Health communications are only effective if target audiences actually receive the messages. One potential barrier to effective health communication is the potential stigma of attending to health information, particularly for stigmatizing health issues. The purpose of the present paper was to examine when participants report self-conscious emotions (e.g., shame, embarrassment) in response to health communications, as well as likelihood of reading health information associated with these emotions. Across three studies, participants read information about preventing diseases that are either highly stigmatized or non-stigmatized. Increased accessibility of stigma cues by (a) manipulating the perceived absence vs. presence of others, or (b) measuring lower vs. higher rejection sensitivity resulted in increased self-conscious emotions in response to information about stigmatized health issues. In addition, stigma cues decreased the likelihood of reading information about stigmatized (but not non-stigmatized) health information. Implications for health outcomes and intervention design are discussed.
La comunicación en torno a la salud solo es efectiva si la audiencia meta recibe el mensaje. Una barrera potencial que tiene la comunicación efectiva sobre salud es el estigma potencial de hacer caso a la información sobre salud, particularmente en temas estigmatizados. El objetivo del presente estudio fue examinar cuándo reportan los participantes emociones conscientes (p.e. vergüenza, culpa) en respuesta a comunicación sobre salud, así como la probabilidad de leer información asociada con estas emociones. A través de tres estudios, los participantes leyeron información sobre prevención de enfermedades que son altamente estigmatizadas o que no lo son. El aumento de la accesibilidad de las señales sobre estigma mediante (a) la manipulación de la ausencia percibida vs. presencia de otros, o (b) la medición de alta o baja sensibilidad al rechazo, resultó en aumento de emociones conscientes en respuesta a la información sobre temas de salud estigmatizados. Además, las señales sobre estigma disminuyeron la probabilidad de lectura de información sobre información estigmatizada (no así para la no estigmatizada). Se discuten las implicaciones sobre consecuencias de salud y diseño de intervención.
Public health researchers and practitioners are concerned with minimizing the prevalence and deleterious consequences of various health conditions. To facilitate this agenda, many public health campaigns have been designed with an eye towards reducing negative health outcomes by increasing awareness of the causes and consequences of health conditions and facilitating disease prevention. However, recent evidence suggests that messages may not be reaching target audiences as individuals who already engage in recommended health behaviours are more likely to actively seek out preventive communications than those who are currently not complying with the recommendation (Earl, Albarracin, Durantini, Gunnoe, Leeper, & Levitt, 2009). Therefore, public health researchers and practitioners must be aware of whether their messages actually reach the audiences for which they are designed.
One potential factor to consider when examining impact of health promotion messages is emotional response to these communications. Although much pas work has delineated the effects of fear in health-promotion interventions (Earl & Albarracin, 2007; Fisher & Fisher, 1992; 2000; Janz & Becker, 1984; Rogers, 1975; Rosenstock, Stecher, & Becker, 1994), in the case of such stigmatized health conditions as Human Immunodeficiency Virus (HIV) or herpes genitalis, selfconscious emotions such as shame or embarrassment may influence attention to a preventive message. In particular, similar to fear, self-conscious emotions can trigger escaping information that elicits the emotion (Clore et al., 1994; Fridja et al., 1989; Siegel & Schrimshaw, 2000). Specifically, individuals are less likely to seek testing for sexually transmitted infections when they feel shame or believe that others would evaluate them negatively (e.g., blame) them for being infected (Fortenberry et al., 2002; Meiberg, Bos, Onya, & Schaalma, 2008). Furthermore, perceived HIV-stigma may prevent disclosure of HIV-positive status to potential relationship partners, thus increasing the spread of HIV within social networks (Derlega, Winstead, Greene, Serovich, & Elwood, 2002).
Similarly, the decision to approach health information may be based, in part, on situational and chronic cues to stigma and subsequent self-conscious emotions. First, the presence of others may influence the activation of stigma cues by heightening norms about how to behave (Ajzen & Fishbein, 1980, 2005; Fishbein & Ajzen, 1975; Goffman, 1963; Shah, 2003). People are often concerned that reading information about preventing a stigmatized health issue may signal that they are infected with the disease (Albarracin, Durantini, & Earl, 2006). As a result, people may report increased self-conscious emotions following information about preventing a stigmatized health issue when that information is presented in the presence of others.
Second, people who are sensitive to rejection (Downey & Feldman, 1996) may be more aware of the potential for stigma and self-conscious emotions in any circumstance (Mendoza-Denton et al., 2002) and thus participants who are chronically sensitive to stigma cues may experience the most shame and embarrassment when information about preventing stigmatized health issues is presented in the presence of others. Taken together, information about preventing stigmatized health issues should elicit self-conscious emotions particularly when environmental or personal conditions strengthen the impact of stigma cues.
In this paper, we examined conditions under which stigma cues would moderate the experience of self-conscious emotions, and whether or not the experience of self-conscious emotions would predict likelihood of attending to health communications. Specifically, we considered if (a) the perceived presence vs. absence of others, or (b) chronic sensitivity to stigma cues would result in increased self-reported self-consciousness following brochure titles or scenarios about preventing stigmatized health issues. Furthermore, we tested the possibility that stigmatized health information may elicit a general negative response, rather than specifically elicited self-conscious emotions, by also measuring fear. Finally, we examined whether the likelihood of attending to stigmatized (versus nonstigmatized) health communications varied as a function of whether or not the information was presented in the perceived presence (versus absence) of others, and if the likelihood of attention varied as a function of stigma cues (versus fear).
Study 1: OverviewStudy 1 investigated if health brochure titles elicited more or less selfconscious emotions when presented in the perceived presence versus absence of others. We hypothesized that self-conscious emotions in response to brochure titles about stigmatized health issues would be higher in the perceived presence versus absence of others.
MethodParticipants and DesignParticipants were sixty-two Introductory Psychology students in a University Subject Pool who received partial course credit in exchange for their participation. Participants were of both genders (29 men, 33 women) and ethnically diverse (4 African-Americans, 39 European-Americans, 10 Asian-Americans, 4 Latino- Americans, and 5 “Other”). The design was a 2 (Presence of others: Others versus Alone) X 2 (Information type: Stigmatized vs. Control) within-subjects factorial.
Materials and methodsMaterials. Participants viewed brochure titles about both stigmatized and control health issues. Stigmatized health brochures (e.g., The Reality of HIV) included titles on topics that were rated as being more stigmatized in a pre-test (Chlamydia, Genital Herpes, Genital Warts, Gonorrhoea, Haemorrhoids, Hepatitis, HIV, Pubic Lice, Scabies). Control health brochures (e.g., Fight the Flu) included titles on topics that were rated as being less stigmatized in a pre-test (Blood Pressure, Carpal Tunnel, Chicken Pox, Flu, Health Disease, Mononucleosis, Salmonella, Vitamin Deficiency, West Nile Virus).
Measures. Participants were asked to evaluate how self-conscious they would feel while reading each brochure either alone or when others were present based on the brochure title. Self-Consciousness when Alone was measured with three items, How ashamed would you feel? How embarrassed would you feel? and How stigmatized would you feel? on ten-point scales ranging from 1 (not at all) to 10 (extremely) (Cronbach's = .86). Self-Conscious when Others Were Present was measured with three items, How ashamed would you feel when others were present? How embarrassed would you feel when others were present? and How stigmatized would you feel when others were present? on ten-point scales ranging from 1 (not at all) to 10 (extremely) (Cronbach's α= .87).
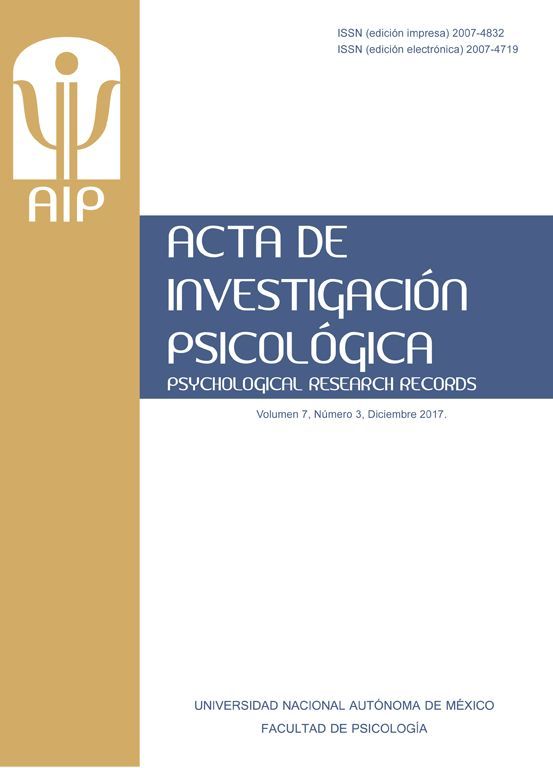
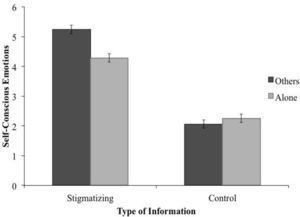
Results and DiscussionWe tested the hypothesis that participants reported increased self-conscious emotions following stigmatized (versus control) information in the perceived presence (versus absence) of others. We used repeated-measures analysis of variance (ANOVA) with presence of others and information type as two withinsubjects factors predicting self-reported self-conscious emotions. There was a significant two-way interaction between presence of others and information type on self-conscious emotions (F1, 61=61.74, p<.001; partial η2 = .50; see Figure 1). Furthermore, following stigmatized information, participants reported more selfconscious emotions in the perceived presence versus absence of others (Mothers = 5.24, SDothers = 0.33; Malone = 4.28, SDalone =0.28; F1, 61 = 44.37, p = .001; Cohen's d = 3.10). However, following control information, participants reported less selfconscious emotions in the perceived presence versus absence of others (Mothers = 2.06, SDothers= 0.15; Malone = 2.25, SDalone =0.14; F1, 61 = 7.28, p = .01; Cohen's d = 1.31). These results suggest that stigma cues such as the perceived presence versus absence of others increased reporting of self-conscious emotions following brochure titles about stigmatizing health issues.
Study 2: OverviewIn Study 1, we examined environmental stigma cues (e.g., perceived presence versus absence of others). However, we have yet to determine if chronic stigma awareness contributes to the level of self-conscious emotions reported in response to information about preventing stigmatized conditions. In particular, we predicted that participants who are high in rejection sensitivity should experience the highest levels of self-conscious emotions when presented with scenarios about preventing stigmatized diseases when the scenario contains information that others are present. Thus, Study 2 examined if chronic and environmental factors associated with cues to stigma interacted or influenced self-conscious emotions additively. Furthermore, we examined if these effects would be localized on selfconscious emotions, or would generalize to negative emotionality in general by assessing self-reported fear.
MethodParticipants and designParticipants were fifty-seven Introductory Psychology students in a University Subject Pool who received course credit in exchange for their participation. Participants were of both genders (30 men, 27 women) and ethnically diverse (2 African-Americans, 32 European-Americans, 12 Asian-Americans, 10 Latino-Americans, and 1 “Other”). The design was a 2 (Information type: stigmatized vs. control) X 2 (Presence of others: others versus alone) X Continuous (Chronic sensitivity to stigma cues) mixed factorial design. In this experiment, information type and presence of others were within-subjects factors and chronic sensitivity to stigma cues was a between-subjects factor.
Materials and measuresMaterials. Participants evaluated eight scenarios varying on two dimensions: stigmatized/control health issue and presence/absence of others. A sample scenario read: While waiting for your appointment at McKinley Health Centre, you decide to read some brochures. The first one says, “The Truth about Genital Herpes” (“Factors that Affect Blood Pressure”). As you look up, you recognize a classmate watching you (realize you are alone).
Measure of chronic sensitivity to stigma cues. Chronic sensitivity to stigma cues was assessed with the Adult Rejection Sensitivity Questionnaire (RSQ; Downey & Feldman, 1996). The scale contains eight scenarios that cover a variety of issues such as borrowing money for one's parents, having an important conversation with a friend, or discussing the issue of sexual protection with one's significant other (α= .77).
Emotion measures. The self-conscious emotions measures were identical to Study 1. Fear was measured with How scared would you feel? on a ten-point scale from 1 (not at all) to 10 (extremely).
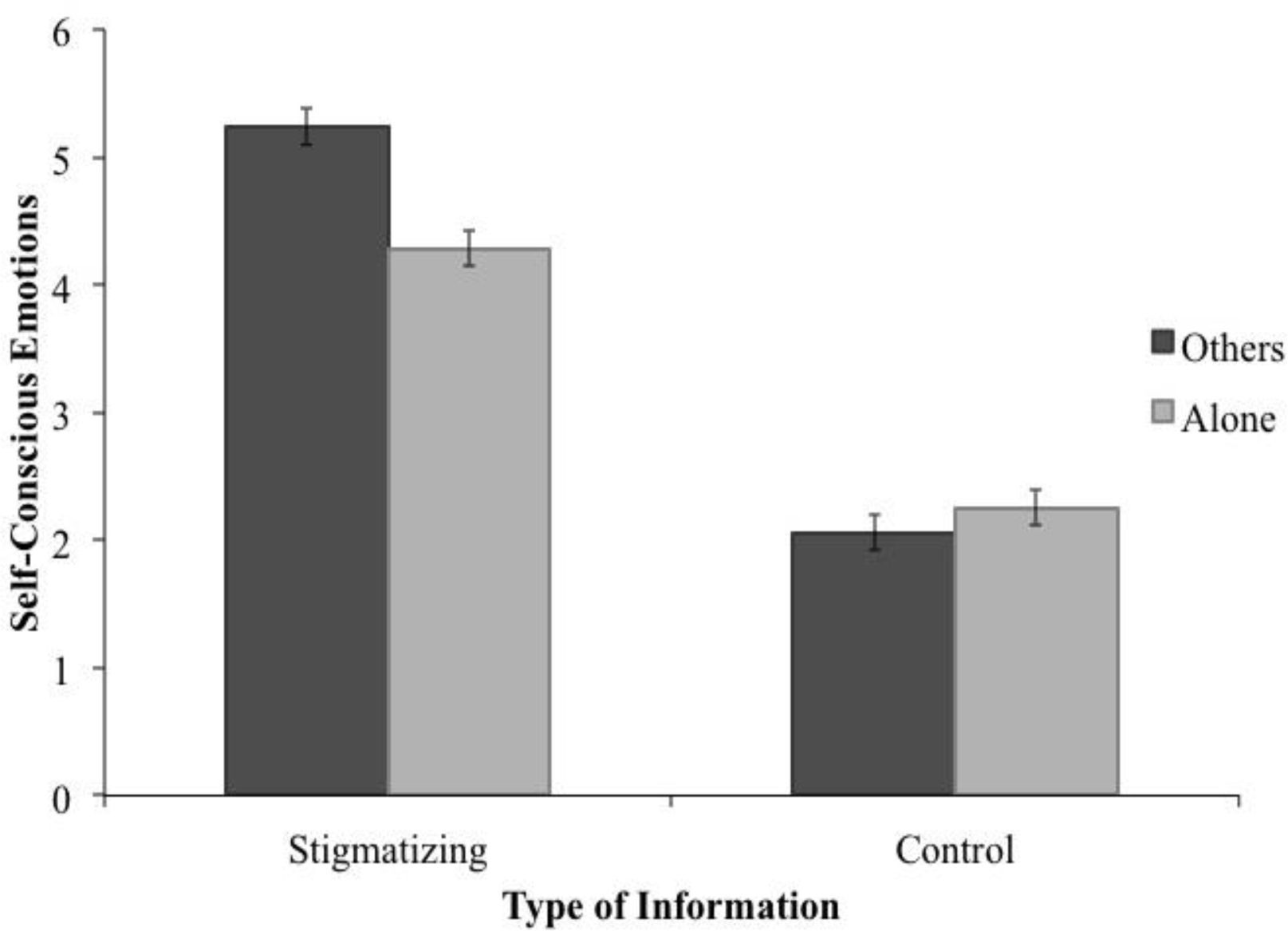
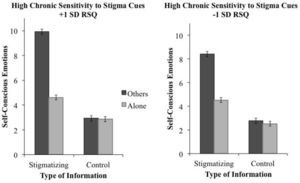
Results and DiscussionStudy 2 tested whether chronic sensitivity to stigma cues (assessed via the Rejection Sensitivity Questionnaire) interacts with situational stigma cues (perceived presence of others). Repeated-measures ANOVA was used with information type (stigmatized vs. control) and presence of others (others present vs. alone) as two within-subjects factors and self-reported chronic sensitivity to stigma cues (the RSQ measure) as a continuous between-subjects variable predicting self-conscious emotions. There was a significant three-way interaction between presence of others, information type, and chronic sensitivity to stigma cues (F(1, 55)=4.56, p = .04; partial η2 = .08; see Figure 2). Overall, selfconscious emotions were highest when scenarios about preventing stigmatized health issues in the presence of others were presented to people with high chronic sensitivity to stigma cues.
Self-reported self-conscious emotions following scenarios about preventing either stigmatizing or control health issues that either indicated the presence or absence of other people, split for people who have high/low chronic sensitivity to stigma cues. For illustrative purposes, means on chronic sensitivity to stigma cues are plotted for participants who are one standard deviation above and below the mean. Standard errors are represented in the figure by the error bars attached to each column.
There were also two significant main effects of information type and presence of others. Participants reported more self-conscious emotions following scenarios about preventing stigmatized (versus control) health issues (Mstigmatized = 5.13, SDstigmatized = 0.21; Mcontrol = 2.24, SDcontrol = 0.20; F(1, 55) = 9.98, p = .003; Cohen's d = 14.09), and when scenarios referenced the presence (versus absence) of others (Mothers = 4.57, SDothers = 0.21; Malone = 2.80, SDalone = 0.19; F(1, 55) = 5.30, p = .03; Cohen's d = 8.84). This replicates Study 1 and suggests that situational effects leading to self-conscious emotions are stronger when people are chronically sensitive to stigma cues.
We also wanted to rule out the possibility that these effects reflected general negative emotionality rather than self-conscious emotions. For this purpose, we used the same analysis to predict self-reported fear. However, the three-way interaction between presence of others, information type, and chronic impression motives was not significant (F(1, 55)=2.73, p = .10; partial η2 = .05). Furthermore, there were no main effects of information type, presence of others, or rejection sensitivity on self-reported fear, nor were any of the two-way interactions significant (all ps > .10; partial η2 < .04).
OverviewSo far we have examined factors that influence stigma cues and subsequent report of self-conscious emotions. Next, we examined if self-conscious emotions influenced the likelihood of attending to health communications. Furthermore, we tested if the effects from the first two studies would generalize across populations by including an Internet sample collected via Amazon's Mechanical Turk.
MethodParticipants and designParticipants were forty-nine users of Amazon's Mechanical Turk who received US$0.50 in exchange for their participation. The design was a 2 (Information type: stigmatized vs. control) X 2 (Presence of others: others versus alone) repeated measures factorial.
Materials and measuresParticipants rated self-conscious emotions and fear following the brochure titles used in Study 1 when the information was either presented in (a) a crowded waiting room or (b) in a private exam room.
Emotion measures. Participants rated both self-conscious emotions (Reading this brochure would lead me to feel self-conscious and be concerned that others would think I have [health issue]) and fear (Reading this brochure would lead me to think about something that is upsetting or overwhelming to think about) on five-point scales ranging from 1 (Strongly Disagree) to 5 (Strongly Agree).
Likelihood measures. Participants rated likelihood of attention to health communications both in a public waiting room (How likely would you be to read this brochure in the waiting room?) and in a private exam room (How likely would you be to read this brochure while alone in a private exam room?) on five-point scales ranging from 1 (Very Unlikely) to 5 (Very Likely).
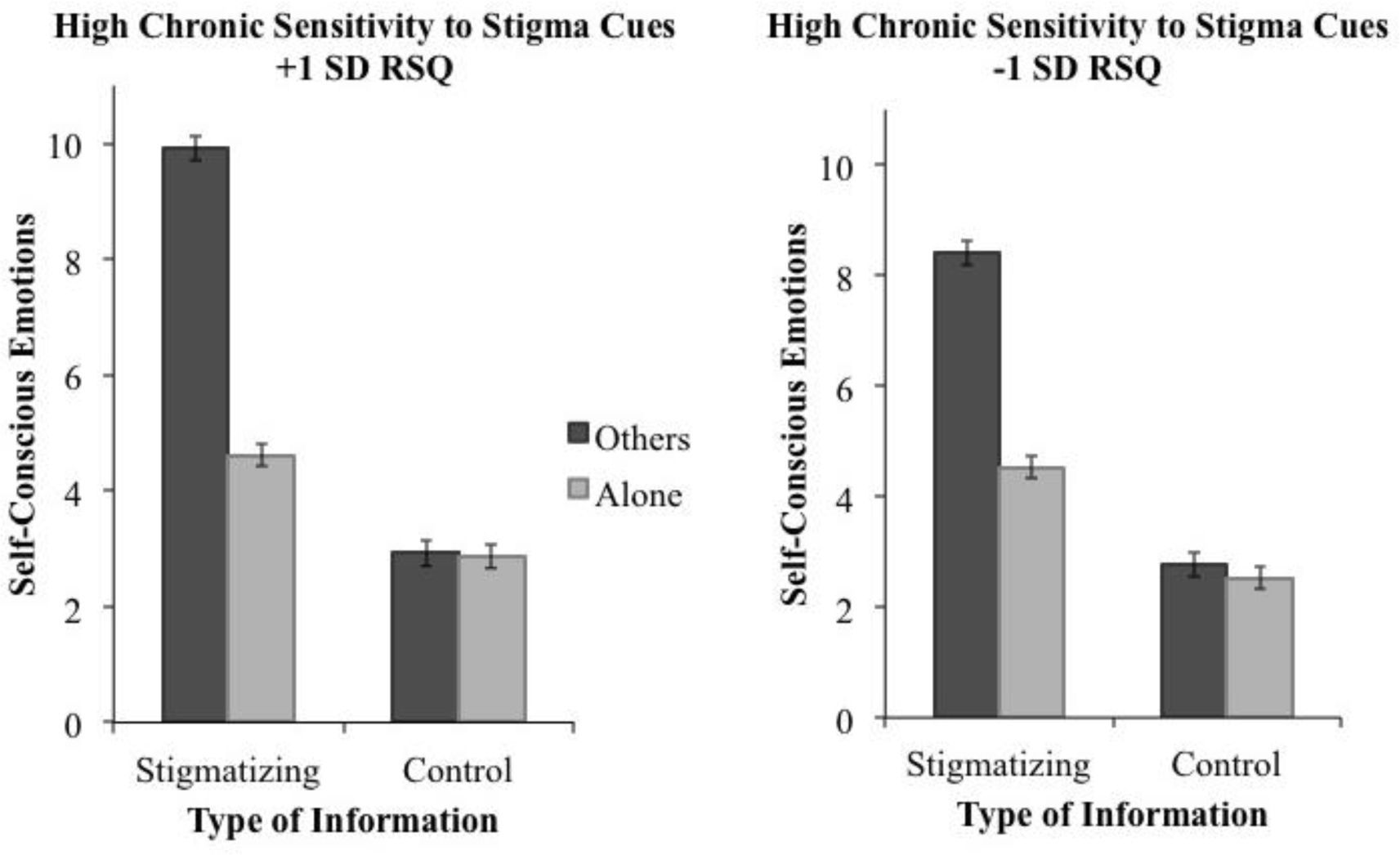
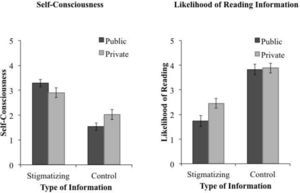
Results and discussionFirst, we tested whether self-conscious emotions would be strongest following stigmatized (versus control) health information presented in a crowded waiting room (versus a private exam room) by using repeated-measures ANOVA with information type and presence of others as two within-subjects factors predicting self-conscious emotion. Replicating the findings from previous studies, there was a significant two-way interaction between presence of others and information type (F(1, 48) = 14.01, p<.001; partial η2 = .27; see Figure 3) such that participants reported increased self-conscious emotion following stigmatized versus control health information (Mstigmatized = 3.09, SDstigmatized= 1.41; Mcontrol = 1.78, SDcontrol = 4.05; F(1, 48) = 62.85, p < .001; Cohen's d = .43), particularly when they imagined being in a public waiting room. In contrast, also replicating earlier results, the interaction between information type and delivery context did not influence fear (F(1, 46) = 0.01, p=.92; partial η2 = .00).
Self-reported self-consciousness (Panel A) and likelihood of attending to information (Panel B) in response to brochures about either stigmatizing or control health issues presented in either a public waiting room or a private exam room. Standard errors are represented in the figure by the error bars attached to each column.
Next, we tested if the likelihood of attending to the health communications varied as a function of information type and delivery context. Paralleling the selfconscious emotion data, there was a significant interaction between information type and delivery context on the likelihood of attending to health communications (F(1, 48)=13.36, p<.001; partial η2 = .22), such that participants were least likely to attend to stigmatizing health communications while in a public waiting room.
Additionally, we examined if self-conscious emotions would influence the likelihood of attending to health communications. For stigmatizing health communications, self-conscious emotions predicted decreased likelihood of attention when the information was presented in a waiting room (β=-.51, p<.001), but not in a private exam room (β=-.05, p = .74). In contrast, fear did not predict the likelihood of attention to stigmatizing communications in either delivery context (waiting room: β=-.18, p=.23; exam room: β = .17, p = .25). Furthermore, the relation between self-conscious emotions and likelihood of attending to stigmatizing health communications in a waiting room remained even when controlling for fear (β=-.54, p<.001). Finally, the difference between selfconscious emotions in the waiting room versus exam room predicted the difference in likelihood of attention to stigmatizing health communications (β=-.35, p = .02). Taken together, these results indicate that increased self-reported self-conscious emotions predict decreased likelihood of attending to health communications.
Summary and Concluding DiscussionAcross three studies, participants reported more self-conscious emotions in response to information about preventing stigmatized health issues when stigma cues are salient. In particular, presenting information about preventing stigmatized health issues when participants (a) perceive that others are present versus absent, and (b) are high versus low in chronic sensitivity to stigma cues resulted in higher levels of self-reported self-conscious emotions. Of note, the pattern of results for self-conscious emotions did not replicate with fear, suggesting a highly specific effect. In addition, self-conscious emotions, but not fear, predicted the likelihood of attending to health communications.
Implications for Health Communication DesignOur work suggests that participants are most likely to report self-conscious emotions when presented with information about preventing stigmatized health issues in the presence of others. Unfortunately, these are precisely the conditions under which information about preventing stigmatized health issues is typically presented at public health facilities and hospitals. One implication of this work, then, is that information designed to prevent such stigmatized diseases as genital herpes or HIV may not reach target audiences. Instead, target audiences may report self-conscious emotions in response to information about preventing stigmatized health issues and subsequently avoid this information as a way of coping with these emotions. More effective strategies of information dissemination might include offering information about preventing stigmatized health issues after participants have left the main waiting room, for instance when participants are waiting for a health care practitioner alone in an individual clinic room.
Another potentially fruitful strategy may be to decrease stigma cues as a way of increasing engagement with information about preventing stigmatized health issues. For instance, a meta-intervention, or scripted introduction to a preexisting intervention program designed to increase enrolment in the program (Albarracin, Durantini, Earl, Gunnoe, & Leeper, 2008), could specifically target stigma cues. Future work should also address the possibility of decreasing the salience of stigma cues as a way of increasing attention to health information.
Limitations and Final NoteAlthough previous work does suggest that self-conscious emotions can have negative effects on testing and health care seeking (Fortenberry et al., 2002; Meiberg et al., 2008), we did not directly measure behaviour in any of our studies. As such, future research should address if the increases in self-conscious emotions and corresponding decreases in likelihood of attending to health communications we reported here do in fact result in decrements in attention to information about preventing stigmatized health issues.
For health communication campaigns to be most effective at ultimately reducing disease, health communications researchers must take into account whether or not target audiences receive prevention messages. Our work suggests that stigma cues may increase reported self-conscious emotions, yet decrease likelihood of attention to health information. As such, health communications researchers should consider how information about preventing stigmatized health issues is presented to minimize the deleterious effects of stigma on attention to health information.
Allison Earl, Department of Psychology, University of Michigan, Christina A. Carino, Department of Psychology, University of Michigan, and Dolores Albarracín, Annenberg School for Communication, University of Pennsylvania.
This research was supported by the National Institute of Mental Health under Grant 1 F31 MH086324-01 to Allison Earl and the National Institutes of Health under Grants K02 MH01861 and R01 NR08325 to Dolores Albarracín. Some of the analyses in some of the studies were included as part of a doctoral dissertation conducted by the first author under the direction of the third author. The authors do not have any financial interest or benefit arising from the direct applications of this research.