Schizoaffective disorder is defined by the appearance of positive psychotic symptomatology as well as affective features, even when it is considered a controversial nosologic entity, proving difficult to accord on its definition or diagnostic criteria. Due to these conceptual differences, it has been a challenge to study effective therapeutic measures and, consequently, the availability of data in the current literature, resulting in the extrapolation of clinical guidelines and recommendations initially established for patients with schizophrenia or bipolar disorder. The current study aimed to systematically search and summarize the published evidence to date about the use of clozapine in patients with schizoaffective disorder. Seven studies were identified, that are heterogeneous on their designs and methodology, including samples of patients mixed with bipolar or schizophrenic disorders. The evidence was summarized both in a table and a narrative fashion, suggesting that clozapine may be an effective treatment for both psychotic and affective symptoms, indistinctively of an acute or maintenance phase.
El trastorno esquizoafectivo se define por la presentación de síntomas psicóticos y clínica afectiva, aun cuando se considera una entidad nosológica controvertida, con dificultad para consensuar definiciones o criterios diagnósticos. Dadas las dificultades conceptuales, ha sido un reto el estudio de medidas terapéuticas eficaces y su publicación en la literatura científica, extrapolándose generalmente las recomendaciones clínicas de aquellas generadas para poblaciones mixtas con esquizofrenia o trastorno bipolar. El presente estudio intentó buscar y resumir de forma sistemática la evidencia publicada hasta la fecha sobre el uso de clozapina en pacientes con trastorno esquizoafectivo. Se identificaron siete estudios en total, heterogéneos en cuanto a diseño y metodología, siendo las muestras siempre mezclas de pacientes con esquizofrenia o trastorno bipolar. Se resumió la evidencia en una tabla y se realizó un resumen narrativo sobre los hallazgos, sugiriendo que la clozapina podría ser un tratamiento eficaz para los síntomas tanto afectivos como psicóticos, indistintamente de una fase aguda o de mantenimiento.
Schizoaffective disorder is defined by the presence of psychotic symptoms prototypical of schizophrenia and affective symptoms in the form of manic or depressive episodes. Its prevalence is between .2 and 1.1%,1,2 a percentage of .32% is estimated in some populations compared to .87% for schizophrenia or .24% for bipolar disorder.3 Placing this controversial nosological entity, borderline between schizophrenia and bipolar disorder, in a category has been a constant challenge since the term "schizoaffective" was coined in 1933.4 Its evolution from initially being considered a subtype of schizophrenia to being established as an independent category in recent years has been marked by a lack of consensus and variations in its definition over time.5,6 Its clinical reliability has often been questioned despite having remained a distinct entity in subsequent classifications.7–9 This conceptual instability results in a significant delay in the evidence on key aspects such as the therapeutic strategy to deploy in these patients. Current clinical recommendations are based on data from observational studies in the main and subgroup analyses of large trials in schizophrenia or extrapolations from samples of bipolar or schizophrenic patients.10
The accepted and most widely used pharmacological approach in schizoaffective disorder in routine clinical practice is based on a combination of mood stabilisers and antipsychotics, as well as antidepressants in some subtypes.11,12 Unlike mood stabilisers, second-generation antipsychotics are the most studied drugs in both acute and long-term episodes with this diagnosis.13,14 Risperidone and paliperidone present the strongest evidence to date.15–20 Therefore, they are proposed as first-line treatment, although the evidence remains very limited.21,22 Clozapine, considered the first atypical or second generation antipsychotic based on its 5HT2A antagonism, has a differential pharmacological profile with a weak affinity for D2, D1 and higher affinity for D4, 5-HT2A, 5-HT2C, 5-HT6, 5-HT7 receptors. Classically, it is known for its superiority over other antipsychotics in patients with schizophrenia,23–26 especially in those with resistant psychotic symptoms, and is the gold standard of efficacy in non-responders to trials with other treatments.27–31 There is clear evidence of its role in reducing suicidal behaviour in both schizophrenic and schizoaffective patients,32–34 and in reducing aggressive behaviour.35 Although the results are more controversial, it seems to have an advantage in relation to negative symptoms, cognitive performance, and global functioning over other molecules in its class.23,36 The evidence has also been growing in recent years of its effect on affective symptoms,37–39 primarily in episodes of mania,40,41 and its usefulness in bipolar patients.42–46 However, the evidence for its use is not well established.
Although it has multiple indications and a recognised efficacy profile, we know that clozapine is, in general and in line with international data, underused in our setting.47–49 There is also significant delay in starting to prescribe the drug and antipsychotic polypharmacy is often used as an alternative.48,49 The risk of severe side effects, primarily agranulocytosis and myocarditis, and others that might prevent it being adequately tolerated, such as weight gain or metabolic syndrome seem to justify relegating its use in favour of other available options.
The aim of this paper was to conduct a systematic review of the literature and summarise the current evidence available on the efficacy of clozapine in patients with schizoaffective disorder.
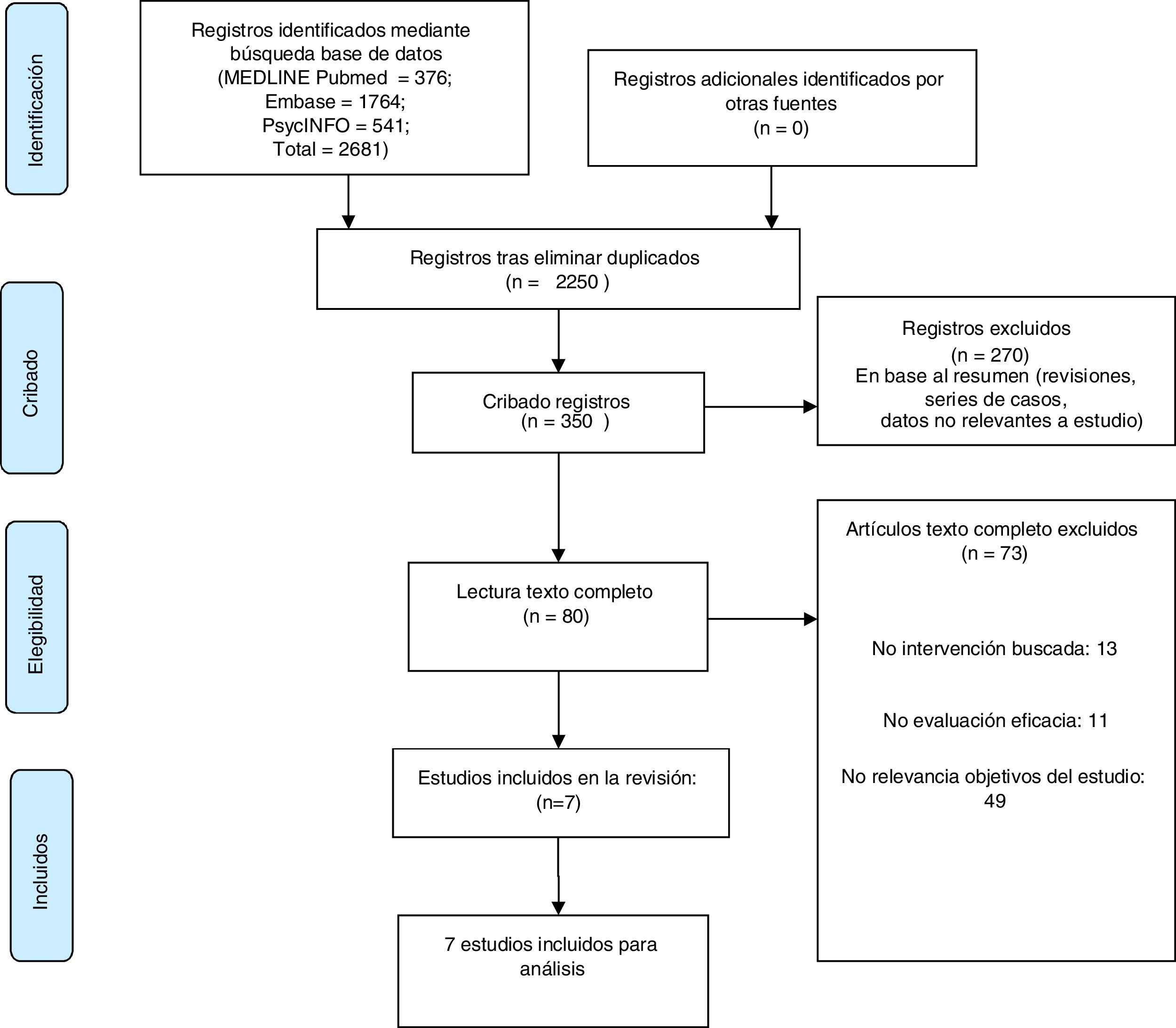
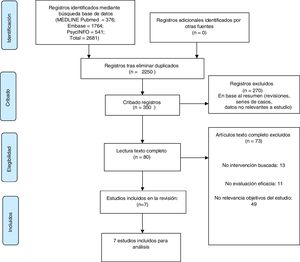
MethodsWe conducted a systematic literature search following the recommendations of the PRISMA50 statement to identify publications evaluating the efficacy of clozapine in patients with schizoaffective disorder.
Information sources and search strategiesStudies were identified through a search of electronic databases. Three databases were used: MeDLINE, EMBASE and PsycINFO. All studies published between 1980 and 2017 were included. A final update search until June 2018 was conducted. The initial strategy included the following terms, thus: "Clozapine" AND "schizoaffective".
Study selection criteriaRandomised controlled clinical trials and prospective trials that evaluated the efficacy of clozapine treatment in patients with a diagnosis of schizoaffective disorder were included. Because we know the evidence is scant, we included studies in which the total sample included several diagnoses of psychotic disorders, such as schizophrenia or bipolar disorder in the phase of psychotic mania, and patients with schizoaffective disorder were only a subgroup of this. Studies of any time duration were included, and no restriction was made in terms of language of publication. Retrospective studies, narrative reviews, systematic or meta-analyses were excluded from the review, as were individual case reports.
Data extractionThe studies were selected independently on a form created by two reviewers who reviewed the search citations and identified relevant abstracts. Disagreements between reviewers were resolved by consensus or by accessing the full report for further analysis. The name of the lead author and year of publication, type of design, population used and number of schizoaffective patients, inclusion/exclusion criteria for participants, study duration, type of intervention and outcome measures were recorded in detail for each study.
ResultsA total of 2681 references were identified in the initial search from the three databases (Fig. 1). After removal of duplicates, 2250 references were obtained, and this was narrowed down to 350 studies after title reading. After evaluating the abstracts, the selection was narrowed down to a total of 80 articles that would meet the inclusion criteria. The full text of these articles was reviewed in detail, 73 were discarded as they did not match the study objectives and seven were finally included in the systematic review.
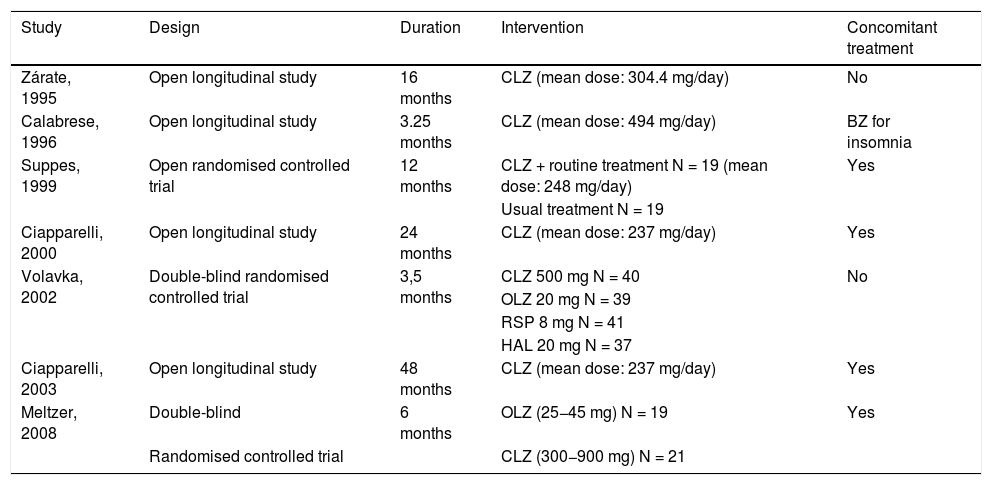
Of the total seven studies chosen for the review, three were randomised controlled trials, one open and two double-blind; four were longitudinal studies. The patients were a total of 118 from all the studies. These were followed for between 13 weeks and 48 months.
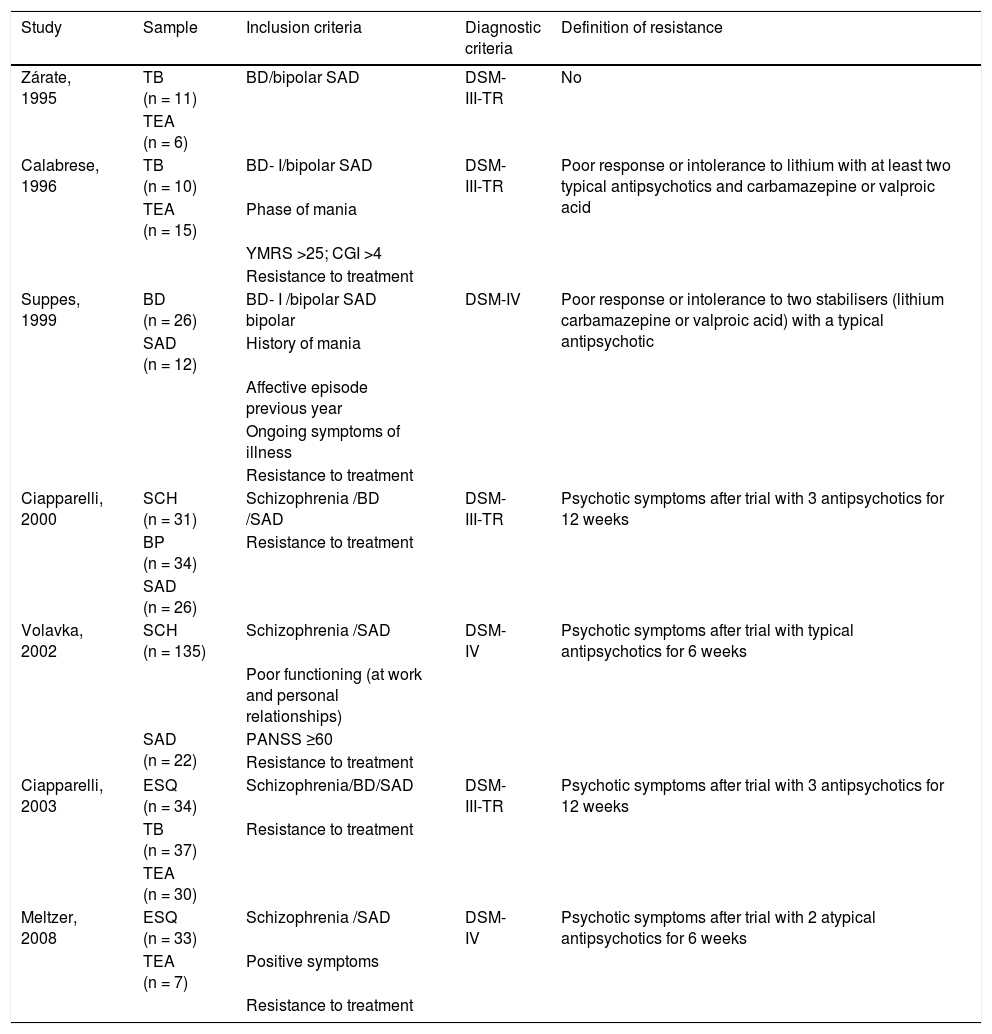
No studies were found that focused exclusively on patients with schizoaffective disorder; all the samples were heterogeneous with patients with bipolar disorder, schizophrenia, and schizoaffective disorder. The diagnostic criteria were as defined in the DSM III-R and DSM IV classifications. Treatment-resistant schizoaffective patients were considered in all studies, although the criteria for resistance varied between studies.
No placebo-controlled trials were found. Comparisons were frequently made with other antipsychotics such as olanzapine, at regular and high doses, risperidone, or haloperidol.
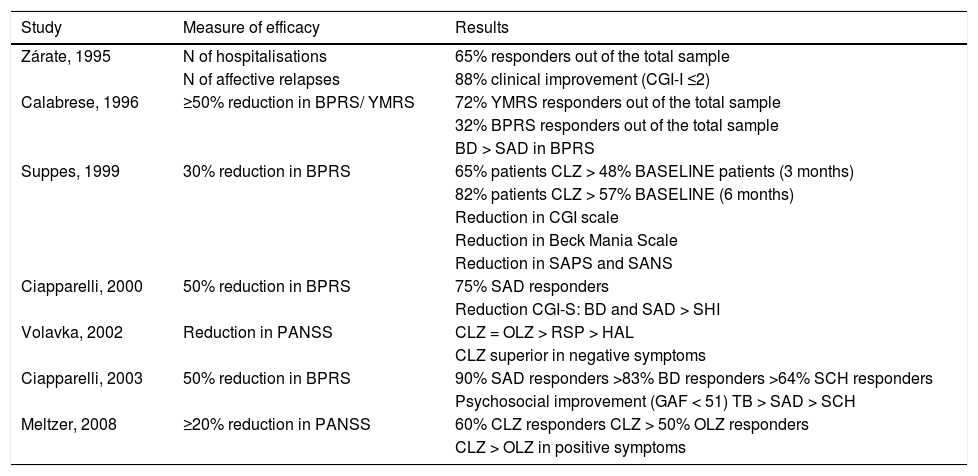
The first study included in the review51 describes a post hoc analysis examining a group of bipolar and schizoaffective bipolar patients (six patients) on clozapine monotherapy. Most of the patients were resistant to or had not tolerated regular treatment with lithium, valproic acid, carbamazepine, or neuroleptics, although this was not a criterion for inclusion in the study. The study found that, after 16 months of clozapine treatment, 65% of patients had no hospitalisations or affective relapses. Furthermore, 88% showed statistically significant clinical improvement (p = .02), measured by the CGI-I scale.
A later 13-week longitudinal study52 included 25 bipolar and schizoaffective patients (15 schizoaffective) with poor response or intolerant to treatment with lithium, and at least two neuroleptics, and carbamazepine or valproate with active symptoms of mania. The results after the clozapine trial showed that 72% of patients showed a marked reduction in Young's scale, and 32% of them showed a marked reduction in the BPRS (reduction greater than or equal to 50%).
The study by Suppes et al.53 compared the efficacy of clozapine in combination with treatment regular treatment in bipolar type I and schizoaffective bipolar patients (32% of the sample) with treatment resistance. Treatment resistance was defined as the persistence of symptoms after using two mood stabilisers and one antipsychotic. Patients who had clozapine added to their baseline treatment showed a greater response measured as a 30% improvement in BPRS score. This improvement took place at six months in 82% of patients in the clozapine group compared to 57% in the regular treatment group. Significant improvements were also found in other comparison measures between the two groups (CGI, SAPS, SANS, Beck mania) except for the depression scale (HDRS). In addition, a reduction in total medication and dropouts was found in the clozapine group.
In another naturalistic study,54 a total of 91 (26 schizoaffective) resistant patients (defined as three trials with different neuroleptics) were followed up with clozapine added to their regular treatment for 24 months. At the end of follow-up, a statistically significant (p < .001), sustained clinical improvement was observed, with the response being superior in the bipolar and schizoaffective patients compared to the schizophrenics. To be specific, 75% of schizoaffective patients responded to treatment with a 50% reduction in BPRS total score.
The double-blind study by Volavka et al.55 focussed on a sample of schizophrenic and schizoaffective patients (14% of the sample), with suboptimal response to treatment with first generation antipsychotics and low level of functioning. The efficacy of three atypical antipsychotics was compared between each and with haloperidol. Both clozapine and olanzapine demonstrated greater efficacy than risperidone and haloperidol, in monotherapy, in symptom control with statistically significant improvements in total PANSS score. Clozapine was superior in improving negative symptoms, although the differences were small.
A 48-month longitudinal study56 was conducted in 2003 on a total of 101 patients (30 schizoaffective), resistant to three different neuroleptic trials, who had clozapine added to their usual treatment. At the end of follow-up, there was a progressive reduction in BPRS score (greater than or equal to 50%) in the schizoaffective patients, with a higher follow-up completion rate with respect to the other diagnoses, as well as an improvement in psychosocial functioning (decrease in GAF scores below 51).
The last trial included57 was a six-month, randomised, controlled, parallel-group study assessing the efficacy of clozapine compared to high-dose olanzapine in patients with schizophrenia or schizoaffective disorder (seven in the sample) resistant to antipsychotic treatment. Mood stabilisers and antidepressants were also combined during the trial in the schizoaffective disorder patients. Both groups had improved PANSS total score (decrease of 20% or more) and in the positive and negative symptom subscales, with clozapine showing superiority in positive symptom remission, Tables 1–3.
Design of each study.
| Study | Design | Duration | Intervention | Concomitant treatment |
|---|---|---|---|---|
| Zárate, 1995 | Open longitudinal study | 16 months | CLZ (mean dose: 304.4 mg/day) | No |
| Calabrese, 1996 | Open longitudinal study | 3.25 months | CLZ (mean dose: 494 mg/day) | BZ for insomnia |
| Suppes, 1999 | Open randomised controlled trial | 12 months | CLZ + routine treatment N = 19 (mean dose: 248 mg/day) | Yes |
| Usual treatment N = 19 | ||||
| Ciapparelli, 2000 | Open longitudinal study | 24 months | CLZ (mean dose: 237 mg/day) | Yes |
| Volavka, 2002 | Double-blind randomised controlled trial | 3,5 months | CLZ 500 mg N = 40 | No |
| OLZ 20 mg N = 39 | ||||
| RSP 8 mg N = 41 | ||||
| HAL 20 mg N = 37 | ||||
| Ciapparelli, 2003 | Open longitudinal study | 48 months | CLZ (mean dose: 237 mg/day) | Yes |
| Meltzer, 2008 | Double-blind | 6 months | OLZ (25−45 mg) N = 19 | Yes |
| Randomised controlled trial | CLZ (300−900 mg) N = 21 |
BZ: benzodiazepines; CLZ: clozapine; HAL: haloperidol; OLZ: olanzapine; RSP: risperidone.
Inclusion and sample of each study.
| Study | Sample | Inclusion criteria | Diagnostic criteria | Definition of resistance |
|---|---|---|---|---|
| Zárate, 1995 | TB (n = 11) | BD/bipolar SAD | DSM-III-TR | No |
| TEA (n = 6) | ||||
| Calabrese, 1996 | TB (n = 10) | BD- I/bipolar SAD | DSM-III-TR | Poor response or intolerance to lithium with at least two typical antipsychotics and carbamazepine or valproic acid |
| TEA (n = 15) | Phase of mania | |||
| YMRS >25; CGI >4 | ||||
| Resistance to treatment | ||||
| Suppes, 1999 | BD (n = 26) | BD- I /bipolar SAD bipolar | DSM-IV | Poor response or intolerance to two stabilisers (lithium carbamazepine or valproic acid) with a typical antipsychotic |
| SAD (n = 12) | History of mania | |||
| Affective episode previous year | ||||
| Ongoing symptoms of illness | ||||
| Resistance to treatment | ||||
| Ciapparelli, 2000 | SCH (n = 31) | Schizophrenia /BD /SAD | DSM-III-TR | Psychotic symptoms after trial with 3 antipsychotics for 12 weeks |
| BP (n = 34) | Resistance to treatment | |||
| SAD (n = 26) | ||||
| Volavka, 2002 | SCH (n = 135) | Schizophrenia /SAD | DSM-IV | Psychotic symptoms after trial with typical antipsychotics for 6 weeks |
| Poor functioning (at work and personal relationships) | ||||
| SAD (n = 22) | PANSS ≥60 | |||
| Resistance to treatment | ||||
| Ciapparelli, 2003 | ESQ (n = 34) | Schizophrenia/BD/SAD | DSM-III-TR | Psychotic symptoms after trial with 3 antipsychotics for 12 weeks |
| TB (n = 37) | Resistance to treatment | |||
| TEA (n = 30) | ||||
| Meltzer, 2008 | ESQ (n = 33) | Schizophrenia /SAD | DSM-IV | Psychotic symptoms after trial with 2 atypical antipsychotics for 6 weeks |
| TEA (n = 7) | Positive symptoms | |||
| Resistance to treatment |
BD: Bipolar Disorder; CGI: Clinical Global Impression Scale; PANSS: Positive and Negative Syndrome Scale; SAD: schizoaffective disorder; SCH: schizophrenia; YMRS: Young Mania Rating Scale.
Summary of the results of each study.
| Study | Measure of efficacy | Results |
|---|---|---|
| Zárate, 1995 | N of hospitalisations | 65% responders out of the total sample |
| N of affective relapses | 88% clinical improvement (CGI-I ≤2) | |
| Calabrese, 1996 | ≥50% reduction in BPRS/ YMRS | 72% YMRS responders out of the total sample |
| 32% BPRS responders out of the total sample | ||
| BD > SAD in BPRS | ||
| Suppes, 1999 | 30% reduction in BPRS | 65% patients CLZ > 48% BASELINE patients (3 months) |
| 82% patients CLZ > 57% BASELINE (6 months) | ||
| Reduction in CGI scale | ||
| Reduction in Beck Mania Scale | ||
| Reduction in SAPS and SANS | ||
| Ciapparelli, 2000 | 50% reduction in BPRS | 75% SAD responders |
| Reduction CGI-S: BD and SAD > SHI | ||
| Volavka, 2002 | Reduction in PANSS | CLZ = OLZ > RSP > HAL |
| CLZ superior in negative symptoms | ||
| Ciapparelli, 2003 | 50% reduction in BPRS | 90% SAD responders >83% BD responders >64% SCH responders |
| Psychosocial improvement (GAF < 51) TB > SAD > SCH | ||
| Meltzer, 2008 | ≥20% reduction in PANSS | 60% CLZ responders CLZ > 50% OLZ responders |
| CLZ > OLZ in positive symptoms |
BD: Bipolar Disorder; BPRS: Brief Psychiatric Rating Scale; CGI: Clinical Global Impression Scale; CLZ: clozapine; GAF: Global Assessment of Functioning; HAL: haloperidol; OLZ: olanzapine; PANSS: Positive and Negative Syndrome Scale; RSP: risperidone; SAD: schizoaffective disorder; SCH: schizophrenia; YMRS: Young Mania Rating Scale.
The aim of the present study was to review the published evidence on the efficacy of clozapine in the population with schizoaffective disorder.
With a clear profile of use and efficacy in psychotic patients, there seems to be progressively greater evidence41,44,46 of the usefulness Clozapine in affective symptoms. There is a trend towards under-prescription and under-use of this antipsychotic that may be because it has been associate with potentially serious side effects.58,59 However, in relation to these effects, different studies show that onset of the most serious complication, agranulocytosis, is rare and its risk decreases after the first six months of treatment.60–62
In general, there are very few of trials that evaluate drug treatment in schizoaffective disorder, and there even fewer on clozapine. Previous reviews21,22 have reported that that the treatment of schizoaffective disorder has been little studied and that current treatment guidelines are based on limited evidence, the approach being predominantly symptomatic and non-specific. This lack of studies may be due to the difficulty in establishing stable and unified diagnostic criteria, and the low diagnostic stability reported for this disorder,63,64 which may limit patient choice and comparison of results.
We found no studies in the review that focused exclusively on schizoaffective population samples. In all the references found, they appear as a subgroup alongside bipolar or schizophrenic patients. This makes it difficult to interpret and compare the results, which in most studies are not reported by diagnostic category.
The studies reviewed are generally of low quality. They are characterised by small sample sizes51,52 that make a correct analysis of efficiency difficult; they have short follow-ups52,55 that either do not evaluate long-term maintenance treatment, or do so only to a limited extent, and they lack randomisation and a control group.51,52,54,56 In addition, there is significant heterogeneity in the use of clozapine in monotherapy or in combination, half the studies found allowed the associated use of mood stabilisers and antidepressants compared to those that assess clozapine in monotherapy. This again makes it difficult to compare results.
Although the evidence is limited, the results found would support the usefulness of clozapine in the control and reduction of affective symptoms in schizoaffective patients. In particular, one controlled trial53 and one longitudinal follow-up trial52 show its efficacy in reducing symptoms of mania, both in monotherapy52 and in combination with routine treatment53 in patients in whom other mood stabilisers have failed. In the studies reviewed, the efficacy of clozapine on depressive symptoms appears to be limited, showing no significant improvement. Since clozapine is known to have an effect in reducing suicidal behaviour, this may support the hypothesis of its effect through a mechanism independent of symptom reduction. Another longitudinal study of clozapine monotherapy shows a reduction in affective relapses and number of hospitalisations.51
In line with the effect that is already known in other diagnoses,29–31 clozapine would show efficacy in controlling psychotic symptoms in resistant schizoaffective patients. Two controlled studies55,57 suggest its efficacy in controlling both positive and negative psychotic symptoms, in monotherapy and in combination with other treatments, with results similar or even superior to those of olanzapine.
Overall, uncontrolled studies51,52,54 suggest that clozapine has a long-term stabilising effect. Longitudinal follow-up, although with major methodological limitations, finds a significant clinical improvement that increases with time on the treatment.56 In addition, clozapine reduces the use of concomitant drugs including mood stabilisers in studies that used combined treatments. Although only one of the studies measured this effect, it suggests an improvement in psychosocial functioning with clozapine.56
We should note that the patients selected for inclusion in all but one of the reviewed studies51 are resistant to treatment with lithium, valproic acid or other mood stabilisers, and first- or second-generation antipsychotics. This choice of patients seems to follow the usual line of prescribing clozapine in patients who are resistant or intolerant to conventional treatment. Although the criteria for measuring this resistance are heterogeneous across the studies, the results would support the use of clozapine in patients with refractory schizoaffective disorder.
ConclusionsThe results of studies suggest that clozapine appears to have an effect on both acute and long-term affective symptoms of mania and psychotic symptoms, which may be indicative of its usefulness in schizoaffective patients. However, the data on this diagnosis are limited, there are few studies examining the efficacy of clozapine in patients with schizoaffective disorder, and more studies are needed with an adequate design to evaluate this indication.
Conflict of interestsDr Vieta has received grants and has been a CME consultant, advisor or speaker for the following entities: AB-Biotics, Abbott, Allergan, Angelini, AstraZeneca, Bristol-Myers Squibb, Dainippon Sumitomo Pharma, Farmindustria, Ferrer, Forest Research Institute, Gedeon Richter, Glaxo-Smith-Kline, Janssen, Lundbeck, Otsuka, Pfizer, Roche, SAGE, Sanofi-Aventis, Servier, Shire, Sunovion, Takeda, the Brain and Behaviour Foundation, the Generalitat de Catalunya (PERIS), the Ministry of Science, Innovation and Universities (CIBERSAM), EU Horizon 2020 and the Stanley Medical Research Institute.
Dr Benabarre has been a speaker for: Lundbeck, Otsuka, Janssen.
Please cite this article as: Rey Souto D, Pinzón Espinosa J, Vieta E, Benabarre Hernández A. Clozapina en pacientes con trastorno esquizoafectivo: una revisión sistemática. Rev Psiquiatr Salud Ment (Barc.). 2021;14:148–156.