The Embera, an indigenous group in Colombia, particularly in regions like Risaralda, face significant challenges including poverty, displacement, and high rates of preventable diseases. In recent years, there has been a concerning rise in suicide rates within this community. This study presents a case series of 6 Embera patients who attempted suicide with high lethality and were treated in an ICU in Pereira, Risaralda, during 2023. Additionally, a systematic literature review following PRISMA guidelines was conducted to identify studies on suicide among the Embera population, using databases such as PubMed, EMBASE, Web of Science, and Google Scholar, covering articles published between 2000 and 2023. The case series revealed predominant methods of suicide attempts involving substances like Paraquat and the challenges in managing these cases in the ICU. The literature review identified a limited number of studies addressing suicide among the Embera, revealing gaps in understanding the cultural, socioeconomic, and healthcare system factors contributing to these behaviors. The findings underscore the need for comprehensive research and culturally sensitive interventions to address the complex interplay of sociocultural determinants influencing suicide. It is concluded that collaborative efforts involving healthcare professionals, policymakers, and community leaders are essential to develop effective strategies that mitigate suicide risks and promote comprehensive well-being in indigenous communities.
Los embera, un grupo indígena de Colombia, particularmente en regiones como Risaralda, enfrentan desafíos significativos que incluyen pobreza, desplazamiento y altas tasas de enfermedades prevenibles. En los últimos años, se ha observado un preocupante aumento en las tasas de suicidio en esta comunidad. Este estudio presenta una serie de casos de 6 pacientes embera que intentaron suicidarse con alta letalidad y fueron atendidos en una UCI en Pereira, Risaralda, durante 2023. Además, se realizó una revisión sistemática de la literatura siguiendo las directrices PRISMA para identificar estudios sobre el suicidio en la población embera, utilizando bases de datos como PubMed, EMBASE, Web of Science y Google Scholar, abarcando artículos publicados entre 2000 y 2023. La serie de casos reveló métodos predominantes de intentos de suicidio que involucran sustancias como el paraquat y los desafíos en el manejo de estos casos en la UCI. La revisión de la literatura identificó un número limitado de estudios que abordan el suicidio entre los embera, revelando brechas en la comprensión de los factores culturales, socioeconómicos y del sistema de salud que contribuyen a estos comportamientos. Los hallazgos subrayan la necesidad de investigación exhaustiva e intervenciones culturalmente sensibles para abordar la compleja interacción de los determinantes socioculturales que influyen en el suicidio. Se concluye que los esfuerzos colaborativos que involucren a profesionales de la salud, responsables políticos y líderes comunitarios son esenciales para desarrollar estrategias efectivas que mitiguen los riesgos de suicidio y promuevan el bienestar integral en las comunidades indígenas.
The Embera are an indigenous group in Colombia, notably in the regions of Risaralda, Chocó, Antioquia, and Valle del Cauca. They are organized into family clans with collective decision-making, although each community has its own leadership. The Embera group includes the Chami, Katio, Siapidara, and Wounan, and their language is crucial to their culture, though many also speak Spanish.1 Traditional Embera houses are simple huts built from natural materials near rivers. Their economy relies on fishing, hunting, agriculture, and handicrafts, particularly weaving and basket production. Located in rural areas, the Embera are often distant from urban populations, and preserving their ancestral lands and culture has been vital for many years.2
The public health issueThe Embera face numerous challenges, including extreme poverty, land shortages, forced displacement, and high illiteracy rates, predominantly among women. They also suffer from preventable diseases such as malaria, respiratory infections, tuberculosis, diarrheal diseases, malnutrition, alcoholism, drug addiction, chronic diseases, and rising suicide and AIDS rates.3
Since 2009, suicidal behavior among the Embera has increased alarmingly, prompting research into its causes. The suicide rate among Indigenous populations can be up to 40 times higher than the general population.3,4 UNICEF reports a suicide rate of 500 cases per 100,000 among the Embera, compared to 5.2 per 100,000 in the rest of Colombia. Recently, methods have shifted from hanging to exposure to substances like organophosphates and Paraquat.5
There are no systematic reviews linking increased suicidal behavior and high lethality in this population.5,6 A Scoping Review is needed to explore the breadth of research, identify gaps, and make policy recommendations. This study is motivated by the high lethality of suicide attempts among Embera patients treated in an Intensive Care Unit in Risaralda in 2023, where 6 out of 20 cases involved Embera patients, with 5 resulting in death.
The objectives of this Scoping Review are to (a) map the existing literature published since 2000–2023 to identify and evaluate factors that may influence high lethality suicide attempts in the Embera population of Colombia; (b) identify knowledge gaps; and (c) include recommendations on how to advance research on this distinct population.
MethodsInitially, summarized clinical information is presented for 6 Embera patients who attended an ICU in Pereira, Risaralda, Colombia, from January to October 2023.
The scoping review followed the original methodological framework suggested in the literature. The method and five stages are described below. To ensure rigor and guide reporting, the PRISMA Extension for Scoping Reviews was followed (see PRISMA-ScR checklist Appendix A).
Identifying the research questionThe following research question guided the Scoping Review: What are the factors that influence high lethality suicide attempts in the Embera population?
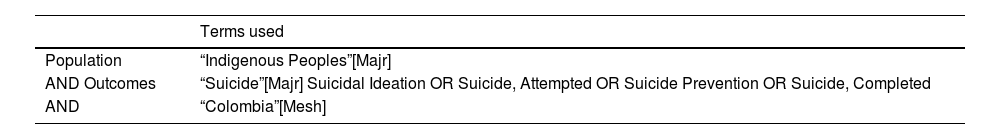
Identifying relevant studiesPubMed, EMBASE, Web of Science, and Google Scholar were searched. Search terms covered the population and outcomes relevant to the research question and included overlapping terms to ensure that the broadest possible scope of studies was identified by searching the electronic databases (Table 1). A copy of the PubMed search is included (Appendix B). The second step consisted of reviewing the reference list of the studies identified in the search of electronic databases to identify any additional studies. The searches were conducted between October and November 2023. The reason for taking the year 2000 as the cut-off point for the beginning of observation is because it was in that decade that an increase in suicidal behavior in this population began to be observed.
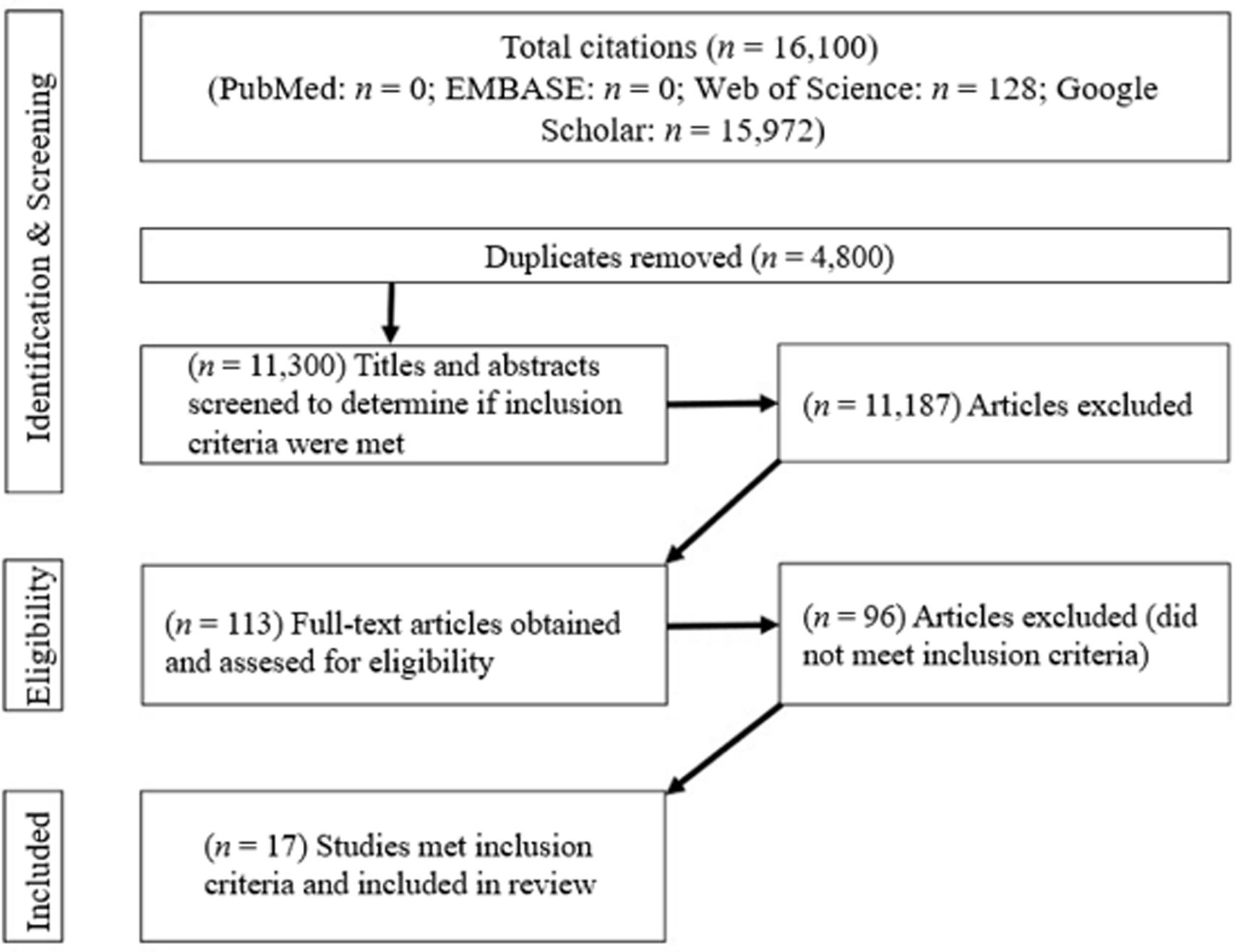
Study selectionThe PRISMA-ScR flowchart (Fig. 1) documents the search and study selection process. The search strategies generated an initial set of 16,100 articles. Using EndNote, 4800 duplicates were identified and eliminated. The titles and abstracts of the 11,300 articles were reviewed, of which 11,187 were eliminated. The remaining 113 articles were reviewed in depth, resulting in the deletion of another 96 articles.
The following predefined inclusion criteria were applied: (a) research published between 2000 and 2023; (b) published in Spanish or English; (c) studies addressing suicide attempts in the Embera population; (d) studies addressing characteristics of the mechanism and lethality of suicide attempt as well as its survival; (e) reported data collected by quantitative, qualitative or mixed methods.
The following exclusion criteria were applied: (a) prevalence studies alone; (b) reviews, abstracts, dissertations, books, commentaries, editorials, and letters; (c) studies whose target population was indigenous people from countries other than Colombia.
Initially, one author (MA) screened the retrieved titles and abstracts for eligibility. The full text of potentially eligible articles was retrieved, and MA reviewed them to determine whether they met the inclusion criteria. Two authors (LC and CJ) double-screened 10% of eligible articles, respectively. The identified studies were then subjected to a second screening phase in which the full text of each article (LC and JF) was read to determine whether all inclusion criteria were met. The reference lists of these articles were reviewed, but no additional articles were identified for inclusion.
Data chartingData were extracted and tabulated in Microsoft Excel (2019). Two templates were generated for this stage. The first template consisted of plotting descriptive data for each study: authors, year of publication, country, study design, setting, sampling method, sample size and makeup, and materials used. Data extraction was performed independently by MA and JF, and conflicts were resolved where a final decision was agreed upon.
Collating, summarizing, and reporting resultsThe heterogeneity of the methodologies necessitated a qualitative synthesis of the research results rather than a quantitative meta-analysis. This approach is distinct from reviews that perform a thematic summary of qualitative research and is consistent with the specific focus of the scoping review. No formal assessment of study quality was performed, which was consistent with the nature of scoping reviews. The categorization, summarizing and report of the results for the article were performed by MM, JM and GM.
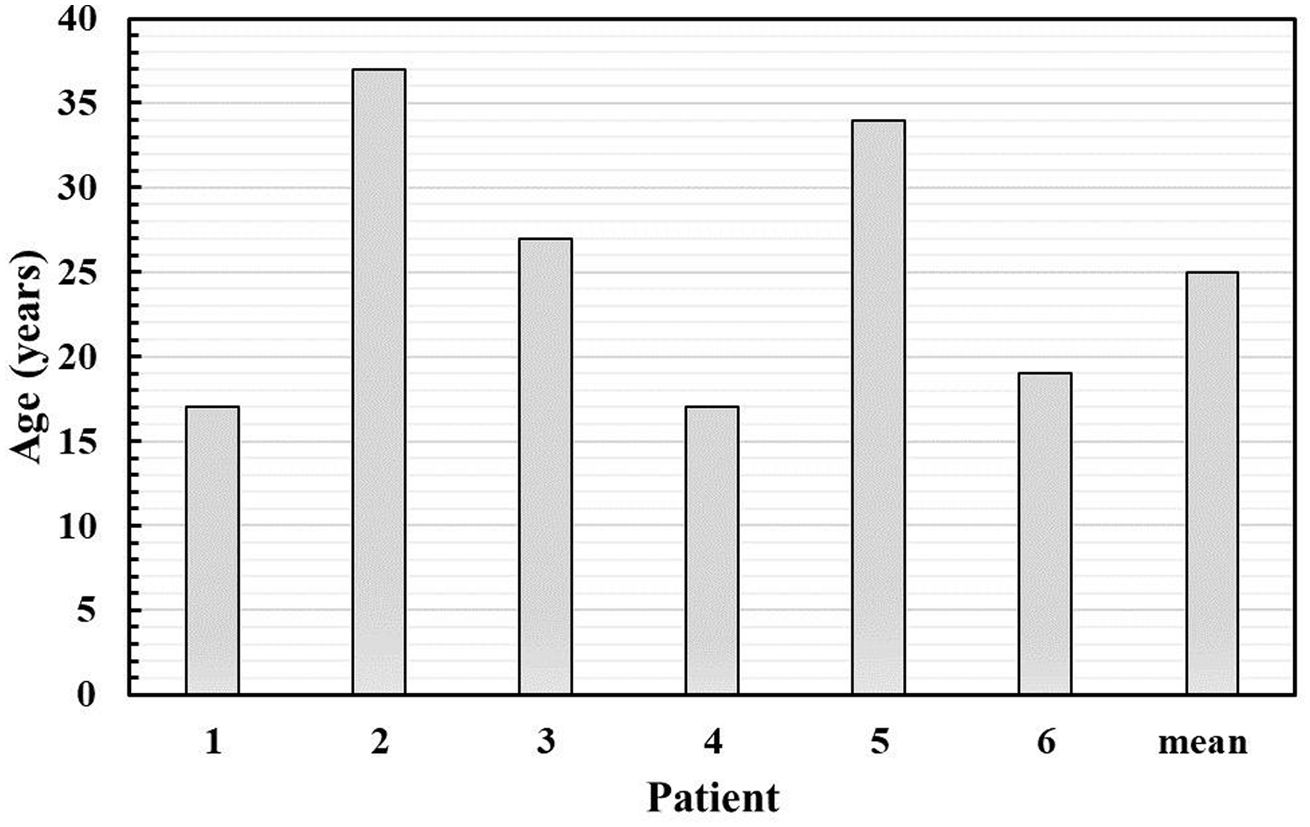
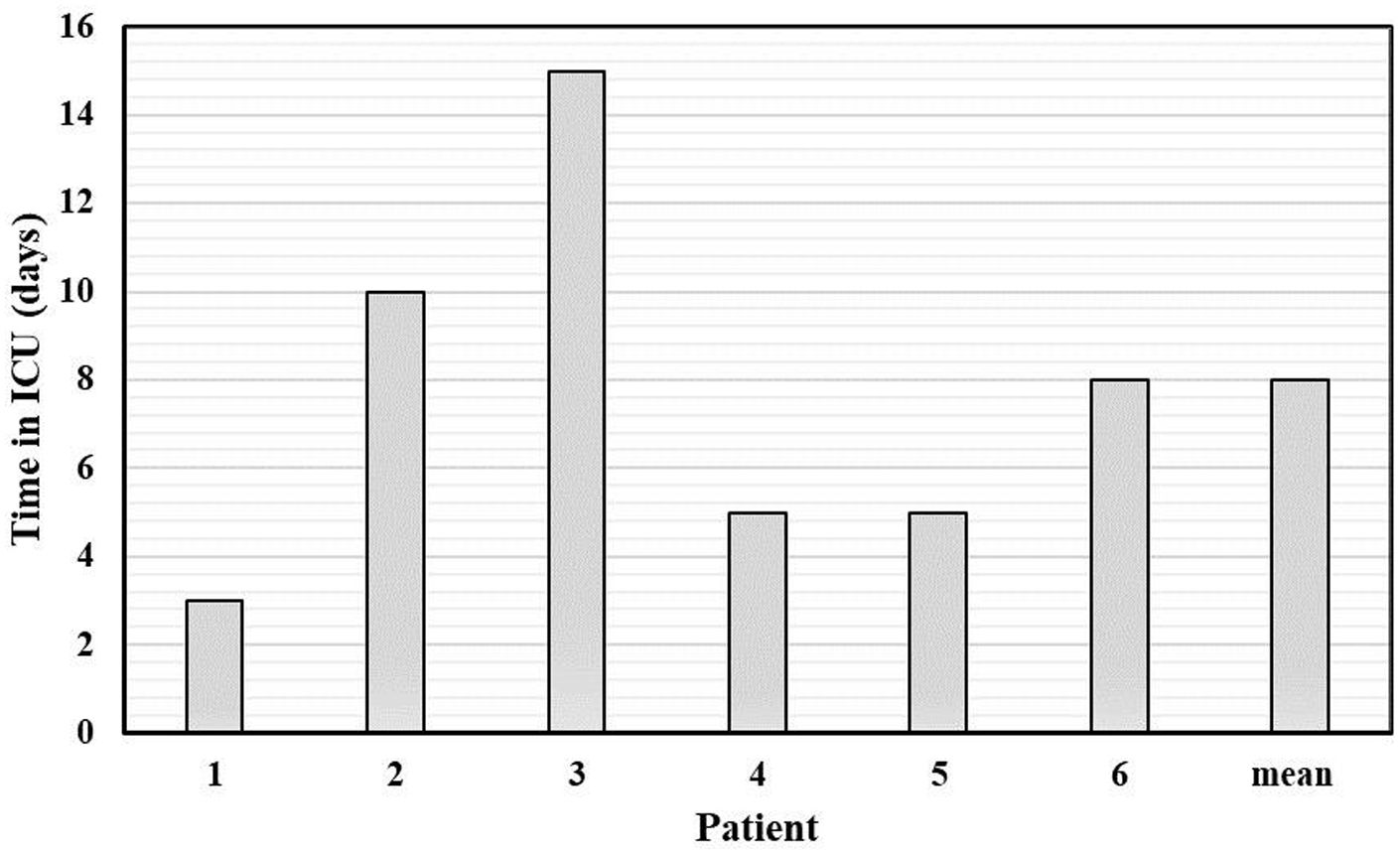
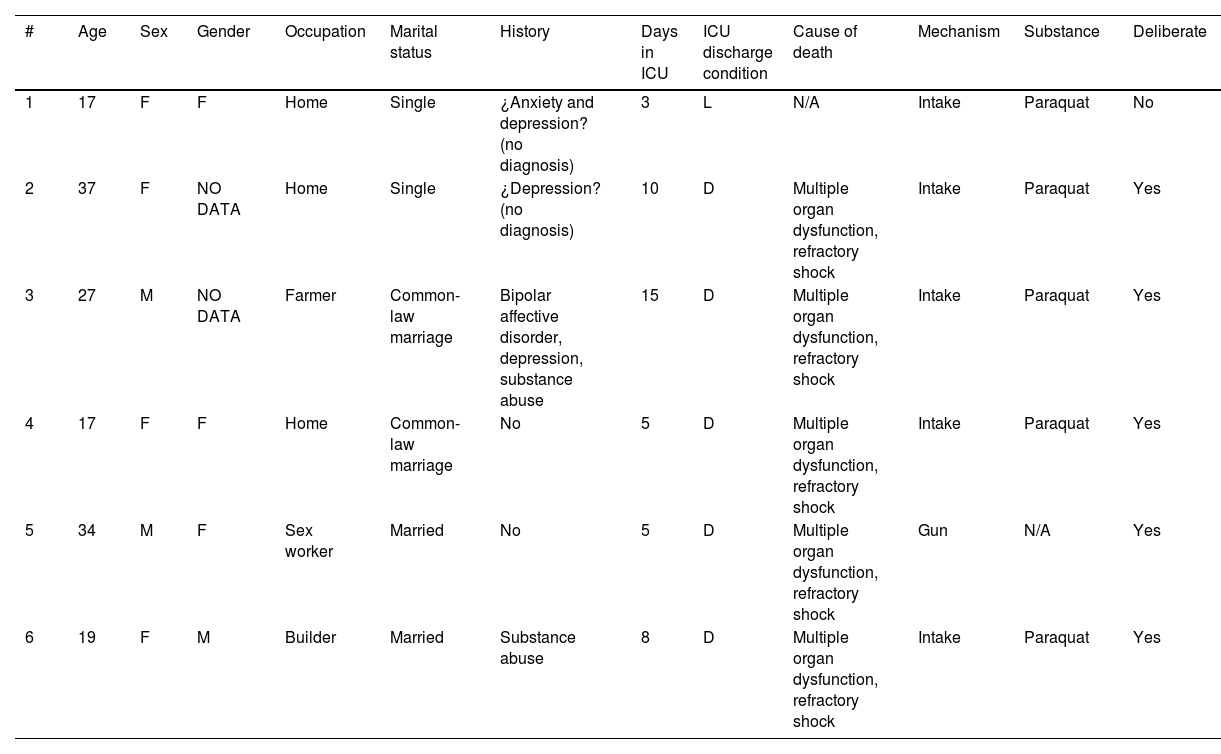
ResultsThe cases that motivated this reviewIn a tertiary-level hospital in Pereira, Risaralda, Colombia, 20 cases of high-lethality suicide attempts were treated in the ICU from January to October 2023. Of these, 30% (n=6) were Indigenous Embera. The average ICU stay was 7.6 days (range 3–15 days). Among the 6 cases, 83% (n=5) involved ingestion of Paraquat, a highly lethal substance, with one case reported as accidental but still requiring ICU care. The other case involved an intentionally self-inflicted gunshot wound, resulting in death due to injury severity. Detailed sociodemographic characteristics are described in Table 2, Figs. 2 and 3.
Sociodemographic characteristics of the patients.
| # | Age | Sex | Gender | Occupation | Marital status | History | Days in ICU | ICU discharge condition | Cause of death | Mechanism | Substance | Deliberate |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 | 17 | F | F | Home | Single | ¿Anxiety and depression? (no diagnosis) | 3 | L | N/A | Intake | Paraquat | No |
| 2 | 37 | F | NO DATA | Home | Single | ¿Depression? (no diagnosis) | 10 | D | Multiple organ dysfunction, refractory shock | Intake | Paraquat | Yes |
| 3 | 27 | M | NO DATA | Farmer | Common-law marriage | Bipolar affective disorder, depression, substance abuse | 15 | D | Multiple organ dysfunction, refractory shock | Intake | Paraquat | Yes |
| 4 | 17 | F | F | Home | Common-law marriage | No | 5 | D | Multiple organ dysfunction, refractory shock | Intake | Paraquat | Yes |
| 5 | 34 | M | F | Sex worker | Married | No | 5 | D | Multiple organ dysfunction, refractory shock | Gun | N/A | Yes |
| 6 | 19 | F | M | Builder | Married | Substance abuse | 8 | D | Multiple organ dysfunction, refractory shock | Intake | Paraquat | Yes |
Management followed national intoxication guidelines with toxicology hotline support. Four patients with severe intoxication required advanced life support, including ventilatory support, vasopressors, sedoanalgesia, renal replacement therapy, and comprehensive care by healthcare personnel with social work and psychological support for families. Despite all efforts, all patients died due to refractory shock and multiple organ dysfunction.
Search resultsOf the 16,100 articles identified by searching electronic databases, 17 met the inclusion criteria.
Description of reviewed studiesMost of the studies were published between 2015 and December 2020 (n=14), and all were conducted in Colombia. Most of the studies addressed the problem of indigenous peoples in the country from a bio-psycho-social perspective (n=15). Only one addressed the situation in the Latin American population, where many indigenous peoples share geographical and cultural relationships.
In the Colombian context, we find the Department of Risaralda among those that, during the years 2020 and 2021, had the highest rates of suicide attempts reported in the Colombian Public Health Surveillance System (SIVIGILA) platform; the classification data by age groups allow us to identify that the range in which most suicide attempts are presented is between 15 and 19 years old.7 In addition, data provided by the Secretary of Health of Risaralda show that, in the first half of 2022, 509 cases were reported in this department, of which 68% correspond to adolescents and young people between 12 and 26 years of age (2022).8
DiscussionSuicide has emerged as a critical issue in some Indigenous communities, previously believed to be insulated against such behaviors. While the general causes of suicide in Indigenous populations may be similar, the Embera face unique cultural and social challenges that exacerbate the problem. From an epidemiological standpoint, suicide should be understood as a social phenomenon rather than an individual one, resulting from an imbalance between destructive and protective health processes.2,9 This perspective emphasizes the necessity of addressing both the broader social determinants and the specific cultural factors contributing to the crisis.
Suicide in this group, known as Bera Detasí, “almost killed himself,” and Mietabú beabatao, “killed himself,” has multiple connotations and is far from being just a symptom, as it is often approached in the medical practice. In a local study on the conception of suicide in this population they emphasize that suicide is a form of resistance and a rejection response to the loss of territory, a cultural fracture, as well as moods that they mention as “boredom,” “boredom,” “banzo,” “vital listlessness,”; partly derived from the cultural syncretism through the years with the groups of black descent, the Catholic religion, and with the white-mestizos.10
For the Embera, health intertwines the body, community, and spirituality. This interrelationship makes the Embera have wikira ekni, “mental health,” which implies fulfilling the pre-established social roles within the community and following the tradition while preserving their culture. Any disruption can lead to resistance and confrontation, which not only occurs externally but also may derive from an internal conflict between adopting a new set of beliefs and keeping the pre-established. Suicidal behavior is therefore seen as an “adaptive” response to their suffering. For that reason, Therefore, culturally sensitive diagnosis and intervention are crucial, as Western medical practices can exacerbate stress in an already emotionally fragile individual.10
Among the multiple causes of suicide found, some can be associated, but not limited to:
- 1.
Displacement and land loss: over 50 years of land struggles and forced displacement have severely impacted the Embera, causing cultural identity loss and acts of violence. Globalization and educational systems that ignore Indigenous cultural identity exacerbate these issues.6
- 2.
Violence and armed conflict: the areas where the Embera communities live have been historically affected by violence and armed conflict. Forced involvement with illegal groups has been documented, losing the opportunity to carry out their traditional activities and roles. This violent social pressure and high-stress environment increase the risk of suicide.5,6,11,12
- 3.
Limited access to health and mental health services: indigenous communities often find it challenging to access quality health care services, among other reasons, due to their geographical distribution and their healthcare perception. Hierarchical figures often manage initial treatments, delaying professional medical intervention and increasing morbidity and mortality.12,13
- 4.
Political and socioeconomic inequalities: government policies do not provide a detailed and strong structure for coexistence and development. This context of lack of opportunities contributes to a shortage of economic resources and difficulties obtaining essential household goods can lead to the feeling of hopelessness.14
- 5.
Substance abuse: alcohol and drug abuse pose significant risks within the Embera community, often misunderstood and inadequately addressed due to cultural perceptions and limited access to appropriate healthcare. Substance abuse increases the likelihood of developing affective disorders such as depression and anxiety, which are strongly associated with suicidal behavior. The Embera's traditional understanding of mental health and illness does not always align with Western medical concepts, leading to delays in recognizing and treating substance-related disorders.12,14
- 6.
Social pressure and expectations: cultural expectations and technological influences significantly impact the Embera community, adding stress and contributing to altered self-image and gender identification issues, which can lead to conflicts and potentially suicidal behavior. The advent of the Internet, while a source of valuable information, also exposes individuals to harmful challenges and misinformation that can negatively affect mental health.8
In the studied sample, two patients experienced cultural shock, describing physical traits and dress corresponding to the opposite gender, possibly indicating transgender or gender nonconforming identity. This situation highlights the complex interplay between traditional cultural norms and modern influences. The Embera's traditional values may not readily accept non-conforming gender identities, leading to social and family discrimination. This discrimination can exacerbate feelings of isolation, depression, and hopelessness, increasing the risk of suicidal behavior. Additionally, these individuals often face internal conflicts as they navigate their identities within a community that may not fully understand or support them.15 Interviews with relatives of the patients revealed previous drug use and unclear diagnoses of depression or bipolar disorder.
- 7.
Act of resistance: this phenomenon goes back to historical facts, precisely to colonial times, where collective suicides were seen as an action of resistance against invasion. Bearing in mind that people use their oral traditions to disseminate their customs and knowledge, these previously used practices are part of the information that may be related to the structuring of the suicidal idea.5
- 8.
Incidence of previous suicides: the occurrence of previous suicide cases within the Embera communities can have a profound and detrimental effect, potentially normalizing the behavior and increasing the risk of future incidents. When a community experiences multiple suicides, it can create a sense of inevitability or acceptance of suicide as a coping mechanism for dealing with distress and hardship.
The medical care of indigenous communities poses unique challenges for healthcare professionals, and critical care specialists are no exception. The most common high-lethality suicide attempt in this population group has gone from violent methods to primarily ingesting narcotics and multiple substances, complicating targeted therapeutic approaches communication difficulties with patients and their families, coupled with ICU conditions not tailored for Indigenous needs, hinder the participation of families and community leaders and the incorporation of traditional measures, which could support patient outcomes. The precarious clinical conditions, including poor history, nutrition, and chronic disease control, further complicate care for the Embera.16
From a cultural point of view, the intensivist needs to understand the gaps that exist not only in linguistics but also conceptual differences and population expectations when one of their members is admitted to the ICU. Educating the entire intensive care team on these differential conditions is necessary to provide effective care. Recognizing the importance of community and family in an Embera's life is crucial for addressing suicide effectively.16–18
Suicide treatment and prevention in the Embera community requires an interdisciplinary approach involving mental health professionals, social workers, community leaders, and other experts. The critical care physician can play a crucial role in identifying at-risk patients serving as an early warning for the prevention and timely management of other critical events in the patient's community.16,18,19
A public health approach is essential for better prevention and health care promotion. Educating the community allows the recognition of behaviors that may trigger suicide attempts and strengthens initial management and rapid referral to health centers. Informing adults about the lethality of the substances to which they may have access can generate a restrictive use of such chemicals and thus impact the availability of the input for people at risk.20
Sharing this information with at-risk populations could improve responsiveness in initial healthcare units. Over time, timely primary care could influence beliefs about suicide, providing new generations with better tools to face difficulties, supported by governmental institutions. The high lethality of substances, depending on dose and time elapsed since ingestion, often leads to fatal outcomes, especially during transport to the ICU. Despite adequate treatment, patients frequently die from multiple organ dysfunction caused by toxins, necessitating vigilant care teams and timely intervention.8,21
Recommendations for future researchThis review highlights the critical need for specialized research to better understand and classify the factors associated with suicide in the Embera population. Historically, studies on this issue have lacked robust theoretical frameworks, limiting their ability to reveal the deeper processes and dynamics that drive suicidal behavior. Future research should aim to uncover these underlying mechanisms, tracing the trajectory from initial suicidal ideation to high-lethality attempts. This comprehensive approach may benefit from incorporating molecular and genetic studies to provide a more holistic understanding of the increasing incidence of high-lethality suicide attempts.
Employing qualitative research methods might be very helpful constructing robust theories about suicide within Indigenous communities. Future studies should explore the Embera's cultural beliefs about suicide, examining how these beliefs are perceived across different age groups and the role of support networks within the community and healthcare settings. Understanding these cultural nuances and communication networks can help predict the development of suicidal ideation and inform effective prevention strategies.
Additionally, research should move beyond mere descriptive studies that use demographic characteristics as stand-ins for psychographic variables. Instead, it should focus on systematically testing relevant predictors identified through theory-based approaches to assess the impact of psychosocial and health interventions on suicide rates. This shift toward more rigorous, theory-driven research will provide a clearer picture of the factors contributing to suicide and the most effective ways to address them.
It is essential to consider the situation of other indigenous communities in Colombia and Latin America, as they face similar challenges regarding mental health and suicide risk. Previous studies have identified that indigenous populations like the Embera are not the only ones affected by high rates of suicidal behavior. Comparing the findings of this research with communities such as the Embera Chamí in Colombia and other indigenous groups across Latin American countries could provide a broader context and enrich the analysis, offering insights into how cultural, social, and economic factors contribute to this phenomenon in different regional settings.
LimitationsLike all research, this review has limitations. Focus on high-lethality suicide attempts in the Embera population, excludes studies on the broader prevalence of suicide among Indigenous people in Colombia and Latin America, limiting the generalizability of the finding. Additionally, the reliance on secondary data from studies published between 2000 and 2023 means historical data that could offer further insights were not considered. Methodological constraints required a qualitative synthesis instead of a quantitative meta-analysis, and no formal assessment of study quality was performed, potentially affecting the robustness of the findings. The review also highlighted the lack of robust theoretical frameworks in existing studies, limiting the depth of understanding of suicidal behavior dynamics. Significant barriers in accessing health and mental health services for the Embera were noted but not extensively quantified, pointing to the need for more research on healthcare systems’ roles. Finally, while emphasizing culturally sensitive strategies, the review recognized that many current healthcare practices may not align with Embera cultural contexts, necessitating further investigation into culturally appropriate interventions.
ConclusionThe comprehensive review presented here illuminates critical insights into the complexities of addressing high-lethality suicide attempts within special populations. It underscores the pervasive influence of socio-cultural determinants such as displacement, violence, substance abuse, and socio-economic disparities, which collectively contribute to elevated suicide rates. Importantly, the study identifies significant gaps in current research, emphasizing the need for robust theoretical frameworks and qualitative methodologies to better understand the underlying cultural beliefs and support structures that shape suicidal behaviors. Moreover, the review highlights the inadequacies of existing healthcare systems in meeting the specific needs of Indigenous communities, underscoring the imperative for interdisciplinary, culturally sensitive approaches in suicide prevention and intervention. Moving forward, there is a clear call to action for researchers, healthcare professionals, and policymakers to collaborate on developing evidence-based strategies that address these multifaceted challenges comprehensively, aiming not only to reduce suicide rates but also to promote holistic well-being across diverse populations globally.
Ethics approval and consent to participateThis report was written following Helsinki's declaration. Ethical approval is not required for this type of case report.
Consent for publicationInformed written permission was obtained from a relative of each patient.
FundingNone.
Conflicts of interestNone of the authors declare conflicts of interest.
To the intensive care unit staff of the Hospital Universitario San Jorge. Pereira, Risaralda, Colombia.
Special thanks to Dr. Julio César Gutiérrez Segura, who guided the development of this work from the hospital's psychiatry department.