After the outbreak of the COVID-19 was considered a global pandemic in March 2020, the state of alarm was declared in Spain. In this situation, health professionals are experiencing high levels of stress due to the overload of work the pandemic is generating and the conditions in which they are working. The aim of this study was to evaluate the factors that can destabilize the mental health of these professionals in our context.
Materials and MethodsThe sample was composed of 421 health professionals. The data were gathered by an online questionnaire sent to them by e-mail. The DASS-21 was used to assess anxiety, stress and depression, and the EAI to measure sleep difficulties. In addition, other descriptive variables that could be related to psychological symptomatology were collected from the sample.
ResultsThe results show that the COVID-19 pandemic has generated symptoms of stress, anxiety, depression and insomnia among health workers, with higher levels among women and older professionals. Some factors such as having been in contact with the virus or fear at work, triggered greater symptomatology.
ConclusionsIn this critical situation, professionals are in the front line and therefore, are directly exposed to certain risks and stressors. This contributes to the development of diverse psychological symptoms. Consequently, it is recommended to offer them psychological help in order to reduce the emotional impact of the COVID-19, and thus, to ensure not only the mental health of our health professionals, but also the adequate care they provide.
Tras declararse en marzo de 2020 el brote por el virus COVID-19 pandemia mundial, se decretó el estado de alarma en España. En esta situación, el personal sanitario está viviendo altos niveles de estrés por la sobrecarga de trabajo y las condiciones de este. El objetivo del presente estudio fue evaluar los factores que pueden desestabilizar la salud mental de dichos profesionales en nuestro contexto.
Materiales y métodosLa muestra estuvo compuesta por 421 profesionales de la salud. Los datos se recogieron mediante un cuestionario online que se les envió a través del correo electrónico. Se empleó el DASS-21 para evaluar las variables de ansiedad, estrés y depresión, y la EAI para medir las dificultades con el sueño. Además, se recogieron otras variables descriptivas de la muestra que podrían estar relacionadas con estos niveles de sintomatología psicológica.
ResultadosLos resultados muestran que la pandemia del COVID-19 ha generado entre el personal sanitario síntomas de estrés, ansiedad, depresión e insomnio, con mayores niveles entre las mujeres y profesionales de más edad. Variables como haber estado en contacto con el virus o el miedo en el trabajo, desencadenaron una mayor sintomatología.
ConclusionesEn esta situación crítica, el colectivo de profesionales se sitúa en primera línea, por lo que está expuesto directamente determinados riesgos y estresores. Esto contribuye a que desarrollen sintomatología psicológica diversa. Consecuentemente, se recomienda ofrecerles ayuda psicológica para reducir el impacto emocional del COVID-19, y asegurar así, no sólo su salud mental, sino también el adecuado cuidado que dispensan.
With the current COVID-19 pandemic, healthcare professionals face very intense work stressors. These include prolonged job shifts, work overload, strict safety instructions and measures, the constant need for concentration and surveillance, the lack of protective equipment and reduced social contact, as well as having to perform tasks for which many professionals have not been prepared.1,2
This situation of stress puts both their physical and mental health at risk. It may produce symptoms of anxiety, depression or post-traumatic stress disorder.1,3 It is also possible that this stress can cause vicarious traumatisation stemming from compassion towards the patients that they are treating.4
In previous research on epidemics, adverse psychological reactions were seen among male and female healthcare workers. For example, such reactions were found in the severe acute respiratory syndrome (SARS) outbreaks,5–7 the Middle East respiratory syndrome (MERS) upsurge8 and now in the face of COVID-19.9 These studies showed that the workers feared catching the disease and infecting their relatives, friends and colleagues,7 and that they felt insecure and stigmatised.5,7 This could lead to long-term psychological consequences.4 In addition, as has been demonstrated in the context of other epidemics, stress and anxiety among the staff directly impact their health and indirectly affect the healthcare system when a staff member fails to go to work because of such stress and anxiety.10
Female and male healthcare professionals in China have shown an incidence of severe anxiety of 2.17%, moderate anxiety of 4.78% and mild, of 16.09%.11 According to another study, severe levels of anxiety, depression and stress in healthcare personnel in China seem to be especially high (depression 16.5%, anxiety 28.8% and stress 8.1%)12 in comparison with the results of another study in India and Singapore (severe levels of depression 5.3%, of anxiety 8.7% and of stress 2.2%).13
Another aspect that can be altered by work overload is sleeping. Sleep habits have been shown to be a key indicator of health,14 given that besides improving efficiency and the way of handling patients, getting enough good-quality sleep maintains optimum immunological function to prevent infections.15 A recent study16 carried out in China in light of the current pandemic revealed that the individuals with better sleep quality suffer less post-traumatic stress.
The complex relationship among these variables has to be added to all of this. On the one hand, there is evidence that stress functions as a trigger for the symptoms of anxiety and depression in young healthcare personnel.17 In the context of the COVID-19 pandemic, both work overload and the fear of possible infection might be causing and increasing the levels of stress.18 In addition, the incidence of these symptoms (for example, anxiety) is generally greater in female medical staff than in males.10 As for age, a recent study19 on the psychological effects of the pandemic on the Chinese population found that the youngest individuals (less than 35 years old) were at greater risk of suffering anxiety and depression.
At present, in the face of COVID-19 expansion in Spain, there is a lot of concern about these issues. This is especially true about the psychological adjustment and recovery of healthcare staff that treat patients having this virus.20 However, at the moment, there are barely any studies on the matter. Bearing all of this in mind, the objective of this study was to assess the levels of stress, anxiety, depression and sleep alteration among healthcare personnel that treat patients exposed to the COVID-19 virus in 2 autonomous communities: the Basque Country (País Vasco; CAPV is the acronym in Spanish) and Navarra. Other descriptive variables in the sample that might be related with these levels of psychological symptomatology were also studied.
Material and methodsThis study was performed with a total sample of 421 healthcare professionals in the Department of Health in the CAPV and Navarra autonomous communities. All the participants were active professionals working in various public and private hospital centres in these 2 communities. The sample was obtained using a non-probabilistic snowball sampling method. The minimum age was 18 years old and the maximum, 74 years old. Of these individuals, 338 were women (mean age = 42.6; standard deviation [SD] = 10.2) and 83 were men (mean age = 47.4; SD = 13.4). As for place of work, 66.7% (n = 281) worked in Bizkaia, 16.6% (n = 70) in Gipuzkoa, 10.2% (n = 43) in Araba and 6.5% (n = 27) in Navarra.
A questionnaire was designed, containing socio-demographic data (sex and age) and questions as to whether the healthcare professionals lived with someone that had a chronic disease, if they had had contact with people infected with the COVID-19 virus and if they experienced fear when they went to work. In addition, they were asked about their perception of whether the population was adhering to the COVID-19 lockdown.
Depression was assessed with the Spanish version of the Depression Anxiety and Stress Scale-21.21 This consists of 21 items with 4 options for replying (from 0 = “this has never happened to me,” to 3 = “this has happened to me often or most of the time”) that are grouped in 3 factors: depression, anxiety and stress. For this study, the cut-off points of Portocarrero AN and Jiménez-Genchi A22 were used: no symptomatology, and mild moderate, severe and extremely severe symptomatology. As for the reliability of the scale, Cronbach’s alpha coefficient for the scales was α = 0.76 for depression, α = 0.82 for anxiety and α = 0.75 for stress.
The Spanish version of the Athens Insomnia Scale (AIS) was used to ascertain the severity of insomnia symptoms.23 This is an instrument designed to quantify sleep difficulty based on the International Classification of Diseases (ICD-10). It is made up of 8 elements; the first 4 refer to quantitative sleep variables, including sleep induction and night-time wakening, final waking up and total length of sleep. The fifth element refers to sleep quality, and the last 3, to the impact of insomnia on day-time performance. The items are scored from 0 to 3; the highest scores indicate the most deteriorated sleep conditions. The total score ranges from 0 to 24 points. In our study, a total AIS score of 6 or more was considered insomnia.23 With respect to scale reliability, the Cronbach alpha coefficient was 0.70.
The study received the approval of the public university in the Basque Country (UPV/EHU is the acronym used in Spain for Universidad del País Vasco/Euskal Herriko Unibertsitatea) (code: M10/2020/055). The healthcare professionals were contacted by email. After we received consent for the participation of the subjects, the answers were gathered using an online questionnaire between 1 and 10 April 2020. In the questionnaire, both the study objectives and the procedure to be followed were explained. For the data gathering, all the requirements established by Organic Law 15/99 on Protection of Personal Data were followed.
The data were analysed using the IBM SPSS Statistics for Windows, Version 25.0 statistical programme (Armonk, NY, USA). Firstly, the frequencies and percentages of the socio-demographic variables. Next, a successive multivariate analysis of the variance (MANOVA) was performed to ascertain the differences among the levels of depression, anxiety, stress and insomnia depending on the socio-demographic variables analysed.
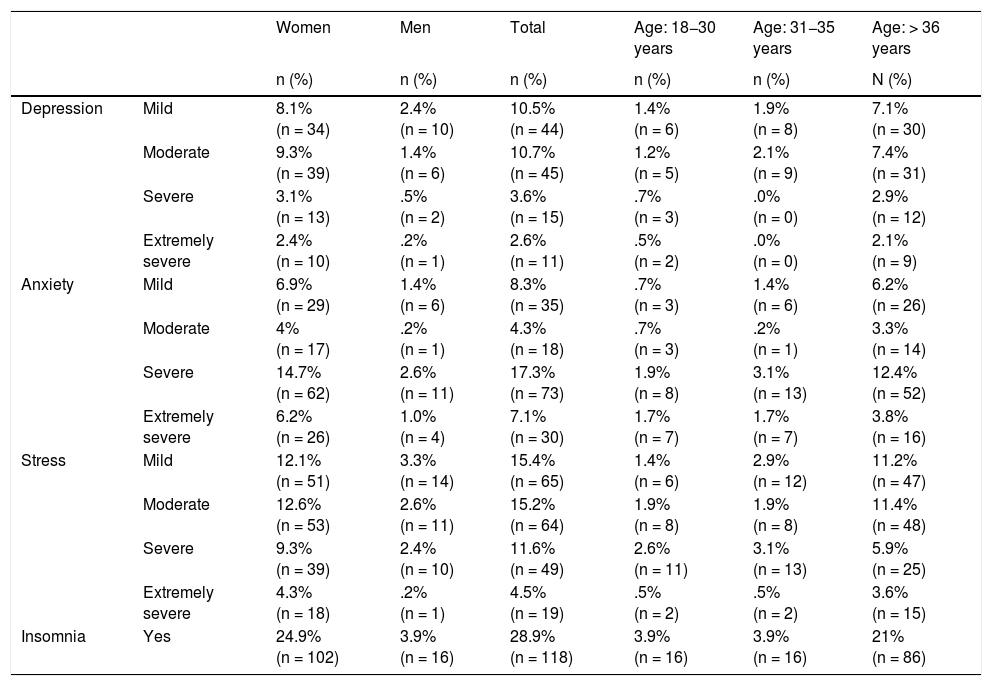
ResultsTable 1 presents the data on prevalence of the subjects that were suffering depression, anxiety, stress and insomnia by the sex and age of the participants. The results were that 46.7% of the participants indicated that they suffered stress; 37%, anxiety; 27.4%, depression; and 28.9%, sleep problems. As for differences by sex, women showed higher levels of anxiety (t [419] = 2.66, P = .008) and stress (t [419] = 2.21, P = .027). The healthcare professionals older than 36 years old showed stress (32.1%), anxiety (25.3%), insomnia (21%) and depression (19.5%) to a greater extent.
Frequencies and rates of healthcare staff that suffer depression (mild, moderate, severe and extremely severe) and insomnia, broken down by sex and age.
| Women | Men | Total | Age: 18−30 years | Age: 31−35 years | Age: > 36 years | ||
|---|---|---|---|---|---|---|---|
| n (%) | n (%) | n (%) | n (%) | n (%) | N (%) | ||
| Depression | Mild | 8.1% (n = 34) | 2.4% (n = 10) | 10.5% (n = 44) | 1.4% (n = 6) | 1.9% (n = 8) | 7.1% (n = 30) |
| Moderate | 9.3% (n = 39) | 1.4% (n = 6) | 10.7% (n = 45) | 1.2% (n = 5) | 2.1% (n = 9) | 7.4% (n = 31) | |
| Severe | 3.1% (n = 13) | .5% (n = 2) | 3.6% (n = 15) | .7% (n = 3) | .0% (n = 0) | 2.9% (n = 12) | |
| Extremely severe | 2.4% (n = 10) | .2% (n = 1) | 2.6% (n = 11) | .5% (n = 2) | .0% (n = 0) | 2.1% (n = 9) | |
| Anxiety | Mild | 6.9% (n = 29) | 1.4% (n = 6) | 8.3% (n = 35) | .7% (n = 3) | 1.4% (n = 6) | 6.2% (n = 26) |
| Moderate | 4% (n = 17) | .2% (n = 1) | 4.3% (n = 18) | .7% (n = 3) | .2% (n = 1) | 3.3% (n = 14) | |
| Severe | 14.7% (n = 62) | 2.6% (n = 11) | 17.3% (n = 73) | 1.9% (n = 8) | 3.1% (n = 13) | 12.4% (n = 52) | |
| Extremely severe | 6.2% (n = 26) | 1.0% (n = 4) | 7.1% (n = 30) | 1.7% (n = 7) | 1.7% (n = 7) | 3.8% (n = 16) | |
| Stress | Mild | 12.1% (n = 51) | 3.3% (n = 14) | 15.4% (n = 65) | 1.4% (n = 6) | 2.9% (n = 12) | 11.2% (n = 47) |
| Moderate | 12.6% (n = 53) | 2.6% (n = 11) | 15.2% (n = 64) | 1.9% (n = 8) | 1.9% (n = 8) | 11.4% (n = 48) | |
| Severe | 9.3% (n = 39) | 2.4% (n = 10) | 11.6% (n = 49) | 2.6% (n = 11) | 3.1% (n = 13) | 5.9% (n = 25) | |
| Extremely severe | 4.3% (n = 18) | .2% (n = 1) | 4.5% (n = 19) | .5% (n = 2) | .5% (n = 2) | 3.6% (n = 15) | |
| Insomnia | Yes | 24.9% (n = 102) | 3.9% (n = 16) | 28.9% (n = 118) | 3.9% (n = 16) | 3.9% (n = 16) | 21% (n = 86) |
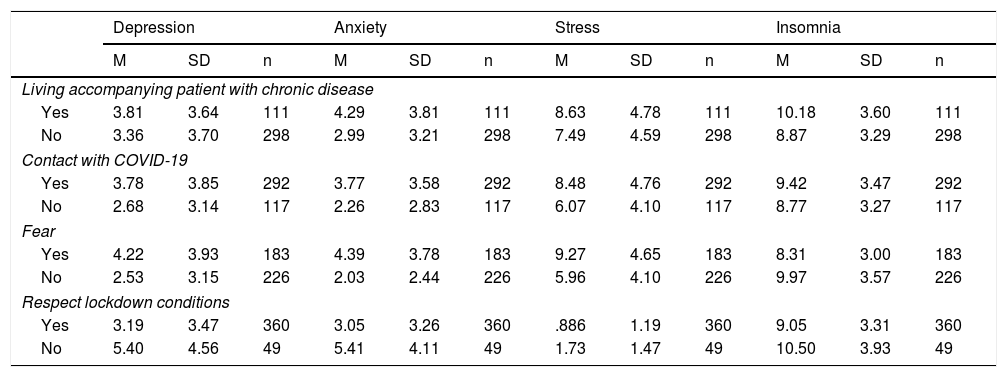
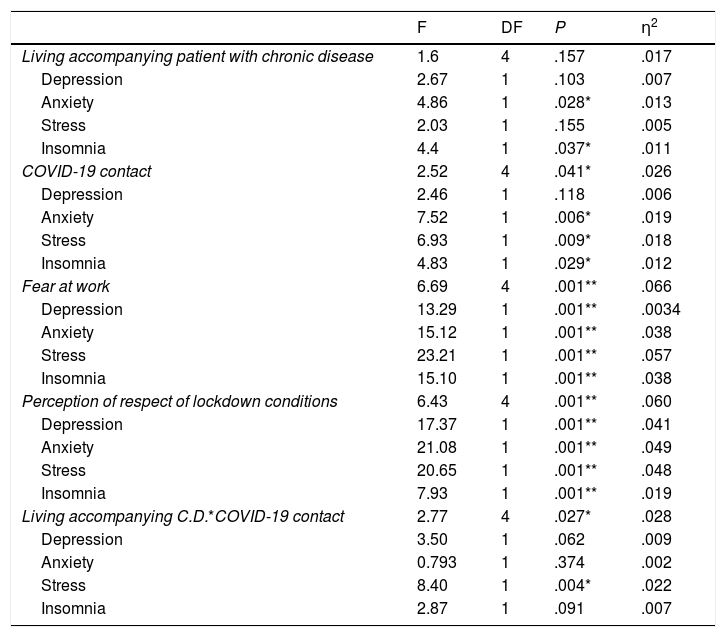
The data gathered from the specific questionnaire revealed that 72.2% of the sample (n = 298) did not live with anyone that had a chronic disease. However, 71.5% (n = 292) had indeed had contact with people infected with COVID-19 and 44.4% (n = 183) indicated that they experienced a fear of contagion. Finally, 88.4% (n = 360) perceived that the population was respecting lockdown regulations. A MANOVA was performed to explore whether these variables were linked to the levels of depression, anxiety, stress and insomnia. Table 2 presents the descriptive results, while the relationships that were statistically significant can be seen in Table 3.
Means (M) and standard deviations (SD) in depression, anxiety, stress and insomnia based on the personal variables gathered.
| Depression | Anxiety | Stress | Insomnia | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| M | SD | n | M | SD | n | M | SD | n | M | SD | n | |
| Living accompanying patient with chronic disease | ||||||||||||
| Yes | 3.81 | 3.64 | 111 | 4.29 | 3.81 | 111 | 8.63 | 4.78 | 111 | 10.18 | 3.60 | 111 |
| No | 3.36 | 3.70 | 298 | 2.99 | 3.21 | 298 | 7.49 | 4.59 | 298 | 8.87 | 3.29 | 298 |
| Contact with COVID-19 | ||||||||||||
| Yes | 3.78 | 3.85 | 292 | 3.77 | 3.58 | 292 | 8.48 | 4.76 | 292 | 9.42 | 3.47 | 292 |
| No | 2.68 | 3.14 | 117 | 2.26 | 2.83 | 117 | 6.07 | 4.10 | 117 | 8.77 | 3.27 | 117 |
| Fear | ||||||||||||
| Yes | 4.22 | 3.93 | 183 | 4.39 | 3.78 | 183 | 9.27 | 4.65 | 183 | 8.31 | 3.00 | 183 |
| No | 2.53 | 3.15 | 226 | 2.03 | 2.44 | 226 | 5.96 | 4.10 | 226 | 9.97 | 3.57 | 226 |
| Respect lockdown conditions | ||||||||||||
| Yes | 3.19 | 3.47 | 360 | 3.05 | 3.26 | 360 | .886 | 1.19 | 360 | 9.05 | 3.31 | 360 |
| No | 5.40 | 4.56 | 49 | 5.41 | 4.11 | 49 | 1.73 | 1.47 | 49 | 10.50 | 3.93 | 49 |
Results of the multivariate and univariate analyses of variance for the symptomatology.
| F | DF | P | η2 | |
|---|---|---|---|---|
| Living accompanying patient with chronic disease | 1.6 | 4 | .157 | .017 |
| Depression | 2.67 | 1 | .103 | .007 |
| Anxiety | 4.86 | 1 | .028* | .013 |
| Stress | 2.03 | 1 | .155 | .005 |
| Insomnia | 4.4 | 1 | .037* | .011 |
| COVID-19 contact | 2.52 | 4 | .041* | .026 |
| Depression | 2.46 | 1 | .118 | .006 |
| Anxiety | 7.52 | 1 | .006* | .019 |
| Stress | 6.93 | 1 | .009* | .018 |
| Insomnia | 4.83 | 1 | .029* | .012 |
| Fear at work | 6.69 | 4 | .001** | .066 |
| Depression | 13.29 | 1 | .001** | .0034 |
| Anxiety | 15.12 | 1 | .001** | .038 |
| Stress | 23.21 | 1 | .001** | .057 |
| Insomnia | 15.10 | 1 | .001** | .038 |
| Perception of respect of lockdown conditions | 6.43 | 4 | .001** | .060 |
| Depression | 17.37 | 1 | .001** | .041 |
| Anxiety | 21.08 | 1 | .001** | .049 |
| Stress | 20.65 | 1 | .001** | .048 |
| Insomnia | 7.93 | 1 | .001** | .019 |
| Living accompanying C.D.*COVID-19 contact | 2.77 | 4 | .027* | .028 |
| Depression | 3.50 | 1 | .062 | .009 |
| Anxiety | 0.793 | 1 | .374 | .002 |
| Stress | 8.40 | 1 | .004* | .022 |
| Insomnia | 2.87 | 1 | .091 | .007 |
C.D. = Patient with a chronic disease.
Our results indicate that the healthcare staff that live accompanied by someone with a chronic disease have greater levels of anxiety (F [1.404] = 4.46, P = .028, η2 = .013) and insomnia (F [1.404] = 4.40, P = .037, η2 = 0.011), although the size of the effect is small. Staff members that have been in contact with people infected with the COVID-19 virus show the greatest levels of anxiety (F [4.404] = 7.52, P = .06, η2 = 0.019), stress (F [1.404] = 6.93, P = .009, η2 = 0.018) and insomnia (F [4.404] = 4.83, P = .029, η2 = 0.012).
The subjects that replied that they experienced fear at work also present greater levels of depression, anxiety and stress. Stress is the dependent variable showing the greatest effect size (F [1.404] = 23.21, P = .001, η2 = 0.057). Next in order are the variables anxiety (F [1.404] = 15.12, P = .001, η2 = 0.038) and depression (F [1.404] = 13.29, P = .001, η2 = 0.034).
All the professionals that feel that, in general, the population is not respecting the measures that have been imposed with respect to lockdown show the greatest levels of depression (F [1.404] = 17.37, P = .001, η2 = 0.041), anxiety (F [1.404] = 21.08, P = .001, η2 = 0.049), stress (F [1.404] = 20.65, P = .001, η2 = 0.048) and insomnia (F [1.404] = 7.93, P = .001, η2 = 0.019)]. All these results are of an intermediate effect size, except for insomnia, which shows a small size. The staff members that have been in contact with people infected with the COVID-19 virus and that live with a patient with a chronic disease show the greatest levels of stress (F [1.402] = 8.40, P = .004, η2 = 0.022), with a small effect size.
DiscussionThe impact of COVID-19 and its implications represent an important challenge for healthcare professionals, who often face a significant work overload, under mentally and psychologically demanding conditions, and with the feeling of having few means and little support available.1,2 Although this type of pandemic has already shown that it gives rise to high levels of various types of symptoms among healthcare staff,9 this reality has not been studied in the context of our country. Consequently, the objective of this study was to assess the differences in symptomatology depending on sex and age, as well as in relation to other relevant sample variables.
The data revealed that a high percentage of healthcare professionals indicated that they suffered symptoms of anxiety, stress, depression and sleep disorders. The prevalence of anxiety, depression and stress found were higher than that of previous studies on COVID-19.12 The severe levels of anxiety reported are even higher than those found in China.11
The study also showed that women suffered higher levels of anxiety, depression, stress and insomnia; the differences were statistically significant for anxiety and stress, in line with previous studies.11,24 The women’s greater tendency to internalise the symptomatology has also been supported by prior studies.25 The primary role of care-giver that women carry out in their homes (for children and parents) might be behind their greater anxiety and stress, due to the fear of contagion. Nevertheless, these results should be put in context, given that somewhat more than 80% of our study sample were women.
With respect to age, in contrast to what has been found in other studies,19 older healthcare professionals (both male and female) revealed the highest levels in all the symptomatology assessed. It is possible that the greater the age, the more probable it is that the participants have families, children and/or parents, under their care. This would increase the pressure of responsibility, the fear of bringing the virus to their homes, etc.
Related to what was expressed in the previous paragraph, it was observed that living with a person that had a chronic disease also increased the levels of anxiety in the study participants, due to the fear of contagion. In addition, the fact that the professionals worked with patients infected with COVID-19 also increased the levels of anxiety, stress and insomnia. And if, in addition to working with patients infected with the COVID-19 virus, the study participants lived with individuals with chronic diseases, their levels of anxiety were even greater. It is evident that the fear of contagion is very much present among the healthcare personnel that participated in the study (44% declared that they were afraid). Fear is a natural response to a threat and COVID-19 is currently being viewed as such. This is because of, to a great extent, the huge knowledge gap that there is about the virus. The lack of knowledge awakens feelings of vulnerability or loss of control, and concerns about personal and family health and about isolation.26
Lockdown and social distancing (together with hygiene measures) are currently the main means of prevention for the population, and an elevated percentage of our participants (88.4%) perceived that citizens were adhering to them. However, the professionals that felt that the population was not following these measures had the highest levels of depression, anxiety, stress and insomnia. If people do not follow prevention measures strictly, the risk of healthcare collapse is greater. That is why healthcare personnel are especially worried about the social responsibility of the citizenship.
Up until now, no studies in Spain have examined the psychological impact of the pandemic on healthcare personnel. This would be the principal strength of our study. The practical implications of the study are also relevant. The psychological impact on healthcare personnel (especially women and older individuals) has to be reduced. To accomplish this, based on the measures that are working well in China,24 we recommend training on COVID-19, strengthening safety measures and guaranteeing the basic needs of the staff (such as food and sleep). Rest areas should be provided and periodic visits by mental health professionals or psychological help by telephone should be facilitated. These services will need to be sustained over some time, because work overload continues and possible cases of post-traumatic stress caused by this pandemic have to be prevented and treated.11
As for the limitations of the study, we should point out that the sample distribution (more than 80% women) means that the results in differences by sex be viewed with a little caution. Likewise, the generalisation of the results is limited, given that this is a non-probabilistic sample in which there might be a certain selection bias: participation was voluntary, so individuals especially impacted emotionally might have participated. Future studies should increase the sample, obtaining a more balanced probabilistic sample with respect to sex and making it extensible to more autonomous communities.
FundingThis study has not received specific funding from organisations in the commercial or public sectors or from non-profit entities.
Conflict of interestsThe authors have no conflicts of interest to declare.
We are grateful for the participation of all the healthcare personnel; without their invaluable help, the study could not have been carried out.
Please cite this article as: Dosil Santamaría M, Ozamiz-Etxebarria N, Redondo Rodríguez I, Jaureguizar Albondiga-Mayor J, Picaza Gorrochategi M. Impacto psicológico de la COVID-19 en una muestra de profesionales sanitarios españoles. Rev Psiquiatr Salud Ment (Barc). 2021;14:106–112.