Schizophrenia and other psychotic disorders are associated with high morbidity and mortality, due to inherent health factors, genetic factors, and factors related to psychopharmacological treatment. Antipsychotics, like other drugs, have side-effects that can substantially affect the physical health of patients, with substantive differences in the side-effect profile and in the patients in which these side-effects occur. To understand and identify these risk groups could help to prevent the occurrence of the undesired effects.
Material and methodA prospective study, with 24 months follow-up, was conducted in order to analyse the physical health of severe mental patients under maintenance treatment with atypical antipsychotics, as well as to determine any predictive parameters at anthropometric and/or analytical level for good/bad outcome of metabolic syndrome in these patients.
ResultsThere were no significant changes in the physical and biochemical parameters individually analysed throughout the different visits. The baseline abdominal circumference (lambda Wilks p=.013) and baseline HDL-cholesterol levels (lambda Wilks p=.000) were the parameters that seem to be more relevant above the rest of the metabolic syndrome constituents diagnosis criteria as predictors in the long-term.
ConclusionsIn the search for predictive factors of metabolic syndrome, HDL-cholesterol and abdominal circumference at the time of inclusion were selected, as such that the worst the baseline results were, the higher probability of long-term improvement.
La esquizofrenia y otros trastornos psicóticos se asocian a una elevada morbimortalidad debido a factores de salud inherentes a la propia enfermedad, factores genéticos y factores asociados al tratamiento psicofarmacológico. Los antipsicóticos, al igual que otros fármacos, presentan efectos secundarios que pueden repercutir de manera sustancial en la salud física de los pacientes, existiendo diferencias importantes en cuanto al perfil de efectos secundarios y en los pacientes en que se producen dichos efectos. Conocer e identificar estos grupos de riesgo podría contribuir a prevenir la aparición de los efectos indeseados.
Material y métodoEstudio prospectivo, de seguimiento a 24 meses, para analizar la salud física de los pacientes mentales graves en tratamiento de mantenimiento con antipsicóticos atípicos con el fin de verificar la existencia de parámetros predictores a nivel antropométrico y/o analítico para la buena/mala evolución del síndrome metabólico en estos pacientes.
ResultadosNo hubo cambios significativos de los parámetros físicos y bioquímicos estudiados individualmente a lo largo de las diferentes visitas. El perímetro abdominal basal (lamba de Wilks p=0,013) y los niveles de colesterol HDL basal (lamba de Wilks p=0,000) son los parámetros que parecen tener mayor relevancia, por encima del resto de los criterios diagnósticos constituyentes del síndrome metabólico, como factores predictores en la evolución a largo plazo.
ConclusionesEn la búsqueda de parámetros predictores del síndrome metabólico resultaron seleccionados el colesterol HDL y el perímetro abdominal en el momento de la inclusión, de modo que a peores valores iniciales, mayor probabilidad de mejoría a largo plazo.
Schizophrenia and other psychotic disorders are associated with high morbidity and mortality rates, the causes of which, in part, may possibly be associated with antipsychotic treatment.
Patients with schizophrenia have a life expectancy 20% lower than the general population, with a loss of around 25 years of life.1 A relative risk of 2.41-fold is estimated for mortality from natural causes, especially cardiovascular, infectious, respiratory and endocrine diseases2 (60% of premature deaths in these patients).
The higher cardiovascular mortality associated with schizophrenia and other diseases within the psychotic spectrum has been put down to the presence of modifiable risk factors for cardiovascular disease, which are between one and five times greater than for the rest of the population.3 Among their causes are health factors inherent in the disease itself, genetic factors, and those associated with psychopharmacological treatment, reduced access to adequate physical health care and unhealthy living habits.
Since the appearance of antipsychotics in the late 1950s, the prognosis of patients with schizophrenia has improved markedly. However, like any other type of drug, they have side effects that can have a substantial impact on patients’ physical health, quality of life and adherence to treatment, such as a higher prevalence of metabolic and endocrine disorders and an increased risk of developing cardiovascular disease in the case of atypical antipsychotics.
Among atypical antipsychotics there are important differences in the profile of different side effects, and these adverse effects occur only in certain patients.4 The current situation is that risk groups are not yet sufficiently identified to be able to combat each of these adverse effects.
Discovering and identifying these risk groups could, in some cases, contribute to preventing the onset of undesirable effects by establishing preventive strategies to improve the physical health of patients with severe mental illness.5,6
The majority of studies on the prevention of metabolic and cardiovascular risk, associated with atypical antipsychotics, have focussed on early episodes, but there are very few studies on the progression of these parameters in the continuation phase of treatment in patients with chronic disease and long-term follow-up. This stage is, a priori, very important to ascertain the development of cardiovascular risk, considering the long duration of these treatments. In particular, it seems important to be aware of predictors of progression in order to devise preventive strategies.
This is why a prospective 2-year study was designed to analyse the physical health of the seriously mentally ill on maintenance treatment with atypical antipsychotics in order to verify the existence of predictive parameters at the anthropometric and analytical level for positive/negative development of the metabolic syndrome, as well as assess whether patients’ progress in this area can be improved by psychoeducational programmes.
Material and methodsParticipantsA total of 75 patients from the Day Hospital at the Hospital Universitario de Valladolid were included. Patients, who could be of either sex, had to be over 18 years of age, diagnosed as having schizophrenia, schizoaffective disorder or bipolar disorder; either admitted to the Day Hospital (hospitalised or under surveillance) and on treatment with an atypical antipsychotic. Use of 2 antipsychotics was not permitted (except for an atypical antipsychotic together with a classic low dose antipsychotic used as an adjuvant, for example as a hypnotic drug, or an atypical depot antipsychotic together with an oral antipsychotic—typical or atypical—at low doses, when the oral drug is used as depot adjuvant, for example, as a hypnotic drug). Patients on treatment with eukaryotes and anti-Parkinson drugs were included. The use of benzodiazepines and antidepressants was permitted for a short period.
During the study, anthropometric and analytical data was collected periodically (at baseline and at 3, 6, 12, 18 and 24 months), which also included socio-demographic data, health habits, diagnosis, treatment, personal history and that of relatives, on cardiovascular risk factors and other relevant data for the study.
The study protocol was approved by the Research Committee of the Valladolid University Hospital and drafted in accordance with the Declaration of Helsinki.
At the time of patient selection and signing the consent, the nature of the study was explained to the patients and, if necessary, to their relatives and/or legal guardians, reminding them that at any time, if they wished, they could leave the study, without this affecting their treatment in any way.
Statistical methodThe main endpoints of the present study were changes recorded in the criteria that define the metabolic syndrome.
For the statistical procedure, parametric tests were used in cases where the sample followed a normal distribution, and non-parametric in the rest, using the SPSS® programme. The level of significance was set at p<.05 for all tests.
As the most relevant methods, firstly, the χ2 test can be highlighted as a method to assess the statistical significance of changes between visits in qualitative terms (appearance or disappearance of alterations at the physical, analytical and hormonal level) for each of the diagnostic criteria within the metabolic syndrome, in patients treated with different antipsychotics; secondly, Student's t test for related data to assess the statistical significance of changes in these variables, in quantitative terms, between visits, in the percentages of analytical values for patients under treatment with different drugs; and thirdly, multivariate analysis to look for predictive factors of progression in the metabolic syndrome.
To process lost data, the methods of observed cases and the last observation were used.
ResultsOf the 75 patients included in the study, 44 were males. The mean age of the sample was 41.63 years (22–75), with 38 patients diagnosed with schizophrenia (50.7%), 25 with bipolar disorder (33.3%) and 12 with schizoaffective disorder (16%). The majority of the sample (85.3% of the patients) followed a psychoeducation programme.
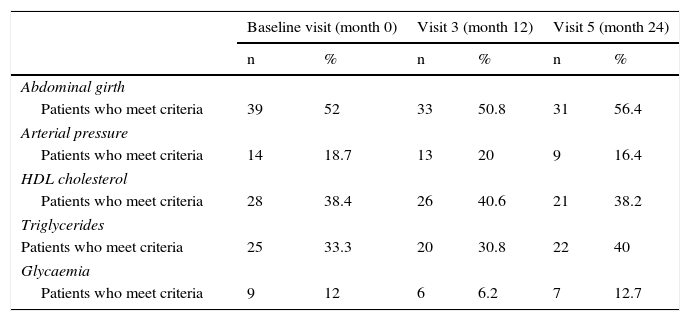
Table 1 shows the mean changes in the physical parameters which constitute the metabolic syndrome (abdominal girth and blood pressure) and biochemical parameters (glucose, HDL cholesterol and triglycerides) at different successive visits (at the baseline visit, month 12 and month 24). The total number of patients was 75 at baseline, 65 at 12 months and 55 at 24 months (except for HDL cholesterol, which was 73 at baseline and 64 at 12 months). In subsequent statistical analyses no significant changes were observed in these physical and biochemical parameters, individually studied throughout the different visits. When analysing the number of metabolic syndrome criteria met by patients throughout the study, 20% of the patients became worse (the number of criteria they met increased), 36% improved (the number of criteria they met decreased) and 44% maintained the same number of criteria.
Descriptive progression of physical and biochemical variables of metabolic syndrome throughout the study.
| Baseline visit (month 0) | Visit 3 (month 12) | Visit 5 (month 24) | ||||
|---|---|---|---|---|---|---|
| n | % | n | % | n | % | |
| Abdominal girth | ||||||
| Patients who meet criteria | 39 | 52 | 33 | 50.8 | 31 | 56.4 |
| Arterial pressure | ||||||
| Patients who meet criteria | 14 | 18.7 | 13 | 20 | 9 | 16.4 |
| HDL cholesterol | ||||||
| Patients who meet criteria | 28 | 38.4 | 26 | 40.6 | 21 | 38.2 |
| Triglycerides | ||||||
| Patients who meet criteria | 25 | 33.3 | 20 | 30.8 | 22 | 40 |
| Glycaemia | ||||||
| Patients who meet criteria | 9 | 12 | 6 | 6.2 | 7 | 12.7 |
Source: National Cholesterol Education Program (NCEP) Expert Panel on Detection, Evaluation and Treatment of High Blood Cholesterol in Adults (Adult Treatment Panel III).7
In the same way, and for the purposes of the studying predictive factors, the final study sample was divided into 3 groups: patients who remained in the same diagnostic group (presenting or not metabolic syndrome from baseline to the end of the study), with a total of 82.7% classified in this group; patients who, throughout the study, developed metabolic syndrome, this group totalling 4% of the sample; and patients where the metabolic syndrome disappeared during the study. This third group totalled 13.3% of the sample.
After this division of the sample, a multivariate regression analysis was run, taking appearance or disappearance of metabolic syndrome during the study as a dependent variable and introducing different physical, biochemical and hormonal parameters as independent variables.
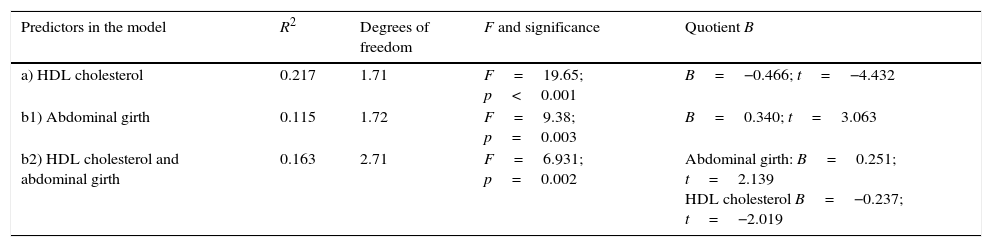
Thus, by introducing abdominal girth, HDL cholesterol, triglycerides, glucose, SBP, DBP, weight, BMI, TSH and PRL as independent variables, it was observed that the variable that could be considered as a predictor for change in the metabolic syndrome was HDL cholesterol at the baseline visit (a in Table 2).
Predictors of metabolic syndrome progression. Multivariate regression analysis on metabolic syndrome criteria and other physical and hormonal parameters and progression of 2-year metabolic syndrome.
| Predictors in the model | R2 | Degrees of freedom | F and significance | Quotient B |
|---|---|---|---|---|
| a) HDL cholesterol | 0.217 | 1.71 | F=19.65; p<0.001 | B=−0.466; t=−4.432 |
| b1) Abdominal girth | 0.115 | 1.72 | F=9.38; p=0.003 | B=0.340; t=3.063 |
| b2) HDL cholesterol and abdominal girth | 0.163 | 2.71 | F=6.931; p=0.002 | Abdominal girth: B=0.251; t=2.139 HDL cholesterol B=−0.237; t=−2.019 |
a) Dependent variable: progression of metabolic syndrome at 2 years. Independent variables: abdominal girth, HDL cholesterol, triglycerides, glucose, systolic blood pressure, diastolic blood pressure, body mass index (BMI), thyroid stimulating hormone and prolactin.
b) Dependent variable: progress of metabolic syndrome at 2 years. Independent variables: abdominal girth, HDL cholesterol, triglycerides, glucose, systolic blood pressure, diastolic blood pressure.
And after running a further analysis, this time analysing only parameters that were part of the diagnostic criteria of the metabolic syndrome (abdominal girth, HDL cholesterol, triglycerides, glucose, SBP and DBP) as independent variables, we found as predictors both HDL cholesterol and abdominal girth at the baseline visit (b1 and b2 in Table 2).
Once these analyses had been completed, a secondary analysis was run on these parameters, obtaining statistical significance, both in abdominal girth and HDL cholesterol.
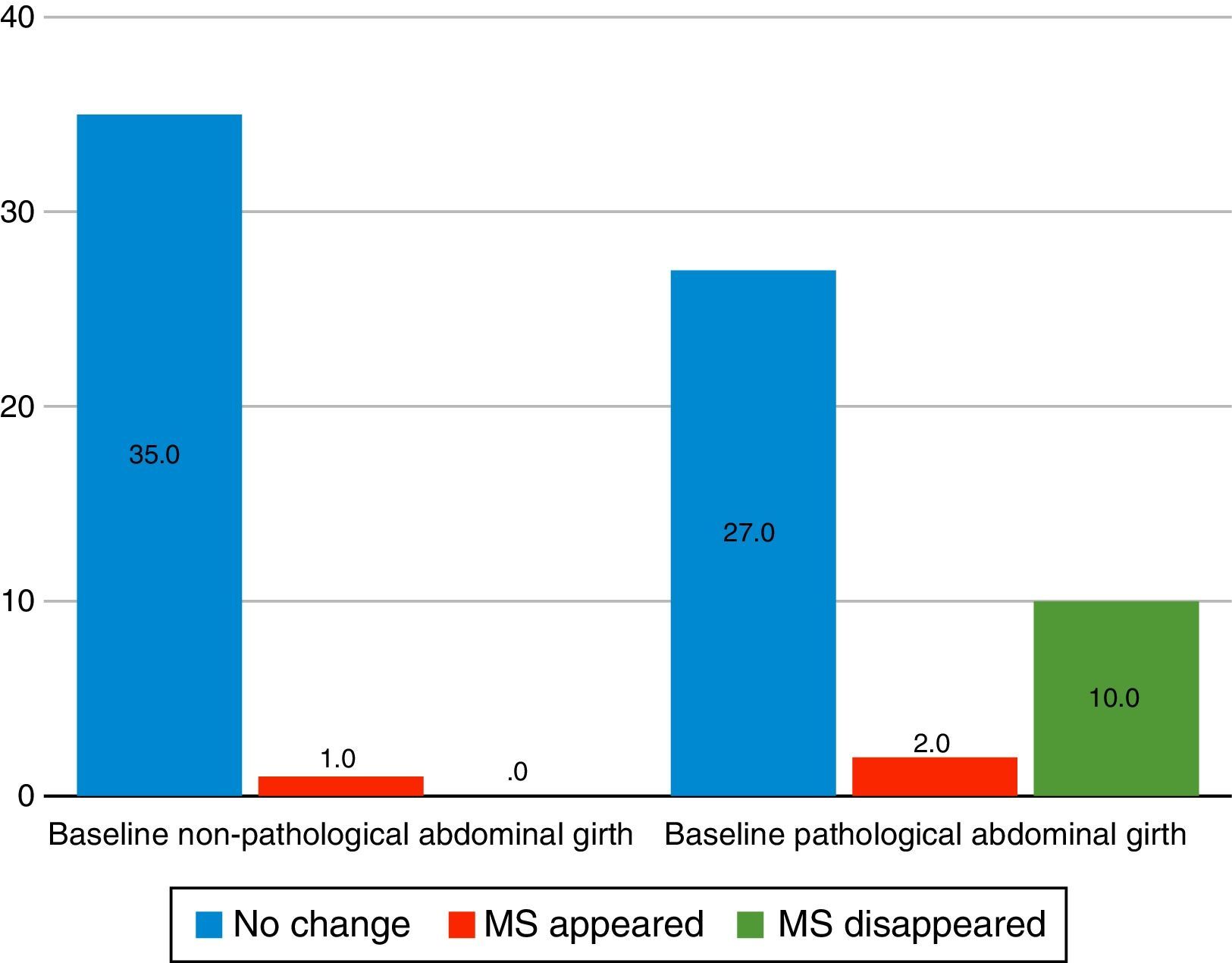
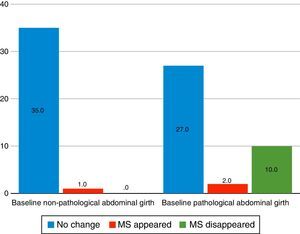
Abdominal girthAfter analysing with χ2, it was observed that patients with poorer scores at the beginning of the study were more likely to improve during it, so that out of the 39 patients who presented pathological scores for abdominal girth (according to ATP III7 criteria) at the beginning of the follow-up, in 10 the metabolic syndrome disappeared during the study, in 2 it appeared, and in 27 the diagnosis did not change (p=0.004, χ2=11.26, gl=1.74). When studying this by gender, it was seen that there were still significant differences in males (p=0.009, χ2=9.51, gl=1.43), but not in females (p=0.089, χ2=2.90, gl=1.30) (Fig. 1).
Variation of the 2-year metabolic syndrome (MS) as a function of baseline abdominal girth. Source: National Cholesterol Education Programme (NCEP) Expert Panel on Detection, Evaluation and Treatment of High Blood Cholesterol in Adults (Adult Treatment Panel III).7
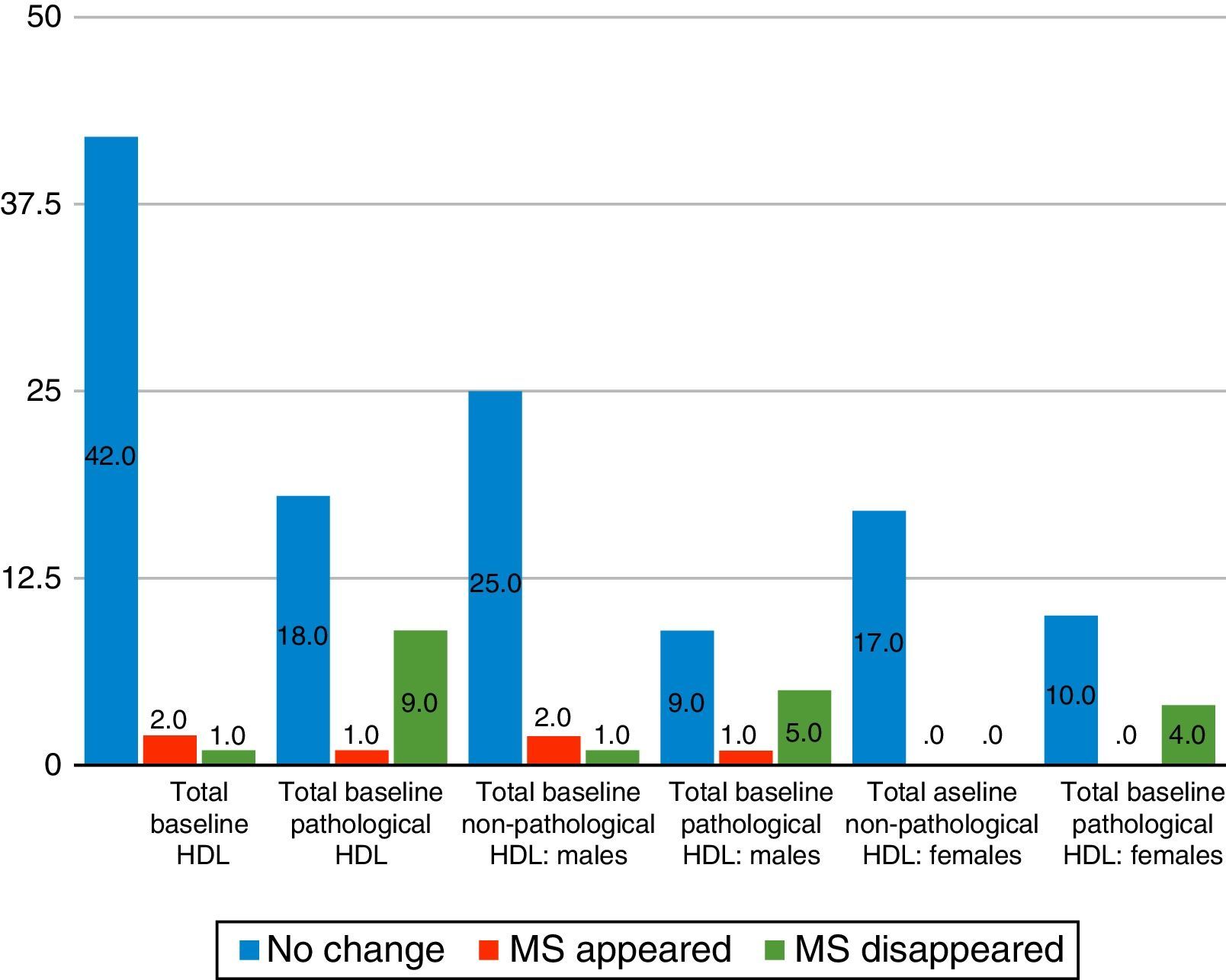
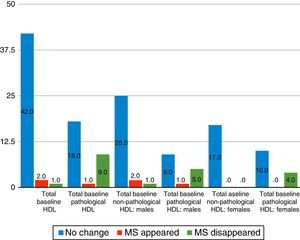
When HDL cholesterol levels were analysed with χ2 levels, it was observed that, with poorer initial scores, the greater the probability of final improvement, so that of the 28 patients with abnormal HDL cholesterol levels (according to ATP III criteria) at baseline follow-up, in 9 cases the metabolic syndrome disappeared, one case developed it and in 18 cases the diagnosis did not vary. This was significant both at the global level (p=0.001, χ2=13.08, gl=1.72) and in its differentiation by sexes (males p=0.022, χ2=7.26, gl=1.42; women p=0.018, χ2=5.58, gl=1.30) (Fig. 2).
Variation of 2-year metabolic syndrome (MS) as a function of HDL cholesterol. Source: National Cholesterol Education Programme (NCEP) Expert Panel on Detection, Evaluation and Treatment of High Blood Cholesterol in Adults (Adult Treatment Panel III).7
Statistical analysis enables us to conclude that the baseline abdominal girth (Wilks lambda p=0.013) and baseline HDL cholesterol levels (Wilks lambda p=0.000) in our sample were the parameters that appeared to be most important, over and above the rest of the diagnostic criteria which constitute the metabolic syndrome, as predictive factors in long-term progression.
DiscussionThe diagnostic parameters of the metabolic syndrome (abdominal girth, blood pressure, triglycerides, HDL cholesterol and glucose) did not present statistically significant changes at 2 years of follow-up in our sample. This fact concurs with the data in the literature,8–11 which confirms stabilisation of the different factors in the metabolic syndrome over the period during which treatment with atypical antipsychotics was maintained, after decompensation in its initial phases.
De Hert et al.12 argue that the introduction of atypical antipsychotics may induce cardiovascular and metabolic changes, such as obesity, glycaemic changes, dyslipidaemia and metabolic syndrome, associated with increased risk of type 2 diabetes mellitus and cardiovascular risk.4 In the same vein, Chadda et al.,13 present a review of the literature on the metabolic syndrome and each of its diagnostic criteria in patients diagnosed with schizophrenia with no previous antipsychotic treatment, detecting an increase in the prevalence of the metabolic syndrome in these patients when treated with antipsychotics in short-term studies. This data is consistent with Khalil's studies in 2013.14
However, Gentile,8 in a review of the literature, adds that in the long-term studies the differences in weight gain seen between different treatments with atypical antipsychotics became less marked. In the same vein, Gebhardt et al.,9 Kinon et al.,10 and McIntyre et al.,11 report that accelerated weight gain in the initial months of treatment may eventually stabilise over time. This is consistent with the results of this study for weight and metabolic syndrome changes.
This stabilisation in our sample may be influenced by our patients’ treatment regime at the Day Hospital, which involved close follow-up with individual and family support and a psychosocial approach with psychoeducation (received by 85.3% of the sample at the time of inclusion). The follow-up on these psychoeducational programmes, which have been shown to be effective in different studies, such as Amiaz et al.,15 may have influenced the absence of significant changes in the parameters of the metabolic syndrome throughout the study, halting what in the literature is considered its usual progression,12–14 at least in the initial stages of treatment.
In addition, as we have already mentioned, in our sample, HDL cholesterol and abdominal girth appeared to be predictors of long-term development of the metabolic syndrome, so that the poorer the initial values, the greater the probability of long-term improvement.
This data contrasts with part of the current literature, as it has been described that a higher BMI, both personally and in the family during the first stages of the disease, predicts worse long-term progression of the metabolic syndrome in treatment with atypical antipsychotics, as commented by Gebhardt et al.,9 and there are some authors who have recently related these 2 components of the metabolic syndrome (HDL cholesterol and abdominal girth) specifically with an increase in cardiovascular risk, especially in patients over 55 years of age (Saloojee et al.).16 However, there are references in the literature, some of these at more advanced stages of the disease, concerning an inverse correlation between the initial parameters and their later progression, as in the article on weight gain by Cortés et al.17 where the association between the increase in BMI with atypical antipsychotics and the initial BMI turned out to be negative, as supported by Lipkovich et al.,18 and Gentile,19 concurring with our results. However, the comparison with our study is relative, since the patients’ stage of progression was totally different. Most of the literature consulted10,14,16 focuses on the early stages of the disease, while our group of patients had full symptoms, with maintenance treatment already in place for some time.
Our results coincide with the point made by Cornier et al.20 to the World Health Organisation when it concluded that, although the metabolic syndrome is to be considered as an educational concept, its use is practically limited as a diagnostic tool, stating that the importance of the concept of metabolic syndrome is that it offers an opportunity to encourage patients to make lifestyle changes that may mitigate the risks of future cardiovascular and metabolic events.21
Taking into account these findings, it would be necessary to consider the reason why patients with worse HDL cholesterol levels and initial abdominal girth were the ones who most improved over the long term, if only because they were the cases that had greatest capacity to Improve or, on the contrary, this was due, in most of our sample, to psychoeducational programmes. In this case it Is important to re-emphasise the need to implement this type of comprehensive programme in the care of patients with severe mental illness, to prevent and attenuate the problems derived from treatment with atypical antipsychotics, as supported by the studies by Sugawara et al.22 and CRESSOB.23
This study should not conclude without pointing out some of its strengths and weaknesses.
Thus, as limitations, it is firstly worth noting the sample size of the study, which prevents adequate comparison between the actions of the different atypical antipsychotics on metabolic syndrome.
Another limitation would be derived from the absence of a control group and the particular characteristics of the sample group (patients on maintenance treatment with an atypical antipsychotic, on a comprehensive programme with psychopharmacological, psychological and psychosocial treatment; control of somatic problems, with support at both individual and family level, integrated within psychoeducational programmes, health education, treatment compliance, and hygiene and dietary measures, etc.). Our findings cannot therefore be generalised to include young people with early episodes of schizophrenia or patients treated with combination antipsychotics; or even psychotic patients on maintenance treatment in the community.
In addition, follow-up losses, although common in any prospective study, and which we have attempted to study as far as possible using the last observation technique, may also imply a potential bias for the assessment of patients who complete the control period. The cause would be a possible overestimation of side effects in patients on treatment with the best tolerated antipsychotics.19
Another possible methodological limitation derived from the use of other adjuvant treatments, that may increase the risk of developing metabolic and cardiovascular changes, was at least partially ruled out in the analysis of the different results obtained.
As a strong point, we should stress the particular characteristics of the sample, as previously mentioned. Although these may limit generalising the results across the board, in our opinion, they open a way forward, making it possible to approach psychotic patients with long-term atypical antipsychotic treatment through comprehensive programmes to control the physical factors involved in the metabolic syndrome, thus avoiding progressive development and, at least, not worsening the burden of disease which, in itself, is associated with schizophrenia and other serious mental illnesses.
In addition, the paucity of long-term studies in patients receiving maintenance therapy with atypical antipsychotics in monotherapy enhances the value of this study, since, as noted above, most studies are usually short-term and run at early stages of the disease, despite the type of treatment they are based on.
At the present moment, with the results obtained and the relevant literature reviewed, the data is inconclusive, it being therefore necessary to run future studies to be able to ascertain the risks that antipsychotic treatment entails. Also required is further research into the determinants of metabolic risk in these diseases, as well as the pathogenic potential of the different antipsychotics for metabolic syndrome, each of the factors it is composed of; and other anthropometric, analytical and hormonal factors. This is necessary to reach a level of excellence in clinical practice based on ethical principles,24 scientific evidence and precision psychiatry.25
Ethical disclosuresProtection of human and animal subjectsThe authors state that the procedures followed conformed to the ethical standards of the committee on responsible human experimentation and in agreement with the World Medical Association and the Declaration of Helsinki.
Confidentiality of dataThe authors state that they have followed their centre's protocols on the publication of patient information.
Right to privacy and informed consentThe authors have obtained the informed consent of the patients and/or subjects referred to in the article. This document is in the possession of the correspondence author.
Conflict of interestsThe authors have no conflicts of interest to declare.
Please cite this article as: Franch Pato CM, Molina Rodríguez V, Franch Valverde JI. Síndrome metabólico y antipsicóticos atípicos. Posibilidad de predicción y control. Rev Psiquiatr Salud Ment (Barc). 2017;10:38–44.