Eye movement desensitization and reprocessing (EMDR) is a relatively new psychotherapy that has gradually gained popularity for the treatment of post-traumatic stress disorder. In the present work, the standardised EMDR protocol is introduced, along with current hypotheses of its mechanism of action, as well as a critical review of the available literature on its clinical effectiveness in adult post-traumatic stress disorder. A systematic review of the published literature was performed using PubMed and PsycINFO databases with the keywords “eye movement desensitization and reprocessing” and “post-traumatic stress disorder” and its abbreviations “EMDR” and “PTSD”. Fifteen randomised controlled trials of good methodological quality were selected. These studies compared EMDR with unspecific interventions, waiting lists, or specific therapies. Overall, the results of these studies suggest that EMDR is a useful, evidence-based tool for the treatment of post-traumatic stress disorder, in line with recent recommendations from different international health organisations.
El tratamiento de desensibilización y reprocesamiento por movimiento ocular (EMDR de sus siglas en inglés: eye movement desensitization and reprocessing) es una terapia relativamente novedosa que de forma progresiva ha ido ganando popularidad en el tratamiento del trastorno por estrés postraumático. El objetivo de este trabajo es introducir el protocolo estándar EMDR, ofrecer una revisión de las hipótesis actuales sobre su mecanismo de acción y analizar la evidencia científica disponible sobre su eficacia clínica en pacientes adultos con diagnóstico de trastorno por estrés postraumático. Se realizó una revisión sistemática de la literatura publicada en las bases de datos PubMed y PsycINFO con los términos «eye movement desensitization and reprocessing» y «posttraumatic stress disorder» y sus contracciones en inglés «EMDR» y «PTSD». Se obtuvieron como resultado 15 ensayos controlados aleatorizados de elevada calidad metodológica que compararon EMDR con tratamientos no específicos, lista de espera y con tratamientos específicos. Los resultados de estos estudios permiten concluir que EMDR es una herramienta útil y basada en evidencia científica, tal y como refleja su reciente recomendación como tratamiento de elección en el trastorno por estrés postraumático por parte de distintas organizaciones internacionales de salud.
Post traumatic stress disorder (PTSD) is a psychiatric disorder classified within the group of anxiety disorders. PTSD may develop following exposure to a traumatic event in which there is a real risk of death, a threat or suffering severe injuries. l PTSD has a highly significant negative repercussion on patients’ lives, and its prevalence stands at from 7% to 8% of the population.1,2 According to the fourth edition of the Diagnostic and statistical manual of mental disorders, DSM), this disorder includes 4 main groups of symptoms: (i) re-experiencing the traumatic event in the form of nightmares, flashbacks and distressing thoughts; (ii) physiological hyperactivation that manifests as increased irritability, hypervigilance, sleep alterations and/or difficulty in concentrating; (iii) behaviour that avoids people or places associated with the traumatic events, developing feelings of detachment and/or making efforts to avoid certain thoughts, and (iv) persistent negative alterations in thoughts as well as in mood.3
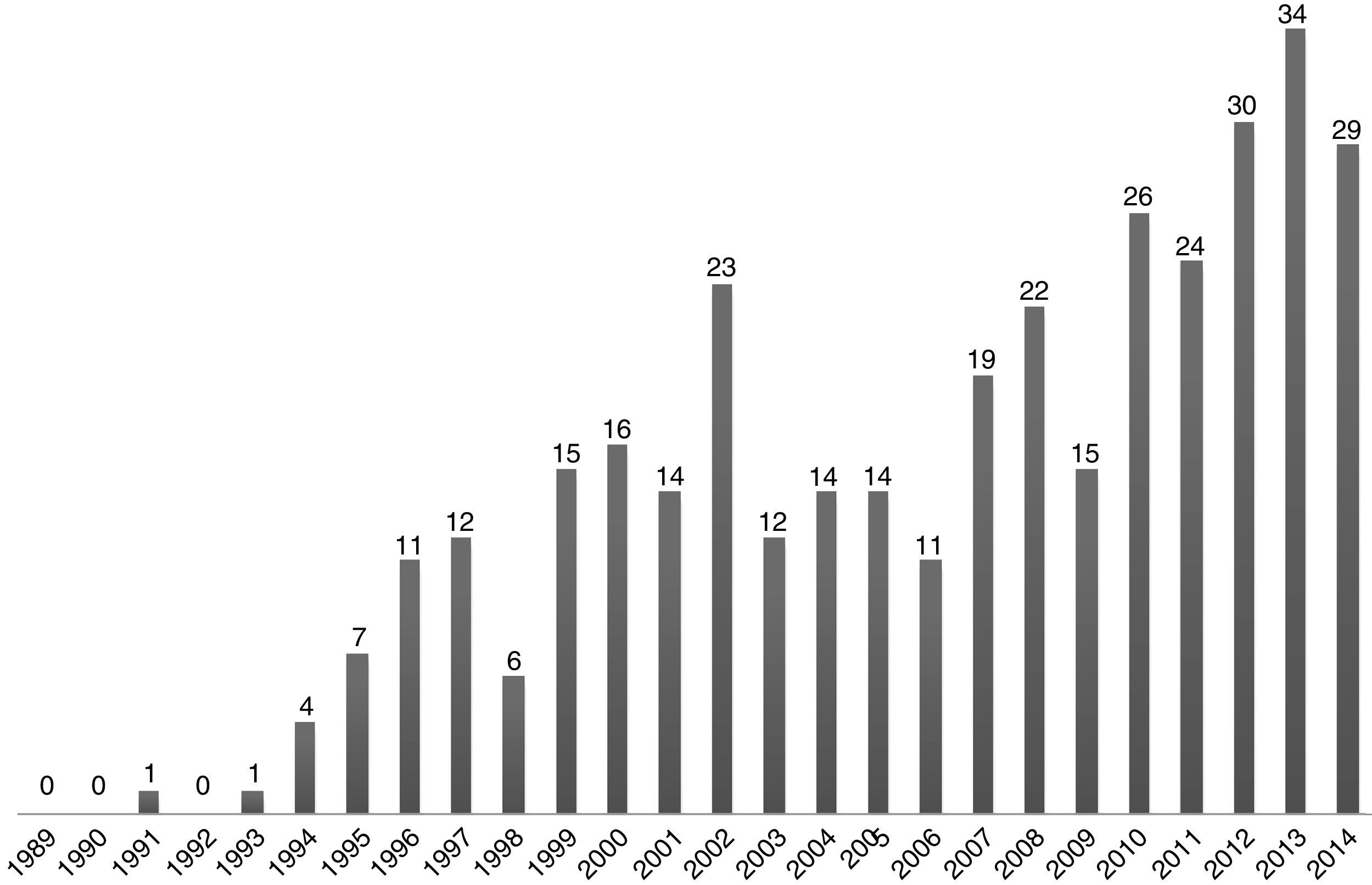
There are currently several non-pharmacological therapeutic approaches in the treatment of PTSD4: cognitive-behavioural therapy (CBT) that centres on the trauma, exposure therapy and treatment by eye movement desensitization and reprocessing (EMDR). In recent years EMDR has attained a significant popularity, with increasing numbers of therapists being trained in the technique and the subsequent considerable increase in its clinical use in different European countries.5 There has also been a significant increase in the number of scientific publications indexed in PubMed about the efficacy of using PTSD for other indications too, together with hypotheses about its mechanism of action (Fig. 1).
Due to the growing popularity of EMDR and the arrival of the 25th anniversary of its introduction as a treatment, this work contains a review of what EMDR consists of as well as its standard protocol for use and the current hypotheses on the mechanisms of action that underlie the therapy. Finally, it will systematically evaluate the literature which has examined the efficacy of EMDR treatment in cases of PTSD in comparison with non-specific treatments or remaining in a waiting list, other specific interventions and pharmacological treatment.
EMDR: basic concepts and application protocolEMDR is a psychotherapy that was developed in the 1980s by the North American psychologist Francine Shapiro.6 Shapiro originally described a standard intervention protocol that centred on working on traumatic memories and the stress symptoms associated with them. The protocol has been refined over time and by the addition of new knowledge until the standard protocol now in use was obtained.7–11 The most striking and controversial aspect of EMDR may be the use of bilateral stimulation, in the majority of cases by horizontal saccadic eye movements, to desensitise the discomfort caused by traumatic memories. This aims to reprocess these memories and include them within the normalised biographical memories of the patient.11
The standard protocol now includes the 8 phases which are described below:
- (1)
Patient history: in this first phase the therapist centres on evaluating the attachment history of the patient and on identifying traumatic episodes and how they connect with their current symptoms. The patient's medical history and current physical problems are also recorded. The bases and foundations of the therapy are then explained and a treatment plan is prepared. The traumatic memories to be worked on are selected, always following the temporal pattern of past-present-future.
- (2)
Patient preparation: the different forms of bilateral stimulation are tested in the second phase:
- •
Horizontal eye movements: the therapist moves his fingers within the horizontal plane of the patient's visual field, so that the latter follows them with his eyes, keeping the head immobile, at a speed of 2 movements per second and up to a total of approximately 30–40 movements.
- •
“Tapping”: this consists of gently and alternately tapping the backs of the patient's hands, which have to be resting on his knees. This too should be at a speed of 2 taps per second, although the speed and intensity may vary, depending on the patient.
- •
Bilateral auditory stimulation: this may consist of tones or bilateralised music played through headphones given to the patient.
- •
- (3)
Evaluation of the primary aspects of the memory: this step basically consists of accessing the traumatic memory and identifying the thoughts, emotions and bodily physical sensations associated with it. The therapist asks the patient which image represents the worst part of the traumatic memory and which negative cognition about the self that is a statement that can be generalised and pronounced in the present time they associate with that image (for example, “I am a failure”). The patient is then asked to identify the most suitable positive cognition to replace the negative one. This new cognition must express what the patient would like to believe about himself when thinking of the image (for example, “I am a valid person”). The patient evaluates the degree to which the positive cognition is true when thinking of the traumatic memory image on a scale of from 1 to 7, where 1 is completely false and 7 is completely true. Finally, the patient identifies which emotions he feels when bringing the traumatic experience and negative cognition to mind, as well as the level of alteration in units of subjective discomfort. The Subjective Units of Distress scale is used for this, with scores of from 0 to 10, where 10 is the maximum level of discomfort and 0 is the minimum.
- (4)
Desensitisation of the memory: the therapist asks the patient to bring the traumatic image and negative cognition to mind, together with the associated emotion and physical discomfort which this causes at the present time. The therapist then starts bilateral stimulation (eye movement, “tapping” or auditory stimulation) for 30–40s. Eye movements are general advisable, although if these are not tolerated well by the patient then the other 2 forms of bilateral stimulation may be used. During the periods of stimulation the therapist informs the patient that they should be a mere observer of what happens without making any type of judgement. After each round of stimulation the patient is given time to express what they have thought or felt, without the therapist making and type of comment, judgement or interpretation. Once new material ceases to emerge and the traumatic image no longer causes discomfort in the present (obtaining a score on the Subjective Units of Distress scale of 0 or 1 at most) the next phase commences.
- (5)
Installation of the positive cognition: the therapist now asks the patient to bring the positive cognition to mind and associated it with the original experience. Further periods of bilateral stimulation then take place to link the positive cognition with the original memory.
- (6)
Body scan: the patient is asked to close their eyes and concentrate on the original experience and the positive cognition, observing their body in case any type of feeling arises. IF the patient expresses any negative or unpleasant sensation, the therapist will commence bilateral stimulation until it disappears. If the sensation is positive it is reinforced using periods of bilateral stimulation lasting for 10–12s.
- (7)
Debriefing: the possible effects that may occur after the EMDR session are explained, such as the emergence of “insights”, new thoughts, memories or even dreams and nightmares, and recommendations about what to do in each cases are made.
- (8)
Re-evaluation: this has the aim of evaluating the effect that the patient may have experienced after the last session, re-evaluating the memory that was worked on to check whether it has been functionally processed.
The number of sessions dedicated to each phase as well as the number of phases worked on in each session may vary from one patient to another.
Hypothesis on how EMDR worksEMDR is an eclectic psychotherapy which contains elements that are compatible with the majority of psychological approaches.11 For example, the importance of childhood memories clearly fits with the psychodynamic model, while the exercise of keeping the image of the trauma in mind is similar to the exposure in imagination used in trauma-centred CBT.12 As well as being an experience-based client-centred method, EMDR also fits with the concept of positive and negative judgements about oneself that has deep roots in the field of phenomenological and humanist therapy.13 Due to all of this, some authors have suggested that the effectiveness of EMDR basically arises thanks to the common effects of different therapies.14 Nevertheless, Shapiro and Maxfield15 propose a theoretical model in which they offer data indicating that rhythmic bilateral stimulation is a fundamental and indispensable part of EMDR. The theoretical framework proposed by Shapiro to explain the observed clinical efficacy of EMDR is the Adaptive Information Processing model, AIP-model, which involves recovering the information about past negative experiences to re-include them in a positive emotional and cognitive framework.11 The core component of EMDR consists of keeping the attention focused on two different things, the traumatic memory and the rhythmic bilateral stimulation. This state of attention is fundamental as it is able to induce certain physiological conditions that activate information processing. Hypothetically bilateral stimulation is able to unblock brain processing centres, creating a connection between the previous adverse information and a response to a normal non-traumatic stimulation. Bilateral stimulation causes a response of relaxation and a series of physiological responses that, when they connect with stored information on previous adverse experiences, generate new information that is functionally reintegrated.
Given the theoretical framework proposed by Shapiro, study of the role of bilateral stimulation and of eye movements most of all, has aroused the curiosity of many researchers who are interested in EMDR. The first studies of the effect of eye movements were undertaken by Wilson et al.16 and Andrade et al.17 Based on the results of these studies, 3 main hypotheses have been suggested to explain the effect of eye movements.
The first hypothesis is that eye movements increase the connection between hemispheres. According to this model, PTSD symptoms are due to a fault in the processing of episodic memories. Bilateral eye movements would facilitate interaction between the hemispheres by increasing neuronal activation and connectivity to promote processing of the information. The result would be an improvement in the capacity to remember all of the elements of the traumatic event, facilitating the inclusion of the episodic memory in semantic memory.18–20 However, some recent electroencephalogram studies do not support this first theory, as they show that eye movements do not aid communication between the 2 hemispheres of the brain.20,21 This has led to other mechanisms being proposed within this model, in connection with changes in functional brain connectivity.22
The second hypothesis states that eye movements lead to physiological changes similar to those that occur during the REM (rapid eye movement) sleep phase.23 This model holds that the integration of episodic memory within the semantic memory occurs during sleep. Repeated bilateral eye movements would activates neurological mechanisms similar to those of the REM phase through an orientation response, thereby making it possible to include traumatic memories. There is now one controlled study which shows an improvement in sleep alterations in PTSD patients who receive EMDR in comparison with a control group.24 Within the physiological model, some authors have also suggested that bilateral stimulation would activate an exploratory reflex which places the organism in a state of alert; in the context of the therapy, as there are no real dangers, a relaxation response would arise that would involve a reduction of arousal, thereby facilitating the reprocessing and integration of the traumatic memory.25–28
The third and last hypothesis is that eye movements induce a demanding attentional task which has the effect of “exhausting” the working memory.29 As the working memory has a limited capacity, the dual attentional task of (i) keeping the traumatic content and is associated characteristics “online”, while at the same time, (ii) concentrating on bilateral eye movements may alter the quality of storage of traumatic memories, reducing the intensity of episodic memories and, with this, the symptoms of PTSD.30 Some authors, such as Gunter and Bodner,29 consider that the unpleasant memories worked on during EMDR sessions are kept in the visual-spatial agenda, as one of the components of the working memory that is in charge of maintaining and handling visual or spatial information. According to these authors, as the therapy progresses the stored content gradually becomes less vivid and emotional as the eye movements exhaust processing resources.
Recommendation by international clinical associationsThe scientific evidence for the efficacy of EMDR in the treatment of PTSD has been recognised by several international associations. The American Psychiatric Association has awarded it a level of confidence ii, equivalent to a “recommendation with moderate clinical reliability”.31 The American Psychological Association considers this treatment to have “strong research support”.32 According to the National Institute for Care Excellence (NICE),33 EMDR may be recommended with degree of evidence A for the treatment of PTSD in adults, with the backing of 11 controlled randomised studies. Additionally, in 2013 EMDR was included in the guide of the World Health Organisation as the first option for the treatment of PTSD in adults, children and adolescents.34
Systematic review of studies of the clinical efficacy of EMDR in PTSDThe scientific evidence for treatment using EMDR has been taken from different reviews and meta-analyses. The first meta-analysis of the efficacy of EMDR was published by Davidson and Parker in 2001,14 and it included 34 studies. The results showed that EMDR was equally effective as other exposure techniques. In another meta-analysis performed in 2006, Seidler and Wagner35 reported that trauma-centred EMDR and CBT tended to be equally effective in the treatment of PTSD. Similarly, the systematic review by Bisson et al.4 in 2013 concluded that EMDR and CBT centred on trauma have very similar effects, and they stated that both treatments have stronger empirical backing than stress-management programmes. Finally, a meta-analysis published in 2014 that included 26 controlled randomised trials found that EMDR therapy significantly reduces the symptoms of PTSD, depression and anxiety.36
ObjectivesThe aim of this review is to identify, synthesise and critically evaluate research into EMDR treatment in adults with PTSD diagnosed according to the DSM-IV. The increasing popularity of EMDR, the increase in the number of available studies in databases and the recent publication of protocols adapted to other mental illnesses (by Amann et al.,37 for example) show that this review is timely. Although previous reviews in this field exist,4,35 they include studies of doubtful methodological quality and have a predominantly narrative approach. This review is an advance as it identifies and includes 15 controlled randomised studies that were evaluated using the Jadad scale38 to determine their methodological quality. This scale covers distortions due to randomisation, masking and losses during follow-up. The scale runs from 0 to 5 points, where 5 points is considered to refer to a rigorous randomised clinical trial and where less than 3 points indicates a low quality clinical trial. For this study works that obtained a score of 3 or more were selected.
Lastly, this work was undertaken using a systematic review methodology that performs a critical evaluation of research techniques and the results of the studies included, adapting the Preferred Reporting Items for Systematic Reviews and Meta-Analyses39,40 into Spanish. This is a set of 27 items based on the evidence established by minimum criteria for the presentation of reports in systematic reviews and meta-analyses.
MethodA systematic review was undertaken of scientific papers that evaluated the efficacy of EMDR in the treatment of PTSD. These papers were identified in a search of the bibliography using systematic review techniques. Following the Thesaurus of the National Medicine Library (Medical Subject Heading Terms, MeSH) and the Psychological Index Terms of the American Psychological Association it was decided to use the following as the most appropriate search terms: “eye movement desensitization and reprocessing” and “post-traumatic stress disorder”, as well as their acronyms in English “EMDR” and “PTSD”. The final search equation was defined using the Boolean connector OR in each one of the 2 equations. The databases consulted were Medline (via PubMed) and PsycINFO. The search was restricted to from 1/1/1984 to 31/12/2014. It was restricted to human beings and no subheadings or tags were used, so that the search took place in all fields. A search was also carried out of the secondary literature, with the aim of covering other forms of publication. In this way the bibliographies of the papers selected in the main search were examined to detect studies that had not been identified in the computerised search.
The final selection of the papers was undertaken using the following inclusion criteria: (i) original papers published in peer-reviewed journals; (ii) adult population (over the age of 16 years old); (iii) patients diagnosed PTSD according to DSM criteria, when the version used corresponded to the year the original work was published: DSM-III-R (APA, 1987), DSM-IV (APA, 1994) or DSM-IV-TR (APA, 2000), and (iv) a trial design with a control group.
The exclusion criteria were: (i) studies that were not original (reviews, meta-analyses, other types of experiment); (ii) studies of the basic working mechanisms of EMDR, and (iii) quasi-experimental studies (of a single group or a single case). Studies were selected by the authors PNN and BLA. Disagreements were resolved by RGWB.
After selecting the 18 papers that fulfilled the inclusion and exclusion criteria described above the Jadad scale was used to evaluate the methodological quality of each clinical trial.38 Absolute and relative frequencies were calculated for statistical analysis using SPSS 16.0 for Windows software (SPSS, Inc., Chicago, IL, U.S.A.).
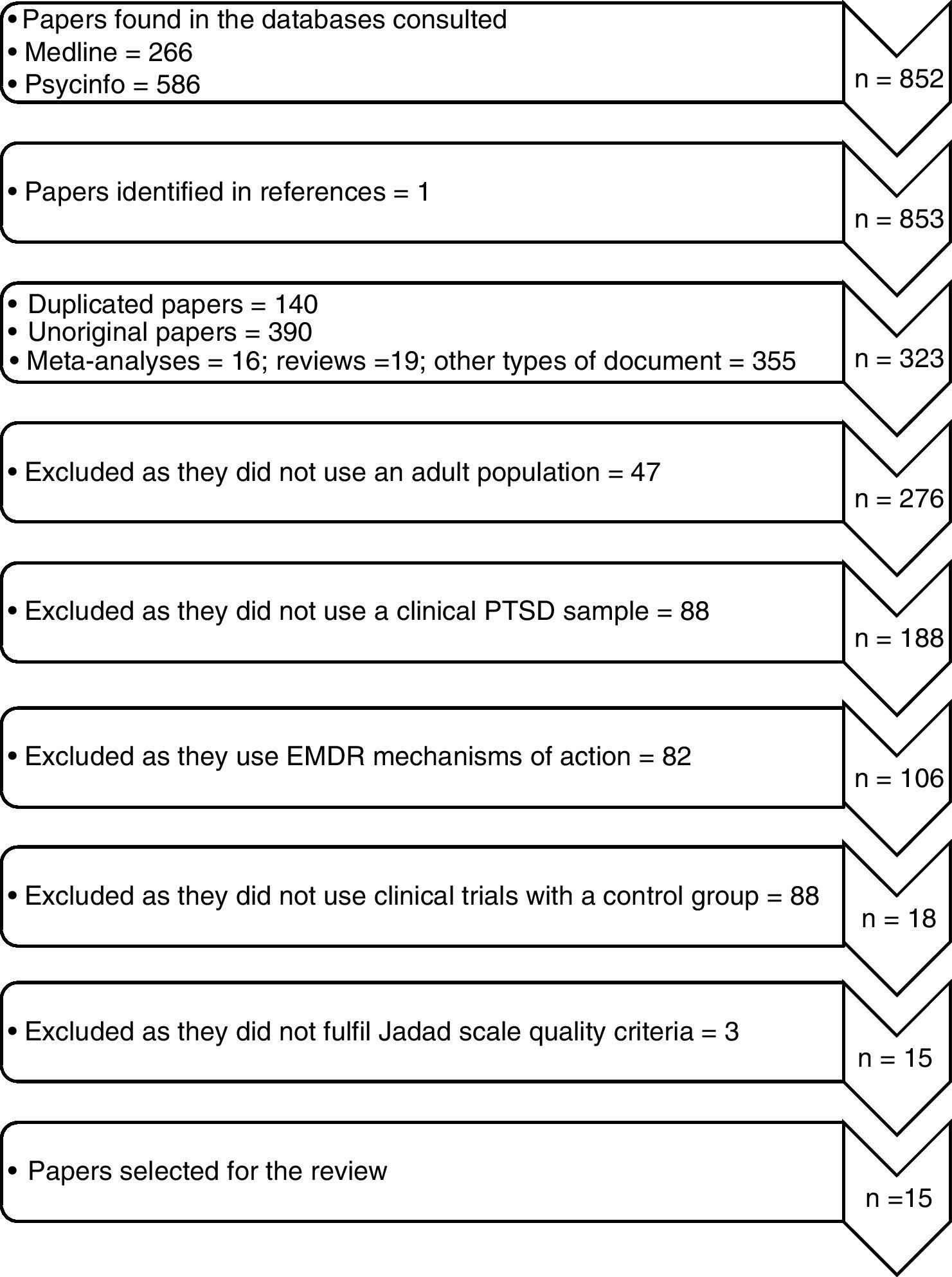
ResultsFig. 2 shows a flow chart that describes the selection of the studies. A total of 852 original works were identified, of which 266 were found in Medline and 586 in PsycINFO. When reviewing the bibliographies of the papers found, one work was selected that had not been detected in the primary search. When both searches were compared 140 duplicated works were found, as well as 390 papers that were not original which were eliminated, leaving 323 original papers. Of the resulting 323 papers, 305 were excluded as they did not use an adult population (n=47), as they did not use a clinical sample of PTSD (n=88), as they studied the mechanism of action of EMDR (n=82) and as their clinical trials were neither randomised nor controlled (n=88). After applying the Jadad scale questionnaire 3 works were excluded due to their poor technical quality, resulting in the final selection of the 15 papers included in this review, with an average methodological quality of 4 points (Jadad). In general the methodological quality of the clinical trials was found to be appropriate, and it was also found to have improved over time. As well as the Jadad criteria, the number of sessions was reviewed, together with the replicability of the treatments and/or whether they were manual, the training of therapists and supervision of the therapy by an independent evaluator. The work also fulfilled the majority of the criteria in the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (19 of 27 criteria), excepting those on the quantitative study of results.
Analysis of current scientific production gives rise to the following statistics: the average age of the papers was 11.73±1.37 years (CI 95% 8.79–14.67), with a minimum of 2 years and a maximum of 20 years. The obsolescence of the papers analysed using the median (Burton–Kebler index) was of 12 years, and the Price index stands at 13.33 (the percentage of papers less than 5 years old).
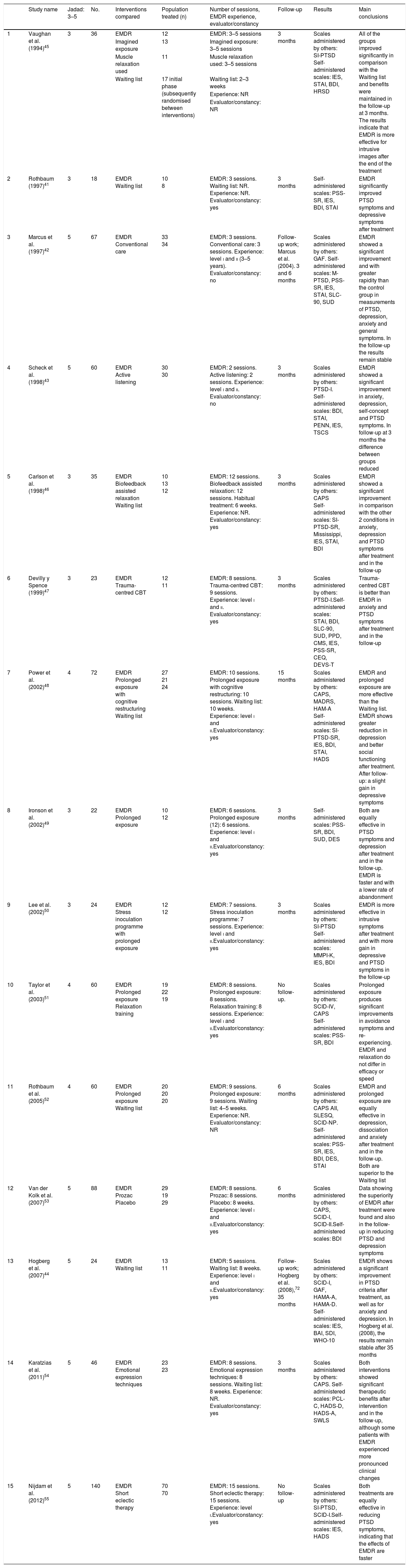
Clinical trials of EMDR in post-traumatic stress disorderEMDR versus waiting list group and/or non-specific treatmentsOf the 15 clinical trials included (Table 1), 4 of them compared the efficacy of EMDR with non-specific treatments.41–44 All of these studies showed a significant clinical improvement with EMDR in comparison with other treatments. The average methodological quality of these works was 4.5 points (Jadad).
Studies of the efficacy of eye movement desensitization and reprocessing in post-traumatic stress disorder in adults (n=15).
| Study name | Jadad: 3–5 | No. | Interventions compared | Population treated (n) | Number of sessions, EMDR experience, evaluator/constancy | Follow-up | Results | Main conclusions | |
|---|---|---|---|---|---|---|---|---|---|
| 1 | Vaughan et al. (1994)45 | 3 | 36 | EMDR | 12 | EMDR: 3–5 sessions | 3 months | Scales administered by others: SI-PTSD Self-administered scales: IES, STAI, BDI, HRSD | All of the groups improved significantly in comparison with the Waiting list and benefits were maintained in the follow-up at 3 months. The results indicate that EMDR is more effective for intrusive images after the end of the treatment |
| Imagined exposure | 13 | Imagined exposure: 3–5 sessions | |||||||
| Muscle relaxation used | 11 | Muscle relaxation used: 3–5 sessions | |||||||
| Waiting list | 17 initial phase (subsequently randomised between interventions) | Waiting list: 2–3 weeks | |||||||
| Experience: NR | |||||||||
| Evaluator/constancy: NR | |||||||||
| 2 | Rothbaum (1997)41 | 3 | 18 | EMDR Waiting list | 10 8 | EMDR: 3 sessions. Waiting list: NR. Experience: NR. Evaluator/constancy: yes | 3 months | Self-administered scales: PSS-SR, IES, BDI, STAI | EMDR significantly improved PTSD symptoms and depressive symptoms after treatment |
| 3 | Marcus et al. (1997)42 | 5 | 67 | EMDR Conventional care | 33 34 | EMDR: 3 sessions. Conventional care: 3 sessions. Experience: level i and ii (3–5 years). Evaluator/constancy: no | Follow-up work; Marcus et al. (2004). 3 and 6 months | Scales administered by others: GAF. Self-administered scales: M-PTSD, PSS-SR, IES, STAI, SLC-90, SUD | EMDR showed a significant improvement and with greater rapidity than the control group in measurements of PTSD, depression, anxiety and general symptoms. In the follow-up the results remain stable |
| 4 | Scheck et al. (1998)43 | 5 | 60 | EMDR Active listening | 30 30 | EMDR: 2 sessions. Active listening: 2 sessions. Experience: level i and ii. Evaluator/constancy: no | 3 months | Scales administered by others: PTSD-I. Self-administered scales: BDI, STAI, PENN, IES, TSCS | EMDR showed a significant improvement in anxiety, depression, self-concept and PTSD symptoms. In follow-up at 3 months the difference between groups reduced |
| 5 | Carlson et al. (1998)46 | 3 | 35 | EMDR Biofeedback assisted relaxation Waiting list | 10 13 12 | EMDR: 12 sessions. Biofeedback assisted relaxation: 12 sessions. Habitual treatment: 6 weeks. Experience: NR. Evaluator/constancy: yes | 3 months | Scales administered by others: CAPS Self-administered scales: SI-PTSD-SR, Mississippi, IES, STAI, BDI | EMDR showed a significant improvement in comparison with the other 2 conditions in anxiety, depression and PTSD symptoms after treatment and in the follow-up |
| 6 | Devilly y Spence (1999)47 | 3 | 23 | EMDR Trauma-centred CBT | 12 11 | EMDR: 8 sessions. Trauma-centred CBT: 9 sessions. Experience: level i and ii. Evaluator/constancy: yes | 3 months | Scales administered by others: PTSD-I.Self-administered scales: STAI, BDI, SLC-90, SUD, PPD, CMS, IES, PSS-SR, CEQ, DEVS-T | Trauma-centred CBT is better than EMDR in anxiety and PTSD symptoms after treatment and in the follow-up |
| 7 | Power et al. (2002)48 | 4 | 72 | EMDR Prolonged exposure with cognitive restructuring Waiting list | 27 21 24 | EMDR: 10 sessions. Prolonged exposure with cognitive restructuring: 10 sessions. Waiting list: 10 weeks. Experience: level i and ii.Evaluator/constancy: yes | 15 months | Scales administered by others: CAPS, MADRS, HAM-A Self-administered scales: SI-PTSD-SR, IES, BDI, STAI, HADS | EMDR and prolonged exposure are more effective than the Waiting list. EMDR shows greater reduction in depression and better social functioning after treatment. After follow-up: a slight gain in depressive symptoms |
| 8 | Ironson et al. (2002)49 | 3 | 22 | EMDR Prolonged exposure | 10 12 | EMDR: 6 sessions. Prolonged exposure (12): 6 sessions. Experience: level i and ii.Evaluator/constancy: yes | 3 months | Self-administered scales: PSS-SR, BDI, SUD, DES | Both are equally effective in PTSD symptoms and depression after treatment and in the follow-up. EMDR is faster and with a lower rate of abandonment |
| 9 | Lee et al. (2002)50 | 3 | 24 | EMDR Stress inoculation programme with prolonged exposure | 12 12 | EMDR: 7 sessions. Stress inoculation programme: 7 sessions. Experience: level i and ii.Evaluator/constancy: yes | 3 months | Scales administered by others: SI-PTSD Self-administered scales: MMPI-K, IES, BDI | EMDR is more effective in intrusive symptoms after treatment and with more gain in depressive and PTSD symptoms in the follow-up |
| 10 | Taylor et al. (2003)51 | 4 | 60 | EMDR Prolonged exposure Relaxation training | 19 22 19 | EMDR: 8 sessions. Prolonged exposure: 8 sessions. Relaxation training: 8 sessions. Experience: level i and ii.Evaluator/constancy: yes | No follow-up. | Scales administered by others: SCID-IV, CAPS Self-administered scales: PSS-SR, BDI | Prolonged exposure produces significant improvements in avoidance symptoms and re-experiencing. EMDR and relaxation do not differ in efficacy or speed |
| 11 | Rothbaum et al. (2005)52 | 4 | 60 | EMDR Prolonged exposure Waiting list | 20 20 20 | EMDR: 9 sessions. Prolonged exposure: 9 sessions. Waiting list: 4–5 weeks. Experience: NR. Evaluator/constancy: NR | 6 months | Scales administered by others: CAPS AII, SLESQ, SCID-NP. Self-administered scales: PSS-SR, IES, BDI, DES, STAI | EMDR and prolonged exposure are equally effective in depression, dissociation and anxiety after treatment and in the follow-up. Both are superior to the Waiting list |
| 12 | Van der Kolk et al. (2007)53 | 5 | 88 | EMDR Prozac Placebo | 29 19 29 | EMDR: 8 sessions. Prozac: 8 sessions. Placebo: 8 weeks. Experience: level i and ii.Evaluator/constancy: yes | 6 months | Scales administered by others: CAPS, SCID-I, SCID-II.Self-administered scales: BDI | Data showing the superiority of EMDR after treatment were found and also in the follow-up in reducing PTSD and depression symptoms |
| 13 | Hogberg et al. (2007)44 | 5 | 24 | EMDR Waiting list | 13 11 | EMDR: 5 sessions. Waiting list: 8 weeks. Experience: level i and ii.Evaluator/constancy: yes | Follow-up work; Hogberg et al. (2008),72 35 months | Scales administered by others: SCID-I, GAF, HAMA-A, HAMA-D. Self-administered scales: IES, BAI, SDI, WHO-10 | EMDR shows a significant improvement in PTSD criteria after treatment, as well as for anxiety and depression. In Hogberg et al. (2008), the results remain stable after 35 months |
| 14 | Karatzias et al. (2011)54 | 5 | 46 | EMDR Emotional expression techniques | 23 23 | EMDR: 8 sessions. Emotional expression techniques: 8 sessions. Waiting list: 8 weeks. Experience: NR. Evaluator/constancy: yes | 3 months | Scales administered by others: CAPS. Self-administered scales: PCL-C, HADS-D, HADS-A, SWLS | Both interventions showed significant therapeutic benefits after intervention and in the follow-up, although some patients with EMDR experienced more pronounced clinical changes |
| 15 | Nijdam et al. (2012)55 | 5 | 140 | EMDR Short eclectic therapy | 70 70 | EMDR: 15 sessions. Short eclectic therapy: 15 sessions. Experience: level i.Evaluator/constancy: yes | No follow-up | Scales administered by others: SI-PTSD, SCID-I.Self-administered scales: IES, HADS | Both treatments are equally effective in reducing PTSD symptoms, indicating that the effects of EMDR are faster |
AII: Assault Information Interview; BAI: Beck Anxiety Inventory; BDI: Beck Depression Inventory; CAPS: Clinician-Administered PTSD Scale; CEQ: Credibility/Expectancy Questionnaire; CMS: Mississippi Scale for Civilian PTSD; DES: Dissociative Experiences Scale; DEVS-T: Distress Evaluation Scale for Treatment; EMDR: eye movement desensitization and reprocessing; GAF: Global Assessment of Functioning; HADS-A: The Hospital Anxiety and Depression Scale-Anxiety; HADS-D: The Hospital Anxiety and Depression Scale-Depression; HAMA-A: Hamilton Anxiety Rating Scale-Anxiety; HAMA-D: Hamilton Anxiety Rating Scale-Depression; HRSD: Hamilton Rating Scale for Depression; IES: Impact of Event Scale; Jadad: scale that measures the methodological quality of studies; MADRS: The Montgomery-Asberg Depression Rating Scale; Mississippi: Mississippi Scale for Combat-Related PTSD; MMPI-K: Minnesota Multiphasic Personality Inventory K-Scale; M-PTSD: Modified PTSD Scale; NR: not reported; PCL-C: Posttraumatic Stress Disorder Checklist, civilians version; PENN: Penn Inventory for Posttraumatic Stress Disorder; PPD: Personal Problem Definition Questionnaire; PSS-SR: PTSD Symptom Scale Self-Report; PTSD: post-traumatic stress disorder; PTSD-I:PTSD Interview; SCID-I: Structured Clinical Interview for DSM-IV Axis I Disorders; SCID-II: Structured Clinical Interview for DSM-IV Axis II Disorders; SCID-IV: Structured Clinical Interview for DSM Disorders IV; SCID-NP: Structured Clinical Interview for DSM-IV Non-Patients Version; SDI: Social Disability Index; SI-PTSD: Davidson's Structured Interview for PTSD; SLC-90: Symptom Checklist-90; SLESQ: Stressful Life Events Screening Questionnaire; SR: self-report; STAI: State-Trait Anxiety Inventory; SUD: Subjective Units of Distress; SWLS: Satisfaction with Life Scale; CBT: cognitive-behavioural therapy; PTSD: post-traumatic stress disorder; TSCS: Tennessee Self-Concept Scale; WHO-10: World Health Organization Ten Well-Being Scale.
More specifically, EMDR was compared with waiting list,41,44 with active listening according to Rogers’ model43 and with counselling.42 In the studies that evaluated the symptoms of PTSD by self-reporting and standardised clinical interviews, EMDR showed a significant reduction in the symptoms of PTSD, as well as the symptoms of depression and anxiety in comparison with the non-specific treatment group. Some studies also showed a significant reduction in dissociative symptoms41 and an improvement in self-concept43 when EMDR was used in comparison with patients in waiting lists or those who received no specific treatment.
In 3 of the 4 studies included the therapeutic effect of EMDR remained after 3 months,42 after 6 months41 and after 35 months44 of follow-up. Some studies observed an association between the improvement in symptoms and increased adherence to the treatment41,44 and improved training for the therapists.42–44
EMDR versus specific treatments11 clinical trials were found that compared the efficacy of EMDR with other specific treatments.45–55 EMDR was compared to long-term imaginary exposure,45,49,51 muscle relaxation,45,51 biofeedback assisted muscle relaxation,46 trauma-centred CBT,50 prolonged exposure with cognitive restructuring,48 a stress inoculation programme,50 pharmacological treatment,53 emotional expression techniques54 and short eclectic therapy.55
EMDR was found to be equally effective as other specific techniques in 5 studies (Jadad 3.8 points). The first study compared EMDR with muscle relaxation and imaginary exposure without finding any significant differences between the groups.45 Similarly, 2 clinical trials found that there were no significant differences when EMDR was compared to prolonged exposure,49,52 as both interventions were found to be equally useful in treating PTSD. Nevertheless, the study by Ironson et al.49 found that EMDR was faster in reducing symptoms and that it was tolerated better by patients, given that a lower rate of abandonment was recorded. Karatzias et al.54 showed that EMDR and emotional liberation techniques produced significant therapeutic benefits, although they state that there was a slightly higher proportion of patients with clinical improvement in the group that received EMDR. The authors hypothesise that these results were due to the fact that both therapies share fundamental elements, such as desensitisation, distraction and exposure. Lastly, Nijdam et al.55 compared EMDR with short eclectic therapy and found that both treatments were equally effective in reducing the symptoms of PTSD, and they indicate that the effects of EMDR were faster.
Four clinical trials with an average quality of 3.8 points (Jadad) obtained favourable results with EMDR in comparison with specific techniques. The comparison of EMDR with biofeedback-assisted relaxation training46 showed results in favour of EMDR in reducing the symptoms of anxiety, depression and PTSD after treatment and after a follow-up period of 3 months. The work by Power et al.48 found that EMDR was superior to prolonged exposure with cognitive restructuring in reducing depressive symptoms and improving social functioning after treatment, and these effects were maintained after a 15 month follow-up. EMDR was also found to be more effective that the stress inoculation programme with gradual exposure50 for the symptoms of avoidance and PTSD flashbacks after treatment and after a 3 month follow-up. Only one study compared the efficacy of EMDR with pharmacological treatment. Van der Kolk et al.53 compared a group of patients with PTSD who were treated using EMDR with another group of patients treated with a placebo and another group treated using antidepressive drugs. The results indicated that the intervention with EMDR was more effective than the pharmacological therapy in achieving a substantial and sustained reduction at 6 months of the PTSD symptoms as well as depression in the majority of the patients.
Lastly, 2 trials were found with unfavourable results for EMDR, with an average methodological quality of 3.5 points (Jadad). Devilly and Spence (1999) compared the efficacy of EMDR with trauma-centred CBT. Their results indicated that CBT was more effective and better tolerated than EMDR after treatment and after a 3 month follow-up. In the second study Taylor et al.51 showed that prolonged exposure was more effective than EMDR in reducing avoidance and flashback symptoms, and that it was also faster in reducing avoidance symptoms.
DiscussionAs it is the 25th anniversary of the introduction of EMDR, this work has the aim of briefly illustrating the history and development of this treatment. It reviews its basic administration protocol, shows the results of recent studies of its mechanism of action and reviews its clinical efficacy. A systematic review was carried out controlled randomised trials with appropriate methodological quality and in adult populations diagnosed PTSD according to DSM-IV criteria. The review was performed according to the standardised methodological quality criteria for conducting systematic reviews.
Since it was introduced EMDR has generated a considerable amount of debate in the clinical and scientific communities. This mainly centres on the role of bilateral stimulation (and more specifically of eye movements) as an active part of treatment, and the uncertainty about whether its efficacy is due to overlap of its elements with other psychotherapeutic techniques. Eye movements were originally described as the “crucial” part of EMDR.6 This argument was subsequently revised,9 concluding that dual attention is the causal mechanism for the effect of EMDR. Some studies have found that eye movements make a unique contribution to the success of the intervention,13,17,56,57 while others have found no differences in the result when the same procedure with and without eye movements is compared.14,58 These studies are difficult to compare, as they differ widely in methodological terms. However, a recent meta-analysis found that eye movements make a significant contribution in processing emotional memories.59 The results of this study were not free of controversy, as there were accusations of bad praxis in the development of the research60 and a subsequent refutation.61
On the other hand, the debate on the degree to which the causal mechanisms of its effect differ substantially or not from those that function in trauma-centred CBT or standard exposure is sterile from a methodological standpoint. This is due to lack of knowledge and agreement on which biological mechanisms function in general in all psychotherapies. Trauma-centred CBT consists of a combination of exposure techniques and cognitive interventions, while EMDR is an eclectic psychotherapy which includes a set of structured procedures and protocols. Although many procedures seem to overlap with trauma-centred CBT, the National Institute for Care Excellence has stated that the 2 approaches are different as they require specific training programmes.33 In a paper published in 2002 Rogers and Silver62 describe the differences between EMDR protocols and those involving exposure in detail, the latter being a key component of trauma-centred CBT.
The basic protocol for administering EMDR is a parsimonious and painstakingly detailed procedure, facilitating its clinical use as well as scientific scrutiny. The majority of the studies that have examined its mechanism of action have centred on studying one part of EMDR therapy, bilateral stimulation, and more specifically on eye movement. 3 hypotheses have fundamentally emerged from these studies on the possible effect of bilateral stimulation: memory resource overload, a fall in physiological arousal or improved connectivity between the hemispheres of the brain. These theoretical models, which often overlap each other, point to the directions of future research which aims for increased conceptual clarity and consistency.
The level of sophistication of studies of the mechanism of action of EMDR has increased exponentially in recent years. A study undertaken by Landin-Romero et al.63 using functional neuroimaging techniques stands out. This showed for the first time that EMDR is able to modulate patterns of neuronal net activation and deactivation by default. This brain system has chiefly been linked with autobiographical and introspective thought by an individual. Nevertheless, with very few exceptions the majority of these studies have major methodological limitations. Their results should therefore be considered to be preliminary, so that hypotheses about the underlying biological effects of EMDR are currently mainly speculative.
Finally, this work presented a systematic review of 15 randomised controlled studies which compared the efficacy of EMDR in the treatment of PTSD with that of other psychotherapeutic interventions. According to the recommendations of different international psychological and psychiatric associations, and in spite of the fact that this work lacks quantitative analysis of the results, it can be said that there are sufficient high-methodological quality studies which indicate that EMDR is at the least equally effective as a therapy as trauma-centred CBT. Additionally, some studies seem to indicate that EMDR is more effective at reducing symptoms in a shorter period of time, and that it is a therapy that is tolerated better by patients.5,49,51
It should be pointed out that the first studies of EMDR were criticised because of aspects linked to the methodology used.64 These were mainly the absence of a control group to isolate the possible placebo effect of the intervention,25,65 the lack of double blind evaluations,45 exclusive use of measurements supplied by self-reports and ambiguity about the severity and diagnosis of PTSD. Clinicians who specialise in EMDR11 also pointed out some factors that may have hindered the observation of positive effects of the treatment. These included the insufficient number of EMDR sessions25,43,66 and/or the administration of psychotherapy by professionals who lack training41 or who had not properly followed the protocol. More recent studies can be seen to have attempted to overcome these methodological problems, and the methodological quality can be seen to have improved in general, as have the criteria proposed in increasingly clinical areas for EMDR. Branches of comparison with specific techniques are now included, together with clinical interviews and standardised self-completed reports to evaluate symptoms,51,53 evaluators who are blind regarding the intervention conditions49,50 and qualified professionals with training and years of experience in the use of EMDR.44
It is important to point out that EMDR is gaining ground in the treatment of other psychiatric diseases that are comorbid with PTSD or traumatic events, such as addictions,67 bipolar disorder,37,68 unipolar depression69 or psychosis.70,71 There is now preliminary scientific evidence for the technique in controlled randomised studies with promising results.
To conclude, there is a growing number of clinical studies, reviews and meta-analyses which supply data on the effectiveness and safety of EMDR in the treatment of PTSD. They place it at the same level as other treatments of choice, such as trauma-centred CBT. Nevertheless, research into EMDR is still at an early stage. Further studies are still necessary to gain greater understanding of its mechanism of action and the neurobiological foundations underlying the therapy. Finally, more clinical trials with an appropriate methodological quality are needed to strengthen the results obtained to date on the efficacy of EMDR in the treatment of patients diagnosed PTSD, and to confirm the first positive results of using it to treat other mental illnesses which have trauma as a comorbidity.
Conflict of interestsFrancisca García is the President of the Spanish EMDR Association, and Isabel Fernández is the President of the European EMDR Association. Benedikt L. Amann, Ramón Landin-Romero and Walter Lupo have been guest speakers in several national and international EMDR conferences.
This review was supported by the European and Spanish EMDR Association, the Centro de Investigación Biomédica en Red de Salud Mental (CIBERSAM), several grants from the National Plan for R&D&I, the Instituto de Salud Carlos III-Subdirección General de Evaluación y Fomento de la Investigación, Plan Nacional 2008–2011 and 2013–2016, and The European Regional Development Fund (FEDER): stabilisation contract (CES 12/024) and grants FIS (PI07/1278, PI10/02622 and PI/15/02242) for Benedikt L. Amann.
Please cite this article as: Novo Navarro P, Landin-Romero R, Guardiola-Wanden-Berghe R, Moreno-Alcázar A, Valiente-Gómez A, Lupo W, et al. 25 años de Eye Movement Desensitization and Reprocessing: protocolo de aplicación, hipótesis de funcionamiento y revisión sistemática de su eficacia en el trastorno por estrés postraumático. Rev Psiquiatr Salud Ment (Barc.). 2018;11:101–114.