Uterine arteriovenous malformation (UAMM) for some authors, considered an arteriovenous fistula, represents between 1% and 2% of genital and intraperitoneal hemorrhage as a result of spontaneous or provoked vascular rupture after a surgical intervention.
We present a case of maternal death that occurred during a walk on a slope, presenting metrorrhagia and fainting with a fatal outcome. The medico-legal autopsy showed a pregnancy uterus with myometrial hemorrhage and multiple blood clots, diagnosed pathologically as a uterine arteriovenous malformation.
Maternal death is a multifactorial public health problem in underdeveloped countries. Uterine arteriovenous malformation is a rare cause, however some authors consider it underdiagnosed; reported cases have increased in recent years and in developing countries it can be lethal.
La malformación arteriovenosa uterina (MAVU) para algunos autores considerada como fistula arteriovenosa representa entre el 1-2% de la hemorragia genital e intraperitoneal como resultado de la rotura vascular espontánea o provocada posterior a una intervención quirúrgica.
Exponemos un caso de muerte materna ocurrida durante una caminata sobre una pendiente presentando metrorragia y desvanecimiento con desenlace letal. La autopsia médico legal demostró, útero gestante con hemorragia del miometrio y múltiples coágulos hemáticos, diagnosticada anatomopatológicamente como malformación arteriovenosa uterina.
La muerte materna es un problema de salud pública multifactorial en países subdesarrollados, la malformación arteriovenosa uterina es una causa poco frecuente, sin embargo algunos autores la consideran subdiagnosticada; han aumentado el reporte de casos en los últimos años y en los países en desarrollo puede ser letal.
Severe haemorrhages cause 75% of maternal deaths. At any time during pregnancy a severe haemorrhage may threaten the life of a woman if it is not resolved in less than 2 hours.1 Uterine arteriovenous malformation (UAVM), which some authors consider to be an arteriovenous fistula, accounts for from 1% to 2% of genital and intraperitoneal haemorrhages. It may be caused by spontaneous vascular rupture or one following surgery.2--4
Following the first published case of a UAVM in 1926 by Dubreil, the true incidence of UAVM is still unknown. O’Brien reported a prevalence of 4.3% in patients seen due to vaginal bleeding.5
Medical-forensic descriptionA 33 year-old woman who lived in a rural town, with unknown pathological history and a gynaecological-obstetric history of a second gestation, a caesarean and no birth, with a pregnancy in its third quarter and without prenatal medical care, suffered abundant transvaginal bleeding and fainting while walking up a hill. She received basic first aid in a private home, without success, and the mother and child died. The cadaver was taken to the Forensic Medicine Department (SEMEFO) in Puebla, Mexico.
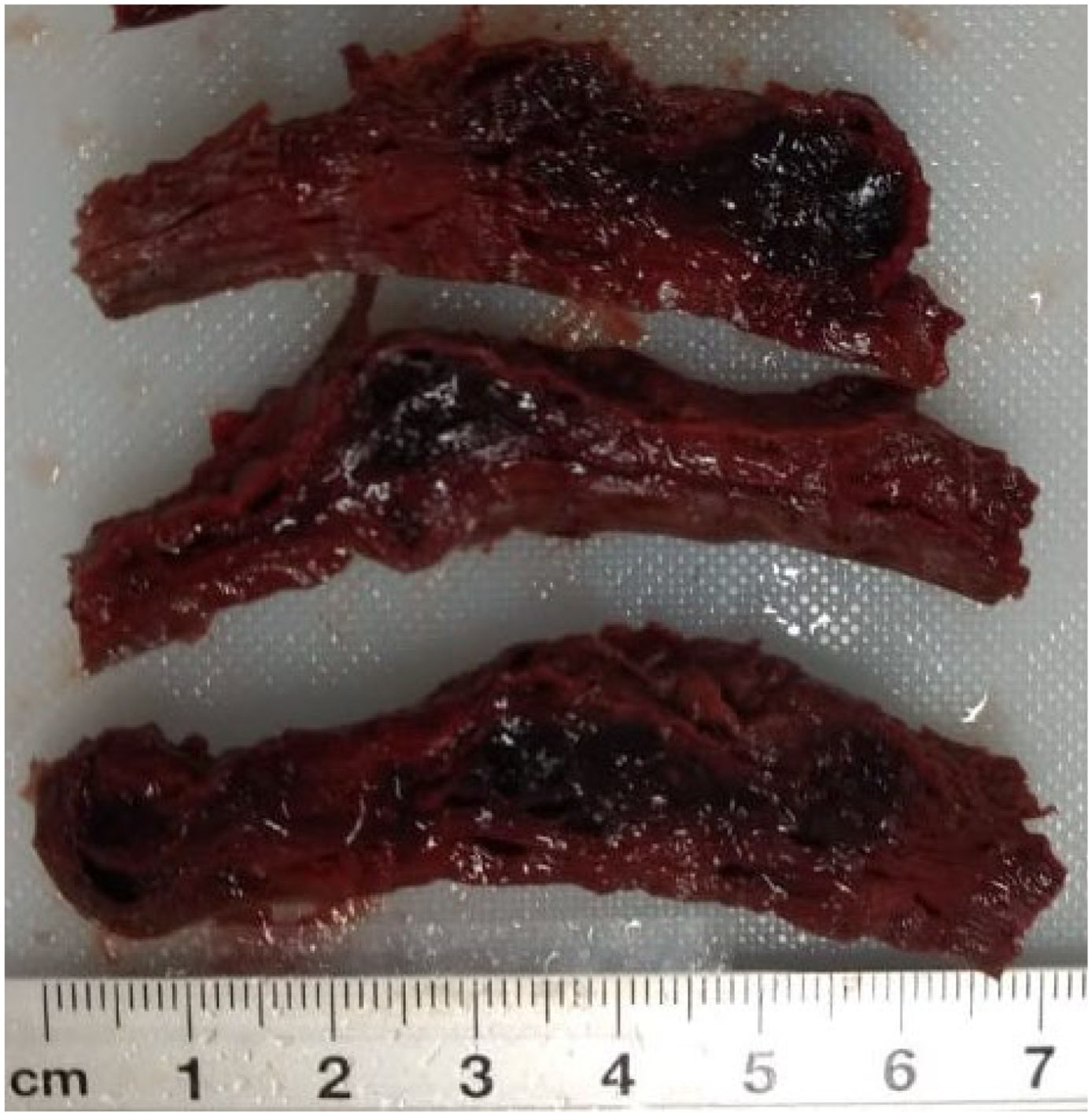
External appearance with pale mucus membranes, skin and tissues, with marks of blood on the external genitals that extended down the anterior face of both legs to the ankles. The thoracic cavity was free of anomalous fluids, the organs were pale and in their usual positions, the lungs with a visceral pleura of reddish coffee colour, a smooth surface and spongy consistency; the size and shape of the heart were normal, and in the abdominal cavity the liver and spleen were whole and in their usual positions. The gestating uterus measured 30 × 20 × 15 cm with the dead product of gestation. A haemorrhagic segment was observed on the front wall of the uterus (Fig. 1) composed of a vascular sphere measuring 6 × 2 cm, located on the anterior wall of the body and the segment of uterus (Fig. 2).
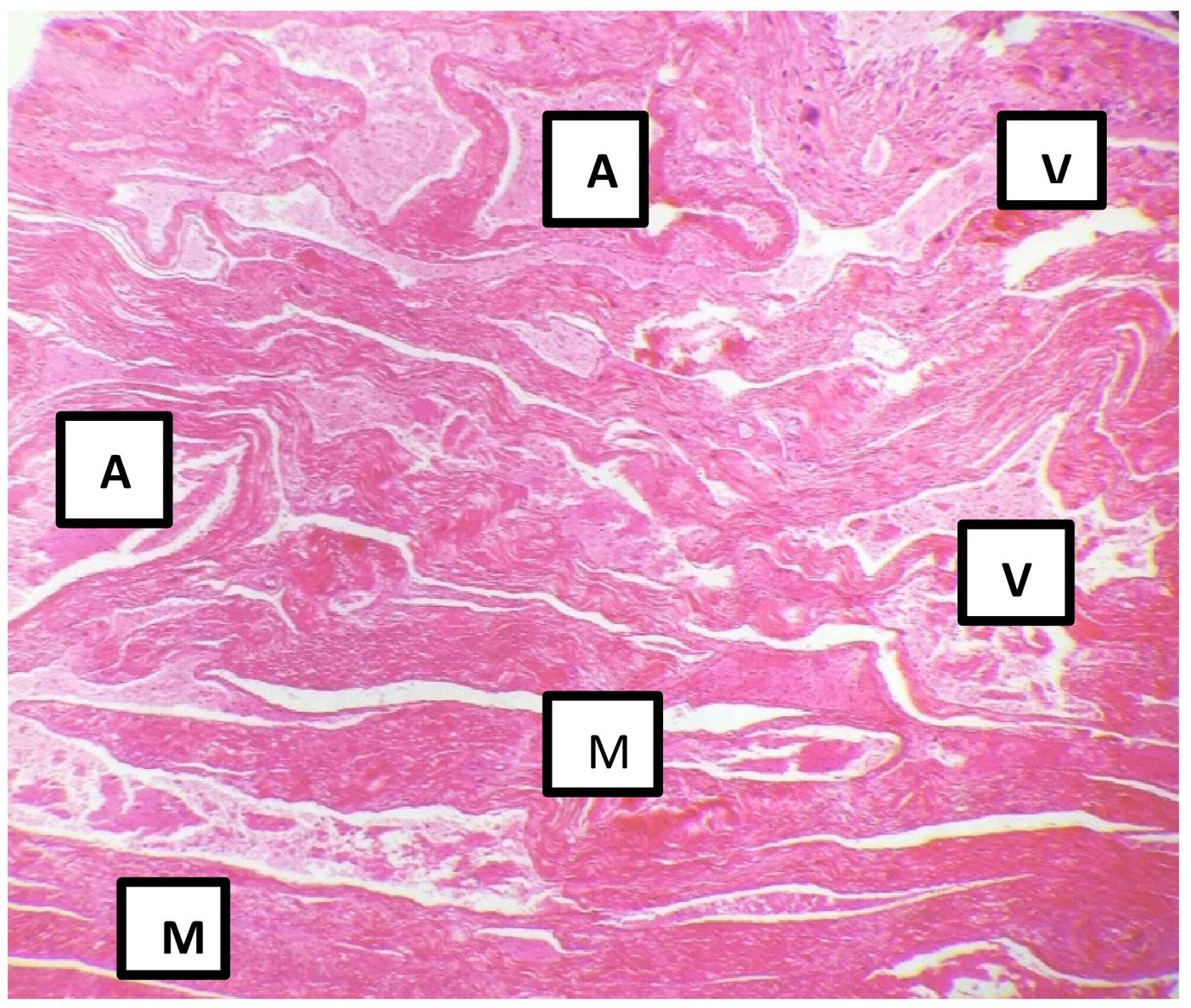
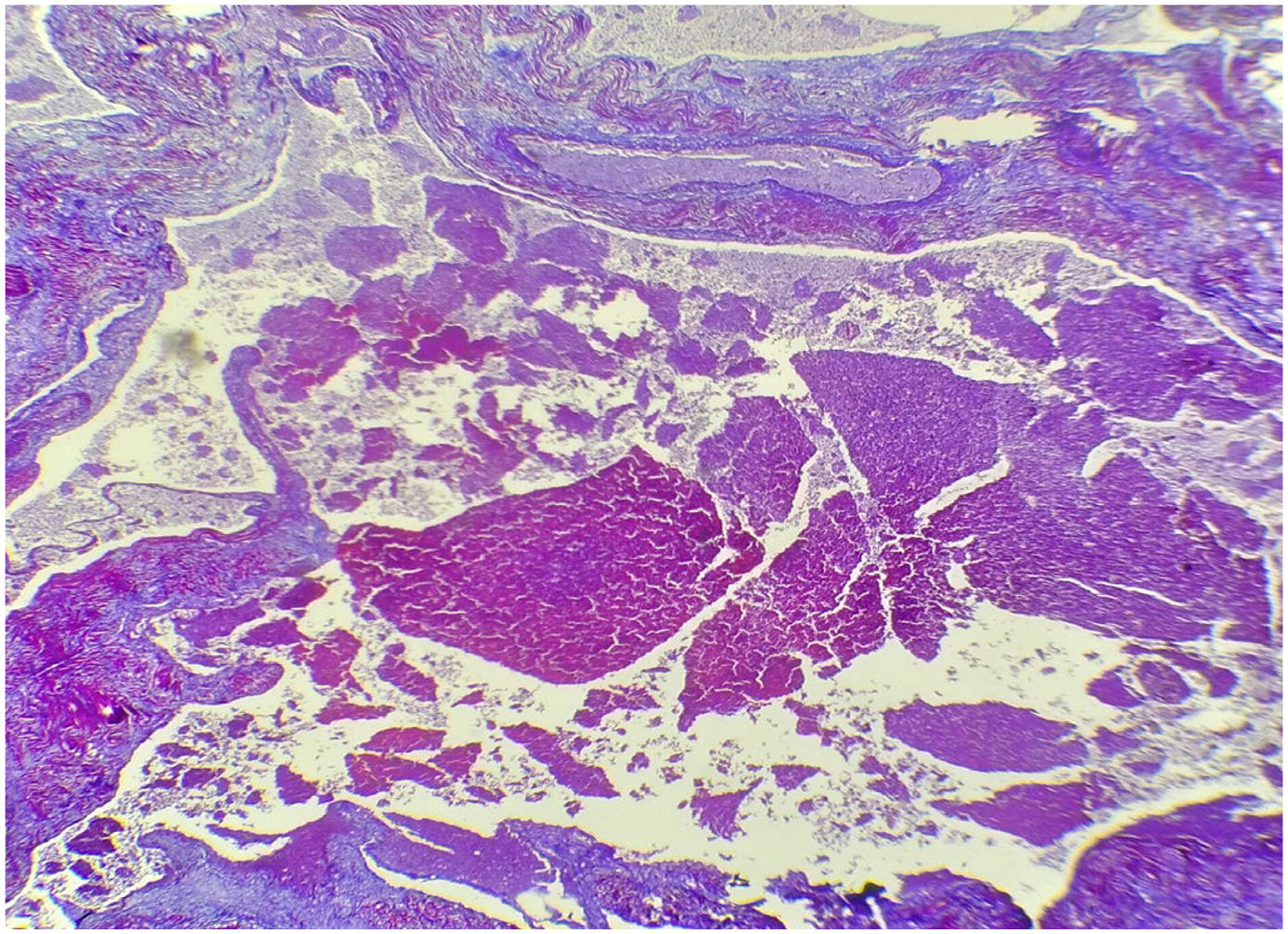
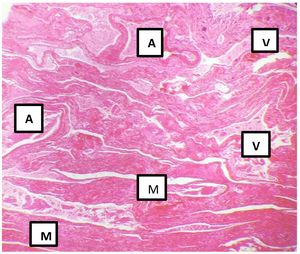
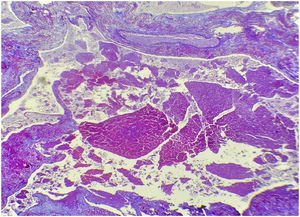
Histological slices of the myometrium showed multiple dilated vascular spaces occupied by haematic coagulates, with no capillaries between them (Fig. 3, Fig. 4).
The anatomical pathology diagnosis was hypovolemic shock due to massive uterine bleeding caused by a UAVM.
DiscussionUAVM is a rare entity that may cause uterine bleeding. It is considered to be a defect of the high flow low resistance vascular system, where abnormal connections of the arteries and veins are identified, characterized by the absence of the capillary network located in the myometrium; this is chiefly due to the increase in the number of vessels due to an anomalous angiogenesis.
These malformations may be congenital or acquired: congenital cases are exceptional, and they include patients who have not previously undergone any intervention on the uterus. A hypothesis is that they originate due to a defect in the differentiation of the primitive capillary plexus during foetal angiogenesis. The acquired cases show myometrial fistulas between the arterial and venous branches. Their arteries stem from normal internal iliac arteries, without vascular supplementation from outside the uterus, and they have the characteristic sphere where patients have undergone an intervention on the uterus such as curettage, a Caesarean, an abortion, a biopsy, cervical or endometrium neoplasia, myomectomy, a trophoblastic disease or direct traumatism of the uterus. Some authors suggest that pregnancy plays an important role in the formation of arteriovenous anomalies. The average age of presentation is 29 years (range 15-51 years).6--11
Worldwide there are approximately 300 reported cases of uterine arteriovenous malformation. These include case reports and observational studies, of which only 5% have been confirmed histopathologically. This is why this case is so important, as we believe that it was acquired, in association with the previous event of a Caesarean, and because of its anatomical location in the uterus.12
The diagnosis of UAVM has traditionally been established afterwards, by histopathological study after a hysterectomy, although it is also possible to use an ECO-Doppler imaging study followed by magnetic resonance imaging, and an angio CT scan to make the diagnosis precise. Hysteroscopy has also been used.
The current treatment of choice in women who wish to conserve their fertility is the embolization of the uterine arteries, or the laparoscopic bipolar coagulation, depending on the size of the lesion, its location and the age of the patient, although selective surgical ablation may also be used.13--15
ConclusionsWithin the field of forensic medicine it is indispensable to evaluate the physiopathological processes which are associated with the basic cause of death, as well as the factors which triggered the same. Autopsy is still a fundamental tool in understanding rare diseases, and the latter may increase as medical science progresses. This progress includes Caesarean operations, which have increased in number in recent years, above all in the Latin American countries even though it is unnecessary in a high percentage of cases. It may give rise to other diseases, including acquired UAVM, and we should keep this in mind in cases of women with a history of surgery in the uterus.
Please cite this article as: Jiménez Herrera R, Fernández Vazquez MU, Hernández y Ballinas A, et al. Muerte materna asociada a una malformación arteriovenosa uterina. Revista Española de Medicina Legal. 2022. https://doi.org/10.1016/j.reml.2022.05.001.