There has been little change in the incidence of suicidal behaviour and reattempts in recent years. Evidence is needed on the incidence of suicidal behaviour in the psychiatric population and its follow-up.
Material and methodA prospective multi-centre case–control study. The sample covered the cases of 440 patients seen as psychiatric emergencies. For this purpose, we used the Vital Adverse Event Scale by Brugha and screening with the Columbia Scale. The sample was divided into three groups: patients without prior suicide attempts, patients with an index attempt and patients with more than one attempt. At two years, the clinical histories of these patients were reviewed, assessing for suicidal behaviour.
ResultsA total of 49.1% (n=216) of the patients required urgent psychiatric care during the follow-up period, and 2.7% eventually committed suicide. The data shows a differential profile between the three groups analysed. Among them, the group of reattempters required the highest number of interventions regarding suicide behaviour (11.0%; χ2=30.3; d.f.=2; p<.001). Eventually, 6.1% of the patients without prior suicide attempts tried to commit suicide for the first time, and 21.7% (n=60) of the remaining sample repeated their prior attempts. The highest risk of attempt was in the thirty days following the urgent intervention. After this period, risk distribution varied for each group. Three items from the Columbia Scale predict suicide behaviour.
ConclusionsThe results show the need for assessing suicidal behaviour for all patients who receive psychiatric urgent care, including during the follow-up period. A more thorough control should be performed during the first months for patients without prior suicide attempts, and longer periods for those patients who have already tried to commit suicide.
La incidencia de la repetición de conductas suicidas no ha variado en los últimos años. Es necesario aportar evidencias sobre la incidencia de la conducta suicida en población psiquiátrica y su seguimiento.
Material y métodoEstudio multicéntrico caso-control, prospectivo. La muestra se compuso de 440 pacientes atendidos en los servicios de urgencias de psiquiatría. Se aplicó la Escala de acontecimientos vitales adversos de Brugha y la Escala Columbia de cribado del riesgo suicida. La muestra se dividió en tres grupos: pacientes sin intentos de suicidio previos, pacientes index y pacientes con más de un intento. A los dos años se revisaron las historias clínicas de dichos pacientes analizando la presencia de conducta suicida.
ResultadosEl 49,1% (n=216) repitieron atención en urgencias de psiquiatría en el periodo de seguimiento. El 2,7% fallecieron por suicidio. Se ha encontrado un perfil diferencial entre los tres grupos estudiados. El grupo de los repetidores fue el que más atenciones recibió con relación a conductas suicidas (11,0%; χ2=30,3; g.l.=2; p<0,001). El 6,1% (n=10) de los pacientes que nunca habían tenido un intento realizaron su primer intento, y el 21,7% (n=60) del resto de la muestra lo repitieron. El mayor riesgo de intento fue en los 30días siguientes a la atención en urgencias. Pasado ese tiempo, la distribución del riesgo varía en cada grupo. Tres ítems de la Escala Columbia predicen las conductas suicidas.
ConclusionesEs necesario valorar el riesgo de conductas suicidas en todos los pacientes que acuden a urgencias de psiquiatría y durante su seguimiento. Este debería ser más intenso en los primeros meses para quienes no tienen intentos previos, y a más largo plazo para quienes ya lo han intentado.
Suicide attempts are very prevalent and constitute a major public health problem.1 Non-lethal attempts account for 10–20% of total care in psychiatric emergency departments.2 A crucial area for further research is the relationship between completed suicides and suicide attempts.
It is estimated that about two thirds of suicide deaths occur at the first attempt.3 However, from a clinical perspective an attempt is a clear risk factor, since among those who survive, the probability of dying in a subsequent attempt is 40–66 times greater than in the general population.4 A systematic review of 90 studies estimated that 16% of those who had made a non-fatal attempt reattempted after one year, and 2% completed suicide. The suicide death rate increased to 7% after 9 years.5
However, some methodological limitations could underestimate the relevance of this problem. For example, not considering previous suicide attempts in the subjects’ full history, but only in the study period, or using convenience samples, which have limited generalisation.
Taking these limitations into account, a cohort study that followed a sample of patients who had made a first attempt for between 3 and 25 years found a suicide rate of 5.9%. Of the deaths, 59.3% occurred on the first attempt, and 80% of those who committed suicide subsequently did so in the first year. Therefore, research should focus on identifying populations vulnerable to first attempts and on reducing the risk of these groups.6,7
People with mental disorders would be one of the main groups. After a first suicide attempt, the risk of death by suicide is highest between the first 6 months to one year following the attempt, with the risk increasing if the individual has a severe mental disorder.8 In fact, a population cohort study found that the absolute risk of suicide among mental disorders is 2–8%, a risk that doubles in all diagnostic groups after a non-fatal suicide attempt.9
A promising line of research is based on analysing the clinical differences between those who have made a single suicide attempt and those who make more than one. Patients who repeat would be more vulnerable and at greater risk of certain adverse life events or changes in their psychopathological situation.10
The specific contribution of this study is to provide more evidence to identify specific risk factors for suicidal behaviour recurrence in vulnerable populations. In particular, in this research study the suicidal behaviours of patients attended in the psychiatric emergency department was followed up for two years by identifying the differences between patients who had not made a suicide attempt, those who had made an index attempt and those who had made more than one suicide attempt.
The objectives of this study are: (1) to analyse the differential profile of patients attended in the psychiatric emergency department according to previous suicide attempts (without a prior suicide attempt, index and reattempters); (2) to learn at what point after care in the psychiatric emergency department attempts or completed suicides might occur, and (3) to determine the factors that predict such behaviour.
Material and methodThe Clinical Research Ethics Committee of the Government of Navarra's Department of Health authorised this research study (project n. 95/2014). In this study, all patients attended due to a suicide attempt in the emergency departments of the Hospital Complex of Navarra and the Hospital ‘Reina Sofía’ in Tudela between January and October 2015 (n=207) and a sample of patients who attended in the same period for a reason other than the suicide attempt (n=233) were followed up. For this purpose, once a patient was identified as a suicide attempter, the next patient who was not attended for that reason was recruited. The final sample comprised 440 patients. A previous study compared the differences between cases and controls at the time they were attended in the ED. No differential profile was found between the two groups.11
In this prospective multicentre case–control study, any self-inflicted, potentially harmful behaviour with a non-fatal outcome for which there is explicit or implicit evidence of intention to die was considered a suicide attempt.12
The criteria for inclusion were to be over the age of 18, having attended the psychiatric emergency department and having signed informed consent. The criteria for exclusion were not agreeing to participate, being unable to respond, having difficulty with the language or an intellectual disability.
InstrumentsA protocol was applied that included sociodemographic variables, clinical variables and a psychiatric assessment.
The sociodemographic variables collected were age, sex, marital status, place of birth, occupation, educational level, socioeconomic level, domestic situation, children and religious belief.
The clinical variables assessed were: personal history of mental disorder, previous suicide attempts, disabling physical illness (diagnosed medical illness with functional and chronic repercussions), family history of suicide, previous care in the psychiatric emergency department, previous admissions to the psychiatric ward, current mental health care, psychopharmacological treatment, current social/family support, family history of mental disorder, medication adjustment in the emergency department and main clinical diagnosis in the emergency department according to the International Classification of Diseases (ICD-10).13
In the psychiatric assessment, Brugha's adverse life events scale14 and the Columbia Suicide-Severity Rating Scale (C-SSRS)15 for screening for suicidal ideation were used.
Brugha's adverse life events scale is an inventory that uses 12 dichotomous items to examine a patient's life events over the past 6 months. The greater the number of events, the greater the severity.
The Columbia Suicide-Severity Rating Scale (C-SSRS)15 is a semi-structured interview that captures the severity and intensity of suicidal ideation, behaviour and lethality. It has recently been validated with a Spanish sample.16 This project uses the screening version, which includes 5 types of ideation of increasing severity with a 5-point ordinal scale (from 1=wish to be dead to 5=active suicidal ideation with specific plan and intent) and a last question for suicidal behaviour. Questions 3–5 are only asked if the patient has responded yes to question 2.
The clinical variables that were collected at two years were: being in mental health treatment, repeat care in the psychiatric emergency department, repeat autolytic attempt, method used, death by suicide or other causes during follow-up.
ProcedureIn this two-year follow-up study, the 440 patients evaluated were divided into three groups based on the suicide attempts recorded in their medical records at the time of inclusion in the study: (1) patients without a prior suicide attempt (n=163; 37.0%); (2) patients with an index attempt (index; n=153; 34.8%), and (3) patients with more than one attempt (n=124; 28.2%). This means that, at the time of starting the study, 100% of the patients in the group without attempts attended the psychiatric emergency department for a reason other than a suicide attempt. In the index group of patients, 113 (73.9%) were recruited because they had attended for a suicide attempt, and 94 (75.8%) in the group with more than one attempt.
Two years after the initial evaluation, each of the patients’ computerised clinical histories was reviewed and the variables included in the follow-up were collected. Patient deaths were coded in the clinical records. When a patient was found to have died, it was checked with the Institute of Forensic Medicine whether the cause was suicide.
Data analysisAll analyses were carried out using SPSS software (v. 15.0). First, comparisons were made between the different subgroups using the χ2 test or analysis of variance depending on the nature of the variables used. Secondly, a Kaplan–Meier survival analysis was performed for suicide attempts and/or completed suicides. Calculations of the significance of the differences found were made using log-rank tests. Probabilities less than .05 were considered statistically significant. Finally, two Cox regression models were performed to identify possible risk or protective factors for suicide attempts and completed suicide during the follow-up. Those that had shown p values greater than .20 in inter-group comparisons were included as covariates. The conditional forward method was used for selection of variables. High b values indicate a higher risk of self-harm attempt.
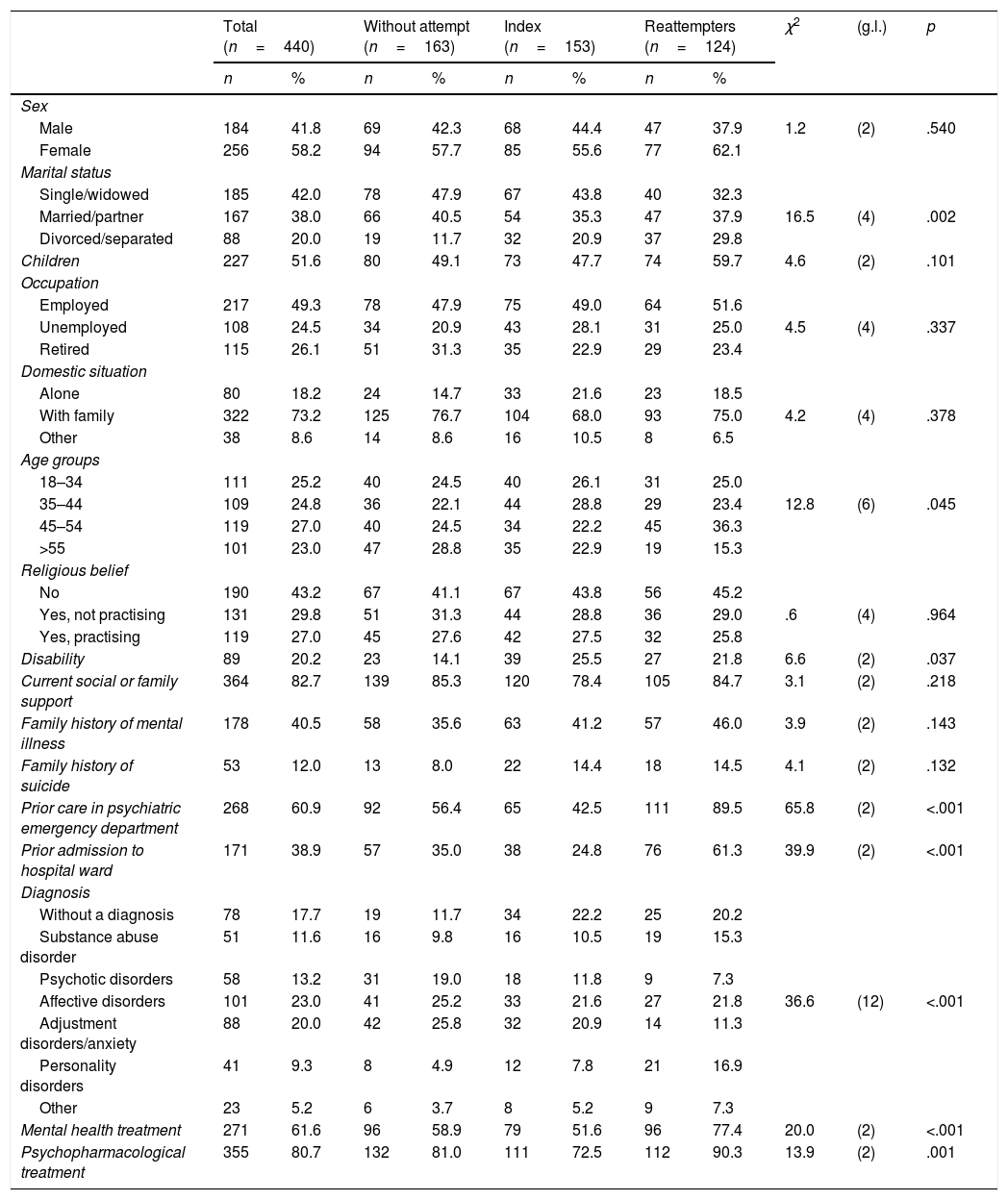
ResultsDifferences between patients according to previous suicide attemptsTable 1 presents the differences between the three groups of patients in socio-demographic and clinical variables at the beginning of follow-up. Those who had more than one suicide attempt in their history were more likely to be divorced/separated, the 45–54 age group range predominated, they had received more previous care in the psychiatric emergency department, more admissions to the psychiatric ward and had more substance use and personality disorders. In addition, a greater proportion of them were under mental health follow-up and psychopharmacological treatment.
Comparison in socio-demographic and clinical variables at the start of follow-up.
| Total (n=440) | Without attempt (n=163) | Index (n=153) | Reattempters (n=124) | χ2 | (g.l.) | p | |||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| n | % | n | % | n | % | n | % | ||||
| Sex | |||||||||||
| Male | 184 | 41.8 | 69 | 42.3 | 68 | 44.4 | 47 | 37.9 | 1.2 | (2) | .540 |
| Female | 256 | 58.2 | 94 | 57.7 | 85 | 55.6 | 77 | 62.1 | |||
| Marital status | |||||||||||
| Single/widowed | 185 | 42.0 | 78 | 47.9 | 67 | 43.8 | 40 | 32.3 | |||
| Married/partner | 167 | 38.0 | 66 | 40.5 | 54 | 35.3 | 47 | 37.9 | 16.5 | (4) | .002 |
| Divorced/separated | 88 | 20.0 | 19 | 11.7 | 32 | 20.9 | 37 | 29.8 | |||
| Children | 227 | 51.6 | 80 | 49.1 | 73 | 47.7 | 74 | 59.7 | 4.6 | (2) | .101 |
| Occupation | |||||||||||
| Employed | 217 | 49.3 | 78 | 47.9 | 75 | 49.0 | 64 | 51.6 | |||
| Unemployed | 108 | 24.5 | 34 | 20.9 | 43 | 28.1 | 31 | 25.0 | 4.5 | (4) | .337 |
| Retired | 115 | 26.1 | 51 | 31.3 | 35 | 22.9 | 29 | 23.4 | |||
| Domestic situation | |||||||||||
| Alone | 80 | 18.2 | 24 | 14.7 | 33 | 21.6 | 23 | 18.5 | |||
| With family | 322 | 73.2 | 125 | 76.7 | 104 | 68.0 | 93 | 75.0 | 4.2 | (4) | .378 |
| Other | 38 | 8.6 | 14 | 8.6 | 16 | 10.5 | 8 | 6.5 | |||
| Age groups | |||||||||||
| 18–34 | 111 | 25.2 | 40 | 24.5 | 40 | 26.1 | 31 | 25.0 | |||
| 35–44 | 109 | 24.8 | 36 | 22.1 | 44 | 28.8 | 29 | 23.4 | 12.8 | (6) | .045 |
| 45–54 | 119 | 27.0 | 40 | 24.5 | 34 | 22.2 | 45 | 36.3 | |||
| >55 | 101 | 23.0 | 47 | 28.8 | 35 | 22.9 | 19 | 15.3 | |||
| Religious belief | |||||||||||
| No | 190 | 43.2 | 67 | 41.1 | 67 | 43.8 | 56 | 45.2 | |||
| Yes, not practising | 131 | 29.8 | 51 | 31.3 | 44 | 28.8 | 36 | 29.0 | .6 | (4) | .964 |
| Yes, practising | 119 | 27.0 | 45 | 27.6 | 42 | 27.5 | 32 | 25.8 | |||
| Disability | 89 | 20.2 | 23 | 14.1 | 39 | 25.5 | 27 | 21.8 | 6.6 | (2) | .037 |
| Current social or family support | 364 | 82.7 | 139 | 85.3 | 120 | 78.4 | 105 | 84.7 | 3.1 | (2) | .218 |
| Family history of mental illness | 178 | 40.5 | 58 | 35.6 | 63 | 41.2 | 57 | 46.0 | 3.9 | (2) | .143 |
| Family history of suicide | 53 | 12.0 | 13 | 8.0 | 22 | 14.4 | 18 | 14.5 | 4.1 | (2) | .132 |
| Prior care in psychiatric emergency department | 268 | 60.9 | 92 | 56.4 | 65 | 42.5 | 111 | 89.5 | 65.8 | (2) | <.001 |
| Prior admission to hospital ward | 171 | 38.9 | 57 | 35.0 | 38 | 24.8 | 76 | 61.3 | 39.9 | (2) | <.001 |
| Diagnosis | |||||||||||
| Without a diagnosis | 78 | 17.7 | 19 | 11.7 | 34 | 22.2 | 25 | 20.2 | |||
| Substance abuse disorder | 51 | 11.6 | 16 | 9.8 | 16 | 10.5 | 19 | 15.3 | |||
| Psychotic disorders | 58 | 13.2 | 31 | 19.0 | 18 | 11.8 | 9 | 7.3 | |||
| Affective disorders | 101 | 23.0 | 41 | 25.2 | 33 | 21.6 | 27 | 21.8 | 36.6 | (12) | <.001 |
| Adjustment disorders/anxiety | 88 | 20.0 | 42 | 25.8 | 32 | 20.9 | 14 | 11.3 | |||
| Personality disorders | 41 | 9.3 | 8 | 4.9 | 12 | 7.8 | 21 | 16.9 | |||
| Other | 23 | 5.2 | 6 | 3.7 | 8 | 5.2 | 9 | 7.3 | |||
| Mental health treatment | 271 | 61.6 | 96 | 58.9 | 79 | 51.6 | 96 | 77.4 | 20.0 | (2) | <.001 |
| Psychopharmacological treatment | 355 | 80.7 | 132 | 81.0 | 111 | 72.5 | 112 | 90.3 | 13.9 | (2) | .001 |
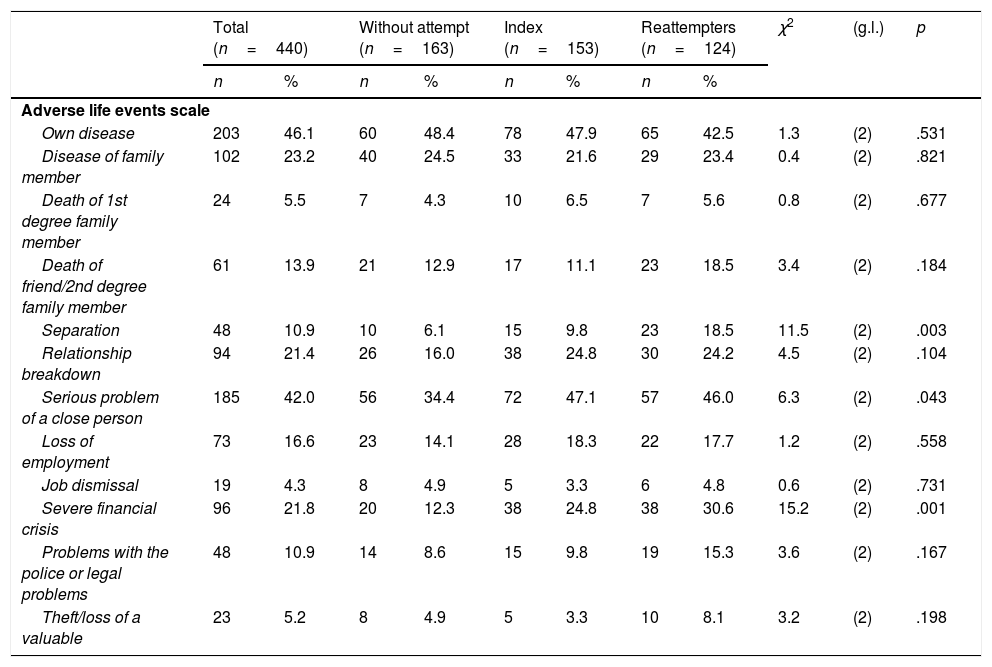
Table 2 presents the differences between the three groups in terms of the adverse life events scale and the Columbia Suicide-Severity Rating Scale. Patients in the reattempter group accumulated a greater number of psychosocial stressors, followed by those in the index group. With regard to the Columbia Suicide-Severity Rating Scale, the differences are between those without prior suicide attempts and the other two groups.
Comparison in the Brugha Scale and Columbian Scale at start of follow-up.
| Total (n=440) | Without attempt (n=163) | Index (n=153) | Reattempters (n=124) | χ2 | (g.l.) | p | |||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| n | % | n | % | n | % | n | % | ||||
| Adverse life events scale | |||||||||||
| Own disease | 203 | 46.1 | 60 | 48.4 | 78 | 47.9 | 65 | 42.5 | 1.3 | (2) | .531 |
| Disease of family member | 102 | 23.2 | 40 | 24.5 | 33 | 21.6 | 29 | 23.4 | 0.4 | (2) | .821 |
| Death of 1st degree family member | 24 | 5.5 | 7 | 4.3 | 10 | 6.5 | 7 | 5.6 | 0.8 | (2) | .677 |
| Death of friend/2nd degree family member | 61 | 13.9 | 21 | 12.9 | 17 | 11.1 | 23 | 18.5 | 3.4 | (2) | .184 |
| Separation | 48 | 10.9 | 10 | 6.1 | 15 | 9.8 | 23 | 18.5 | 11.5 | (2) | .003 |
| Relationship breakdown | 94 | 21.4 | 26 | 16.0 | 38 | 24.8 | 30 | 24.2 | 4.5 | (2) | .104 |
| Serious problem of a close person | 185 | 42.0 | 56 | 34.4 | 72 | 47.1 | 57 | 46.0 | 6.3 | (2) | .043 |
| Loss of employment | 73 | 16.6 | 23 | 14.1 | 28 | 18.3 | 22 | 17.7 | 1.2 | (2) | .558 |
| Job dismissal | 19 | 4.3 | 8 | 4.9 | 5 | 3.3 | 6 | 4.8 | 0.6 | (2) | .731 |
| Severe financial crisis | 96 | 21.8 | 20 | 12.3 | 38 | 24.8 | 38 | 30.6 | 15.2 | (2) | .001 |
| Problems with the police or legal problems | 48 | 10.9 | 14 | 8.6 | 15 | 9.8 | 19 | 15.3 | 3.6 | (2) | .167 |
| Theft/loss of a valuable | 23 | 5.2 | 8 | 4.9 | 5 | 3.3 | 10 | 8.1 | 3.2 | (2) | .198 |
| M | d.t. | M | d.t. | M | d.t. | M | d.t. | F | |
|---|---|---|---|---|---|---|---|---|---|
| Total adverse life events | 2.2 | 1.5 | 1.9 | 1.5 | 2.2 | 1.4 | 2.6 | 1.5 | 8.3 |
| Columbia Suicide-Severity Rating Scale | n | % | n | % | n | % | n | % | χ2 | (g.l.) | p |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Wish to be dead | 346 | 78.6 | 91 | 55.8 | 140 | 91.5 | 115 | 92.7 | 80.3 | (2) | <.001 |
| Non-specific Active Suicidal thoughts | 262 | 59.5 | 38 | 23.3 | 119 | 77.8 | 105 | 84.7 | 142.5 | (2) | <.001 |
| Active suicidal ideation without intent to act (n=262) | 215 | 82.1 | 28 | 73.7 | 95 | 79.8 | 92 | 87.6 | 4.4 | (2) | .110 |
| Active suicidal ideation with some intent to act without specific plan (n=262) | 171 | 65.3 | 19 | 50.0 | 79 | 66.4 | 73 | 69.5 | 4.8 | (2) | .090 |
| Active suicidal ideation with intent and plan (n=262) | 91 | 34.7 | 6 | 15.8 | 49 | 41.2 | 36 | 34.3 | 8.2 | (2) | .017 |
| Suicidal behaviour | 101 | 23.0 | 5 | 3.1 | 56 | 36.6 | 40 | 32.3 | 58.6 | (2) | <.001 |
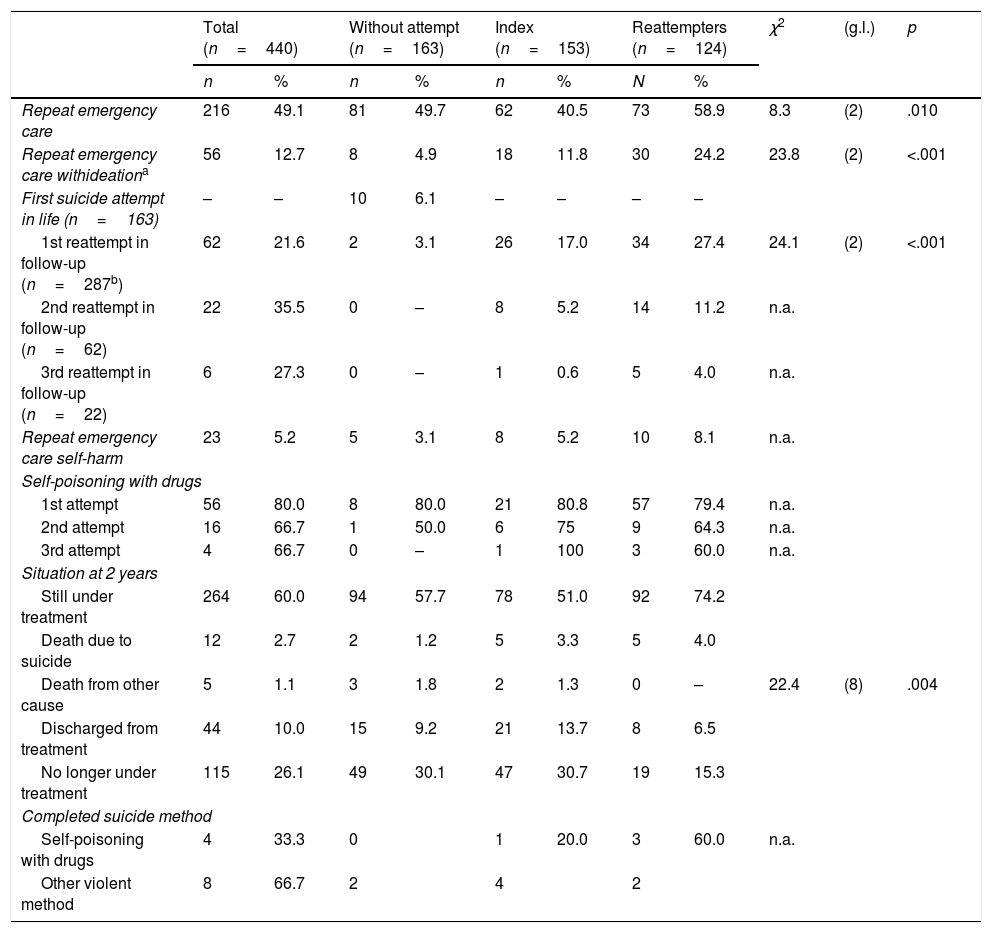
Table 3 shows the comparison as follow-up progressed between the three groups assessed. A total of 216 patients (49.1%) were re-attended in the psychiatric emergency department during follow-up. During this period 102 patients (23.2%) were attended for suicidal ideation (n=56; 12.7%) and/or for self-harm attempts (n=46; 10.5%). The group with the highest percentage of care related to suicidal behaviour was that of the reattempters (38.7%; n=48), followed by the index group (23.5%; n=36) and those without an attempt (11.0%; n=18; 2=30.3; g.l.=2; p<.001).
Comparison of progression in follow-up.
| Total (n=440) | Without attempt (n=163) | Index (n=153) | Reattempters (n=124) | χ2 | (g.l.) | p | |||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| n | % | n | % | n | % | N | % | ||||
| Repeat emergency care | 216 | 49.1 | 81 | 49.7 | 62 | 40.5 | 73 | 58.9 | 8.3 | (2) | .010 |
| Repeat emergency care withideationa | 56 | 12.7 | 8 | 4.9 | 18 | 11.8 | 30 | 24.2 | 23.8 | (2) | <.001 |
| First suicide attempt in life (n=163) | – | – | 10 | 6.1 | – | – | – | – | |||
| 1st reattempt in follow-up (n=287b) | 62 | 21.6 | 2 | 3.1 | 26 | 17.0 | 34 | 27.4 | 24.1 | (2) | <.001 |
| 2nd reattempt in follow-up (n=62) | 22 | 35.5 | 0 | – | 8 | 5.2 | 14 | 11.2 | n.a. | ||
| 3rd reattempt in follow-up (n=22) | 6 | 27.3 | 0 | – | 1 | 0.6 | 5 | 4.0 | n.a. | ||
| Repeat emergency care self-harm | 23 | 5.2 | 5 | 3.1 | 8 | 5.2 | 10 | 8.1 | n.a. | ||
| Self-poisoning with drugs | |||||||||||
| 1st attempt | 56 | 80.0 | 8 | 80.0 | 21 | 80.8 | 57 | 79.4 | n.a. | ||
| 2nd attempt | 16 | 66.7 | 1 | 50.0 | 6 | 75 | 9 | 64.3 | n.a. | ||
| 3rd attempt | 4 | 66.7 | 0 | – | 1 | 100 | 3 | 60.0 | n.a. | ||
| Situation at 2 years | |||||||||||
| Still under treatment | 264 | 60.0 | 94 | 57.7 | 78 | 51.0 | 92 | 74.2 | |||
| Death due to suicide | 12 | 2.7 | 2 | 1.2 | 5 | 3.3 | 5 | 4.0 | |||
| Death from other cause | 5 | 1.1 | 3 | 1.8 | 2 | 1.3 | 0 | – | 22.4 | (8) | .004 |
| Discharged from treatment | 44 | 10.0 | 15 | 9.2 | 21 | 13.7 | 8 | 6.5 | |||
| No longer under treatment | 115 | 26.1 | 49 | 30.1 | 47 | 30.7 | 19 | 15.3 | |||
| Completed suicide method | |||||||||||
| Self-poisoning with drugs | 4 | 33.3 | 0 | 1 | 20.0 | 3 | 60.0 | n.a. | |||
| Other violent method | 8 | 66.7 | 2 | 4 | 2 | ||||||
n.a.: not applicable (excess categories).
Over the period studied, 6.1% (n=10) of patients who had never made an attempt made their first attempt. Among patients in the index and reattempter groups, 21.7% (n=60) made a total of 93 new suicide attempts.
Of the sample, 3.8% died during follow-up (n=17). Of these, 12 patients died by suicide (2.7% of the total sample). Among the 12 suicide deaths, 9 died on their first attempt after the start of follow-up: 2 with no previous attempts (1.2% of the without an attempt group); 2 of the index group (1.3%) and 5 of the reattempters’ group (4.0%). The remaining three cases died on the second attempt and belonged to the index group (2.0% of their group).
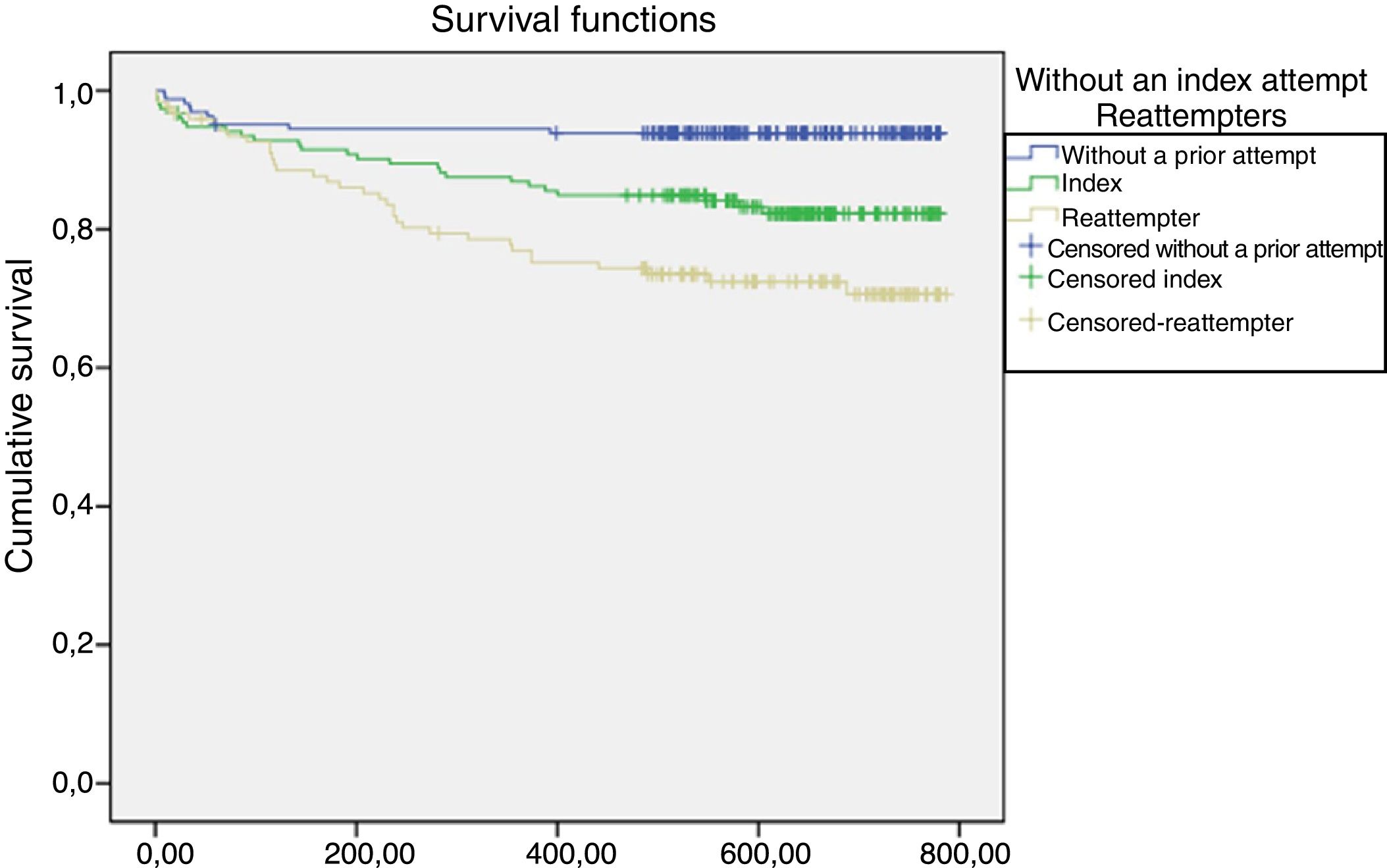
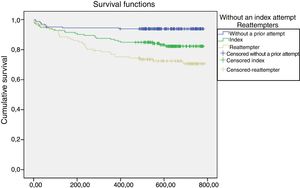
Timing of suicide attempts according to groupFig. 1 shows the cumulative proportion of surviving patients (who had not made a suicide attempt).
In terms of the timing of first suicide attempt in the follow-up, a statistically significant difference was found between the three groups analysed (Fig. 1). Of the attempts and/or suicides, 24.3% (n=17) occurred in the first 30 days after care in the emergency department, with different distribution among the groups: among those without a prior attempt 40% (n=4); among those who had made an index attempt 30.8% (n=8), and 17.7% (n=5) among those who had made more than one attempt.
In the case of patients without a prior attempt, a further 40% (n=4) of the attempts were made in the second month. From the fourth month onwards, in which the reattempters had made 6 attempts (17.64%), the evolution of the attempts between the index group and the reattempters is very similar.
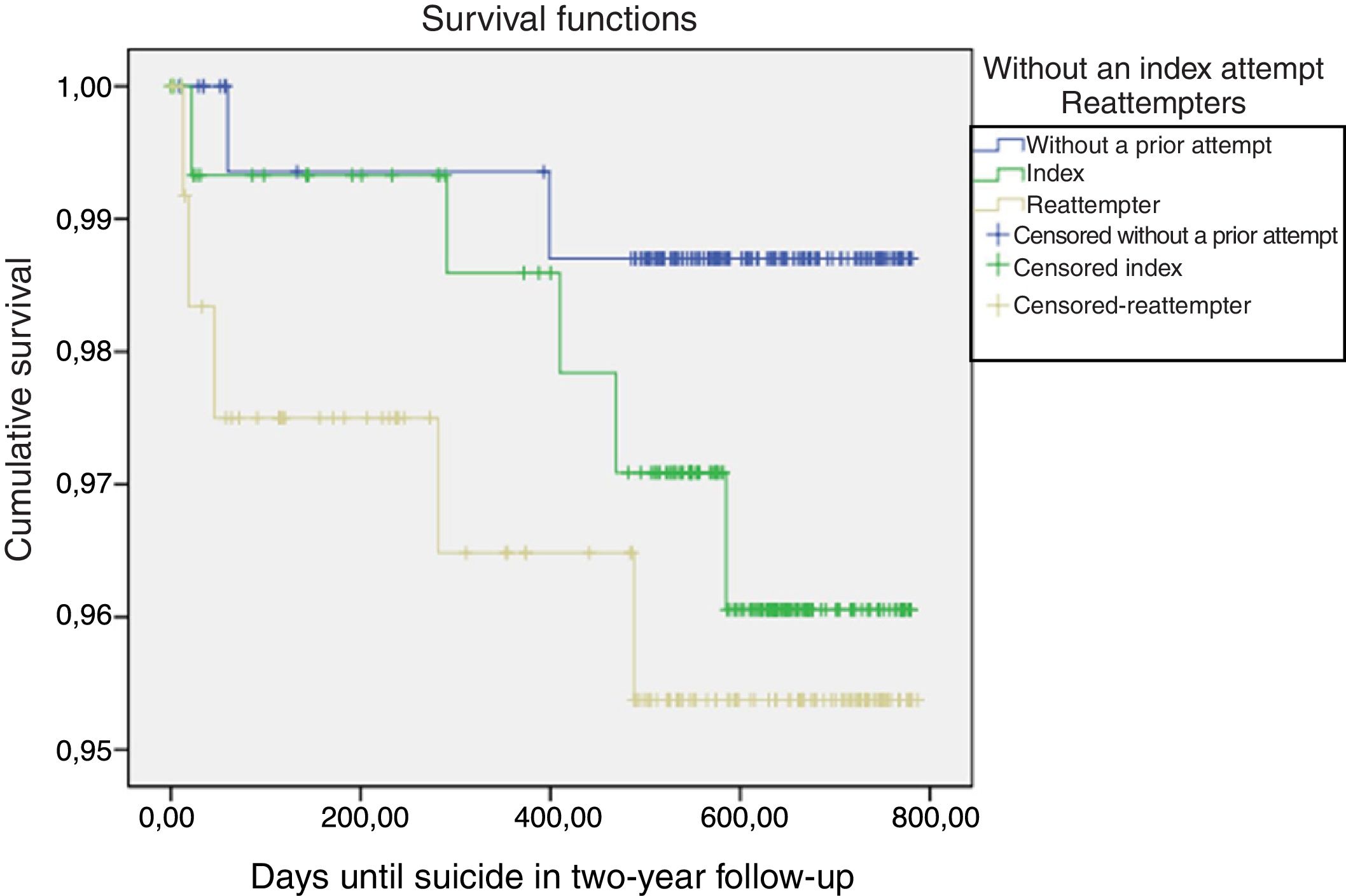
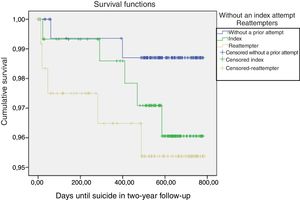
In terms of completed suicides, no statistically significant difference was found between the three groups (Fig. 2). Five of the 12 completed suicides occurred in the first two months after care in the psychiatric emergency department: one involved a person who had not made any prior attempts, another after an index attempt and three who had already made prior attempts. The remaining deaths occurred after more than 282 days.
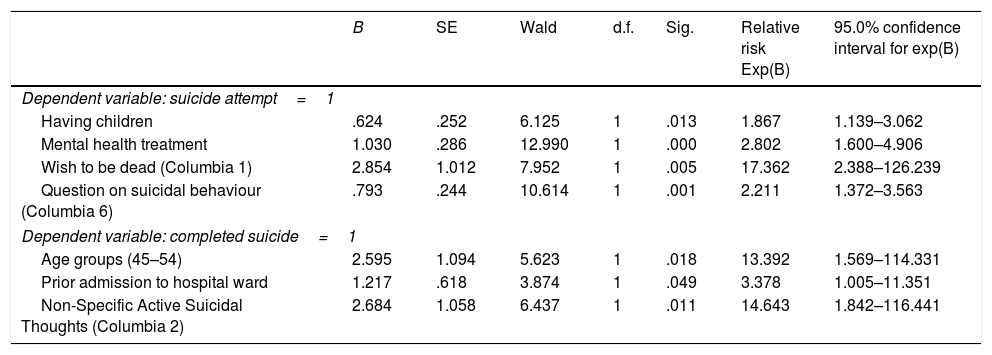
Variables predictive of suicide attempts and suicidesThe estimated coefficients for the variables that make up the final Cox regression models are presented in Table 4. The four variables that predict an attempt in follow-up are being under mental health treatment, intention to engage in suicidal behaviour, expressing a wish to be dead, and having children. For suicide, in follow-up, the predictor variables are having had non-specific active thoughts of suicide, aged between 45 and 54 and having had a prior admission to the psychiatric ward.
Risk factors for suicide attempts and completed suicide.
| B | SE | Wald | d.f. | Sig. | Relative risk Exp(B) | 95.0% confidence interval for exp(B) | |
|---|---|---|---|---|---|---|---|
| Dependent variable: suicide attempt=1 | |||||||
| Having children | .624 | .252 | 6.125 | 1 | .013 | 1.867 | 1.139–3.062 |
| Mental health treatment | 1.030 | .286 | 12.990 | 1 | .000 | 2.802 | 1.600–4.906 |
| Wish to be dead (Columbia 1) | 2.854 | 1.012 | 7.952 | 1 | .005 | 17.362 | 2.388–126.239 |
| Question on suicidal behaviour (Columbia 6) | .793 | .244 | 10.614 | 1 | .001 | 2.211 | 1.372–3.563 |
| Dependent variable: completed suicide=1 | |||||||
| Age groups (45–54) | 2.595 | 1.094 | 5.623 | 1 | .018 | 13.392 | 1.569–114.331 |
| Prior admission to hospital ward | 1.217 | .618 | 3.874 | 1 | .049 | 3.378 | 1.005–11.351 |
| Non-Specific Active Suicidal Thoughts (Columbia 2) | 2.684 | 1.058 | 6.437 | 1 | .011 | 14.643 | 1.842–116.441 |
Survival analysis: Cox regression model.
This study found a differential profile between patients who attended the psychiatric emergency department without a prior suicide attempt, those with only one attempt and those with more than one attempt. In addition, it was shown that in the 30 days following a visit to the emergency department there is a high risk of a suicide attempt (whether one had made one before or not) and that after the first 30 days the distribution of risk varies in each of the three groups studied. Specific items on the Columbia Scale were found to be predictive variables in the case of subsequent attempts and completed suicides.
With regard to the profile of the three groups of patients, as previously shown, no statistically significant differences were obtained in relation to sex or age. A greater presence of people who were separated was found among the reattempters,17 together with a higher prevalence of personality and substance abuse disorders. It is precisely these two diagnoses that have been identified as risk factors for repeated suicide attempts18–20 and for completed suicide.7 The group of reattempters also presented greater psychiatric comorbidity, more suicidal ideation, a greater number of psychiatric hospitalizations and more were under psychiatric treatment.10,21,22 In short, greater clinical severity is deduced than in the other two groups. In addition, they have more stressful life events, related to economic and/or emotional losses. These losses, together with a possible cumulative effect of stressors throughout life and axis II disorders, could favour repetition of suicidal behaviours.23
Patients’ therapeutic adherence is a factor that could prevent the repetition of suicidal behaviours. Patients with follow-up are less likely to repeat a suicide attempt in the first year, although this effect has not been confirmed in the long term6,24 and the risk of suicide mortality is higher among those who refuse follow-up.25 Unlike other studies in which half of the people attended in the ED for a suicide attempt are not subsequently followed up in mental health,26 in this sample 60% of the patients were in treatment, and an additional 10% had been discharged from treatment within the period. Furthermore, most of the reattempters were in treatment at the time of the attempt and were still in treatment after two years. Unfortunately, these data indicate that in some patients the intervention offered did not result in prevention of suicidal behaviour,6 and therefore they will have to be offered other therapeutic alternatives. Even so, there is a need to innovate adherence strategies, since in the case of the no prior attempt and index groups one third of the patients were no longer under treatment.
With regard to reattempt rates, in this study, with a very specific sample of patients attended in the psychiatric emergency department, it was found that: (1) 21% of the sample with a prior suicide attempt repeated it over the two years of follow-up; (2) 6.1% of those with no prior attempt made an attempt for the first time, and (3) 2.7% died for this reason. These data are similar to those of previous studies.5,20,27,28 The number of completed suicides was the same for the index group as for the group of reattempters. However, three cases of the index group were in fact reattempters (they had made another attempt during the follow-up), therefore these data support the hypothesis that the likelihood of completing suicide is proportional to the number of attempts.18,29
In this study, the 30 days following a visit to the emergency department carried a high risk of suicide attempt (whether or not a prior attempt had been made). After the first 30 days, the distribution of risk varies in each of the three groups studied. The main finding for those without a prior suicide attempt was that the most critical period is the first two months after emergency care. This flags up the vulnerability of the patient attended in the psychiatric emergency department and the need for suicide risk assessment along with intensive follow-up after emergency care. For those with only one attempt, the most critical period is the first four months, and among reattempters the following year,28 therefore these patients would benefit from more extensive follow-up.
Being under mental health treatment is one of the variables predictive of a repeat suicide attempt. The characteristics of the sample suggest that these are severely ill patients who are more vulnerable to repeated suicidal behaviour, even though they are part of the health system. Being in the system is likely to prolong the time between repeat attempts. For those cases where mental health treatment does not prevent a repeat attempt, more specific psychotherapeutic interventions need to be investigated, as well as the use of other short contact alternatives that could reduce the frequency of reattempts.28
With respect to completed suicides, one of the predictors already reported in other studies30,31 is a previous admission to the psychiatric unit prior to the date of emergency care. Furthermore, a recent meta-analysis adds that there is a 30 times greater risk even years after discharge.32
Three items on the Columbia Scale have been found to be predictive of suicide attempts as well as completed suicides. The items that assess a wish to die and active suicidal ideation have previously been found to be good predictors of suicidal behaviour.33,34 In this research study, despite the fact that the suicide scales show low sensitivity and have psychometric and conceptual flaws,35 these items have had good predictive validity. It would be advisable to include this scale in emergency care as screening.
This paper has some limitations that may affect generalisation of the conclusions. The study was carried out only in the context of psychiatric emergencies and therefore the results obtained are limited to patients who have attended a psychiatric emergency department at some time (regardless of the reason for the consultation). Furthermore, the data collected in the follow-up were obtained from the Computerised Clinical History of the Community of Navarra. This means that there is a lack of data for patients who may have received some care in another community, and therefore some data may have been underestimated. Finally, the percentages presented in this study may vary depending on how the different subsamples are considered, and therefore care must be taken when extrapolating. This is a limitation common to all the studies carried out in this field and which has recently been flagged up.6 Despite these limitations, the present study provides new evidence on the need to assess the risk of suicidal behaviour in all patients attending the psychiatric emergency department and also during their follow-up. This follow-up should be more intense in the first months for those who have not made any prior attempts, and more continuous and long term for those who have already attempted suicide.
Declaration of transparencyThe principal author confirms that this manuscript is an honest, accurate and transparent account of the study presented, that no important aspects of the study have been omitted and that differences with the study that was initially planned have been explained.
FundingThis paper was financed with a grant from the Department of Health of the Government of Navarra (Resolution 3036/2014).
Conflict of interestLeire Azcárate worked as research support staff with a 12-month contract with the grant received for the project. The rest of the authors have no conflict of interests to declare.
Please cite this article as: López-Goñi JJ, Goñi-Sarriés A, Azcárate-Jiménez L, Sabater-Maestro P. Repetición de conductas suicidas en urgencias psiquiátricas en pacientes sin intentos previos, index y repetidores: un estudio prospectivo. Rev Psiquiatr Salud Ment (Barc.). 2020;13:192–201.