Suicidal behaviour is a major public health issue. Suicidal behaviour is one of the main causes of years of life lost and it is the third leading cause of death among young adults. This project was initiated by the Spanish Society of Psychiatry and the Spanish Society of Biological Psychiatry with the aim of providing a document containing the main recommendations on the prevention and management of suicidal behaviour; these recommendations should be based on the best available evidence and the experts’ opinion.
Material and methodsIn this article we summarise the review of the available evidence on the epidemiology and impact of suicidal behaviour, risk and protective factors, evaluation tools for the assessment of suicide risk, international and local preventive protocols, educational interventions for health professionals, and potential interventions for at risk populations.
ResultsBased on this review, a panel of psychiatrists summarised and agreed with a set of recommendations about the impact, prevention and management of suicidal behaviour.
ConclusionThe recommendations on the prevention and management of suicidal behaviour were summarised in the ten conclusions reported in this article.
El suicidio es un problema importante de salud pública que constituye una de las principales causas de años de vida perdidos por enfermedad y la tercera causa de mortalidad en adultos jóvenes. El objetivo de este proyecto iniciado por la Sociedad Española de Psiquiatría y la Sociedad Española de Psiquiatría Biológica fue preparar un documento que, a partir de la evidencia disponible y la opinión de los expertos, realizara unas recomendaciones sobre la prevención y el manejo del comportamiento suicida.
Material y métodosEn este trabajo se resume la revisión de la evidencia disponible sobre la magnitud e impacto epidemiológico de la conducta suicida, los factores de riesgo y factores protectores, los instrumentos de evaluación del riesgo de conducta suicida, los protocolos preventivos existentes a nivel internacional y local, las intervenciones preventivo-educativas a nivel de los profesionales de la salud, y las posibles intervenciones sobre poblaciones de riesgo.
ResultadosDe esta revisión un amplio grupo de psiquiatras expertos sintetizó y consensuó un conjunto de recomendaciones sobre el impacto, la prevención y el manejo de la conducta suicida.
ConclusionLas recomendaciones sobre la prevención y el manejo del comportamiento suicida fueron resumidas en las diez conclusiones que se presentan en este trabajo.
Suicide is a major public health issue, whose true significance is underestimated due to statistical limitations in documenting completed suicides, nationally and internationally. Despite this, the figures are high and data from the World Health Organisation (WHO) illustrate that more than 1 million people commit suicide per year globally, making suicide the third leading cause of death among people aged 15–44 years old.1 The epidemiological magnitude and social impact of suicide include not only death by completed suicide, but also suicidal ideation and suicide attempt, as well as the consequences that all of the above have on the quality of life of a population. In this regard, the data from WHO place suicide as one of the leading causes of years of potential life lost (YPLL) due to illness.2
Given the significance of suicidal behaviour, the European Pact for Mental Health and Well-being3 incorporates suicidal behaviour prevention into 5 areas of priority action. In addition, the American Psychiatric Association has developed some guides for suicide prevention and risk evaluation4 and has plans to include a reference for assessing, as an independent axis, the presence or absence of suicide risk in the next edition of the Diagnostic and Statistical Manual of Mental Disorders (DSM-5).5
Nevertheless, in Spain, psychiatrists’ actions when confronting the risk of suicidal behaviour still vary, especially in both suicide risk assessment and adequate documentation of patients’ clinical histories.6,7 For that reason, the Spanish Psychiatry Society (SEP in Spanish) and the Spanish Biological Psychiatry Society (SEPB) are interested in undertaking the initiative described in this article. Their final objective is to develop recommendations for management and prevention of suicidal behaviour. To this end, they carried out meetings with experts in which they reviewed the current evidence available concerning epidemiology, risk factors, assessment and suicide prevention and intervention programs. This information was the basis for an elaboration of the recommendations that make up final guidelines.
MethodsIn preparing the recommendations for suicide management and prevention, the project coordinators (JB, JS and JG), as representatives of the Spanish Biological Psychiatry Society, the Spanish Psychiatry Society and the Spanish Foundation for Psychiatry and Mental Health, established a small group of experts in charge of said review. In addition, they decided to survey psychiatrists in Spain in order to evaluate the conduct patterns of these professionals in the presence of patients with risk of suicidal behaviour; the results of this survey have become the objective of another publication.6
This group of selected psychiatry experts wrote a first draft that summarised the evidence available on the problem magnitude, risk factors and different methods of assessment, prevention and intervention. This first draft was discussed in a second meeting with a broader group of experts (Annex 1). During this meeting they analysed the aspects most relevant to suicidal behaviour management, which served as a basis for preparing the final recommendations.
At a third meeting, the project coordinators, in collaboration with the reviewing authors, on the basis of the reviewed information and new suggestions from the first 2 meetings, prepared a draft of recommendations presented systematically in the form of guidelines. This draft was distributed among all project participants for review, comments and approval.
Below is all the information prepared by the group of experts, as well as the final guidelines approved by all the participants.
Epidemiological magnitude and social impact of suicidal behaviourSuicidal behaviour encompasses various phenomena, among which the most relevant are completed suicide, suicide attempt and suicidal ideation. Completed suicide refers to self-inflicted death with evidence (explicit or implicit) that the person had the intention of dying; suicide attempt is defined as self-injury with non-fatal results accompanied by evidence (explicit or implicit) that the person had the intention of dying; and suicidal ideation refers to a person thinking about causing their own death.4 The distinction between each of these phenomena is important when determining its impact, given that 2 different approaches can be taken: assess each of these phenomena separately or assess them together, that is to say, study suicidal behaviour holistically. The prevalence of suicidal ideation has recently been explored in 2 European studies, in both of which Spain participated.8,9 In the first one, the European Study of the Epidemiology of Mental Disorders (ESEMeD), observed a vital prevalence of 7.8% for suicidal ideation and 1.8% for suicide attempts. In Spain the figures were less than those of the main sample (4.4% for suicidal ideation and 1.5% for suicide attempts). This same trend was observed in the Outcomes of Depression International Network (ODIN) study, carried out in 5 European countries, Spain being one of them. The results of that study illustrated that suicidal ideation in Spain (2.3%) is relatively low in comparison with other European countries (7.4% in Norway, 9.8% in Finland and 14.6% in Ireland).9
With respect to death by suicide, it is estimated that 54,280 people committed suicide in the year 2000 in the WHO EUR-A European region (which includes Spain), which makes up 1.3% of total estimated deaths in the region in that year. Higher rates were seen in the age groups 15–44 years old and 60 or older.10
In the specific case of Spain, the pattern of death by suicide is similar to that of the rest of the European population. In 2006, the crude suicide mortality rate was 11 for every 100,000 men and 3 for every 100,000 women, which constitute 1.3% and 0.4%, respectively, of the total mortality rate.11 Among men as well as women, the highest number of deaths occur in people over 60 years old.
As for the method used to commit suicide, hanging is more common among men (40% of total suicides), followed by jumping from height (28% of total), as indicated by death certificate. Among women, jumping from height was the method most used (59% of total), followed by hanging (14%).12
Suicide makes up 3.1% of total YPLL in men and 1.4% in women. By age group, the highest percentage is found for both men and women in the 15–29 group, in which suicide makes up 10.5% of total YPLL in men and 7.6% in women. Suicide is the ninth cause of YPLL in men and ranks 21 in women. Nonetheless, in the age group 15–44 years old, suicide is the third cause of YPLL in men, after traffic accidents and AIDS; in women it ranks fourth after traffic accidents, breast cancer and AIDS.11
In comparison with the data from the European region, suicide composes a smaller proportion of YPLL in Spain than in the entire rest of the region. Even though it is a country at lower risk than other European countries, the lineal increase trend observed in suicide mortality in Spain over the last few years is worrisome.13
Risk factors and protective factorsRisk factors of suicidal behaviour are classically divided into 2 groups, those that are clinically alterable (such as psychiatric disorders) and those that are not (such as hereditary factors, sex or age). In addition to risk factors, it is important to take protective factors into account to assess and prevent suicide risk. Within this section, we will review the most relevant protective and risk factors.Many studies agree that a history of suicide attempts in the patient's past is a risk factor that most reliably predicts the possibility of a future completed suicide.14–17 In a systematic review of 14 cohorts totalling 21,385 subjects,18 it was estimated that people with previous self-injury attempts were nearly 25 times as likely to commit suicide than the general population. Approximately 1–6% of patients hospitalised for a suicide attempt will commit suicide in the following year, the risk being higher in older patients or those with a history of repeated attempts.19–21
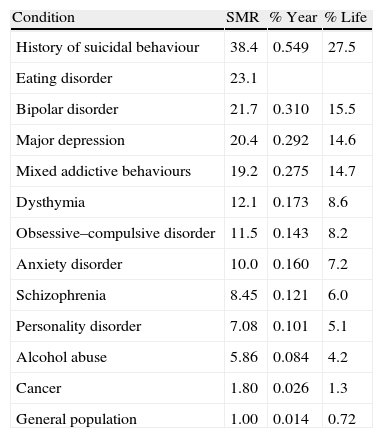
The existence of psychiatric disorders is another major risk factor of suicide.22,23Table 1 presents the estimated suicide risk for those with mental disorders according to the APA Guide published in 2003.4 As shown in the table, bipolar disorder, major depressive disorder and mixed addictive behaviours are the psychiatric conditions most at risk for suicidal behaviour.
Suicide risk in specific disorders.
| Condition | SMR | % Year | % Life |
| History of suicidal behaviour | 38.4 | 0.549 | 27.5 |
| Eating disorder | 23.1 | ||
| Bipolar disorder | 21.7 | 0.310 | 15.5 |
| Major depression | 20.4 | 0.292 | 14.6 |
| Mixed addictive behaviours | 19.2 | 0.275 | 14.7 |
| Dysthymia | 12.1 | 0.173 | 8.6 |
| Obsessive–compulsive disorder | 11.5 | 0.143 | 8.2 |
| Anxiety disorder | 10.0 | 0.160 | 7.2 |
| Schizophrenia | 8.45 | 0.121 | 6.0 |
| Personality disorder | 7.08 | 0.101 | 5.1 |
| Alcohol abuse | 5.86 | 0.084 | 4.2 |
| Cancer | 1.80 | 0.026 | 1.3 |
| General population | 1.00 | 0.014 | 0.72 |
SMR: standardised mortality ratio (ratio between mortality observed in study group and the expected mortality in the population of reference, commonly the general population); % Year: annual suicide rate; % Life: estimated suicide rate over the life cycle.
Major depressive disorder can increase suicide risk by as much as 20 times, especially at the beginning or at the end of a depressive episode, as the psychomotor slowdown and inhibition during the episode prevent action from being taken.24,25 Nonetheless, in patients with moderate depressive disorder (more frequent than major depressive disorder), the suicide risk is lower; that is why the suicide mortality rate for patients with depression has fallen from 15% to 5% overall.26 The suicide rate among patients with bipolar disorder oscillates between 10% and 15%. According to some authors, the rate is higher in patients with bipolar disorder II and it increases in comorbidity with other disorders, especially with personality disorders.27 In addition, the lack of treatment adherence in patients with bipolar disorder seems to be related to the increased risk of suicidal behaviour, even though it is not known whether this lack of adherence leads to an increased risk in suicidal tendencies because of specific properties of lithium treatment or simply because it is secondary to stabilising the manic state.28
Patients with schizophrenia, whose risk of suicide is 8.5 times higher than the general poplulation,29 share some of the same risk factors as the general population (such as being male, single, unemployed, living alone or being socially isolated) and they also present other factors specific to schizophrenia, such as psychopathological factors; some of these are well established factors (like depression and hopelessness) and others are still controversial (negative psychotic symptoms).30,31 In addition, there are other risk factors associated with schizophrenia, such as being young, having suffered several relapses with a high rate of psychiatric institute admission and having sexual, social and work impairment due to the illness or low adherence to treatment.30,31 The correlation between antipsychotic use and suicidal behaviour, although it was initially controversial, has since been rejected and, to the contrary, adherence to treatment has been established as a protective factor.31 Studies like that of Johnson et al.32 or those carried out with atypical antipsychotics,33 with fewer side effects, showed that antipsychotics could reduce suicide risk. Among the antipsychotics, clozapine stood out from the rest, given that it caused an 85% decrease in patients’ suicide risk.34 This has made it the only drug currently indicated for treating suicidal behaviour associated with schizophrenia.
On the other hand, the high prevalence of substance abuse disorder and especially alcoholism are often related with an increase in suicide risk.29 Consumption of other drugs (opiates, cocaine, marijuana, sedatives, etc.) and, especially, joint dependence on multiple substances have been associated with a 20 times higher risk of suicide.29
Personality disorders are particularly relevant, given that they can cause suicidal behaviour in various ways: predisposing patients to more serious mental disorders such as depression or alcoholism, leading to problems in interpersonal relationships and social adjustment, precipitating undesirable life events or deteriorating the ability to face a physical or mental illness.35–38 Hopelessness, neuroticism and extraversion are personality traits that show the most association with suicidal behaviour, while others (such as aggression, impulsiveness, irritability, hostility or anxiety) demonstrate less conclusive associations.39
The risk of suicidal ideation or attempt is determined by a complex interaction between genetic and environmental factors.40 Certain authors estimate that 43% of suicidal behaviour can be contributed to genetic make-up and the remaining 57% to environmental factors.41,42 Inheritance of suicidal behaviour seems to be determined by at least 2 components: (1) the transmission itself of mental diseases and (2) the genetic endowment related to aggression, impulsiveness and other personality factors.43 A meta-analysis of 21 studies showed that risk of suicidal behaviour tripled for subjects’ immediate family members, despite absence of a psychiatric pathology.44
In the majority of countries, with the exception of China, suicide rates are higher in men than in women.45 However, the rate of suicide attempts is usually higher in women than in men.46 Regarding suicide attempts, in addition to common factors like mental illness, there are others—such as low income or smoking—associated with attempts by men, while a worse perception of health or lower level of education are factors associated with attempts by women.47
Even though the suicide rate increases with age,48 youth and adolescents make up an important at-risk group. In fact, according to data from the National Institute of Statistics, suicide is among the primary causes of death in youth and adolescents.49 In the youth group, one of the more frequent causes of suicidal behaviour is the existence of psychiatric disorders, mainly mood disorders, substance use and behaviour disorders.50 Likewise, suicide risk seems to be 2 times higher for young subjects in a low socioeconomic class,51 5 times higher for those who have dropped out of school and nearly 8 times higher for those without a university education.52 Parent separation also appears to increase suicide risk.50,51 Furthermore, many studies have confirmed the association between suicide attempt in children and physical or sexual abuse.50,53,54
The elderly population makes up another significant at-risk group. Somatic disease or disability55,56 and the loss of autonomy in daily life activities57 are some of the specific risk factors for this population. Likewise, depression seems to be a mediator between somatic disease and suicide in this patient group.58 There is also a clear association between suicide and the social isolation of the elderly.59,60
Other socio-demographic factors that influence suicide risk are, for example, unemployment, financial problems and relationship problems.59,61 Regarding occupation, there is a notable increase in risk for those who have health-related professions.62
The most commonly accepted protective factors of suicide risk can be divided into those of the individual and those of the environment.63,64 Among the first, we can include attitudes and values against suicide, such as the concept of value for one's own life. In addition, social skills, anger management and problem-solving abilities support the decision to not commit suicide. Other variables related to protection are maintenance and pursuit of good mental and somatic health, religious beliefs that disapprove of suicide, fear of pain and risky behaviour, presence of hope and optimism, self-control of impulsiveness, high self-esteem, appropriate confrontational strategies and high resilience. Among the significant environmental factors are the existence of a suitable social and family network with responsibility for others, social participation, access to health solutions, stable surroundings and restrictions on access to potentially lethal weapons or medications.36,60,61 Living with a partner and living with dependent children are also considered to be protective factors against suicide.65 In fact, widowhood and divorce increase suicide risk and appear to affect men more than women.66,67 Other factors like maternity and pregnancy have been identified as protective factors.68,69
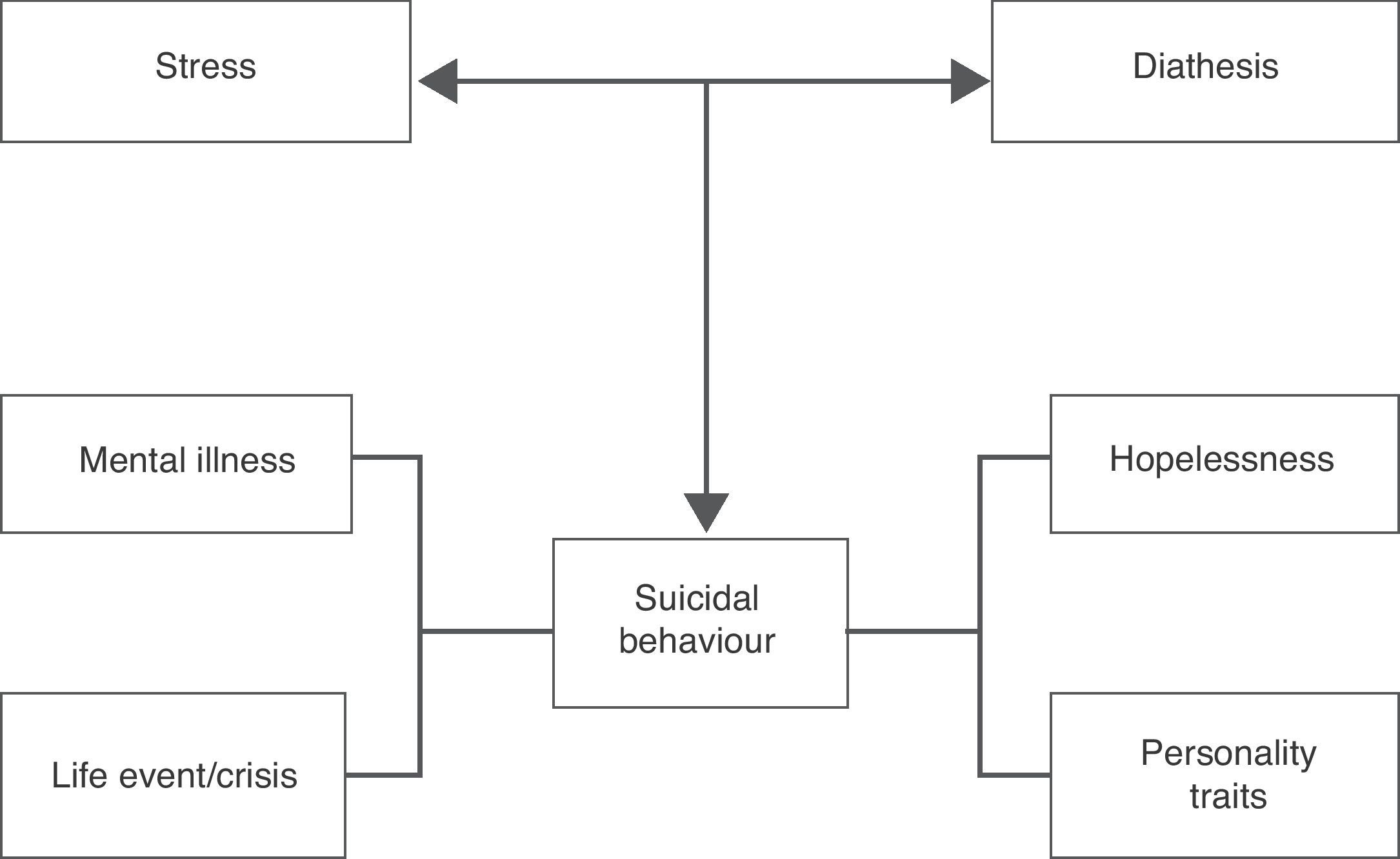
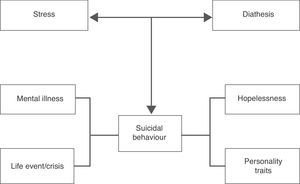
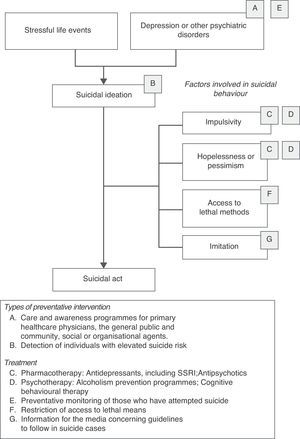
Although suicide risk is related to the number of risk factors present, Mann et al.70,71 proposed a broadened stress-diathesis model, useful in comprehending risk of suicidal behaviour (Fig. 1). The model features 2 interrelated dimensions: the dimension of personality characteristics (genetics, substance abuse, identity or impulsiveness) and the dimension of triggers or precipitators (acute psychiatric illness or adverse life events). The combination of both dimensions would be more important in determining risk of suicidal behaviour than the mere accumulation of risk factors. This highlights the importance of an adequate assessment of patients with suicide risk if they exhibit population risk factors as well as risk factors related to mental illness or disability.
Instruments of assessmentAssessment of suicide risk is one of the most important, complex and difficult tasks that any clinician has to face.4 Under the existing framework in which everyday psychiatric practice develops, increasingly more attention is being paid to the potential liability derived from an insufficient or incorrect suicide risk assessment. One of the most frequent problems consists of failing to adequately document clinical judgments and observations.7,72–74 Furthermore, it should be emphasised that using psychometric scales in assessing suicidal behaviour has yet to be incorporated as a routine method in everyday clinical practice.75,76 Specifically, in Spain, in a recently completed survey of 400 psychiatrists, it was observed that only 10% of them habitually use structured scales and questionnaires to assess suicide risk. To rectify this, the next edition of the Diagnostic and Statistical Manual of Mental Disorders (DSM-5) advocates the need to assess, as an independent axis, the presence (or absence) of suicide risk.5,73,74,76
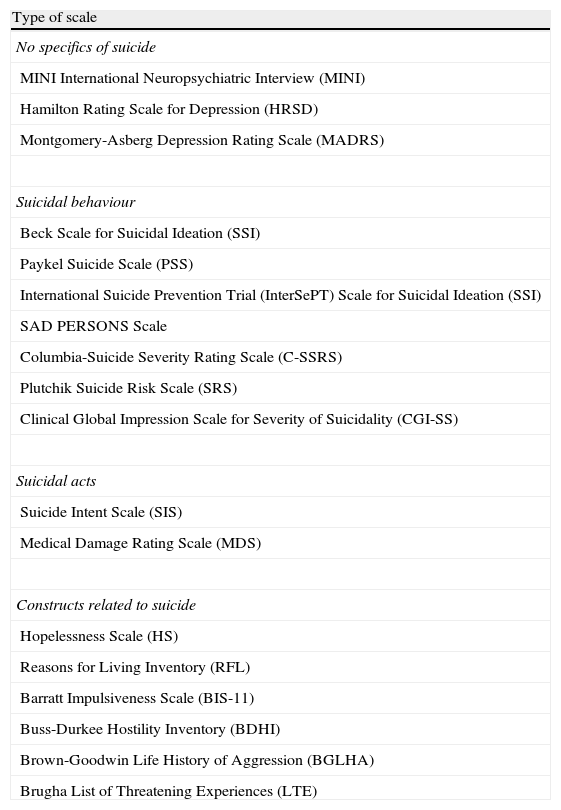
In this context, this article attempts to provide a general reference framework to aid the clinician in settling this problem and in systematising, as much as possible, suicide risk assessment in their clinical practice. To this end, we have selected the scales that we considered most relevant because of their usefulness from the clinician's point of view, or because they have shown to be more useful in research. In Table 2 we have grouped these scales into different sections, according to their specific application in assessing suicidal behaviour.77
Suicide risk assessment scales.
| Type of scale |
| No specifics of suicide |
| MINI International Neuropsychiatric Interview (MINI) |
| Hamilton Rating Scale for Depression (HRSD) |
| Montgomery-Asberg Depression Rating Scale (MADRS) |
| Suicidal behaviour |
| Beck Scale for Suicidal Ideation (SSI) |
| Paykel Suicide Scale (PSS) |
| International Suicide Prevention Trial (InterSePT) Scale for Suicidal Ideation (SSI) |
| SAD PERSONS Scale |
| Columbia-Suicide Severity Rating Scale (C-SSRS) |
| Plutchik Suicide Risk Scale (SRS) |
| Clinical Global Impression Scale for Severity of Suicidality (CGI-SS) |
| Suicidal acts |
| Suicide Intent Scale (SIS) |
| Medical Damage Rating Scale (MDS) |
| Constructs related to suicide |
| Hopelessness Scale (HS) |
| Reasons for Living Inventory (RFL) |
| Barratt Impulsiveness Scale (BIS-11) |
| Buss-Durkee Hostility Inventory (BDHI) |
| Brown-Goodwin Life History of Aggression (BGLHA) |
| Brugha List of Threatening Experiences (LTE) |
In addition to the scales included in Table 2, there are multiple instruments that have been designed for assessing factors directly or indirectly related to suicidal behaviour. There are comprehensive guides of useful assessment tools in the sphere of suicidal behaviours in particular, and for mental and conduct disorders.78,79
Given that no single assessment tool exists, it is recommended to use those that most suit the clinician's needs, according to factors such as a patient's clinical characteristics or the physical location of the assessment. Likewise, whenever possible, it is recommended to use scales that rely on appropriate psychometric properties and that have been adapted and validated within the field. Regardless of the instruments used for assessment, the assessment results should be included in the clinical history.
The World Health Organisation, through their publication of the ICD-10 classification, Mental and Behavioural Disorders for Primary Healthcare,80 produced the following recommendations for suicide risk assessment:
- (a)
Assessment of suicide risk in the immediate future
- •
Suicidal ideation (sporadic vs persistent).
- •
Determination (suicide as a possibility or a firm decision).
- •
Suicide plan (level of elaboration: the more elaborate the suicide plan, the greater the risk; the availability of means to commit suicide increases risk).
- •
Loneliness (lack of social or family support increases risk).
- •
Consumption of alcohol or other substances (limitation of individual self-control can facilitate suicidal behaviour).
- •
Social difficulties (marginalisation, unemployment or lack of expectations increase risk).
- •
- (b)
Assessment of patient with a recent suicide attempt
- •
Hazardousness of chosen method.
- •
Degree of conviction concerning efficiency of chosen method.
- •
Possibility of being discovered.
- •
Degree of relief upon being saved.
- •
Purpose of suicidal behaviour (intended to send a message or to die).
- •
Degree of planning.
- •
Existence (or absence) of changes in psychological or life situation that triggered suicidal behaviour.
- •
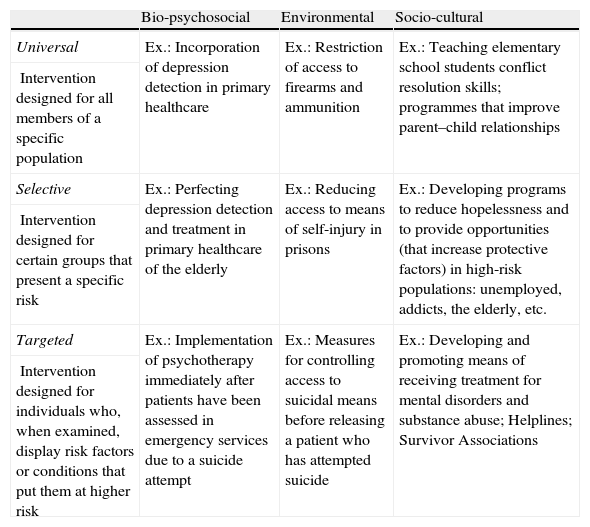
The Chronic Illnesses Commission81 proposed a 3-category classification for preventative measures—primary, secondary and tertiary prevention—that has achieved an important and growing global influence and that has been present in the majority of public health policies. However, this classification system began to turn obsolete, until it started incorporating information and non-mechanistic character concepts in biomedical research and proposed completing the prior classification with an approach focused on an assessment of risks and benefits for different population groups: universal, selective and targeted prevention (Table 3).82 This approach has been taken up to propose a general framework of specific preventative intervention for mental illnesses.83,84 The level at which each type of specific intervention should be categorised depends on empirical results obtained from research and from cost/benefit analyses performed for each specific population and problem. In turn, these 3 types of prevention can be applied on 3 different levels of specificity with respect to the particular context of application: bio-psychosocial interventions, environmental interventions and socio-cultural interventions.85 The different suicide prevention programs will be grouped into each of these 3 dimensions under the 3 categories, offering 9 types of different preventative strategies, which are reflected in Table 3. Other authors have hierarchically classified suicide risk factors into primary, secondary and tertiary.86 Primary factors (medical-psychiatric) are the most powerful predictors of suicide, and their prevention would be under the domain of the healthcare system. Secondary factors (psychosocial), which fall under the domain of political authorities, teachers, psychologists and religious and civil organisations, have a lower preventative value. The same is true of tertiary factors (socio-demographic), which do not fall under a defined domain.
Outline of suicide prevention interventions.
| Bio-psychosocial | Environmental | Socio-cultural | |
| Universal | Ex.: Incorporation of depression detection in primary healthcare | Ex.: Restriction of access to firearms and ammunition | Ex.: Teaching elementary school students conflict resolution skills; programmes that improve parent–child relationships |
| Intervention designed for all members of a specific population | |||
| Selective | Ex.: Perfecting depression detection and treatment in primary healthcare of the elderly | Ex.: Reducing access to means of self-injury in prisons | Ex.: Developing programs to reduce hopelessness and to provide opportunities (that increase protective factors) in high-risk populations: unemployed, addicts, the elderly, etc. |
| Intervention designed for certain groups that present a specific risk | |||
| Targeted | Ex.: Implementation of psychotherapy immediately after patients have been assessed in emergency services due to a suicide attempt | Ex.: Measures for controlling access to suicidal means before releasing a patient who has attempted suicide | Ex.: Developing and promoting means of receiving treatment for mental disorders and substance abuse; Helplines; Survivor Associations |
| Intervention designed for individuals who, when examined, display risk factors or conditions that put them at higher risk |
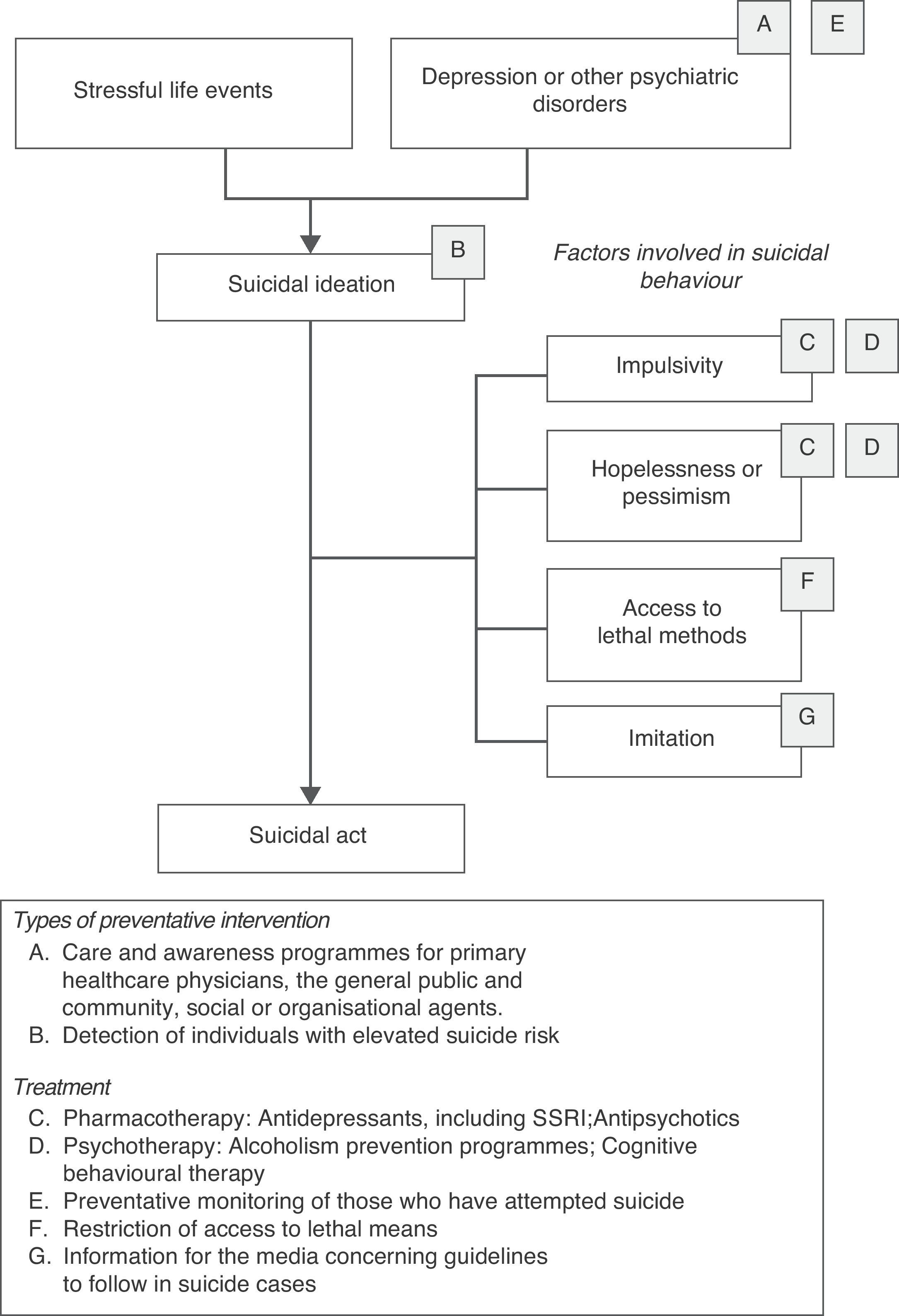
Fig. 2 presents a model that includes the principal risk factors for suicidal behaviour. It also covers the types of interventions that have shown to be most efficient and effective in each of the factors concerning suicide, as per the thorough review carried out by a group of international experts.87 The specific interventions proposed in the model for each of the risk factors for suicidal behaviour can be integrated into the general framework proposed in Table 3. That is, these interventions could in turn be classified as universal, selective or targeted depending on the specific scope and objective, or on the time and location where the preventative action takes place.
Among the world-wide initiatives developed for reducing suicide-related mortality is the WHO project called SUPRE-MISS.88 This program consists of a detailed assessment in 18 different locations of factors associated with suicidal behaviour, and the application of a brief psycho-educational intervention for patients who have attempted suicide. Although some of the results from the SUPRE-MISS study have been published,89 the researchers have yet to release specific data concerning the effectiveness of the socio-educational intervention for those who have attempted suicide. No data concerning the general effectiveness of the study and the WHO policy for influencing the different social agents potentially involved in reducing suicide have been published either.
The WHO initiative in suicide prevention has also entailed the production and dissemination of a series of documents that provide information, recommendations, specific policies and guidelines for different social agents potentially involved in the detection, prevention and treatment of suicidal behaviour: medical professionals, penal institution authorities, professors, the media, etc.90
In Spain, the Strategy in Mental Health of the National Health System, within their Strategic Approach 1 (public awareness of mental health, mental illness prevention and eradication of the stigma attached to people with mental illness) includes suicide prevention as one of their general objectives in the form of carrying out and assessing specific activities to decrease rates of depression and suicide. Nonetheless, even though suicide has become one of the primary focuses of health policy in the European Union and the National Health System, in Spain there is scarce implementation of preventative programs; we now find ourselves at a very low rank compared to other European countries with a similar level of development.91 In fact, there is currently no such national prevention plan in Spain and only local initiatives have been carried out up until now. Such is the case of Cataluña, as a constituent of the European project European Alliance Against Depression (EAAD)92; of Galicia, where a care and prevention program are in full swing, directed towards the early detection of suicide risk in primary healthcare93; or for Asturias, where the European project Monitoring Suicidal Behaviour in Europe (MONSUE)94 has been in development since 2007, focused on thorough monitoring of suicide attempt patients who turn to hospital emergency services. In Asturias as well is the Saving and Empowering Young Lives in Europe (SEYLE) project started in 2009, which was the first European program directed specifically towards the prevention of suicidal behaviour in adolescents.95
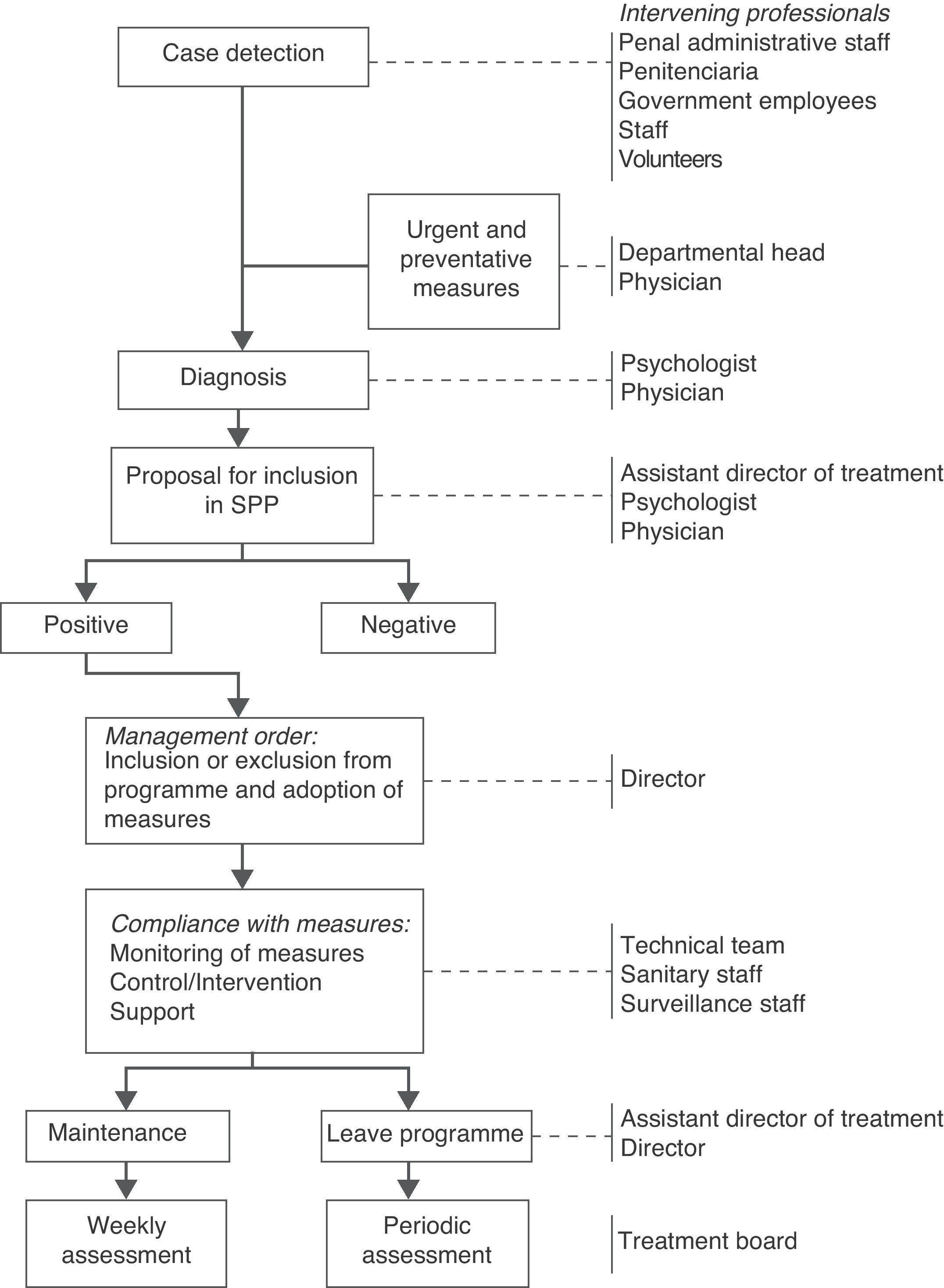
Traditionally, penal institutions have followed a preventative policy focused on restricting access to hazardous or lethal objects for people with a higher risk of self-injury or suicide. On 10 August 2005, the framework for a suicide prevention program was published in penal institutions,96 focused on various steps illustrated in Fig. 3. At the moment, there are no data available on the results of this plan of action. However, the high level of control that the environment permits in this context suggests that effectiveness, given a highly specific plan of action, should be appropriate. Nonetheless, the activities in this framework can hardly be generalised to control and prevent suicide in the community, given the diverse characteristics of the general population and of the participants in the intervention environment.
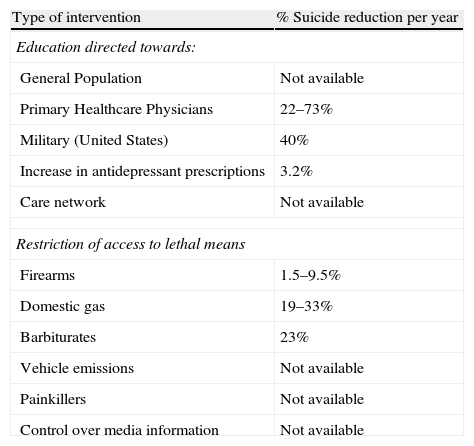
Table 4 presents a summary of the results of the thorough, systematic review of existing suicide prevention strategies and their efficiency, performed by a broad group of world experts in this field.87 Attention-getting facts are the variability in effectiveness of some strategies and, above all, the scarcity of existing data on the effectiveness of the majority of interventions, as well as to the design limitations of the work, the difficulties of generalisation and the rare replications of data. In light of the little evidence available, preventative interventions generally use a comprehensive approach, as proposed by the EAAD,92 combining universal, selective and targeted interventions under different fields and contexts. Moreover, the general recommendation would be that interventions be based on specific characteristics of the population in which they expect to prevent suicidal behaviour. Consequently, if that data were not available, the first step would be to carry out exploratory studies, after which the indications could be based on those results.
Post-intervention reductions in total suicide rate (Mann et al., 2005).
| Type of intervention | % Suicide reduction per year |
| Education directed towards: | |
| General Population | Not available |
| Primary Healthcare Physicians | 22–73% |
| Military (United States) | 40% |
| Increase in antidepressant prescriptions | 3.2% |
| Care network | Not available |
| Restriction of access to lethal means | |
| Firearms | 1.5–9.5% |
| Domestic gas | 19–33% |
| Barbiturates | 23% |
| Vehicle emissions | Not available |
| Painkillers | Not available |
| Control over media information | Not available |
Even though suicide attempt and psychiatric disorders are the principal risk factors for completed suicide, a significant percentage of completed suicide is not preceded by any of these factors. Although identification of suicide attempts and appropriate follow-up for patients with psychiatric disorders in the environment of specialised medical attention is important in the prevention of completed suicide, with that alone we can prevent only a percentage of suicide mortality. That is why it is important to promote prevention programs that include other health professionals who have contact with at-risk patients, particularly primary healthcare physicians, and even social agents and the general public.
The primary healthcare professional has an important role as the gateway to healthcare. Approximately 83% of people who commit suicide had contacted their general practitioner within the previous year and nearly 66% had done so within a month of committing suicide.97 Nonetheless, depression as well as other psychiatric disorders are often under-diagnosed and under-treated in the scope of primary healthcare.98 Consequently, better acknowledgement and treatment of depression, and appropriate of suicide risk assessment by primary care personnel, are key factors that have been shown to be effective in reducing suicide risk.87 In this regard, even though the Spanish Society of Family and Community Medicine (SEMFYC) has proposed some guidelines to action, they are not accompanied by a specific protocol, nor do they specify specific regulations on the steps to follow.
Many European countries have initiated educational programs directed towards primary healthcare professionals. Three of them are training programs, directed towards general practitioners, to improve diagnostic capability and therapeutic management of depression: the Gotland Study in Sweden,99–101 the Jämtland Study in Sweden102 and the Kiskunhalas Study in Hungary.103
In Galicia (Spain), a training and support program in suicide risk detection and assessment is also being carried out for primary healthcare physicians. According to data obtained in January 2010, the 25% of expected suicide attempts after 1 year of follow-up had decreased 3.7%. Towards the end of April 2010, the program had identified 134 patients and continued being given in light of the good results obtained.93
Other initiatives, as in the case of the Nuremberg Alliance Against Depression (NAAD),104–106 include not only medical practitioners, but also the general public, facilitators and high-risk groups. Their results demonstrate the effectiveness of the programme as well as the benefits of a potential synergy effect of multi-level intervention. Because of the results obtained, programmes with a similar methodology have been developed, such as the European Alliance Against Depression (EAAD), in which 17 European countries participate; Spain is among them, due to the involvement of Sant Pau Hospital (Barcelona).92
To summarise, taking into account the data obtained to date in different programmes developed in suicidal behaviour prevention directed towards primary healthcare professionals, the following factors should also be taken into account for launching future initiatives:
- (1)
Know the needs of the area in which the programme is to be implemented (knowledge of the problem magnitude and principal risk factors associated with it).
- (2)
Promote and improve the ability to identify people with suicide risk (keep in mind physical and mental health problems).
- (3)
Provide helpful diagnostic tools that make said detection possible.
- (4)
Improve capacity of detection (diagnostic) and therapeutic management of emotion disorders.
- (5)
The potential to facilitate improvement in diagnostic capabilities and therapeutic management of other pathologies (or population groups) that are highly associated with carrying out suicidal behaviour within the programme implementation area (for example, alcohol dependency, the elderly, etc.).
- (6)
Recognise sex differences upon setting up educational programmes (specific training for management of males with suicide risk).
- (7)
Encourage collaboration with specialised support (psychiatry) and facilitate a proper referral for at-risk patients at that level.
- (8)
Initiate “review courses” every 2 years.
- (9)
Consider the greater effectiveness of multi-level educational programs (general practitioners, general public, facilitators, etc.).
- (10)
Accept the need for internal and external evaluation of the programme.
Given the complexity of the suicide phenomenon, there currently is no specific treatment for it, making the treatment of the underlying psychiatric pathology fundamental. Many suicidal patients are treated with a combination of psycho-pharmaceuticals that may include antidepressants, benzodiazepines, antipsychotics and mood stabilisers.107 Apart from the use of clozapine for schizophrenia108 and of lithium for bipolar disorder,109 there is still no specific treatment for suicidality. That is why treating the underlying psychiatric pathology is essential.
Anti-depressive pharmacological treatment, particularly selective serotonin reuptake inhibitors (SSRIs), corresponds with a drop in suicide rates.110,111 The antidepressant one chooses must first be totally effective and overdose-safe. Sedative antidepressants are often preferred, but if an SSRI is chosen, it may be coupled with a benzodiazepine. In the last few years, there have been several articles written about possible suicide inducement due to SSRI treatment, with these drugs being considered as possible factors responsible for disinhibition in depressive patients with previous suicidal ideation. Using antidepressants in children and adolescents especially has become the centre of the issue.112 In April of 2005, after reviewing available evidence, the European Medicines Agency suggested that SSRI or serotonin noradrenalin reuptake inhibitors (SNRI) not be used in treating children with depression.113 Aursnes et al.114 demonstrated an increased potential suicide risk with antidepressants (paroxetine) at the beginning of treatment and proposed possibly limiting their use to adults. The role of antidepressants in suicide risk seems to be age-dependent: in patients 25 years old or younger, antidepressants are associated with an increase in suicide risk similar to that observed in children; in adults 25–64 years old, using antidepressants does not seem to influence risk; and in those 65 years old or older, the treatment has a protective role against suicide risk.115 Other articles insist on the idea that mortality can be reduced with antidepressant treatment in adults with schizophrenia, especially by adding lithium,87,116,117 whose effectiveness is well-known in unipolar and bipolar patients.118,119 In any case, the effectiveness of a treatment should not be put before its safety.120
With schizophrenia it is necessary to identify at-risk patients, to treat depressive symptomatology and substance abuse specifically and to avoid side effects, especially akathisia, maintaining the antipsychotic effect and adherence to treatment.30,31 Studies with atypical antipsychotics are still not conclusive and only clozapine seems to have an anti-suicidal effect. Regardless, interruption of antipsychotic treatment is associated with an increase in suicide risk.121
Alcoholism is itself a suicide risk factor, but it is also a risk factor due to the comorbidity frequently associated with it: depression, schizophrenia, personality disorder and other substance abuse. Consequently, treatment of a patient with purposefully self-inflicted damage and alcoholism should also include treatment of the frequent comorbidity, especially depression.122
Some authors consider electroconvulsive therapy to be the treatment of choice in mood disorder patients with suicide risk, as the response is often quick, while antidepressants may require 4–6 weeks.107 Other authors highlight its indication in cases with signs of endogenisity.123 The availability of this treatment is one of the factors proposed to explain the assessed reduction of suicide risk in recent studies following-up mood disorders.124 A review of patients with mood disorders concluded that electroconvulsive therapy had a beneficial short-term effect in reducing suicide mortality, but not over the long-term.125 There is evidence in favour of the important effect that continuous antidepressant treatment after electroconvulsive therapy could have in suicide prevention for patients with severe depression.126
There are some promising data concerning the effectiveness of cognitive-behavioural type therapies; however, there are no conclusive results concerning relapse prevention and it is unclear as to which treatments are the most effective. Problem solving techniques seem particularly suitable. Brief psychodynamic interpersonal therapy can have an effective result for those who have attempted suicide, but more studies are needed to show this.87,122,127
Hawton and van Heeringen122 published a review of the effectiveness of psychosocial and pharmacological treatments for preventing recurrent suicide. The data cover the following types of psychosocial intervention: standard aftercare, problem solving therapy, accessible intensive healthcare upon release, provision of an emergency contact card, dialectical behaviour therapy, hospital behaviour therapy, insight-oriented hospital therapy, healthcare continuity (same therapist), change of healthcare (different therapist), general versus high dosage and long-term versus short-term therapy. These authors concluded that there is currently no evidence that would allow them to determine the most effective forms of treatment for patients with purposefully self-inflicted injury, making broader studies necessary. However, 2 interventions offered promising results:
- •
Problem solving therapy: cognitive therapy whose objective is to teach the patient effective alternative responses to solve problems.
- •
Providing an emergency contact card: a card that provides the patient with 24-h access to urgent counselling by a psychiatrist or to hospital admission.
Postvention or help for family members of patients that commit suicide should take place during the early stages of mourning, in order to create a therapeutic relationship that allows the family members to grieve.128 Psychotherapeutic work with family members may include the following129:
- (1)
Confronting the reality of guilt towards oneself and towards others.
- (2)
Helping to correct denials and distortions.
- (3)
Exploring the family members’ fantasies regarding how death will affect them in the future.
- (4)
Working with the anger and rage that this kind of death generates.
- (5)
Confronting the feeling of abandonment with reality.
WHO recommends support groups with the presence of others who have suffered a similar situation as the treatment of choice.130
Intervention in crisis can be defined as an actively influential process in psychological functioning during a period of imbalance, with the purpose of relieving the immediate impact of a stressful event, and of helping to reactive and strengthen the abilities and social resources of those affected.131 In a suicide crisis, the psychiatrist should distinguish between 4 types of patients, independently of whether an underlying psychiatric diagnosis exists or not:
- (1)
Patients who have survived a suicide attempt.
- (2)
Patients whose reason for consulting is suicidal ideation or impulses.
- (3)
Patients who inquire about other complaints, sometimes somatic, but who admit to having suicidal ideation later in the interview.
- (4)
Patients who, despite showing potentially suicidal pathological behaviour, deny having suicidal intentions.
The basic principals of intervention in a suicide crisis are as follows:
- (1)
Identifying the problem and establishing first contact with the suicidal patient.
- (2)
Determining the psychiatric diagnosis or, at least, achieving a syndromic approximation.
- (3)
Assessing the suicide risk.
- (4)
Establishing a therapeutic alliance.
- (5)
Choosing a treatment and a monitoring system.
- (1)
Confronting the suicide phenomenon is a priority in the mental health field as suicide is the primary cause of unnatural death in Spain. The demographic pattern of suicide in our field is characterised by a greater number of completed suicides in men and in those older than 65 years of age. In the last 20 years, Spain has evolved to be a country with a low to moderate suicide risk (WHO criteria).
- (2)
Confronting suicide is especially important in the youth population, given that it is the third cause of death in this age group (15–30 years old) in Spain, after traffic accidents and cancer-related deaths.
- (3)
The 2 principal risk factors for completed suicide are suicide attempts—more prevalent in women—and the presence of a psychiatric disorder. It is necessary to establish healthcare programmes, assessment and monitoring for patients who have attempted suicide. The cases that are identified and attended to in hospital emergency services represent an opportunity to initiate these programs.
- (4)
Suicide prevention should involve accurate detection, diagnosis and treatment of depressive disorders, schizophrenia, anxiety disorders, consumption of toxic substances and personality disorders, among other disorders.
- (5)
In our field there are hardly any specific prevention programmes, intervention protocols or cumulative case records available; and even if they exist, internal and external evaluations are infrequent. Promoting sectored databases through agreements with forensic science institutes is recommended.
- (6)
It is necessary to assess suicidal behaviour more thoroughly and systematically in the clinic, as well as to record the suicide risk assessment.
- (7)
The clinician should encourage self-control, self-esteem and the ability to face one's own individual problems and should promote greater participation and integration in family and social environments.
- (8)
The most effective strategies to prevent suicide include prescribing antidepressant medication to patients who suffer from depression and controlling access to means of committing suicide. Clozapine and lithium have been shown to have a protective effect against suicide in schizophrenic and bipolar patients, respectively. In any case, for patients with mental disorders and suicide risk, continuity of care and support should be ensured, in addition to appropriate treatment that includes verifying their adherence to the full dose of the medication.
- (9)
Programmes directed towards doctors to improve competency in identifying mental disorders and their management have shown to be effective in decreasing rates of suicidal behaviour. In addition, coordination between primary and specialised healthcare also help to decrease these rates.
- (10)
In the last few years, multi-level educational programmes have been directed not only towards primary healthcare physicians, but also towards the general population and social agents (teachers, firemen, law enforcement...), which has also shown to be effective.
Protection of human and animal subjects. The authors declare that no experiments were performed on humans or animals for this investigation.
Confidentiality of data. The authors declare that no patient data appear in this article.
Right to privacy and informed consent. The authors declare that no patient data appears in this article.
Conflict of interestThe authors have no conflict of interest to declare.
The Spanish Psychiatry Society (SEP), the Spanish Biological Psychiatry Society (SEPB) and the authors of this article appreciate the support for this publication through an unconditional grant from Adamed Laboratories. No employee from Adamed participated in any of the meetings or telephone conferences in which these recommendations were prepared, nor did they review or make any comments or suggestions about the content of this manuscript.
Aguilar García-Iturrospe, Eduardo; Arango López, Celso; Artamendi Larrañaga, María; Blanco Garrote, José Antonio; Blasco Fontecilla, Hilario; Bousoño García, Manuel; Braqueais Conesa, Dolores; Carballo Belloso, Juan José; Cervilla Ballesteros, Jorge; Costillas Pérez, Lucía; Díaz Marsá, Marina; Díaz, Ana; Dueñas Herrero, Rosa M.ª; España, Antonio; Ferrer Gómez del Valle, Ernesto; Garcia Marco, Ramón; García-Portilla González, M.ª Paz; Guija Villa, Julio Antonio; Hernández Alvarez, Matilde; Herran Gómez, Andrés; Huertas Sánchez, David; Ibañez Cuadrado, Angela; Jiménez Treviño, Luis; López Castroman, Jorge; Moreno Pardillo, Dolores; Navío Acosta, Mercedes; Nieto Rodriguez, Evaristo; Palao Vidal, Diego; Páramo Fernández, Mario; Parra Uribe, Isabel; Peleteiro, Sita; Pereiro Gómez, César; Pozo Navarro, Pedro; Querejeta Ayerdi, Imanol; Quesada Franco, Marta; Reneses Prieto, Blanca; Roca Bennasar, Miquel; Ros Montalbán, Salvador; Sáiz González, M.ª Dolores; Serrano Vázquez, Manuel; Tejedor Azpeitia, Carmen; Valle Fernández, Jesús.
Please cite this article as: Ayuso-Mateos JL, et al. Recomendaciones preventivas y manejo del comportamiento suicida en España. Rev Psiquiatr Salud Ment (Barc.). 2012;5(1):8-23.
RECOMS Group (Appendix 1).