Erectile dysfunction (ED) inquiry and treatment could have an important role in cardiovascular prevention. The aims of the present study were to: (1) evaluate the association of ED with cardiovascular risk (CVR) factors among patients with no previous cardiovascular events; (2) assess the inquiry of ED in Portuguese primary care.
MethodsCross-sectional study (January–March 2011) conducted in two Lisbon Primary Healthcare Centers among men aged 18–80 years, sexually active and with no cardiac or cerebrovascular disease. We collected data concerning CVR factors and sexual health inquiry through interviews and clinical records and we used the International Index of Erectile Function to evaluate ED. Logistic regression models were used to study the association between ED and CVR factors.
ResultsIn a sample of 90 men (mean age 49.82±15.65), 32% had ED. Hypertension prevalence and the number of CVR factors was significantly higher among men with ED. However, age was strongly associated with ED and, after age-adjustment, the associations found between ED and hypertension lost their statistical significance. The majority of men evaluated their sexual life as “very important” or “important” (98%) and affirmed that sexual problems should be inquired by the general practitioner (93%) but only a minority were inquired about it (14%).
ConclusionED is a frequent problem among men with no previous cardiovascular events and, in our study, it was mostly associated with age. ED is still not inquired appropriately in the primary care.
A abordagem e o tratamento da disfunção erétil (DE) nos cuidados de saúde primários poderiam ter um papel importante na prevenção cardiovascular. Os objetivos deste estudo foram: 1) estudar a relação da DE com os fatores de risco cardiovasculares (FRCV) em indivíduos sem eventos cardiovasculares prévios; 2) avaliar a abordagem da DE nos cuidados de saúde primários portugueses.
MétodosEstudo transversal, exploratório, realizado em 2 centros de saúde de Lisboa, incluindo homens com 18–80 anos de idade sexualmente ativos e sem doença cardíaca ou cerebrovascular. Recolhemos dados relativos à abordagem da DE e dos FRCV através de entrevistas e da consulta de processos clínicos. Avaliámos a DE através do Índice Internacional de Função Eréctil e a associação com os FRCV através de modelos de regressão logística.
ResultadosNuma amostra de 90 homens (média de idade 49,82±15,65), 32% apresentavam DE. A prevalência de hipertensão e o número de FRCV foi significativamente superior em homens com DE. Contudo, a idade esteve significativamente associada à DE e, após ajuste para a idade, a associação encontrada entre a hipertensão e a DE deixou de ser significativa. Apesar de a maioria ter reportado que os problemas sexuais deviam ser abordados pelo médico de família (93%), apenas uma minoria afirmou já ter sido inquirida a este respeito (14%).
ConclusãoA DE é um problema frequente em homens sem eventos cardiovasculares prévios e, no nosso estudo, associou-se sobretudo à idade. A DE não é suficientemente abordada nos cuidados de saúde primários portugueses.
There has been a growing interest in sexual health research as the diagnosis of a sexual dysfunction may provide an opportunity to learn about other health conditions as well as to alleviate the dysfunction.1 The clearest example is erectile dysfunction (ED): it may result from psychological, neurological, hormonal, arterial or cavernosal impairment or from a combination of these factors.2,3 It is currently proposed that ED be defined as a failure to obtain and maintain an erection sufficient for sexual activity or decreased erectile turgidity on 75% of sexual occasions and lasting for at least 6 months, independently of distress.4 Evidence suggests that ED prevalence increases with age: low in men under the aged 40–49 years (median prevalence 6%; range 1–29%); modest in men aged 50–59 years, (median prevalence 16%; range 3–50%); higher in men aged 60–69 years (median prevalence 32%; range 7–74%), and much higher in men aged 70–79 years (median prevalence 44%; range 26–76%).5 ED is highly prevalent in individuals with multiple cardiovascular risk (CVR) factors and/or with cardiovascular disease. In fact, ED is associated with increased risk of cardiovascular events and all-cause mortality.6–9 The onset of ED occurs 2–3 years before symptomatic coronary heart disease and 3–5 years before cardiovascular events.10–13 This makes inquiry about ED in the primary care a useful tool to identify at-risk patients with cardiovascular disease that may not yet have become manifest by other symptoms or signs. ED may even be the first recognized evidence of the presence of CVR factors. Therefore, it is now recommended to sexual inquiry all men.14 Of note, a validated questionnaire, such as the International Index of Erectile Function (IIEF), has been recommended to assess ED instead of a subjective inquiry. Indeed, a systematic review and meta-analysis of cohort studies has shown that patients in whom ED was diagnosed with a questionnaire, the relative risk for total cardiovascular events was higher compared with that in patients in whom ED was diagnosed with a single question.8 Thus, it seems reasonable that ED when correctly evaluated could provide more useful information about the future cardiovascular risk. However, several studies indicate that ED is not inquired appropriately in the primary care.1,15–18 Since sexual health inquiry and support has been defined as a primary care priority and could have an important role in cardiovascular prevention,1 the field is still in need of more studies to evaluate the rate of ED inquiry among male patients with no previous history of cardiovascular events as well as to explore the association of ED with CVR factors in these patients.
This cross-sectional study aims to: (i) explore the association of ED with CVR factors among male patients with no previous history of cardiovascular events; (ii) assess the general practitioner's ED inquiry rate and patient's expectations regarding sexual health discussion in the primary care.
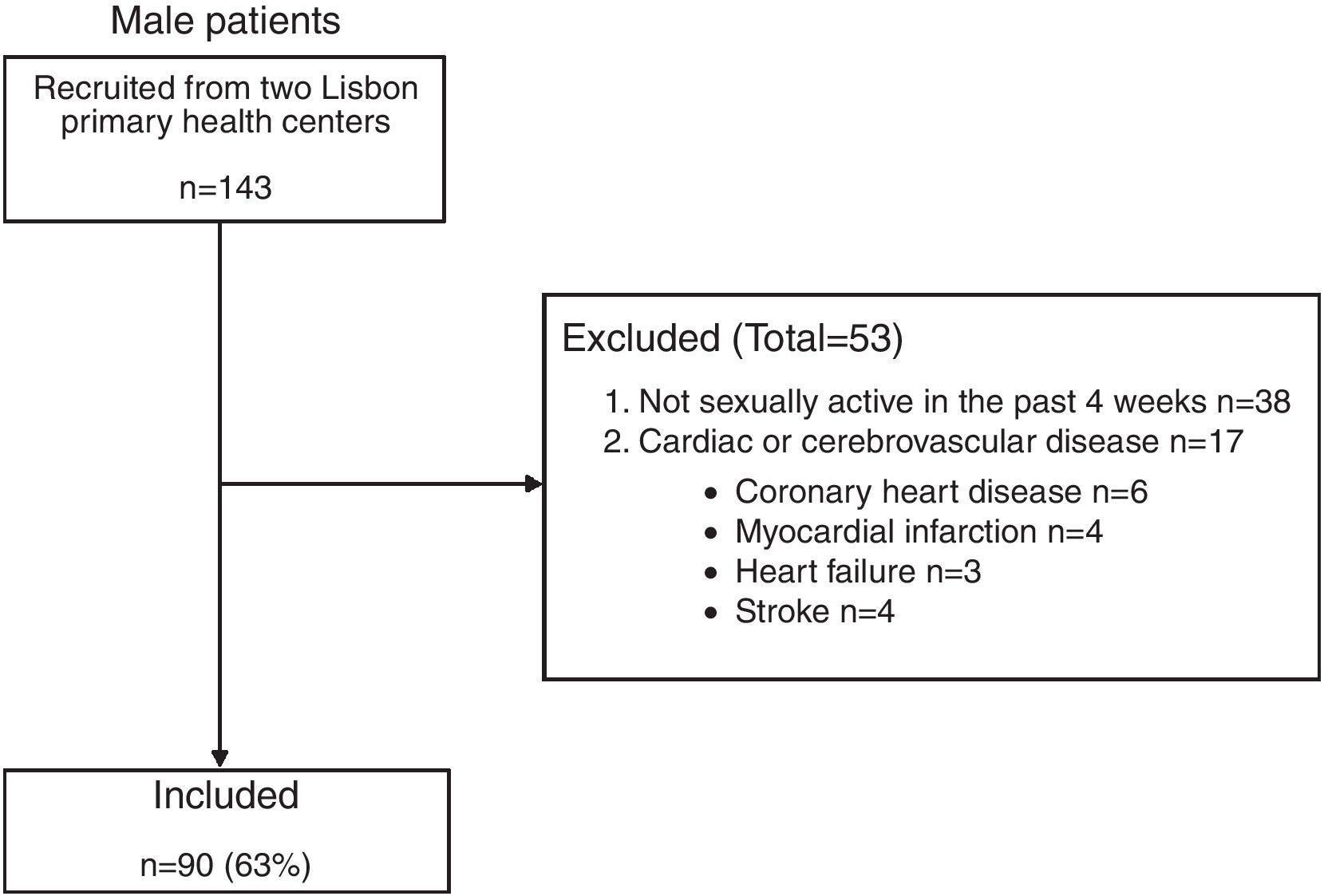
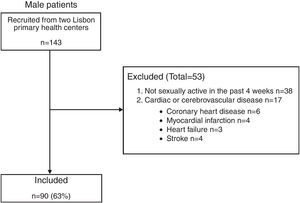
MethodsSample and procedureThis study is part of the Sexual Observational Study in Portugal.15 After obtaining the authorizations from the Ethic Committee of the Lisbon Faculty of Medicine and from the Lisbon and Tagus Valley Regional Health Administration, and the permission from the Portuguese Protection Data Authority, two Lisbon Primary Healthcare Centers (Agrupamento de Centros de Saúde de Odivelas) were solicited to collaborate. All eligible male subjects who had an appointment or presented at these Primary Health Centers between January and March of 2011 were recruited. Inclusion criteria were: (i) aged 18–80 years with no previous history of cardiovascular events; (ii) having a clinical record; (iii) being sexually active in the past 4 weeks – defined as sexual intercourse and/or any type of sexual stimulation. The exclusion criteria were: (i) symptomatic cardiovascular disease or history of previous cardiovascular events (coronary heart disease, heart failure, prior myocardial infarction and stroke); (ii) sexually inactivity in the past four weeks – as the questionnaire used to evaluate ED is validated to assess sexual function only in the past four weeks; (iii) institutionalized subjects; (iv) subjects with marked cognitive impairments that could interfere with the understanding of the questionnaires used; (v) participating in another study, including a treatment intervention (sildenafil, tadalafil and vardenafil) that could interfere with the patient's sexual function. Each participant was interviewed using a standardized questionnaire concerning socio-demographic variables, sexual health inquiry, CVR factors and completed a specific self-administered questionnaire to assess sexual function. Trained male interviewers collected the data. Afterwards, medical records were consulted to seek for missing information concerning patient's general health status, medications and CVR factors. Informed consent was obtained and confidentiality was assured.
Main outcome measuresSociodemographic and sexual health inquirySociodemographic data included age, nationality, ethnicity, religion, marital status, educational level and profession. Sexual health inquiry data included: (i) “Do you think that sexual problems should be inquired by the general practitioner?”; (ii) “Did your general practitioner already questioned you about sexual problems?”; (iii) “Did you already discuss sexual problems with your general practitioner by your own initiative?”; (iv) “What's the importance of sex for your quality of life?” with the following possible answers: “Very Important”, “Important”, “Not much” and “Not at all”. The answers “Not much” and “Not at all” were grouped afterward in a single category: “Not much/Not at all”.
Cardiovascular risk factorsTwo groups of CVR factors were included: biological and lifestyle related factors. The biological CVR factors included were: hypertension, diabetes mellitus, hyperlipidemia and obesity. The diagnostic criteria used were: self-reported, clinically recorded or inferred through typical medications prescribed and recorded in their clinical record. For obesity, body mass index (BMI) was calculated: participants were considered obese if their BMI was ≥30kg/m2. The lifestyle related CVR factors included were: cigarette smoking habits, alcohol overuse, and physical inactivity. Based on their smoking habits, the participants were categorized as current smokers or non-smokers. Former smokers were considered as non-smokers. Alcohol overuse was defined as consumption of an average of 20 or more grams of ethanol per day. Practices of binge drinking at least one day of the week, determined by the consumption of 40 or more grams of ethanol per day of one of the type of drinks, was also considered alcohol overuse. Physical inactivity was considered with less than 1h of vigorous activity per week, 2.5h of moderate activity per week or 3.5h of walking per week, as well as if the sum of hours doing these three types of physical activity was less than 3.5h per week.19 For each participant an index with the number of the aforementioned CVR factors was calculated according to a previous study with similar aims.20
Erectile dysfunctionED was evaluated using the International Index of Erectile Function (IIEF), a 15-item questionnaire developed and validated as a brief and reliable self-administered scale for accessing erectile function.21,22 The erectile function domain has a range of scores from 6 to 30 and discriminates between men with and without ED among those who reported having had sexual intercourse and activity during the previous 4 weeks. ED was diagnosed by a score of ≤25.23
Statistical analysisQuantitative data were expressed as mean±standard deviation (SD) while qualitative data were expressed through absolute (n) and relative (%) frequencies. Student's t-test was used to test significance of difference for quantitative variables. Non-parametric Mann Whitney test was used when neither the data normality assumption for each group nor the homogeneity of variances assumption were verified. Chi-square test was used to test significance of difference for qualitative variables. Fisher's exact test was used when chi-square test was not applicable. Chi-square test for trends was used for ordinal variables. Categories with low frequencies were excluded from the analyses. To study the strength of association between sexual dysfunctions and CVR factors, logistic regression models were used: Odds ratios (OR) and age-adjusted OR were estimated, as well as their 95% Confidence Intervals (95% CI).
Significance level for all statistical tests was 5%. The statistical analysis software used was SPSS Statistics V21.
ResultsStudy populationA total of 143 male participants were recruited. Of these, only 63% (n=90) were found to be eligible and were included in the analysis. For more detailed information regarding excluded participants, e.g., patients-specific details and reasons for excluding, see Fig. 1.
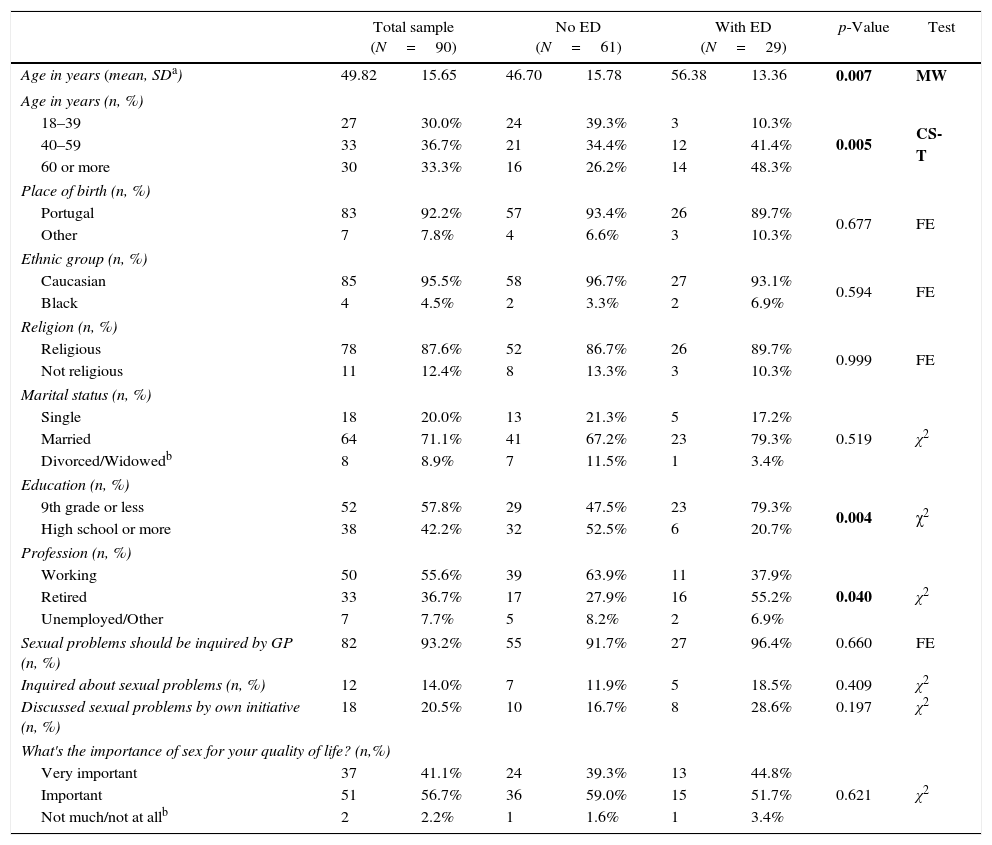
Erectile dysfunctionFrom the sample of 90 eligible men (mean age 49.82±15.65; mean IIEF score 25.02±5.30), 32% had ED (n=29). The socio-demographic variables are presented in Table 1. Men with ED were older compared to men without ED (mean age 56.38±13.36 vs. 46.70±15.78; p=0.007), had a lower educational level (p=0.004) and were more professionally inactive (p=0.040). Concerning sexual health inquiry, there were no significant differences between the two groups. The majority stated that sexual problems should be inquired by the general practitioner (93.2%). Nevertheless, only 14% of patients stated that they were already inquired by their general practitioner regarding the presence of a sexual problem. In general, the discussion of sexual health was initiated by the participant's own initiative (20.5%). The importance of sex for the patient's quality of was evaluated as “very important” or “important” by the majority of men (41.1% and 56.7%, respectively).
Sociodemographic characteristics and sexual health inquiring among male patients.
| Total sample (N=90) | No ED (N=61) | With ED (N=29) | p-Value | Test | ||||
|---|---|---|---|---|---|---|---|---|
| Age in years (mean, SDa) | 49.82 | 15.65 | 46.70 | 15.78 | 56.38 | 13.36 | 0.007 | MW |
| Age in years (n, %) | ||||||||
| 18–39 | 27 | 30.0% | 24 | 39.3% | 3 | 10.3% | 0.005 | CS-T |
| 40–59 | 33 | 36.7% | 21 | 34.4% | 12 | 41.4% | ||
| 60 or more | 30 | 33.3% | 16 | 26.2% | 14 | 48.3% | ||
| Place of birth (n, %) | ||||||||
| Portugal | 83 | 92.2% | 57 | 93.4% | 26 | 89.7% | 0.677 | FE |
| Other | 7 | 7.8% | 4 | 6.6% | 3 | 10.3% | ||
| Ethnic group (n, %) | ||||||||
| Caucasian | 85 | 95.5% | 58 | 96.7% | 27 | 93.1% | 0.594 | FE |
| Black | 4 | 4.5% | 2 | 3.3% | 2 | 6.9% | ||
| Religion (n, %) | ||||||||
| Religious | 78 | 87.6% | 52 | 86.7% | 26 | 89.7% | 0.999 | FE |
| Not religious | 11 | 12.4% | 8 | 13.3% | 3 | 10.3% | ||
| Marital status (n, %) | ||||||||
| Single | 18 | 20.0% | 13 | 21.3% | 5 | 17.2% | 0.519 | χ2 |
| Married | 64 | 71.1% | 41 | 67.2% | 23 | 79.3% | ||
| Divorced/Widowedb | 8 | 8.9% | 7 | 11.5% | 1 | 3.4% | ||
| Education (n, %) | ||||||||
| 9th grade or less | 52 | 57.8% | 29 | 47.5% | 23 | 79.3% | 0.004 | χ2 |
| High school or more | 38 | 42.2% | 32 | 52.5% | 6 | 20.7% | ||
| Profession (n, %) | ||||||||
| Working | 50 | 55.6% | 39 | 63.9% | 11 | 37.9% | 0.040 | χ2 |
| Retired | 33 | 36.7% | 17 | 27.9% | 16 | 55.2% | ||
| Unemployed/Other | 7 | 7.7% | 5 | 8.2% | 2 | 6.9% | ||
| Sexual problems should be inquired by GP (n, %) | 82 | 93.2% | 55 | 91.7% | 27 | 96.4% | 0.660 | FE |
| Inquired about sexual problems (n, %) | 12 | 14.0% | 7 | 11.9% | 5 | 18.5% | 0.409 | χ2 |
| Discussed sexual problems by own initiative (n, %) | 18 | 20.5% | 10 | 16.7% | 8 | 28.6% | 0.197 | χ2 |
| What's the importance of sex for your quality of life? (n,%) | ||||||||
| Very important | 37 | 41.1% | 24 | 39.3% | 13 | 44.8% | 0.621 | χ2 |
| Important | 51 | 56.7% | 36 | 59.0% | 15 | 51.7% | ||
| Not much/not at allb | 2 | 2.2% | 1 | 1.6% | 1 | 3.4% | ||
MW: Mann–Whitney test; CS-T: Chi-square for trends test; FE: Fisher's exact test; χ2: Chi-square test.
The bold values are statistically significant.
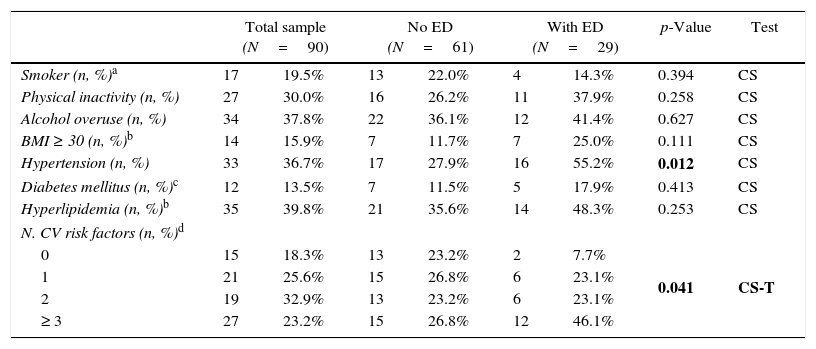
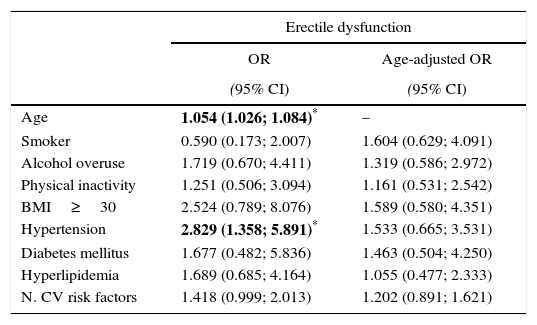
The prevalence of CVR factors is reported in Table 2. Comparing men with ED and without ED, only the prevalence of hypertension was significantly higher among the first group (55.2% vs. 27.9%; p=0.012). However, we observed a trend toward a higher prevalence of CVR factors among men with ED (except for smoking). These were also likely to have a significant higher number of CVR factors (p=0.041): (i) 46.1% of men with ED had at least 3 CVR factors and 7.7% had no CVR factors; (ii) 50% of men without ED had 1 or none CVR factor. Table 3 reports the odds ratios between ED and CVR factors. ED was significantly associated with age (OR=1.054; CI 95% 1.026–1.084) and hypertension (OR=2.83; CI 95% 1.36–5.89) but not with the clustering of CVR factors (OR=1.418; CI 95% 0.999; 2.013). However, after age-adjustment none of these associations remained significant.
Cardiovascular risk factors among male patients.
| Total sample (N=90) | No ED (N=61) | With ED (N=29) | p-Value | Test | ||||
|---|---|---|---|---|---|---|---|---|
| Smoker (n, %)a | 17 | 19.5% | 13 | 22.0% | 4 | 14.3% | 0.394 | CS |
| Physical inactivity (n, %) | 27 | 30.0% | 16 | 26.2% | 11 | 37.9% | 0.258 | CS |
| Alcohol overuse (n, %) | 34 | 37.8% | 22 | 36.1% | 12 | 41.4% | 0.627 | CS |
| BMI ≥ 30 (n, %)b | 14 | 15.9% | 7 | 11.7% | 7 | 25.0% | 0.111 | CS |
| Hypertension (n, %) | 33 | 36.7% | 17 | 27.9% | 16 | 55.2% | 0.012 | CS |
| Diabetes mellitus (n, %)c | 12 | 13.5% | 7 | 11.5% | 5 | 17.9% | 0.413 | CS |
| Hyperlipidemia (n, %)b | 35 | 39.8% | 21 | 35.6% | 14 | 48.3% | 0.253 | CS |
| N. CV risk factors (n, %)d | ||||||||
| 0 | 15 | 18.3% | 13 | 23.2% | 2 | 7.7% | 0.041 | CS-T |
| 1 | 21 | 25.6% | 15 | 26.8% | 6 | 23.1% | ||
| 2 | 19 | 32.9% | 13 | 23.2% | 6 | 23.1% | ||
| ≥ 3 | 27 | 23.2% | 15 | 26.8% | 12 | 46.1% | ||
CS: Chi-square test; CS-T: Chi-square for trends test.
The bold values are statistically significant.
Missing data:
Odds ratios between cardiovascular risk factors and erectile dysfunction.
| Erectile dysfunction | ||
|---|---|---|
| OR | Age-adjusted OR | |
| (95% CI) | (95% CI) | |
| Age | 1.054 (1.026; 1.084)* | – |
| Smoker | 0.590 (0.173; 2.007) | 1.604 (0.629; 4.091) |
| Alcohol overuse | 1.719 (0.670; 4.411) | 1.319 (0.586; 2.972) |
| Physical inactivity | 1.251 (0.506; 3.094) | 1.161 (0.531; 2.542) |
| BMI≥30 | 2.524 (0.789; 8.076) | 1.589 (0.580; 4.351) |
| Hypertension | 2.829 (1.358; 5.891)* | 1.533 (0.665; 3.531) |
| Diabetes mellitus | 1.677 (0.482; 5.836) | 1.463 (0.504; 4.250) |
| Hyperlipidemia | 1.689 (0.685; 4.164) | 1.055 (0.477; 2.333) |
| N. CV risk factors | 1.418 (0.999; 2.013) | 1.202 (0.891; 1.621) |
OR estimated through logistic regression models.
CI=confidence interval.
In the present study within the primary health care setting, ED was a frequent problem among men presenting at two Lisbon Primary Healthcare Centers (32% of patients). The overall ED prevalence was lower than in the Portuguese ED study (48% among men aged 40–69 years; n=3548; IIEF-defined ED)24 and higher than in Episex-PT study for men (13% among men aged between 18 and 75 years; n=1250; self-reported ED)25 and in Quinta Gomes et al.26 (10% among men aged 18–70 years; n=650; IIEF-defined but taking into consideration the frequency criteria proposed by Segraves4). The heterogeneity of patient population enrolled into studies (older patients and with more comorbidities in the Portuguese ED study24; patients enrolled in a community setting as in the Episex-PT study25 and in Quinta Gomes et al.26) and the different diagnostic methods to assess ED may explain the observed differences. Indeed, some variability is noted across several studies.27 Furthermore, in our study, ED prevalence increased significantly with age: 10% in men aged 18–39; 41% in men aged 40–59% and 48% in men aged 60 or more. This finding was in line with the aforementioned Portuguese studies.
Erectile dysfunction and cardiovascular risk factorsIn our sample of men with no previous cardiovascular events, it was shown a significantly higher prevalence of hypertension and number of CVR factors among patients with ED. Nevertheless, age was the only significant predictor of ED. Although ED and cardiovascular disease are thought to share a similar pathophysiology, they do not overlap perfectly. This emphasizes the role of other factors in the etiology, maintenance and progression of ED that go beyond CVR factors. We will try to explore some of these factors according to the results of our study.
Analyzing the CVR factors individually, only hypertension prevalence was significantly higher among men with ED. The use of anti-hypertensive drugs may also account, at least in part, for this observation. However, the observed trend toward a higher prevalence of CVR factors among men with ED (except for smoking) raises the question of whether these differences would be significant with a larger sample. In fact, hyperlipidemia,28,29 hypertension,28–30 diabetes,28,30 smoking,28,31 obesity28,32 and physical inactivity28,33 are well established risk factors for ED and are common among men with ED. Regarding alcohol overuse, there is little evidence of ED other than the acute effect of binge drinking.28 So, the observed trend is in agreement with the medical literature except for smoking in men. The higher proportion of older patients in the ED group who, probably, have different lifestyles compared to younger patients (no smoking habits, physical inactivity and alcohol overuse) may also explain these results. In addition, the existing differences in the population studied, clinical context, and also various definition criteria for evaluation of ED and CV risk factors among different studies may explain in part this discrepancy.
Regarding the number of CVR factors, in our study it was shown that these were significantly higher among men with ED. These findings are in agreement with the evidence that ED is related to poor CV status28 and is an indicator of poor global health.27 In men with ED, our study indicated that 46.1% had at least 3 CVR factors and that only 7.7% had no CVR factors, supporting that most patients with ED are known to have at least one significant CVR factor20,28 and the importance of ED assessment for cardiovascular risk reduction. Indeed, as lifestyle modification and pharmacotherapy for risk factors are effective in improving erectile function,34,35 ED diagnosis and treatment could play an important role in cardiovascular disease prevention due to a better cardiovascular risk assessment and control. Moreover, the pharmacological treatment of ED may have a beneficial impact on cardiovascular risk. Indeed, Frantzen et al.36 showed that 2 years after the use of sildenafil, the relative risk of the incidence of cardiovascular disease among men with ED compared with men without ED significantly decreased from 1.7 to 1.1. In addition, Gazzaruso et al.37 showed that type 5 phosphodiesterase inhibitors reduces the risk of major adverse cardiac events in diabetic patients with coronary artery disease and ED. Still, in our sample, we observed that ED were more related to the aging process than to the presence of CVR factors. Age was significantly associated with ED and after age-adjustment, the association found between ED and hypertension loosed its significance. Even though the lack of a significant association between hypertension and ED is contrary to a large body of evidence, our findings are in agreement with a previous population survey (n=924) aimed to assess factors modifying the effect of blood pressure on erectile function.38 In that study, when adjusted with age, cohabiting status, waist circumference, and education, the association of hypertension and erectile dysfunction was not statistically significant. Instead, they concluded that psychological factors play a major role in men with ED and that hypertension per se does not predispose men to erection problems. Moreover, in a cross-sectional Spanish study, an association was found between CVR factors, their number and the presence and severity of ED.20 However, this association did not include an adjustment for age. In fact, the prevalence of ED increases with age in parallel with many conditions and CVR factors such as diabetes, hypertension and a sedentary lifestyle. Therefore, evaluating the importance of comorbidities or risk factors for ED should include an adjustment for age. Furthermore, it should be noted that our findings are in agreement with the Massachussets Male Aging Study that revealed age as the variable most strongly associated with ED.2 Reasons why, given the same burden of CVR factors, younger patients seem to be protected from ED as compared to older ones are still not well understood. It is known that sexual function in men declines over time, usually beginning during the fifth decade and affecting all domains of sexual health including desire, arousal, erectile function, and ejaculation/orgasm.39,40 However, physiological sexual competency does not guarantee a sexually active relationship. Positive reinforcing feedback is necessary from one partner to the other and novelty of sexual behavior within that relationship.41 In fact, some studies have noted that good physical health, the availability of a partner, and a regular and stable pattern of sexual activity earlier in life predict the maintenance of sexual activity in old age.42 Moreover, a causal relationship between sexual dysfunction in women and the onset of ED has been suggested in one study where it was found that female sexual dysfunctions were frequent before the onset of ED.43 In addition, several studies have found a high prevalence of sexual dysfunctions in female partners of men who present with ED.44 In addition, it should be noted that, in our study, men with ED had a lower educational level and were more professionally inactive than patients without ED. This finding is in agreement with previous studies reporting that educational level and social status is also strongly associated with sexual problems.25,26,45 Findings have indicated that education play a protective role, with well-educated patients reporting lower levels of sexual problems.26 Therefore, even though CV risk factors may negatively impact over erectile function, several other factors such as age, educational attainment, social status and partner issues should also be object of further research in order to better understand their impact on male sexual function.
Erectile dysfunction inquiryThe majority of men stated that sex is “very important” or “important” for their quality of life (97.8%) and affirmed that sexual problems should be inquired by the general practitioner (93.2%) but only a minority were already inquired about it (14%). Our results are in line with previous studies. Indeed, a study focusing on the management of ED found that only 9.6% of GPs routinely asked for ED in patients over 40 years, but this number increased (45.2%) when the patients had risk factors for this condition.17 Moreover, in a study where more than 70% of adult patients considered sexual health to be an appropriate topic for the general practitioner to discuss, evidence of discussion about sexual problems were present in only 2% of cases.18 In addition, a previous research in Portugal, using self-administrated questionnaires applied to general practitioners working in primary healthcare units in the Lisbon, found that routine sexual history taking and consultation of guidelines about sexual dysfunctions are not yet a generalized practice, as only 15.5% of 50 participants actively ask their patients about sexual dysfunctions,16 and several barriers to initiate a dialog about sexual health were recognized, namely: (i) personal attitudes and beliefs; (ii) lack of time, both to deal with these issues and to obtain information for clinical practice – the average time that these appointments took was 24±8.2min; (iii) lack of academic training and of experience in this area – 50% of general practitioners considered that their medical degree was not an adequate source of training and 91% reported a need for continuous training. Interestingly, general practitioners’ gender was not a barrier and, in general, they seemed to be more competent in treating sexual dysfunctions than in discussing them.15 Similar barriers were identified in other studies.46–48 Thus, the low sexual health inquiry rate observed in our study can find its explanation mainly on these barriers.
Our results highlight the need to meet patients’ expectations regarding the discussion of sexual health in primary care. Several factors make primary care the ideal setting for sexual health discussion. First, patients with sexual concerns report feeling most comfortable discussing these issues with their general practitioner and expect to receive advice and treatment49; second, the multifactorial issues surrounding ED are appropriately evaluable by the patient's clinician; and third, the long-term follow-up needed to ensure that ED is resolved is suited to primary care.45 Thus, educational interventions designed to improve general practitioners’ clinical competences in ED assessment and treatment should be developed to overcome the existing barriers and to answer the patient's needs and expectations toward their sexual health. The implementation of sexual inquiry should occur at a minimum during the health surveillance visit or during the initiation of another therapy that might affect sexual function.50
Methodological limitationsFirst and chief among them is the reliance on a small cross-sectional study. A cross-sectional study with a larger sample or, optimally, a longitudinal research is needed to better clarify the role of CVR factors, patient's characteristics and partner issues in the etiology and maintenance of ED in patients with no previous cardiovascular events. Second, the assessment of CVR factors through self-report, clinical record and medication has its own limitations: even this trivalent method may not detect patients with undiagnosed conditions such as hypertension, hyperlipidemia and diabetes. Fourth, we did not assess the effect of other diseases and medications that could interfere with sexual function. Fifth, in the present study, 38 (27%) of the men reported not having had sexual activity and/or sexual intercourse during the past four weeks. This result could be due to a low pattern of sexual activity frequency or due to avoiding sexual contact because of sexual problems experienced previously. The exclusion of these patients can represent an underestimation of ED prevalence and the loss of patients whose ED could be associated with CVR factors. However, some of the largest observational Portuguese studies in this field have also used the same exclusion criteria regarding sexual inactivity in men.24,26 Moreover, the current proposed definition of ED implicates a failure to obtain and maintain an erection sufficient for sexual activity on 75% occasions and lasting for at least 6 months.4 This new definition highlights that some erectile difficulties are transient and should not be diagnosed as ED. So, in our study we may have classified some erectile difficulties in the past 4 weeks that are not “real” ED but represent instead transient erectile difficulties. In fact, the limited assessment of erectile function to the last four weeks, together with the inability to effectively investigate psycho-relational aspects, reveals that IIEF is not a perfect tool for diagnostic purposes. Although not perfect, IIEF is the most widely used instrument to evaluate ED for research purposes due to its excellent validity. So, in further studies, patients without sexual activity should also be characterized and ED should be diagnosed according to new proposed criteria even. Therefore, our results can only be interpreted in light of those patients who were sexually active in the past four weeks. At last, we should mention that the results of the sexual health inquiry should also be interpreted with caution due to the small size of our sample. In fact, further studies with larger and representative samples of the Portuguese primary care setting should be realized to determine more accurately the rate of sexual health inquiry among patients with no previous cardiovascular events. Furthermore, the rate of sexual inquiry could also be better characterized according to the patients and general practitioner's characteristics.
ConclusionIn summary, ED is highly prevalent among men attending the primary care with no history of cardiovascular events and those with ED tend to have a higher prevalence of hypertension and a higher number of CVR factors. Even though age was the only significant predictor of ED, our findings should alert the general practitioners to improve the sexual health inquiry as it could provide an important step in cardiovascular risk reduction. In fact, a low sexual health inquiry rate was observed even though the majority of men stated that sex is “very important” or “important” for their quality of life. Thus, educational interventions designed to improve general practitioners’ clinical competences in ED assessment and treatment should be developed to overcome the existing barriers and answer the patient's needs.
FundingThis study was supported by a scientific grant from AstraZeneca Foundation and by the Program “Educação pela Ciência”, GAPIC/FMUL. The supporters did not have any role in the design and conduct of the study, neither in the collection, management, analysis, and interpretation of the data, or in the preparation, review or approval of the article.
Conflicts of interestThe authors have no conflicts of interest to declare.
We would like to thank ACES-Odivelas Health Units and SEXOS Study Research Team.