We systematically review factors associated with the presence of psychological distress or common mental disorders in migrant populations. Articles published between January 2000 and December 2014 were reviewed and 85 applying multivariate statistical analysis were selected. Common mental disorders were significantly associated with socio-demographic and psychological characteristics, as observed in large epidemiological studies on general populations. The probability of common mental disorders occurrence differs significantly among migrant groups according to their region of origin. Moreover, traumatic events prior to migration, forced, unplanned, poorly planned or illegal migration, low level of acculturation, living alone or separated from family in the host country, lack of social support, perceived discrimination, and the length of migrants’ residence in the host country all increase the likelihood of CMD. In contrast, language proficiency, family reunification, and perceived social support reduce such probability. Factors related with the risk of psychiatric morbidity among migrants should be taken into account to design preventive strategies.
Se revisan sistemáticamente los factores asociados a la presencia de malestar psicológico o trastornos mentales comunes en poblaciones migrantes. Se revisaron los artículos publicados entre enero de 2000 y diciembre de 2014, de los que se seleccionaron 85 que aplicaban análisis estadísticos multivariantes. Los trastornos mentales comunes se asociaban significativamente a características sociodemográficas y psicológicas, lo mismo que se observa en grandes estudios epidemiológicos de poblaciones generales. La probabilidad de trastornos mentales comunes aumentó significativamente entre grupos de migrantes, además de por la región de origen, por los siguientes factores: sucesos traumáticos previos; migración forzosa, escasamente planificada o ilegal; bajo nivel de aculturación, vivir solo o separado de la familia en el nuevo país, falta de apoyo social, discriminación percibida y tiempo transcurrido en el nuevo país. Para diseñar estrategias preventivas se ha de tener en cuenta los factores asociados al riesgo de morbilidad psiquiátrica en poblaciones migrantes.
The study of common mental disorders (CMD) among migrant populations addresses two well-known and opposing phenomena: the healthy-immigrant vs the migration-morbidity hypotheses. The healthy-immigrant perspective (primarily considered as mental health in this review), is supported mainly by studies carried out in Canada1–6 and in the U.S.,7–12 and asserts that migrants have a significantly lower risk of any psychiatric disorder than their Canadian-born or US-born counterparts. Some authors1,10,13 suggest that people who are healthier and better educated are more likely to emigrate. Yet, the probability of a lower risk of psychiatric disorder is not the same for all migrant groups.1,10,11,14 Diverse factors such as initial health status, age, sex, marital status, language skills, region of birth, experiences of discrimination,15 the acculturation process7,8 and the duration of residence in the host country1,9 may produce over time a decline in an initially healthy migrant status.
In contrast to North American research on the subject, numerous studies carried out mainly in Europe find higher rates of CMD among migrants as compared with non-migrants. In Germany,16 CMD prevalence was significantly higher in migrants from Poland and Vietnam as opposed to the non-migrant population. In The Netherlands17 and Belgium,18,19 migrants from Muslim countries had a higher prevalence of CMD than non-migrants. In Sweden, the probability of CMD among migrants (born in other European or non-European countries) doubled that of Swedish-born subjects.20 In Norway,21 the immigrants from low and middle income countries have a higher risk of mental health problems compared to Norwegian-born subjects. In the EMPIRIC (Ethnic Minority Psychiatric Illness Rates in the Community) study,22 the prevalence of CMD was significantly higher in Irish and Pakistani men aged 35–54 years, as well as in Indian and Pakistani women aged 55–74 years, as opposed to White individuals of the same age and sex. Another study in the U.K.23 confirmed a higher prevalence of depressive disorder in Pakistani women living in an inner city area when compared to White European women in the same area, but found no difference among men. In Austria,24 migrants from Eastern Europe had a higher prevalence of CMD than Austrian-born individuals. Several studies in Spain find that migrants, principally those from Latin America, have worse mental health than Spanish-born.25–29 Moreover, studies in Israel find that the prevalence of CMD among former Soviet Union (FSU) migrants was significantly higher than among their Israeli-born counterparts.30,31 In China, the prevalence of psychological symptoms in rural-to-urban migrant workers was significantly higher than in the Chinese general population, according to a meta-analysis including 48 cross-sectional studies.32 In Australia, migrants also reported poorer mental health than their Australian counterparts.33,34
Both hypotheses (healthy-immigrant vs the migration-morbidity) may hold true and, at any rate, are not mutually exclusive. As we have recognized in a previous paper,29 it is necessary to consider the prevalence of CMD in the country of origin of the migrants in order to verify each hypothesis. On the other hand, there is extensive research about the different factors associated with the risk of psychiatric morbidity in migrants, including individual characteristics (i.e., age, sex, world region of origin, marital status), factors surrounding the migration process (i.e., reason for migrating, acculturation, language proficiency) or those having to do with the social and occupational environment in the host country. Since migrants are a vulnerable group in any population, it is fundamental to analyze the different factors that can contribute either to the maintenance (an even to the enhancement) or to the deterioration of their mental health. Therefore, the objective of this study was to answer the following question through a systematic review of original research and previous meta-analyses: What are the factors associated with the presence of CMD in migrant population across the world? The information obtained can, in turn, assist in the design of effective preventive strategies.
MethodTo achieve the above objective, we identified systematically articles focused on CMD and migrants, published between January 2000 and December 2014 and included in the PubMed, Scopus, and PsycINFO databases. A combination of the codes “migrant(s)”, “immigrant(s)” or “migration” with keywords such as “common mental disorders,” “mental distress,” “mental health”, “psychological distress,” “psychiatric morbidity,” “depressive disorders” and “anxiety disorders,” was used. We included epidemiological studies written in English, French or Spanish, reporting on the different factors associated with the presence of CMD among migrants. Our selection was not restricted to any country or world region. Articles about the risk of schizophrenia and other psychoses in migrants were not included because their prevalence is lower and because, considering their nature, research on this topic would require different specific review efforts. We understood the concept of CMD as proposed by the National Institute for Health and Care Excellence (NICE) in Great Britain, which includes depression, generalized anxiety, panic, obsessive-compulsive, post-traumatic stress and social anxiety disorders (http://www.nice.org.uk/guidance/cg123). Furthermore, the etiology of CMD is multicausal so their outcome may involve numerous and different types of variables; for this reason, only epidemiological studies applying multivariate analysis were included. The title and abstracts of all articles were independently reviewed by two researchers. After excluding studies that did not match the above selection criteria, 86 articles were examined, including 72 cross-sectional, 9 longitudinal and 1 cross-sectional and partly longitudinal; in addition 4 meta-analytical studies were included.
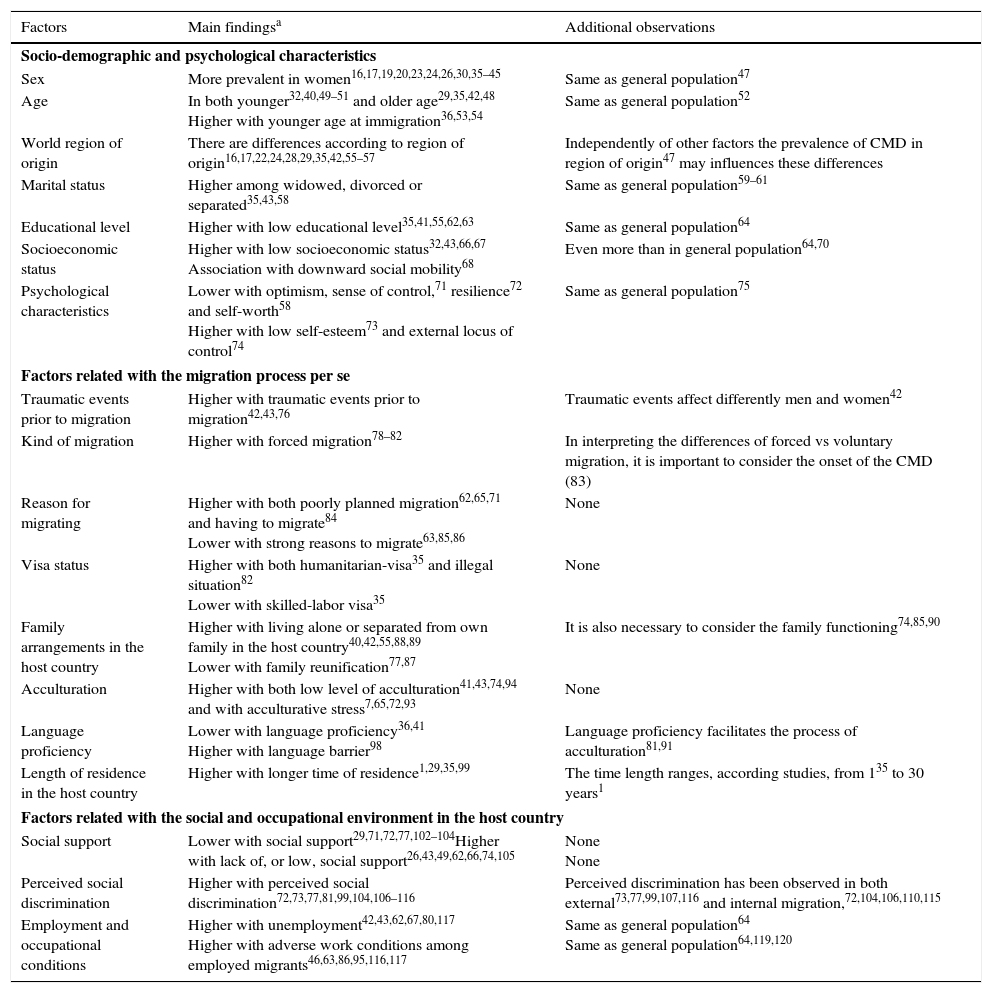
ResultsThe different factors associated with the presence of CMD in migrants, described in the 86 articles, were grouped into: (1) individual socio-demographic (sex, age, world region of origin, marital status, educational level, socioeconomic status) and psychological characteristics; (2) factors surrounding the migration process such as reason(s) for migration, events occurring before to migration, visa status, family arrangements in the host country, acculturation processes, language proficiency and length of residence in the host country; and (3) factors related to the social and occupational environment in the host country, including social support vs social discrimination, and employment and occupational conditions. A summary of the results is shown in Table 1, and a detailed account of all 86 studies is presented in on-line supplementary Table 2.
Summary of factors associated with the presence of psychological distress or common mental disorders among migrants.
| Factors | Main findingsa | Additional observations |
|---|---|---|
| Socio-demographic and psychological characteristics | ||
| Sex | More prevalent in women16,17,19,20,23,24,26,30,35–45 | Same as general population47 |
| Age | In both younger32,40,49–51 and older age29,35,42,48 Higher with younger age at immigration36,53,54 | Same as general population52 |
| World region of origin | There are differences according to region of origin16,17,22,24,28,29,35,42,55–57 | Independently of other factors the prevalence of CMD in region of origin47 may influences these differences |
| Marital status | Higher among widowed, divorced or separated35,43,58 | Same as general population59–61 |
| Educational level | Higher with low educational level35,41,55,62,63 | Same as general population64 |
| Socioeconomic status | Higher with low socioeconomic status32,43,66,67 Association with downward social mobility68 | Even more than in general population64,70 |
| Psychological characteristics | Lower with optimism, sense of control,71 resilience72 and self-worth58 Higher with low self-esteem73 and external locus of control74 | Same as general population75 |
| Factors related with the migration process per se | ||
| Traumatic events prior to migration | Higher with traumatic events prior to migration42,43,76 | Traumatic events affect differently men and women42 |
| Kind of migration | Higher with forced migration78–82 | In interpreting the differences of forced vs voluntary migration, it is important to consider the onset of the CMD (83) |
| Reason for migrating | Higher with both poorly planned migration62,65,71 and having to migrate84 Lower with strong reasons to migrate63,85,86 | None |
| Visa status | Higher with both humanitarian-visa35 and illegal situation82 Lower with skilled-labor visa35 | None |
| Family arrangements in the host country | Higher with living alone or separated from own family in the host country40,42,55,88,89 Lower with family reunification77,87 | It is also necessary to consider the family functioning74,85,90 |
| Acculturation | Higher with both low level of acculturation41,43,74,94 and with acculturative stress7,65,72,93 | None |
| Language proficiency | Lower with language proficiency36,41 Higher with language barrier98 | Language proficiency facilitates the process of acculturation81,91 |
| Length of residence in the host country | Higher with longer time of residence1,29,35,99 | The time length ranges, according studies, from 135 to 30 years1 |
| Factors related with the social and occupational environment in the host country | ||
| Social support | Lower with social support29,71,72,77,102–104Higher with lack of, or low, social support26,43,49,62,66,74,105 | None None |
| Perceived social discrimination | Higher with perceived social discrimination72,73,77,81,99,104,106–116 | Perceived discrimination has been observed in both external73,77,99,107,116 and internal migration,72,104,106,110,115 |
| Employment and occupational conditions | Higher with unemployment42,43,62,67,80,117 Higher with adverse work conditions among employed migrants46,63,86,95,116,117 | Same as general population64 Same as general population64,119,120 |
CMD can affect both men and women migrants. According to numerous studies,16,17,19,20,23,24,26,30,35–45 the probability of experiencing CMD is higher among migrant women compared with men, although two of the studies, one performed in China46 and the other in Spain,28 yielded opposite findings.
The sex differences for CMD among migrants can be partially explained by the different risk or protective factors affecting women and men, and that vary according to the premises of each study and ethnic group(s) under consideration. For example, FSU migrant women in Israel37 scored higher on more specific psychosocial stressors (family problems, inappropriate climatic conditions, anxiety about the future, poor health status, and uncertainty about the present life situation), while men scored higher on protective factors for immigration-related distress (number of reasons for immigration, commitment to the host country, and job adequacy). The same study37 showed that sex mediates the effects of psychosocial risk factors on the migrant's experience. A Norwegian study showed that the social integration of the migrant, measured by visits from friends born in the host country, was a significant protective factor against psychological distress for migrant men but not so for women.42 In turn, migrant women living in a neighborhood with no/low social deprivation in the São Paulo (Brasil) metropolitan area44 showed a higher probability of active anxiety disorder than migrant men under the same conditions.
Ethnicity may also assist in the explanation of sex differences. Among non-institutionalized African Americans in the U.S., women had almost twice the rate of major depressive disorder than their men peers; but among non-institutionalized Caribbean blacks, women had a lifetime rate of major depressive disorder comparable to that of men, which may be due, according to the authors, to employment and educational opportunities that migration to the U.S. allows to Caribbean women.45 Among migrant workers in Shanghai, China,46 being married and experiencing financial/employment difficulties were associated with poor mental health in men but not in women. The authors46 argue that cultural values regarding work and family welfare in Chinese society may weigh more heavily on men, particularly if they are married. Among Chinese migrant workers, most males are married, whereas the majority of females are single: it follows that married men experience a great deal more stress than single women. Moreover, current migration trends in China encourage women in rural areas to leave their villages and seek personal improvement and achievement, eventually enhancing their mental health through increased self-esteem, sense of accomplishment, etc.46 Conversely, some authors argue that the better mental health among Moroccan women migrant in The Netherlands17 or in Spain,28 compared to men, might be explained by their traditional family roles, i.e. child care, domestic tasks, etc. From another perspective, the gap between actual educational level and job qualifications was a risk factor for psychological distress among migrant Bolivian men in Spain, but not so among women.28
In summary, the probability of CMD is generally found to be higher among migrant women than migrant men, as reflected in numerous epidemiological studies in general populations of several countries and reported in a 1980–2013 systematic review and meta-analysis.47 As pointed out, such sex differences among migrant populations can be traced to various psychosocial factors as well as cultural and family values.
AgeCMD have been found to be associated with the migrant's age in both, the older29,35,42,48 and the younger age32,40,49–51 brackets. This finding is strongly demonstrated by the WHO's World Mental Health Survey published in 2007.52 For instance, scores of psychological distress in older (age 60–86) FSU migrants in Israel48 appear to be significantly higher than in middle-aged or young migrants. Similarly, older age is a predictive factor of psychological distress for both migrant women and men in Australia35 and among migrant women in Norway.42 Other studies,32,40,49–51 however, in line with the findings of the WHO'S survey,52 show that younger migrants are not exempt of mental disorders. Moreover, Thai migrant men in Israel49 showed an increased risk of psychological distress that grew with age up to 35 years, the level of stress declining thereafter. A strong association between migration and first episode of any depressive or anxiety disorder was likewise reported among young Mexican immigrants (aged 18–25) in the U.S.50; however, the same study demonstrated a decline, with age, in the risk of any depressive or anxiety disorder. Higher scores of psychological distress have similarly been observed among migrant adolescents in Germany compared with German-born adolescents.40 Second-generation Irish children growing up in Britain experienced high levels of psychological morbidity, which was accounted for by psychological distress among their mothers.51
Thus, it seems clear that age at the time of immigration can influence the mental health of the migrants. Younger age at immigration has been associated with increased risk of current mood, anxiety36,53 and substance use disorders.53 This finding is not universal however, as, inversely internal migration at age 30 or higher is associated with a lower probability of depressive symptoms compared to non-migrants, according to a study in Peru.54
World region of originThe immigrant's world region of origin can be a predictive factor of CMD. In the EMPIRIC study,22 the prevalence of CMD was significantly higher among Irish, Pakistani and Indian migrants as opposed to British White individuals of the same age and sex, while in migrant groups of Black Caribbean's and Bangladeshis there was no such difference. In Amsterdam,17 the prevalence of depressive and/or anxiety symptoms differed among groups, from 18.7% among Turkish migrants to 9.8% in Moroccans, and a lowest 1.2% in the Surinamese/Antillean group; after adjusting for sex and socioeconomic status, only Turkish women showed a significantly higher prevalence of depressive and anxiety disorders compared to the native Dutch women. In Germany,16 Vietnamese experienced worse mental health than Polish migrants, and both groups had a significantly higher prevalence of anxiety and depression than German women.
In Australia,35 migrants coming from Western and developed countries, when compared with those who migrated from Asian countries, were less likely to report psychological distress. The authors of this study35 suggest that psychological distress is in part due to the language barrier. However, as some studies in Spain28,29,55 find significant differences in the probability of suffering CMD (higher in Latin American migrants compared to Spanish-born individuals), the language barrier cannot be considered an explanatory factor of this heterogeneous pattern; such role could perhaps be attributed to the developmental level28 and to the prevalence of mental disorders in the country of origin.29 In this context, a study in Sweden56 found that migrants born outside Europe had more risk of developing depression than Sweden-born and other migrants born in Scandinavia or other parts of in Europe; according to the authors, the non-European immigrants may have been more often exposed to social and economic disadvantages, but the risk of depression remained significant even after adjustment for socioeconomic status, education and other demographic variables.
Traumatic events prior to migration, as war and political conflicts in the country of origin, can influence the mental health differences found across migrant groups. For instance, migrant women from the Middle East (Iran and Turkey) living in Oslo42 showed a higher distress score than other migrant groups of the same sex. The authors argued that hardships experienced in the home countries, mostly conflict zones, could explain the greater risk of psychological distress. In Austria,24 first- and second-generation women from Eastern Europe (particularly from the former Yugoslavia) had a greater probability of suffering dysphoric disorders than Austrian-born subjects, an association not observed among first- and second-generation women who migrated from Western European countries.
Seasonal affective disorder and country of birth appear also associated among migrant men in Oslo57: the probability of suffering from this disorder is much (and significantly) higher in originals from Iran, Pakistan and Vietnam than in those from Sri Lanka; however, the differences among women are not significant.
That CMD among migrants is associated with the world region of origin, is a finding quite in line with those of Steel et al., 1980–2013 systematic review and meta-analysis47 of studies in the general population of 63 countries. There is evidence of consistent regional variation in the prevalence of CMD. For instance, one-year and lifetime prevalence was lower from North and South East Asian and Sub-Sahara-African countries than among those from other regions including English-speaking countries that showed the highest estimates.47
Marital statusMost migration studies report poorer mental health among the widowed, divorced or separated when compared with those married35,43 or never married,58 a finding similar to those comparing individuals with and without a couple partner.55 For instance, among migrants in Australia35 and in Sweden,43 the widowed, divorced or separated, as opposed to married, were more likely to show psychological distress35 or low well-being and anxiety/depression,43 independently of sex and other demographic characteristics. Among male workers migrating from rural to urban areas in China,58 the widowed or divorced have four times more probability of suffering from mental disorders than those never married. In contrast, another study among rural-urban migrants in China46 showed that male subjects who are married have poorer mental health than those who are single, but this correlation was not found among women. This finding might again be explained, at least in part, by cultural values that place a great deal of pressure on men to provide for the welfare of their families in the city.46
The finding that non-married status – in particular widowed, divorced or separated– is associated with psychiatric morbidity among migrant populations is similar to observations from epidemiological studies of the general population.59–61 In a multinational study of mental disorders and marital status,61 several mental disorders, including affective and substance use disorders, were associated with lower likelihood of marriage and higher likelihood of divorce among people aged 18 or more.
Educational level and socioeconomic statusLow educational level is associated with CMD in migrant groups35,41,55,62,63 as is the case in large epidemiological studies of general populations.64 Nevertheless, among migrant Mexican farm workers in the U.S., high educational level was significantly related to high anxiety levels, a finding possibly due to a sense of unachieved goals.65
A lower socioeconomic status (SES) appears to be clearly associated with deficient mental health in migrant populations.32,43,66,67 Similarly, a meta-analysis about the relationship of CMD with migration and social mobility68 described a higher probability of occurrence among migrants who experienced downward social mobility than among those who were upwardly mobile or experienced no changes in their socio-economic position. In the general population, people of lower SES show higher frequencies of CMD,69 even though other studies have found no relation64 or rather an inverse association between CMD and income.70
Psychological characteristicsThe almost intuitive assumption that the psychological characteristics of the immigrants can have, according to their nature, a positive (protective) or negative (risk) impact on their mental health, has been repeatedly confirmed.58,71–74 To some extent, this observation is similar to the correlations of psychotic and non-psychotic syndromes with a variety of pre-morbid personality traits.75 Optimism, sense of control71 and personal resilience72 were protective factors against depressive symptoms among mainland Chinese immigrants into Hong Kong. Similarly, a high self-worth was a protective factor of mental disorder in male rural-urban migrant workers in continental China.58 Contrariwise, a low self-esteem was associated (approaching significance) with depressive symptoms in indigenous Mexican migrants in the U.S.73 In this latter study, a perceived discrimination of the migrant is associated with low self-esteem which, in turn, may lead to increased levels of depressive symptoms. In addition, external locus of control has been associated with psychological distress among FSU migrants in Israel.74
Factors surrounding the migration processTraumatic events prior to migrationTraumatic events prior to the migration process itself can definitely affect the mental health of the immigrants. Among older Somali refugees in Finland,76 exposure to traumatic events prior to migration was associated with both depressive symptoms and psychological distress. Furthermore, traumatic events (pre- or post-migration) seem to impact men and women differently. In men who migrated from different regions of the world to Oslo, Norway,42 lifetime traumatic experiences such as torture, imprisonment and direct witnessing of combat and war actions were associated with psychological distress, independently of negative life events due to the refugee migrant status per se in the host country. It is remarkable, however, that within the migrant women the same lifetime traumatic experiences were not associated with worse mental health, whereas recent negative life events showed a significant relationship with psychological distress in both men and women.42 Similarly, Iraqi and Iranian migrants in Sweden,43 who had experienced traumatic events prior to migration had a higher probability of suffering anxiety/depression than those not exposed. In contrast, a study among Latino immigrants to the U.S.77 did not find an association of depressive symptoms with traumatic events prior or during the migration process itself, unless high poverty levels can justifiably play a chronically traumatizing role in the migrant's life.
Kind of migration and reason for migratingThe kind of migration (voluntary or forced) and the reason for migration (in the case of voluntary migration) may both influence the mental health of migrants. For instance, a longitudinal study among people who were displaced by the construction of the Three Gorges Dam in China, found a causal relation between forced migration and depression.78 A systematic review and meta-analysis based on studies published from 1990 to 2007,79 found that the prevalence of depression and anxiety was lower in labor migrants when compared with refugee migrants. Some, but not all, subsequent studies confirm this relation. In Oru (Nigeria), refugees were three times more likely than non-refugees to have poor mental health.80 Among Latino immigrants to the U.S., acculturative stress was lower for those who migrated voluntarily than for those who had to leave their country of origin as refugees.81 In the Swiss canton of Zurich,82 labor migrants did not show significant difference in symptoms of depression with Swiss residents, while refugees, illegal migrants and asylum seekers (those whose claims for asylum had been accepted) did, with odds ratios of 4.5, 6.9 and 25.2 respectively; these different groups of migrants showed other differences among them in both anxiety symptoms and post-traumatic stress disorder.
In interpreting the differences among subjects with different migration status, it may be important to consider the onset of the mental disorder.83 Rasmussen et al.83 found that both Latino and Asian refugee migrants in the U.S., compared with voluntary migrants, had a higher probability of onset of post-traumatic stress disorder before migration, but the risk of these problems is equalized over post-migration time. According to the authors, the principal implication of this finding is that preventive mental health strategies must be a crucial aspect in the management of all kinds of migrant populations.
Regarding the reason for migration, among Chinese who migrated to Hong Kong,71 a poorly planned migration was associated with depressive symptoms, after controlling for moderating variables such as optimism, sense of control and social support. In male Irish migrants to London, poorly planned migration was a significant predictor of depression, even when controlling for depression prior to migration.62 Among migrant Mexican farm workers in the U.S., a low level of participation in the decision to live as a migrant farm worker was a predictor of anxiety.65 In parallel, among Latino migrants in the U.S.,84 “having to migrate” was associated with increased psychological distress for Puerto Rican and Cuban women compared with their Mexican counterparts who reported “wanting to migrate”. This association was not observed among migrant men. However, in this study84 unplanned migration was significantly associated with a poor physical health among all Latina women.
In contrast, Asian migrants in the U.S. with multiple strong reasons to migrate or with adequate migratory planning were less likely to manifest psychological distress and psychiatric disorders in the past 12 months than those without clear goals or with poorly planned migration.85 Among female Chinese migrants in Shanghai and other cities in China there was better mental health if the reasons for migration revolved around financial and material gains86 and a better future for self and children.63
Visa statusIn older migrants,35 the type of visa was a significant predictor of future psychological morbidity. Migrants with a humanitarian visa were more likely to suffer higher psychological distress than those with a family-reunion type, and migrants with a skilled-labor visa were more likely to report lower levels of psychological distress than those who migrated with a family-reunion visa. This finding, according to the authors, can be attributed to the beneficial effect of a paid work on the psychological well-being. Nevertheless, in a recent study among immigrant women in Spain,29 neither residence nor work permit were significantly associated with CMD.29
Family arrangements in the host countryIn this area, the results of our review are contradictory. Family reunification of migrants is a protective factor from mental disorders.77,87 It would follow that living alone or separated from the family in the host country is associated with a higher psychiatric morbidity among migrants40,42,58,88,89 but this finding has not been unanimous.29,35 On the contrary, living alone has also been associated with a likelihood of reporting lower levels of psychological distress, particularly among older migrants35; among migrant women in Spain,29 living arrangements with their own family, as opposed to living alone, was associated with more probabilities of CMD, a fact that the authors interpret as a possible result of stressful conditions in the everyday family life. Among South Asian migrants in Canada,36 having children younger than 12 years in the household was directly associated with good-excellent (vs poor-fair) self-perceived mental health. Not surprisingly, poor family functioning in general is associated with psychological distress,74,85 and good family functioning with better mental health.90
AcculturationAcculturation, or the process of adaptation of a migrant to the culture of the host country, is conditioned by factors such as the similarity of the two cultures, the receptivity of the host culture, the age of the migrant (adaptation is better in pre-adolescents), individual psychological characteristics (personality or willingness to migrate would influence the adaptation process), and SES.91–93 A low level of acculturation,41,43,74,94 i.e. the maintenance of the migrants’ traditional beliefs49 and subsequent social isolation95 are associated with CMD. An acculturative process dominated or interfered with by a rigid keeping of norms and values of the original culture has been associated with mental health problems including anxiety, depression, hostility, somatic problems, and disaster-related intrusions and avoidance reactions among migrants in The Netherlands affected by a natural disaster, an outcome absent in the non-affected immigrants.96
Acculturation can produce stress, and high acculturative stress is associated with anxiety,65 mood disorders and drug abuse or dependence7 in Mexican migrant farm workers in the U.S.; and with depressive symptoms in migrant Chinese employed in the U.S.93 or in Hong Kong.72 Furthermore, acculturative stress has a mediating role in the relationship between acculturation and depression, so that more acculturated migrants experience less acculturative stress, and less depression, according to a study among Korean migrants in the U.S.97
Language proficiencyProficiency in the language of the host country facilitates the process of acculturation in migrant populations.81,91 Among Latino immigrants in the U.S.,81 acculturative stress was independently and inversely correlated with English proficiency, and directly with native (Spanish) language proficiency. Among Turkish migrants in Germany,41 proficiency in German was inversely correlated with depressive symptoms. In South Asian migrants in Canada, using either English or French when carrying out the Canadian community health survey, was associated with decreased odds of “extremely stressful self-reported life stress”.36 Non-Latino migrants in the U.S. confronting a language barrier, when compared with U.S. citizens without a language barrier, showed more unhappiness, anxiety, and depression, especially in the first 10 years of their life in the host country.98 In contrast, and paradoxically, among Latinos in the U.S.,14 the risk of CMD was significantly higher among those with excellent or good English language proficiency than those with poor or fair English language proficiency; this risk remained after adjusting for education. Based on related research pieces, the authors14 point out that proficiency in English, though being a marker of assimilation into a host culture, may also reflect structural characteristics such as greater job demands influencing health outcomes. Finally, a study24 analyzing the influence of language competence on depression and anxiety among migrants in Austria, did not find a reliable association.
Length of residence in the host countryThe length of residence in the host country can influence the migrants’ mental health, although the actual figures vary in different studies.1,29,35,99 Among older migrants to Australia,35 the level of psychological distress increased throughout a year of follow-up. Among migrant women in Spain, length of stay, independently of age, was a significant predictor of being diagnosed with any psychiatric disorder.29 In contrast, among Arab migrant women in Germany, having lived less than 15 years in the host country was significantly associated with psychological distress as opposed to a longer stay time.99 Among Asian and African migrants in Canada,1 independently of age and other demographic variables, several cohorts had lower rates of depression than the Canadian-born population, except that of migrants with 30 years or more of residence, who showed higher rates.
Other studies do not find conclusive associations in this regard.14,24,74 A study on FSU migrants in Israel74 found that, after 5 years in the host country, the level of psychological distress observed in migrants did not decrease and rather remained high. In a large sample of Latino migrants living in the U.S.,14 with lower probability of psychiatric disorders than the U.S.-born Latinos, length of stay was not significantly associated with psychiatry morbidity when controlling for age, a finding shared by the Austrian study24 cited before.
Complementary to these findings is the fact that the incidence rate of new psychiatric outpatient consultations among migrants in Segovia, Spain has declined from 2001 to 2008, in contrast with the increase observed among Spaniards,100 although this variation is heterogeneous across ICD-10 diagnostic groups. An increase in treated prevalence of mental disorders has been also observed along those years in the general population of Asturias, Spain which the authors101 attribute, at least in part, to population aging.
Factors related with the social and occupational environment in the host countrySocial supportIt is well known that an adequate social support can reduce the negative impact of migration on the mental health of migrants.29,71,72,77,102–104 For example, among Greek students in the U.K., both the quality of social support and the number of close friends were inversely correlated with the degree of “culture shock”.102 Among first-generation immigrant Latino youth in the U.S., the support from both family and teachers was inversely associated with the presence of depression.103 The same occurred in new migrants from mainland China into Hong Kong71; moreover, social support reduced the harmful impact of poor migration planning on depressive symptoms. In the same sample, a 1-year follow-up104 found that both social support and “neighborhood collective efficacy” (social cohesion and informal social control) moderated the effect of perceived discrimination on the depressive symptoms of migrants. Family resilience72 and perceived support from both family and friends29 may also mitigate the negative impact of migration. A good example of this is the case of Latino immigrants in the U.S.,77 among whom both, familism (a strong connection and loyalty to family members, an especially important characteristic of this ethnic group) and effective social support reduced the probability of depressive symptoms. Contrariwise, low social support26,43,49,62,66,74,105 during post-migration, is associated with the presence of CMD in migrant populations.
Perceived social discriminationThe disposition and actual behavior of the host society members toward immigrants and the latter's perception of such set of attitudes definitely affect their mental health status.72,73,77,81,99,104,106–116 In effect, feeling negatively about being a migrant was a predictor of psychological distress among Arab women in Germany.99 Among Latino migrants in the U.S., perceived discrimination – measured by racial/ethnic treatment distinctions,73,77 racial problems in the neighborhood77, and discrimination in goals, in expressions of discomfort or anger or in health care107 – was associated with depressive symptoms73,77 or with a low sense of psychological well-being.107 The relationship between perceived discrimination among migrants and the presence of CMD has also been observed in internal (within a state, country or continent) migration groups. In new migrants from mainland China into Hong Kong,104 perceived discrimination was associated with depressive symptoms; at 1-year follow-up this association remained after adjusting for the presence of depressive symptoms at baseline assessment. A subsequent study of the same population72 found that the relationship between perceived discrimination and depressive symptoms remained after controlling for both personal and family resilience that had shown a protective effect on depressive symptoms. Other studies in China,106,110 including one analyzing school discriminatory experiences among children of migrant workers,115 confirm this association.
Some authors108,109 have demonstrated that discrimination experienced by migrants increases the expectation-reality discrepancy which, in turn, influences the relationship between discrimination experience, mental distress and quality of life in general. Moreover, the perceived discrimination is influenced by different socio-demographic factors73,106,107,111,112,114 which can, as well, modify the strength of the relationship between perceived discrimination and psychological distress. Race/ethnicity influences this process; for instance, the health care discrimination among migrants in the U.S. is higher for Africans than for Mexican Americans and other Latinos.107 Indigenous cultural identification increases the level of perceived discrimination.73 Migrants with higher educational levels perceive more discrimination than less educated ones.114 Economic difficulties,112 low social class,111 and low-income country of birth111 also increase the level of discrimination perceived by migrants. Higher levels of family cohesion moderate (weaken) the effect of perceived discrimination on depressive symptoms as shown by migrant women in Taiwan.106
Employment and occupational conditionsUnemployment among migrant populations is associated with the presence of CMD,42,43,62,67,80,117 a finding similar to those from large epidemiological studies of general populations.64 Student or economically inactive migrants also tend to report higher levels of psychological distress than those currently employed.35 Among employed migrants, the odds of poor mental health are higher in both unskilled and skilled workers than among professionals.80 Individual factors – such as interpersonal tensions and conflicts,46,86 job dissatisfaction,118 coping strategies117 – and working conditions – i.e., feelings of discrimination and lack of respect at work,95 overwhelming daily work hours, and financial and employment difficulties or deficits46,63 – are associated with the occurrence of CMD. In addition, specific occupational–environmental conditions can affect the mental health of migrant workers. Among Thai migrant agricultural workers in Israel, psychological distress was associated with exposure to pesticides,49 a finding that combines subjective perceptions and neurobiological mechanisms such as the association between anti-cholinesterase pesticides and depression.119
In short, unemployment and work conditions of those employed affect the mental health of migrant groups, as it also happens among different types of workers in the general population.64,120,121
DiscussionThe objective of this study was to review the factors associated with the presence of CMD among migrant populations. After reviewing 86 multivariate-analytic studies (published between January 2000 and December 2014), the overall conclusion is that the presence of CMD among migrant populations is directly or inversely associated with a variety of factors. In short, the socio-demographic and psychological characteristics of migrants as well as aspects of work conditions can affect the mental health of migrants in the same way as non-migrants. Moreover, the world region of origin of migrant is associated with the presence of CMD, so that the likelihood of any CMD varies according to region of origin of migrant.16,17,22,24,28,29,35,42,55–57 The strength of this relationship is supported by a 1980–2013 systematic review and meta-analysis that included results of 26 high-income countries and 37 low- or middle-income countries.47
Another important correlation that can explain the differences in mental health across migrant groups24,42 is that of traumatic events prior to migration (i.e., wars and political conflicts in the country of origin) and occurrence of CMD.24,42,43,76 Likewise, perceived social discrimination by migrants has a negative impact on their mental health.72,73,77,81,99,104,106–116 As mentioned, race/ethnicity,107 indigenous cultural identification,73 high educational level,114 economic difficulties,112 low social class111 and low-income country of birth111 increase the level of perceived discrimination. Social support, active coping strategies, group identification116 and family cohesion106 could help buffering the negative impact of perceived discrimination on the mental health of migrants. It follows that a multicultural education and competence on the side of the general population could contribute decisively to diminish or totally eliminate the perceived discrimination of migrants.
Future longitudinal studies about the mental health of migrants are required, particularly those devoted to analyzing the association of world region of origin with the presence of CMD in migrants; if significantly different rates between migrants from different regions are found, it would be important to examine in depth the nature (psychological, socio-cultural, clinical or neurobiological) of such distinctions and whether these differences remain over time. To the best of our knowledge, only one study35 has investigated, from a longitudinal perspective, the influence of world region of origin on CMD in migrants: those coming from Western and developed countries, when compared with those who migrated from Asian countries, were less likely to report psychological distress, a relation that remained at 12-month follow-up. Inter-country, inter-continental and inter-hemispheric comparative studies are, thus, mandatory.
More studies are also needed to determine the impact of the length of residence by migrants in the host country, on the presence of CMD. These studies could clarify whether CMD remain over time, improve, or deteriorate even further the quality of life of migrants. The public health relevance of this approach cannot be underestimated. As mentioned above, some studies find an association between the length of residence of migrants in the host country and CMD,1,29,35,99 but only one35 finds that this association remains at 12 months of follow-up.
The diversity of assessment instruments, both structured diagnostic interviews and self- administered questionnaires (as can be seen in supplementary Table 2), can be considered a limitation of the present review. However, to exclude studies based on questionnaires would have meant to lose a huge source of information on the subject, although an inclusion requirement for each article was the use of multivariate statistics.
On the other hand, in future epidemiological studies about CMD in the general population, it would be fundamental to include the “migration status” variable. In short, migration status and country or world region of origin, besides socio-demographic variables, are very important rubrics in this area of inquiry. Moreover, the co-morbid occurrence (and close inter-relationship at bio-psycho-socio-cultural levels) of physical and mental diseases adds a relatively new and enormously important research dimension.
In this era of impressive technological advances and global health and mental health implications, the study of migrating populations within and outside countries or continents has become a crucial research need and objective. National government agencies and international organizations must devote, both individually and in close and well coordinated collaborative initiatives, adequate financial and human resources to these efforts. The implications for prevention programs and better, sophisticated management strategies are also evident.
ConclusionThe above considerations lead to the conviction that in diagnosing CMD and evaluating the mental health care of migrants across the world, it is important to carefully consider a multitude of contributing factors including socio-demographic, psychological and cultural features, world region of origin, characteristics of the migration process, experiences in and with the host country, and acculturation. Knowledge in this area could guide policy makers, service providers and clinicians to improve the mental health care of migrants and the world population as a whole through adequate detection, management and prevention strategies.122
Conflict of interestsThe authors have no conflict of interests to declare.
Common mental health disorders. Identification and pathways to care. Mayo 2011. NICE clinical guideline 123 [accessed 7 Sep 2015]. Available from: http://www.nice.org.uk/guidance/cg123
Please cite this article as: Jurado D, Alarcón RD, Martínez-Ortega JM, Mendieta-Marichal Y, Gutiérrez-Rojas L, Gurpegui M. Factores asociados a malestar psicológico o trastornos mentales comunes en poblaciones migrantes a lo largo del mundo. Rev Psiquiatr Salud Ment (Barc). 2017;10:45–58.
- Léalo en español
- Descargar PDF
- Bibliografía
- Material adicional