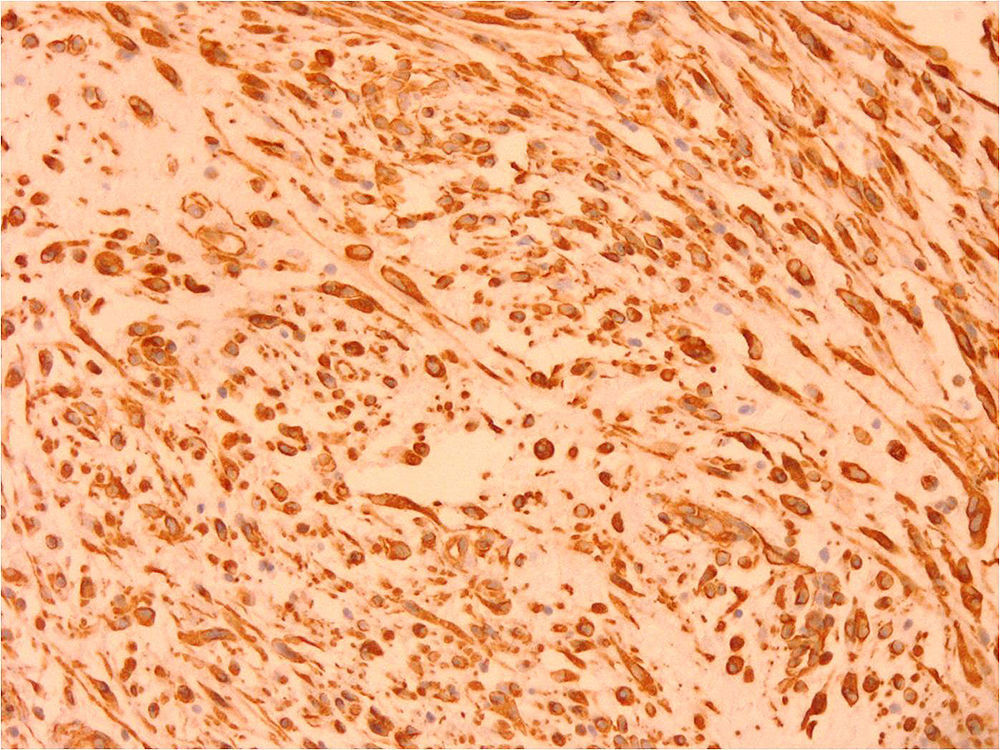
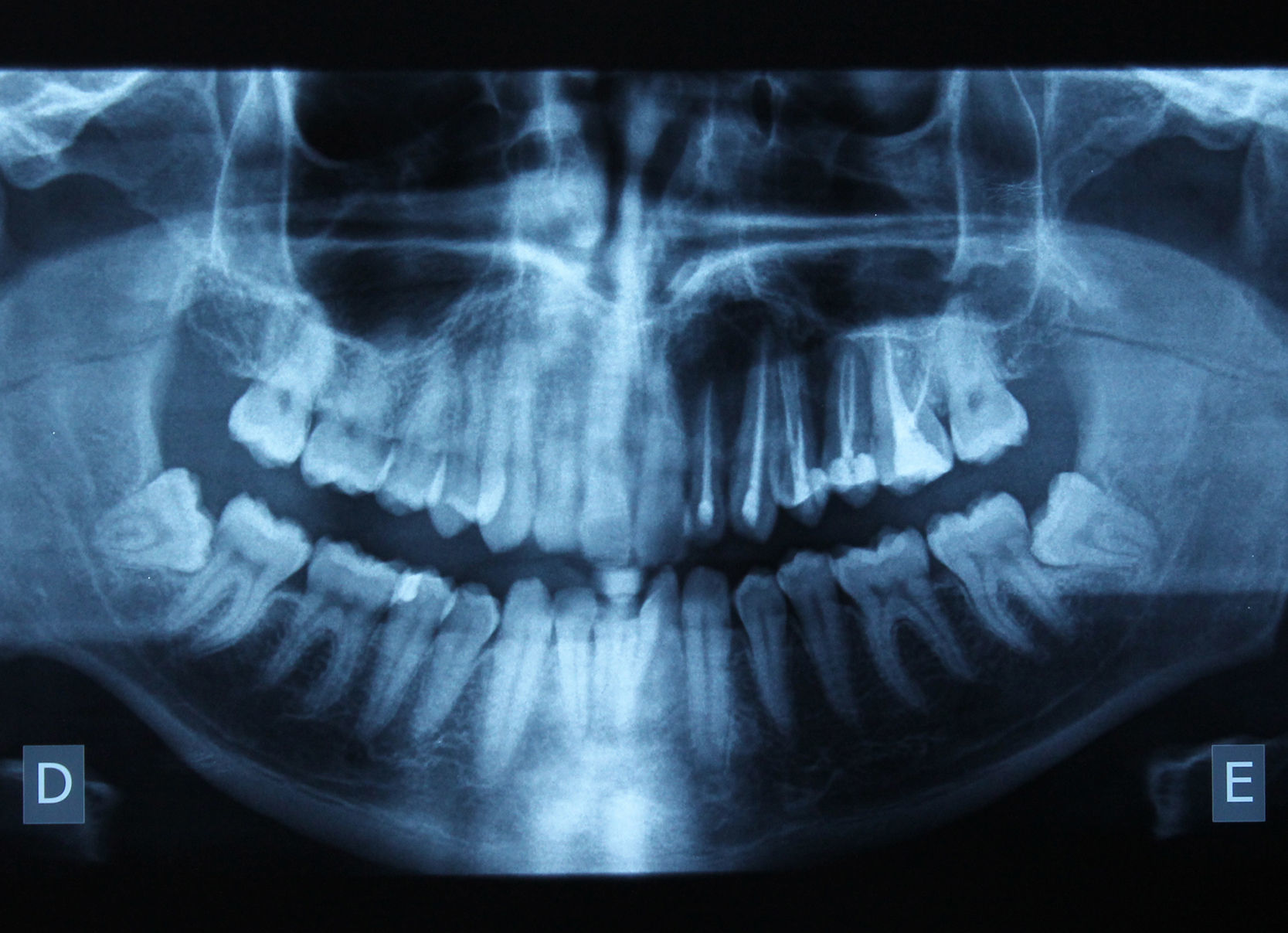
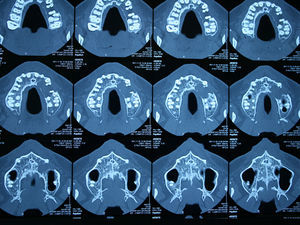
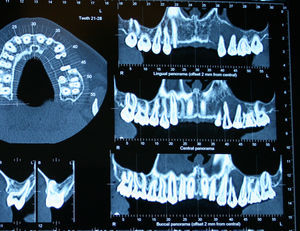
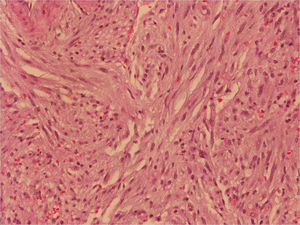
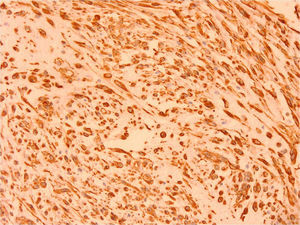
Case reportA 24‐year‐old caucasian male patient attended our dental medicine appointment referring a pressure on the left side of the maxilla. Besides this the patient reported no other symptoms. On the clinical examination we found tooth 25 with mobility. A panoramic radiograph (Fig. 1) was obtained, which revealed the presence of a large radiolucent lesion near the roots of teeth 23, 24 and 25. The patient was asked to take a computerized axial tomography in order to assess the size of the lesion and its relationship with the surrounding anatomical structures (Figs. 2 and 3). The tomography showed a very large lesion that has already induced a great reabsorption of the labial plate and the floor of the maxillary sinus. It was proceeded the root canal treatment of the referred teeth and the lesion was surgically removed. Under general anesthesia, an excisional biopsy was performed. A bucal mucoperiosteal flap was raised and the lesion and the cortical bone that surrounded it were exposed. After removing the cortical plate, the soft lesion was enucleated from the bone. The surgical specimen was fixed in 10% neutral formalin and submitted to histopathological examination (Figs. 4–6). Gross examination revealed a friable russet mass, measuring 2.1cm×1.9cm×0.8cm. The histopathological examination (Fig. 7) revealed a tumor composed of a collagenous stroma rich in spindle shaped fibroblasts without cellular atypia. Few nests of odontogenic epithelium were found. No hard tissue such as bone or cementum‐like material was observed. A low mitotic activity and mononuclear inflammatory cells could be found. An immunocytochemical analysis was performed to search the presence of vimentin (Fig. 8). The expression of this protein was observed in spindle cells. Correlation of clinical, radiographic and histopathological features lead to a definitive diagnosis of central odontogenic fibroma, epithelium‐poor type. Eighteen months after surgery a radiographic control (Fig. 9) was made and it was found that trabecular bone became denser which demonstrates that normal regeneration of the bone lost by the pressure exerted by the fibroma was occurring.
Discussion and conclusionsCentral Odontogenic Fibroma is described in the literature as a benign neoplasm usually diagnosed on the second and third decade of life which is in accordance with our patient.8,9 Most authors describe this lesion as being more common in females8,10 despite in our case it has occurred in a male.1,10 This matches up with the studies of Buchner et al.11 In 2004, Daniels et al.,1 in a review of the literature, shows a ratio of incidence on the mandible and maxilla of 1:1 with a 70% female‐occurrence (49 of 70). On the mandible 26 of 35 cases occurred mainly at the posterior region, and on the maxilla 26 out of 35 of the cases occurred at the anterior region. It was found to occur between the ages 4 and 80 years. On a retrospective study of 8 clinical cases of COF, Hrichi et al.12 found a predilection for male sex (1.67:1) and the most common location of the tumor was on the mandible. The average age was 19.9 years with an age range of 11–38 years. Our case is very similar to that described by Sakamoto et al.13 concerning the age and sex of the patient and the location of the lesion (near teeth 23, 24 and 25).
According to Gardner,14 there are two types of COF:
Fibrous neoplasm or simple type with collagenous fibrous connective tissue containing odontogenic epithelium;
WHO type which apart from the above features, also shows presence of dysplastic dentin or cementum like tissue;
Radiologically, the majority of central odontogenic fibromas are radiolucent. It is originally thought that most of these lesions have multilocular radiolucencies, but the current reports show that there are more unilocular than multilocular radiolucencies. The small lesions are unilocular while the larger ones tend to be multilocular or to have scalloped margins. In some cases, due to the location near the teeth roots, this tumor can mimic anendodontic origin lesion.15 Periapical radiolucencies of nonendodontic origin occur infrequently. When they do occur, however, a proper diagnosis must be made. Dental professionals must not become complacent on the diagnosis of periapical pathoses, but must be aware of other etiologies. The COF is one such example. Although it has been rarely reported, it must be considered on differential diagnosis for a radiolucency associated with the roots of vital and non vital teeth. Covani et al.2 presented a case of COF associated with the root of an erupted tooth. The authors argue the importance of making a correct differential diagnosis of COF with endodontic lesions showing the same radiological lucent image. The diagnosis of the COF is determined by its histology. In our case the lesion was associated with the roots of three teeth and the provisional diagnosis had been a lesion of endodontic origin. After surgical removal the histologic examination revealed the real diagnosis – COF.
COF is believed to arise from the odontogenic ectomesenchyme. Being a mixed tumor, this lesion can be confused with desmoplastic fibroma (absence of odontogenic epithelial rests), ameloblastic fibroma (if odontogenic islands are large and numerous) or myxofibromas (collagen fibers along with stellate/spindle cells).4,16 COF radiographic presentation can be very similar to a dentigerous cyst‐like lesion, which suggests that COF should be included in the differential diagnosis of pericoronal lesions on the posterior mandible.1
As COF is considered a benign odontogenic tumor the treatment of choice is enucleation with careful follow up for a few years, although few cases of recurrence have been reported.17–19 Dunlap and Barker20 presented two cases of maxillary odontogenic fibroma treated by curettage with a follow‐up of 9 and 10 years with no evidence of recurrence. Also none of the 8 cases reported by Hrichi et al.12 showed recurrence on a follow up of 2 years after surgery.
Despite being an extremely rare tumor it is very important that dentists be aware of its clinical, radiographic and histological features in order to include it on the differential diagnosis of odontogenic tumors.
Ethical disclosuresProtection of human and animal subjectsThe authors declare that no experiments were performed on humans or animals for this investigation.
Confidentiality of dataThe authors declare that they have followed the protocols of their work center on the publication of patient data and that all the patients included in the study have received sufficient information and have given their informed consent in writing to participate in that study.
Right to privacy and informed consentThe authors must have obtained the informed consent of the patients and/or subjects mentioned in the article. The author for correspondence must be in possession of this document.