Previous studies have linked processing speed with social cognition and functioning of patients with schizophrenia. A discriminant analysis is needed to determine the different components of this neuropsychological construct. This paper analyzes the impact of processing speed, reaction time and sustained attention on social functioning.
Material and methods98 outpatients between 18 and 65 with DSM-5 diagnosis of schizophrenia, with a period of 3 months of clinical stability, were recruited. Sociodemographic and clinical data were collected, and the following variables were measured: processing speed (Trail Making Test [TMT], symbol coding [BACS], verbal fluency), simple and elective reaction time, sustained attention, recognition of facial emotions and global functioning.
ResultsProcessing speed (measured only through the BACS), sustained attention (CPT) and elective reaction time (but not simple) were associated with functioning. Recognizing facial emotions (FEIT) correlated significantly with scores on measures of processing speed (BACS, Animals, TMT), sustained attention (CPT) and reaction time. The linear regression model showed a significant relationship between functioning, emotion recognition (p=.015) and processing speed (p=.029).
ConclusionsA deficit in processing speed and facial emotion recognition are associated with worse global functioning in patients with schizophrenia.
Estudios previos han relacionado la velocidad de procesamiento con la funcionalidad y la cognición social de los pacientes con esquizofrenia. Se necesita un análisis más discriminativo de los diferentes componentes de este constructo neuropsicológico. El presente trabajo analiza el impacto de la velocidad de procesamiento, del tiempo de reacción y de la atención sostenida sobre el funcionamiento social.
Material y métodosUn total de 98 pacientes ambulatorios de entre 18 y 65 años con diagnóstico DSM-5 de esquizofrenia, con un período de 3 meses de estabilidad clínica, fueron reclutados. Se recogieron datos sociodemográficos y clínicos, y se midieron: velocidad de procesamiento (Test del Trazo [TMT], codificación de símbolos [BACS], fluidez verbal), tiempos de reacción simple y electiva, atención sostenida, reconocimiento de emociones faciales y funcionalidad.
ResultadosLas medidas que se asociaron con funcionalidad fueron: velocidad de procesamiento (medida solo a través de la BACS), atención sostenida (CPT) y tiempo de reacción electiva (pero no simple). El reconocimiento de emociones faciales (FEIT) se correlacionó de forma significativa con la puntuación en las medidas de velocidad de procesamiento (BACS, Animales, TMT), atención sostenida (CPT) y tiempo de reacción simple. El modelo de regresión lineal mostró una relación significativa entre funcionalidad, reconocimiento de emociones (p = 0,015) y velocidad de procesamiento (p = 0,029).
ConclusionesEl déficit en velocidad de procesamiento y reconocimiento facial de emociones se asocia a peor funcionamiento global en pacientes con esquizofrenia.
Processing speed is a central construct in the field of the cognitive alterations which affect schizophrenia patients.1,2 It has been defined as “the number of correct responses that a person is able to give in a test that requires a series of cognitive operations in a limited execution time.3 The tests that have traditionally been used to measure this capacity include verbal fluidity, the symbol coding test and the Trail Making Test (TMT).4 Some studies have shown that these tests may be valid and efficient indicators of overall cognitive functioning,5 and a poor performance in them has been associated with difficulties in overall psycho-social functioning,6,7 problem solving in everyday life,8 keeping a job9 and social skills.10 On the other hand, sustained attention or vigilance, defined as “the capacity of keep attention focused on a task during a long period of time” has also been shown to deteriorate in schizophrenia.11 Poor performance in tests that evaluate sustained attention such as the Continuous Performance Test [CPT]) seems to be associated with genetic risk factors,12 and it is present in the first stages13 as well as in the later phases of the disease.14
Some laboratory studies have tried to differentiate the most basic units in processing speed, using tests that measure reaction time using simple and elective response paradigms.15 Although they are closely related, reaction time is defined and differentiated from processing speed, as “the time required for a motor response to be initiated following the reception of a stimulus by sense organs, and it is set in the early stage of information processing”.16 The fundamental difference is therefore that its value “is not the time taken by the execution of a response, but rather the time required for the external response to be initiated”.17 Although there are conceptual differences between processing speed and reaction time, very few studies have tried to discriminate between both constructs in schizophrenia.
Lastly, a cognitive domain that has been studied a lot in recent years is emotional processing, a part of social cognition that includes the capacity to identify, facilitate, understand and manager emotions.18 Given its relevance in the field of psychosis, social cognition has been included in the Consensus Battery for the evaluation of schizophrenia in the Measurement and Treatment Research to Improve Cognition in Schizophrenia (MATRICS).19 Several studies have found that schizophrenia patients have a facial emotions recognition and discrimination deficit,14,20 especially those of fear and anger.21,22 Recently it has been suggested that there is a connection between attention processes and emotional processing,23 and this may explain the synergic impact of both cognitive dimensions on functioning.
Our working hypothesis is that reaction time, processing speed and sustained attained are variables which are interrelated but different, and that they have different impacts on the social functioning of schizophrenia patients. The aim of this work is to measure performance in terms of reaction time, processing speed and sustained attained in a group of schizophrenia patients, analysing their different impacts on emotional processing and functioning.
Material and methodStudy designThis is a transversal intragroup study that has the aim of analysing the relationships between reaction time, the capacity for sustained attention and processing speed with measurements of overall functioning and emotional processing in sample of patients diagnosed as schizophrenic.
ParticipantsThe sample was composed of 98 patients aged from 18 to 65 years old, diagnosed as schizophrenic according to the Diagnostic and statistical manual of mental disorders, fifth edition (DSM-5),24 recruited consecutively in 2 mental health hospitals in the Catchment area of Príncipe de Asturias University Hospital (Alcalá de Henares, Madrid). All of the patients were clinically stable and maintained the same pharmacological treatment during the previous 3 months. Patients who fulfilled criteria for other diagnoses were excluded, as were those with moderate to severe pharmacological impregnation data according to the Simpson-Angus scale (due to its potential affect on reaction time), mental backwardness, neurological disease, a history of craneoencephalic injury, a serious medical disease, functional analphabetism, the abuse of psychoactive substances—except tobacco—together with those who refused to take part. The Ethics Committee of Príncipe de Asturias University Hospital approved the evaluation protocol, and all of the participants signed their informed consent document.
Variables and instrumentsClinical evaluation was undertaken using the Schizophrenia Positive and Negative Syndrome Scale (PANSS25; Spanish version26). Anxiety symptoms were measured using the State-Trait Anxiety Inventory (STAI27; Spanish version28). The Simpson-Angus Scale29 (Spanish version)30 was used to detect the presence and severity of Parkinsonian symptoms. Overall functionality was evaluated using the Overall Activity Rating Scale (OARS31,32).
Processing speed was evaluated by measuring performance in 3 tests: (a) A symbol coding subtest (Brief Assessment of Cognition in Schizophrenia [BACS]33); (b) The Trail Making Test [TMT-A]34), and (c) a verbal fluidity test (category: “Animals”35).
Reaction time was evaluated using version 2.0 of the SuperLab pro CEDRUS program.36 This involved the observation of a fixed green circle displayed on a computer screen, responding by pressing the tabulator when a visual stimulus in the form of a red circle appeared (simple reaction time). A figure in the form of a square then appeared at random in the centre, right or left of the screen, so that the letter “z”. “hyphen” or “tab” had to be pressed depending on the position of the said figure (elective reaction time). Capacity for sustained attention or vigilance was evaluated using the CPT test.37
Emotional processing was evaluated using the Facial Emotions Identification Test (FEIT38). This standardised test includes 19 photographs of faces expressing one of 6 basic emotions: happiness, sadness, anger, fear, surprise or shame. The stimuli are shown on a computer screen and the task consists of identifying the emotion expressed by each one.
ProcedureSubjects were evaluated individually by a clinical psychiatrist during approximately 50min in the patient's outpatient hospital. With the aim of minimising variability the neuropsychological tests were administered at similar times of day (from 4 to 6p.m.).
Statistical analysisThe average and standard deviation were used to describe continuous data, and percentages were used for categorical data. The fit of quantitative variables with normal distribution was determined using the Kolmogorov–Smirnov test. To compare the equality of 2 sub-groups within the sample (such as monotherapy versus polytherapy) the Student t-test and Mann–Whitney U test were used, depending on the behaviour of the variables studied. Association between variables was analysed using Pearson's partial correlation coefficient, controlling possible confusion variables (such as age or chlorpromazine equivalents) and then used a multiple lineal regression model. Statistical analysis of the data was undertaken using version 19.0 of the SPSS39 statistical package. The level of significance set for all hypothesis comparison tests was 0.05.
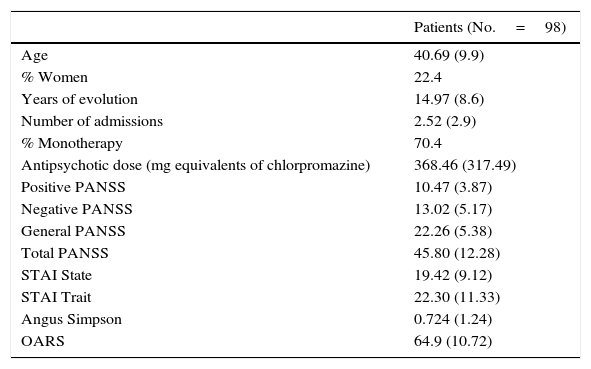
ResultsCognitive variablesThe patients who took part in the study had an average age of 40.6 years old (SD: 9.9) and 22.4% were women (77.6% men). 76.5% were single, 18.4% were married and 6.1% were separated or widowed. In terms of their educational level, 40.8% had primary education, 38.8% secondary education and 18.4% had studied at university. 14.3% were in work, 23.5% were unemployed and 62.2% were retired; 69 patients were treated under monotherapy and 29 under polytherapy. 92.8% of the sample were taking atypical antipsychotic drugs (23.4% paliperidone palmitate; 21.3% risperidone; 20.2% aripiprazol; 18.9% clozapine; 12.1% olanzapine; 5% amisulpride; 3.1% quetiapine; 2% ziprasidone) and 7.2% were taking typical antipsychotic drugs (4.2% haloperidol; 3% fluphenazine decanoate). The clinical characterisation of the sample is shown in Table 1.
Descriptive analysis of the sociodemographic and clinic variables of the sample.
| Patients (No.=98) | |
|---|---|
| Age | 40.69 (9.9) |
| % Women | 22.4 |
| Years of evolution | 14.97 (8.6) |
| Number of admissions | 2.52 (2.9) |
| % Monotherapy | 70.4 |
| Antipsychotic dose (mg equivalents of chlorpromazine) | 368.46 (317.49) |
| Positive PANSS | 10.47 (3.87) |
| Negative PANSS | 13.02 (5.17) |
| General PANSS | 22.26 (5.38) |
| Total PANSS | 45.80 (12.28) |
| STAI State | 19.42 (9.12) |
| STAI Trait | 22.30 (11.33) |
| Angus Simpson | 0.724 (1.24) |
| OARS | 64.9 (10.72) |
Data are shown as averages, standard deviation (SD) and percentages.
In general the patients displayed significantly poorer cognitive performance than normal values (Table 2). Significant relationships were found between cognitive and sociodemographic variables. Although they had the same level of symptoms on the PANSS and equal functionality, the women showed worse processing speed in the TMT (t=−1.991; P=.049) and in the verbal fluidity test (t=2.678; P=.009), as well as a worse simple reaction time (t=−2.278; P=.025). Age was associated with a worse processing time in the TMT tests (P=.533; p=.000), BACS (P=−.425; p=.000), elective reaction time (P=.260; p=.011) and facial emotion recognition (P=−.309; p=.002). Medication is another variable that is related to cognitive performance in some tasks, so that patients under monotherapy showed better sustained attention in the CPT than those who were under polytherapy (2 digits: t=2.723, p=.008; 3 digits: t=3.229, p=.002; 4 digits: t=2.238, p=.028). Nevertheless, there were no significant differences between these 2 groups in terms of processing speed (TMT, BACS and animals), reaction time (simple and elective) or facial emotion recognition (FEIT). The dose they received (measured in chlorpromazine equivalents) correlated with processing speed in BACS (P=−.209; p=.040) and sustained attention (2 digits: P=−.332, p=.001; 3 digits: P=−.368, p=.000; 4 digits: P=−.166, p=.111).
Schizophrenia patients’ scores in cognitive tasks.
| Average (SD) | Normative data Average (SD) | |
|---|---|---|
| Processing speed (TMT-A, Animals, BACS) | 33.08 (13.79) | 50 (9.9) |
| Trail Maker Test (TMT-A) | 43.96 (23.52) | |
| Verbal fluidity (animals) | 19.08 (6.13) | |
| Symbol coding (BACS) | 36.20 (11.71) | 62.26 (15.23) |
| Simple reaction time | 297.396 (156.133) | |
| Elective reaction time | 955.404 (1352.210) | |
| Facial emotion recognition (FEIT) | 12.53 (2.98) | 14.53(1.88) |
| 2 digit sustained attention | 2.717 (1.13) | 4.06 (0.10) |
| 3 digit sustained attention | 2.049 (1) | 3.56 (0.12) |
| 4 digit sustained attention | 1.079 (.8) | 2.27 (0.11) |
A statistically significant correlation was found between the positive PANSS sub-scale score and elective reaction time (P=0.278; p=.006), and between the negative PANSS sub-scale and processing speed shown by TMT (P=.325; p=.001) and BACS (P=−.195; p=.054), verbal fluidity (P=−.248; p=.014), simple reaction time (P=.215; p=.035) and elective reaction time (P=.252; p=.014) and the recognition of facial emotions (P=−.205; p=.043). Anxiety was not associated with any cognitive variable, and anxiety-trait only correlated with verbal fluidity (P=−.216; p=.034).
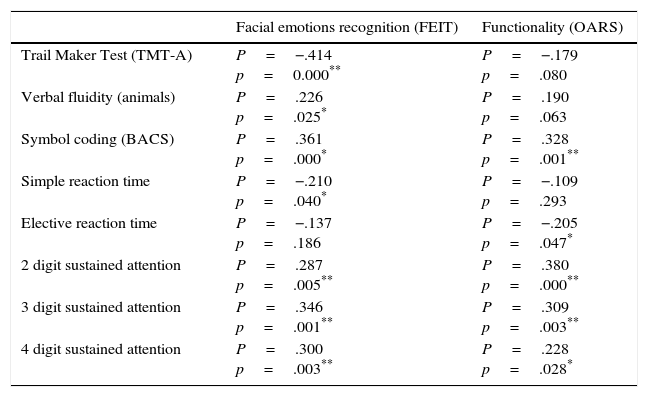
Cognitive variables, facial emotion recognition and functionalityPerformance in the facial emotion recognition test (FEIT) was significantly correlated with processing speed measurement scores (BACS, Animals, TMT), sustained attention (CPT2, CPT3, CPT3) and simple reaction time, although this was not the case for elective reaction time (Table 3). On the other hand, the measurements associated with functionality (OARS scale score) were processing speed (only when it is measured using BACS), sustained attention (CPT2, CPT3, CPT3) and elective reaction time (but not simple reaction time). The subjects with the highest score in the processing speed tests also performed better in the simple reaction time tasks (p<.05 and p<.01) and vigilance (p<.01). No relationship with this was only obtained between the verbal fluidity test and elective reaction time (p>.05).
Correlation between cognitive measurements, emotional recognition and functionality.
| Facial emotions recognition (FEIT) | Functionality (OARS) | |
|---|---|---|
| Trail Maker Test (TMT-A) | P=−.414 p=0.000** | P=−.179 p=.080 |
| Verbal fluidity (animals) | P=.226 p=.025* | P=.190 p=.063 |
| Symbol coding (BACS) | P=.361 p=.000* | P=.328 p=.001** |
| Simple reaction time | P=−.210 p=.040* | P=−.109 p=.293 |
| Elective reaction time | P=−.137 p=.186 | P=−.205 p=.047* |
| 2 digit sustained attention | P=.287 p=.005** | P=.380 p=.000** |
| 3 digit sustained attention | P=.346 p=.001** | P=.309 p=.003** |
| 4 digit sustained attention | P=.300 p=.003** | P=.228 p=.028* |
Pearson's test.
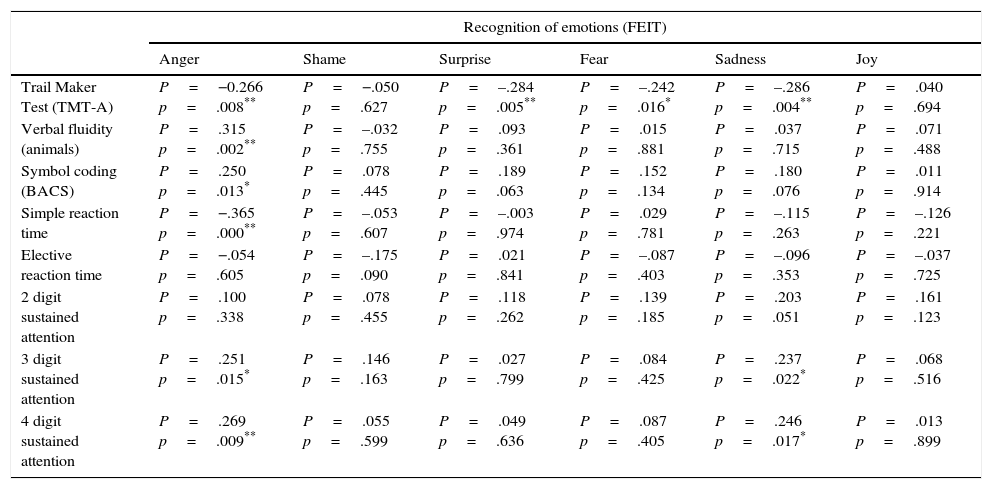
After checking the association between the cognitive variables and emotional processing, this was discriminated according to recognition of the different emotions. The percentages of correct selection for each emotion were as follows: joy (95%), anger (71.6%), surprise (69.9%), fear (61.1%), sadness (60.2%) and shame (39.2%). An inverse correlation was found between the score on the positive PANSS sub-scale and the recognition of joy (P=−.206; p=.012), as well as between the negative PANSS sub-scale and the recognition of sadness (P=−.242; p=.017). Functionality was significantly associated with the recognition of anger (P=.200; p=.049), sadness (P=.244; p=.016), surprise (P=.247; p=.015) and shame (P=.211; p=.038). Patients who showed poorer recognition of anger obtained worse results in the processing speed, reaction time and sustained attention tests (Table 4). The cognitive test that correlated with the highest number of emotions was the TMT in association with the recognition of surprise (P=−.284, p=.005), fear (P=−.242, p=.016) and sadness (P=−.286, p=.004). The sustained attention score (CPT) was associated with the recognition of sadness and anger. However, the recognition of shame and joy did not correlate with any of the cognitive variables, while the recognition of surprise and fear was exclusively associated with the TMT score.
Correlation between the percentage of correct answers in basic emotion recognition (FEIT) and cognitive variables.
| Recognition of emotions (FEIT) | ||||||
|---|---|---|---|---|---|---|
| Anger | Shame | Surprise | Fear | Sadness | Joy | |
| Trail Maker Test (TMT-A) | P=−0.266 p=.008** | P=−.050 p=.627 | P=–.284 p=.005** | P=–.242 p=.016* | P=–.286 p=.004** | P=.040 p=.694 |
| Verbal fluidity (animals) | P=.315 p=.002** | P=–.032 p=.755 | P=.093 p=.361 | P=.015 p=.881 | P=.037 p=.715 | P=.071 p=.488 |
| Symbol coding (BACS) | P=.250 p=.013* | P=.078 p=.445 | P=.189 p=.063 | P=.152 p=.134 | P=.180 p=.076 | P=.011 p=.914 |
| Simple reaction time | P=−.365 p=.000** | P=–.053 p=.607 | P=–.003 p=.974 | P=.029 p=.781 | P=–.115 p=.263 | P=–.126 p=.221 |
| Elective reaction time | P=−.054 p=.605 | P=–.175 p=.090 | P=.021 p=.841 | P=–.087 p=.403 | P=–.096 p=.353 | P=–.037 p=.725 |
| 2 digit sustained attention | P=.100 p=.338 | P=.078 p=.455 | P=.118 p=.262 | P=.139 p=.185 | P=.203 p=.051 | P=.161 p=.123 |
| 3 digit sustained attention | P=.251 p=.015* | P=.146 p=.163 | P=.027 p=.799 | P=.084 p=.425 | P=.237 p=.022* | P=.068 p=.516 |
| 4 digit sustained attention | P=.269 p=.009** | P=.055 p=.599 | P=.049 p=.636 | P=.087 p=.405 | P=.246 p=.017* | P=.013 p=.899 |
Pearson's test.
Analysis of the correlation revealed a statistically significant relationship between functionality and processing speed (through the BACS), sustained attention in each CPT sub-test and elective reaction time. Verbal fluidity and TMT were associated with functionality, although the relationship did not attain statistical significance. Simple reaction time did not show any correlation with functionality. The relationship between the recognition of emotions and functionality was significant too (P=−.338; p=.001).
A linear regression model was then created by successive steps with the OARS (functionality) scores as the dependent variable and the variables previously shown to correlate as independent ones. This model showed a significant relationship between functionality, the recognition of emotions (β=.272; p=.010) and processing speed measured using the BACS (β=.225; p=.033). Due to lack of statistical significance this model excluded the TMT score, verbal fluidity, elective reaction time, sustained attention and the antipsychotic dose received (in chlorpromazine equivalents).
DiscussionThe aim of this work is to analyse in greater depth the relationship between the processing speed deficit shown by schizophrenia patients and their functional deterioration. We firstly discriminated between related variables such as reaction time (simple and elective), processing speed and sustained attention. Our results indicate that these units of analysis can be differentiated and have different impacts on functionality. It was therefore found that processing speed (measured by the BACS)—but not verbal fluidity or TMT—, elective (but not simple) reaction time and sustained attention correlate significantly with degree of functional deterioration. Reaction time (or response time) is a cognitive variable which has hardly been measured in schizophrenia studies. It measures the time which passes between the stimulation of a sense organ and the start of a response or clear reaction. Its simple component (with greater motor reflex influence) measures the latency of response to a series of basis stimuli, while its elective component (which is more closely related to sustained attention and processing speed) involves the processing of more information. Our results suggest that this second component, which is based on the difficulty of processing minimally complex information in a short time, has greater functional consequences in schizophrenia patients. This agrees with other studies which state that processing speed tests (and more specifically the BACS) are based not so much on psychomotor response time (as is the case with simple reaction time), but rather depend on processes associated with attention, memory and executive function.40 The role of antipsychotic medication should therefore be analysed in terms of this cognitive-motor variable. In our sample the dose of medication was not associated with a poorer (simple or elective) reaction time, although it was associated with worse processing speed and sustained attention. Likewise, although the patients under polytherapy had the same reaction time as those under monotherapy, they had worse sustained attention.
Another finding of this study is that it shows how the interaction between processing speed deficit and the recognition of facial emotions has a significant impact on functionality (as is shown by the multiple regression model that was developed). To date schizophrenia patients’ emotional recognition deficit has often been studied (see the meta-analysis by Savla et al.20) using static images that express a certain emotion and which subjects have to guess. The expression of these emotions in real life is dynamic and takes many forms rather than being fixed, i.e., they are perceived not only by visually processing facial expressions, but also on the basis of bodily gestures, auditory and tactile signals and the context, etc.), which has given rise to methodological criticism of the paradigm of emotional processing evaluation.41,42 The hypothesis which emerges from our study is that the deficit which mainly affects the functionality of schizophrenia patients is not so much a difficulty in recognising emotions, but rather consists of the interaction of this (static) deficit with slowness in information processing, i.e., in real life the patient is overloaded with transitory social signals that have to be processed. This collides with the difficulty these patients find in attributing meaning to the many stimuli they receive in reality (salience or the assignation of aberrant relevance)—mediated through the dopaminergic meso-striatal dysfunction43,44—and their proven slowness in information processing.2 This interaction between social cognition and processing speed deficits would partially explain the predictive power of the latter variable for functionality, which has been reported in several studies.45,46 This is also consistent with the idea that social cognition mediates between neurocognition and functionality.47 Our study shows that the recognition of emotions and processing speed are associated, independently of functionality. The possible interaction—multiplicatory or summatory—between both variables will have to be tested in the future.
On the other hand, our study discriminates between the effect of recognition deficit for each one of the basic emotions. Thus, and similarly to previous studies,48 schizophrenia patients found it harder to identify negative emotions. Interestingly, those patients with more positive psychotic symptoms were worse at recognising joyful faces, while those with more negative symptoms found it harder to recognise sad faces. In general low functionality was associated with the recognition of anger, sadness, surprise and shame, while the recognition of anger correlated with different measures of processing speed and attention. The explanation of these finds agrees with those works that underline that emotional attribution errors by schizophrenia patients are not solely based on false positives (paranoiacly attributing anger to neutral or positive facial expressions) but also on false negatives (ignoring angry facial expressions or considering them to express fear or even joy).49 This “threat ignoring” (which is sometimes concomitant with “alert due to false threats”) is associated in our sample with difficulties in processing information in a short time and maintaining sustained attention to a stimulus. These 2 cognitive abilities are probably decisive in the process of reappraising a stimulus to correct an initial inferential error. Some social cognition training therapies (such as the SCIT program for Social Cognition and Interaction Training)50 emphasise training patients to reconsider initial social judgements, preventing the jumping to conclusions which characterises schizophrenia. In this way, steadily re-evaluating a stimulus over a longer period of time and processing more information (by promoting abilities such as processing speed or sustained attention) may leader to better emotional recognition and, hypothetically, better psychosocial adjustment.
This work has several limitations and strengths. Its most important limitations are: (a) that it evaluates functionality using a summarised score, such as the OARS. It would have been preferable to use an exhaustive scale that measures a range of aspects of this complex construct; (b) some predictive cognitive variables of functionality in schizophrenia were not measured, such as working memory or executive function.51 The analysis may therefore be distorted by the omission of a variable; (c) the relationships found between variables are purely correlational, so that the question of causality (do the symptoms cause the social cognition deficit, or vice versa? In which direction does the association between neurocognition and social cognition function?) is still an open question. The main strong points of this study are: (a) it measures—which to date has been infrequent—reaction time as a variable that is related to but which is different from processing time; (b) it evaluates a consecutive (and therefore representative) sample of schizophrenia outpatients; (c) and finally, it discriminates between the analyses of different emotions on the FEIT scale. The association found between processing speed, the recognition of emotions and functionality opens up the field for new studies that elucidate the psychosocial deterioration of schizophrenia patients.
Ethical disclosuresProtection of human and animal subjectsThe authors declare that the procedures followed were in accordance with the regulations of the responsible Clinical Research Ethics Committee and in accordance with those of the World Medical Association and the Helsinki Declaration.
Confidentiality of dataThe authors declare that they have adhered to the protocols of their centre of work on patient data publication.
Right to privacy and informed consentThe authors must have obtained the informed consent of the patients and/or subjects mentioned in the article. The author for correspondence must be in possession of this document.
Conflict of interestsIn the past 3 years Dr. Guillermo Lahera has received fees for giving conferences from Janssen, Lundbeck and Otsuka. The other authors have no conflict of interests to declare.
We would like to thank Professor Manuel Sillero Quintana of the Universidad Politécnica, Madrid, for supplying us with version 2.0 of the SUPERLAB pro program by CEDRUS.
Please cite this article as: Lahera G, Ruiz A, Brañas A, Vicens M, Orozco A. Tiempo de reacción, velocidad de procesamiento y atención sostenida en esquizofrenia: impacto sobre el funcionamiento social. Rev Psiquiatr Salud Ment (Barc). 2017;10:197–205.